Evaluation of Dimensional Stability and Occlusal Wear of Additively and Subtractively Manufactured Resin-Based Crowns after Thermomechanical Aging
Abstract
:1. Introduction
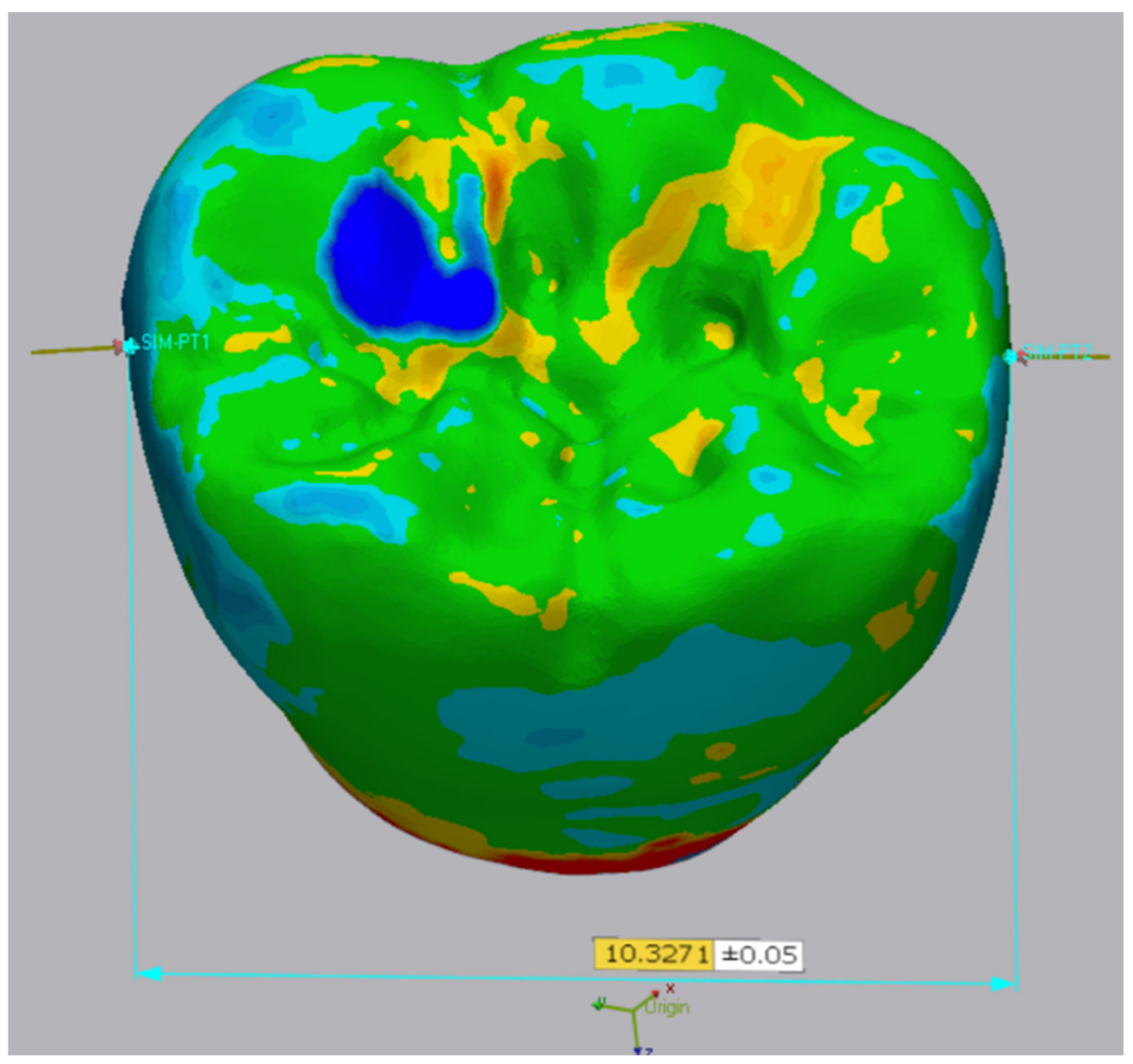
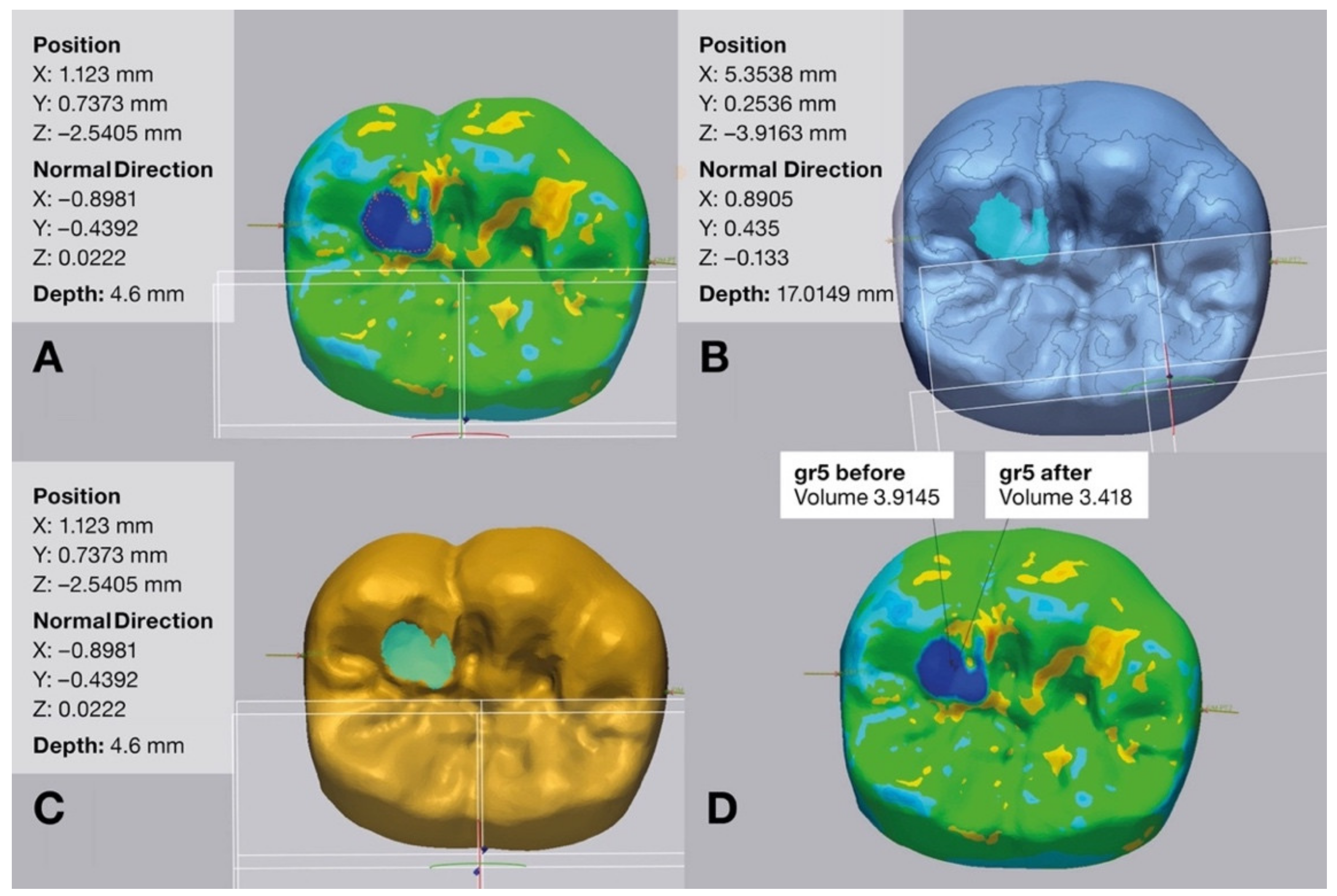
2. Materials and Methods
2.1. Specimen Preparation
2.2. Thermomechanical Aging
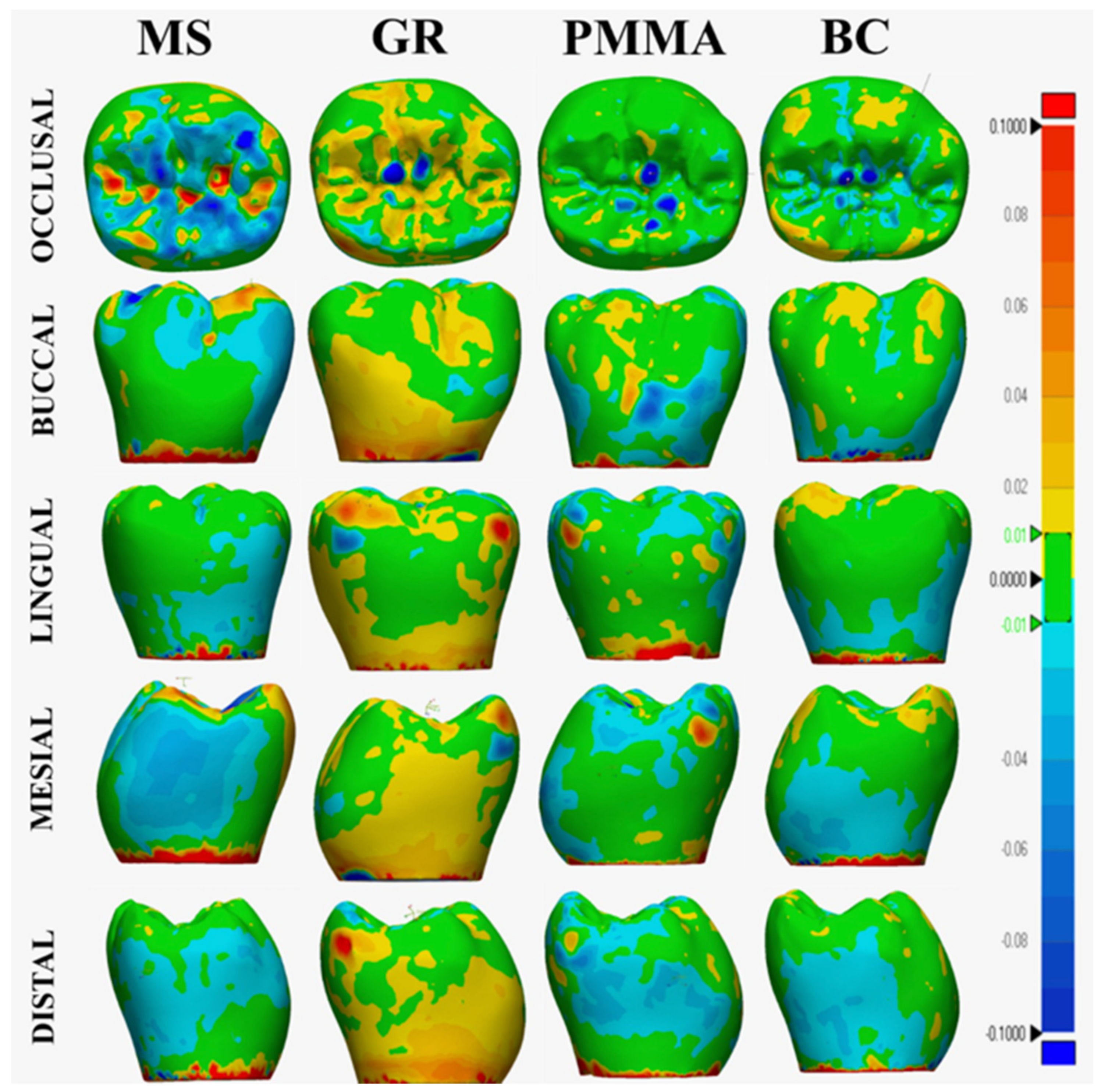
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peng, C.C.; Chung, K.H.; Yau, H.T.; Ramos, V., Jr. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 514–522. [Google Scholar] [CrossRef]
- Guo, N.; Leu, M.C. Additive manufacturing: Technology, applications and research needs. Front. Mech. Eng. 2013, 8, 215–243. [Google Scholar] [CrossRef]
- Ciocan, L.T.; Ghitman, J.; Vasilescu, V.G.; Iovu, H. Mechanical properties of polymer-based blanks for machined dental restorations. Materials 2021, 14, 7293. [Google Scholar] [CrossRef] [PubMed]
- Corbani, K.; Hardan, L.; Eid, R.; Skienhe, H.; Alharbi, N.; Ozcan, M.; Salameh, Z. Fracture resistance of three-unit fixed dental prostheses fabricated with milled and 3D printed composite-based materials. J. Contemp. Dent. Pract. 2021, 22, 985–990. [Google Scholar]
- Agarwalla, S.V.; Malhotra, R.; Rosa, V. Translucency, hardness and strength parameters of PMMA resin containing graphene-like material for CAD/CAM restorations. J. Mech. Behav. Biomed. Mater. 2019, 100, 103388. [Google Scholar] [CrossRef]
- Di Carlo, S.; De Angelis, F.; Brauner, E.; Pranno, N.; Tassi, G.; Senatore, M.; Bossù, M. Flexural strength and elastic modulus evaluation of structures made by conventional PMMA and PMMA reinforced with graphene. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 5201–5208. [Google Scholar]
- Lee, J.-H.; Jo, J.-K.; Kim, D.-A.; Patel, K.D.; Kim, H.-W.; Lee, H.-H. Nano-graphene oxide incorporated into PMMA resin to prevent microbial adhesion. Dent. Mater. 2018, 34, e63–e72. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.S.; Kim, J.E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.Y.; Son, K.; Lee, K.B. Evaluation of intaglio surface trueness and margin quality of interim crowns in accordance with the build angle of stereolithography apparatus 3-dimensional printing. J. Prosthet. Dent. 2021, 126, 231–237. [Google Scholar] [CrossRef]
- Lerner, H.; Nagy, K.; Pranno, N.; Zarone, F.; Admakin, O.; Mangano, F. Trueness and precision of 3D-printed versus milled monolithic zirconia crowns: An in vitro study. J. Dent. 2021, 113, 103792. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Vanini, L.; Rondoni, G.D.; De Angelis, F. Wear properties of dental ceramics and porcelains compared with human enamel. J. Prosthet. Dent. 2016, 115, 350–355. [Google Scholar] [CrossRef]
- Stöckl, C.; Hampe, R.; Stawarczyk, B.; Haerst, M.; Roos, M. Macro- and microtopographical examination and quantification of CAD-CAM composite resin 2- and 3-body wear. J. Prosthet. Dent. 2018, 120, 537–545. [Google Scholar] [CrossRef]
- Diken Turksayar, A.A.; Hisarbeyli, D.; Seçkin Kelten, Ö.; Bulucu, N.B. Wear behavior of current computer-aided design and computer-aided manufacturing composites and reinforced high performance polymers: An in vitro study. J. Esthet. Restor. Dent. 2022, 34, 527–533. [Google Scholar] [CrossRef]
- Zaim, B.; Serin Kalay, T.; Purcek, G. Friction and wear behavior of chairside CAD-CAM materials against different types of antagonists: An in vitro study. J. Prosthet. Dent. 2022, 128, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Corbani, K.; Hardan, L.; Skienhe, H.; Özcan, M.; Alharbi, N.; Salameh, Z. Effect of material thickness on the fracture resistance and failure pattern of 3D-printed composite crowns. Int. J. Comput. Dent. 2020, 23, 225–233. [Google Scholar]
- Zimmermann, M.; Ender, A.; Attin, T.; Mehl, A. Fracture load of three-unit full-contour fixed dental prostheses fabricated with subtractive and additive CAD/CAM technology. Clin. Oral Investig. 2020, 24, 1035–1042. [Google Scholar] [CrossRef]
- Zimmermann, M.; Ender, A.; Egli, G.; Özcan, M.; Mehl, A. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin. Oral Investig. 2019, 23, 2777–2784. [Google Scholar] [CrossRef] [PubMed]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Benalcázar Jalkh, E.; Witek, L.; Sampaio, C.S. 3D-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef]
- Çakmak, G.; Rusa, A.M.; Donmez, M.B.; Akay, C.; Kahveci, Ç.; Schimmel, M.; Yilmaz, B. Trueness of crowns fabricated by using additively and subtractively manufactured resin-based CAD-CAM materials. J. Prosthet. Dent. 2022. [Google Scholar] [CrossRef] [PubMed]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and machinable dental restorative composites for CAD/CAM application—Comparison of mechanical properties, fractographic, texture and fractal dimension analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef]
- Diken Türksayar, A.A.; Demirel, M.; Donmez, M.B.; Olcay, E.O.; Eyüboğlu, T.F.; Özcan, M. Comparison of wear and fracture resistance of additively and subtractively manufactured screw-retained, implant-supported crowns. J. Prosthet. Dent. 2023. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Rauch, A.; Hahnel, S.; Schmidt, M. In-vitro performance of subtractively and additively manufactured resin-based molar crowns. J. Mech. Behav. Biomed. Mater. 2023, 141, 105806. [Google Scholar] [CrossRef]
- Al-Haj Husain, N.; Feilzer, A.J.; Kleverlaan, C.J.; Abou-Ayash, S.; Özcan, M. Effect of hydrothermal aging on the microhardness of high- and low-viscosity conventional and additively manufactured polymers. J. Prosthet. Dent. 2022, 128, 822.e821–822.e829. [Google Scholar] [CrossRef]
- Hernández, J.; Mora, K.; Boquete-Castro, A.; Kina, S. The effect of thermocycling on surface microhardness of PMMA doped with graphene: An experimental in vitro study. J. Clin. Dent. Res. 2020, 17, 152–161. [Google Scholar] [CrossRef]
- Çakmak, G.; Donmez, M.B.; Akay, C.; Abou-Ayash, S.; Schimmel, M.; Yilmaz, B. Effect of thermal cycling on the flexural strength and hardness of new-generation denture base materials. J. Prosthodont. 2023, 32, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Herren, K.V.; Donmez, M.B.; Kahveci, Ç.; Schimmel, M.; Yilmaz, B. Effect of coffee thermocycling on the surface roughness and stainability of nanographene-reinforced polymethyl methacrylate used for fixed definitive prostheses. J. Prosthet. Dent. 2023, 129, 507.e501–507.e506. [Google Scholar] [CrossRef]
- Ionescu, A.C.; Brambilla, E.; Pires, P.M.; López-Castellano, A.; Alambiaga-Caravaca, A.M.; Lenardi, C.; Sauro, S. Physical-chemical and microbiological performances of graphene-doped PMMA for CAD/CAM applications before and after accelerated aging protocols. Dent. Mater. 2022, 38, 1470–1481. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int, J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Sahafi, A.; Flury, S. Bonding of restorative materials to dentin with various luting agents. Oper. Dent. 2011, 36, 266–273. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef]
- The Saremco Website. Available online: https://www.saremco.ch/wp-content/uploads/2021/11/TDS-CROWNTEC_EN_002.pdf (accessed on 6 September 2023).
- Nulty, A.B. A Comparison of full arch trueness and precision of nine intra-oral digital scanners and four lab digital scanners. Dent. J. 2021, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- ISO 12836; Dentistry Digitizing Devices for CAD/CAM Systems for Indirect Dental Restorations: Test Methods for Assessing Accuracy. International Organization of Standardization: Geneva, Switzerland, 2015. Available online: https://www.iso.org/obp/ui/ (accessed on 17 June 2023).
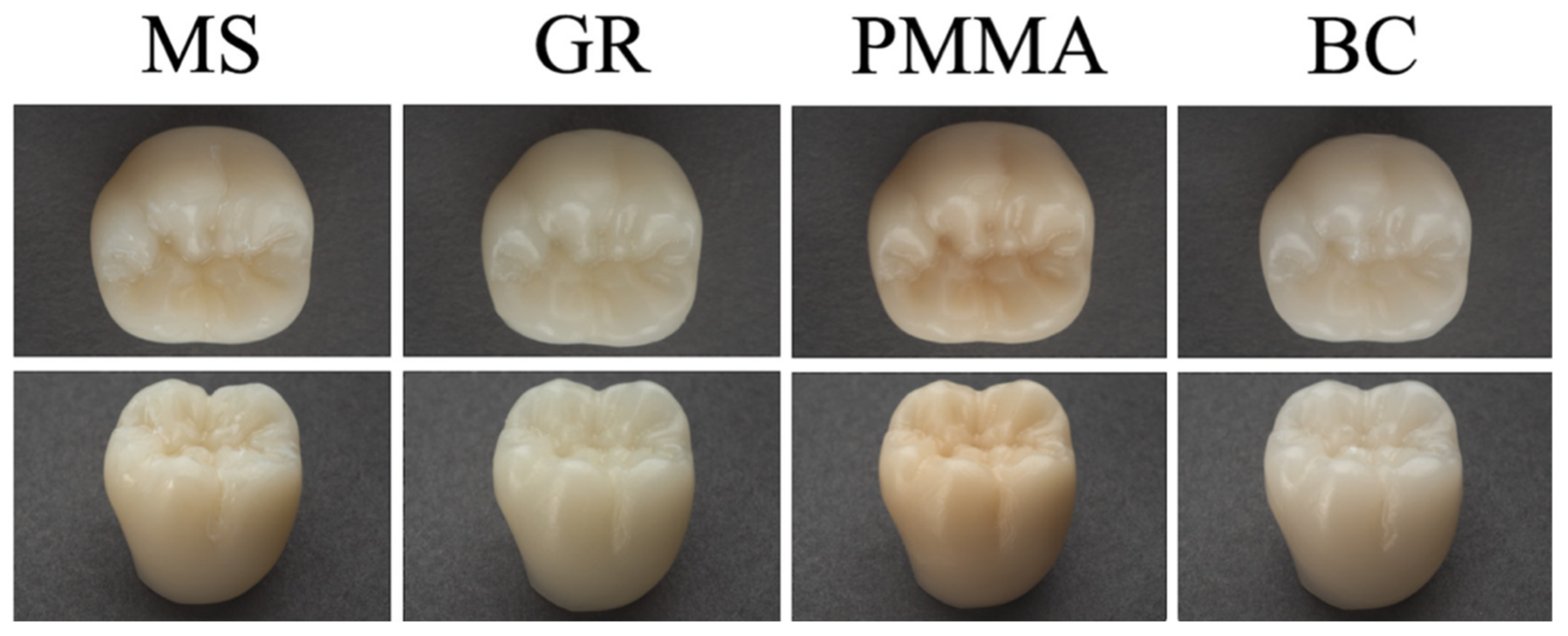


| Material | Type | Composition |
|---|---|---|
| Crowntec (MS) | Additively manufactured composite resin | Esterification products of 4,4′-isopropylidiphenol, ethoxylated and 2-methylprop-2enoic acid, silanized dental glass, pyrogenic silica, initiators. Total content of inorganic fillers (particle size 0.7 μm) is 30–50 wt%. |
| G-CAM (GR) | Subtractively manufactured nanographene-reinforced polymethylmethacrylate | Not disclosed |
| breCAM.monoCOM (PMMA) | Subtractively manufactured polymethylmethacrylate | Polymethylmethacrylate base with low filler content |
| Brilliant Crios (BC) | Subtractively manufactured reinforced composite resin | 70.7 wt% barium glass (<1 µm) and amorphous silica (SiO2; <20 nm), Cross-linked methacrylates (Bis-GMA, Bis-EMA, TEGDMA) |
| External Surface Deviation (µm) | Mesiodistal Width Deviation (µm) | Volume Loss (mm3) | |
|---|---|---|---|
| MS | 149.2 ± 52.0 c | 23.3 ± 11.3 b | 0.7 ± 0.1 ab |
| GR | 105.0 ± 34.0 ab | 15.6 ± 10.3 ab | 0.9 ± 0.23 bc |
| PMMA | 82.9 ± 24.5 a | 9.0 ± 4.7 a | 0.5 ± 0.2 a |
| BC | 132.3 ± 31.1 bc | 8.7 ± 7.1 a | 1.0 ± 0.3 c |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Güven, M.E.; Çakmak, G.; Dönmez, M.B.; Yilmaz, B. Evaluation of Dimensional Stability and Occlusal Wear of Additively and Subtractively Manufactured Resin-Based Crowns after Thermomechanical Aging. Appl. Sci. 2023, 13, 11849. https://doi.org/10.3390/app132111849
Güven ME, Çakmak G, Dönmez MB, Yilmaz B. Evaluation of Dimensional Stability and Occlusal Wear of Additively and Subtractively Manufactured Resin-Based Crowns after Thermomechanical Aging. Applied Sciences. 2023; 13(21):11849. https://doi.org/10.3390/app132111849
Chicago/Turabian StyleGüven, Mehmet Esad, Gülce Çakmak, Mustafa Borga Dönmez, and Burak Yilmaz. 2023. "Evaluation of Dimensional Stability and Occlusal Wear of Additively and Subtractively Manufactured Resin-Based Crowns after Thermomechanical Aging" Applied Sciences 13, no. 21: 11849. https://doi.org/10.3390/app132111849





