Acoustic Fabrication of Collagen–Fibronectin Composite Gels Accelerates Microtissue Formation
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Generation and Characterization of Acoustic Fields
2.2. Fabrication of Composite Collagen–Fibronectin Hydrogels
2.3. Multiphoton Microscopy
2.4. Temperature Measurements
2.5. Microtissue Formation Assay
2.6. Adhesion Assay
2.7. Statistical Analyses
3. Results
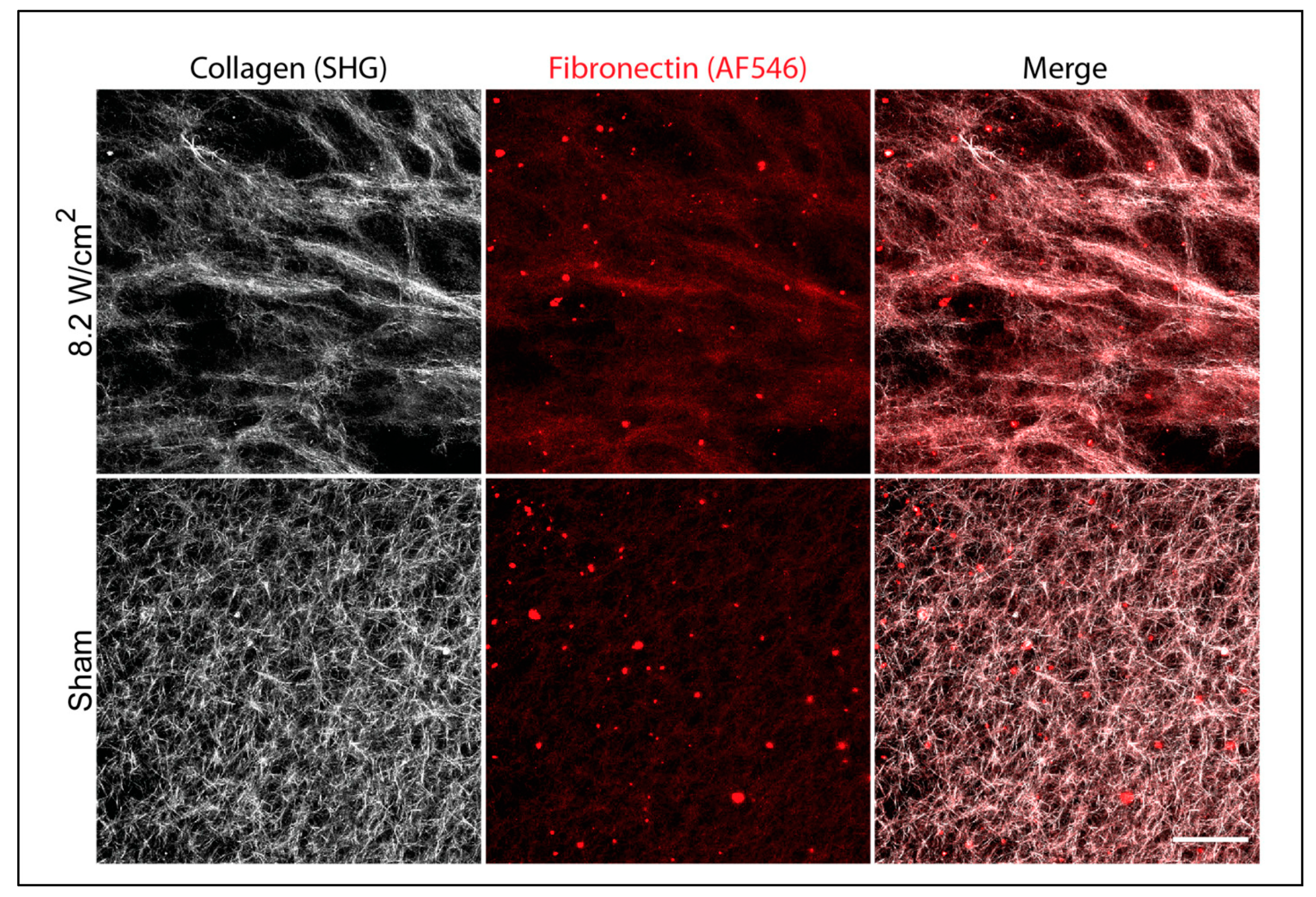
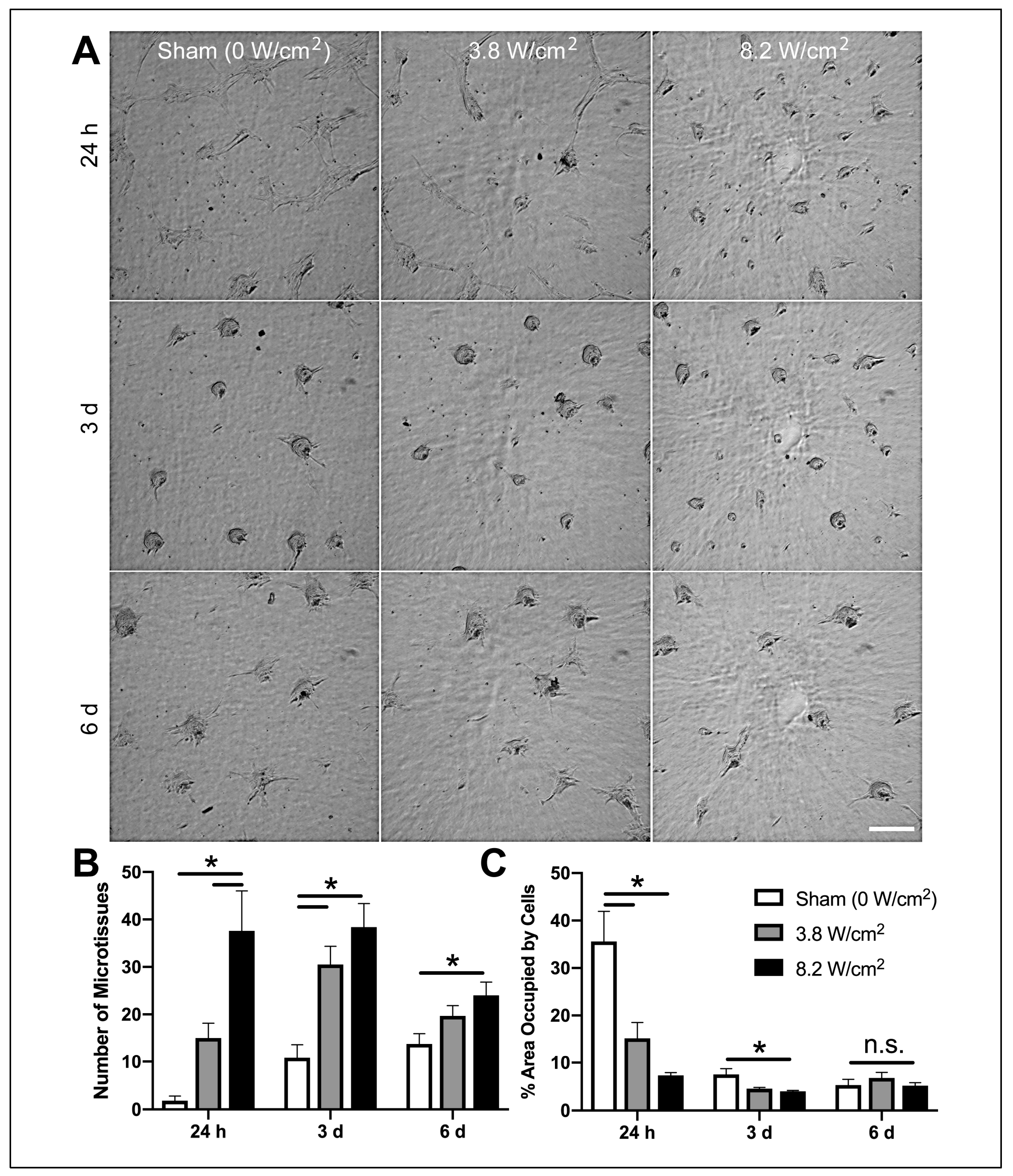
3.1. Ultrasound Exposure Produces Changes in Collagen–Fibronectin Fiber Structure that Support Accelerated Microtissue Formation
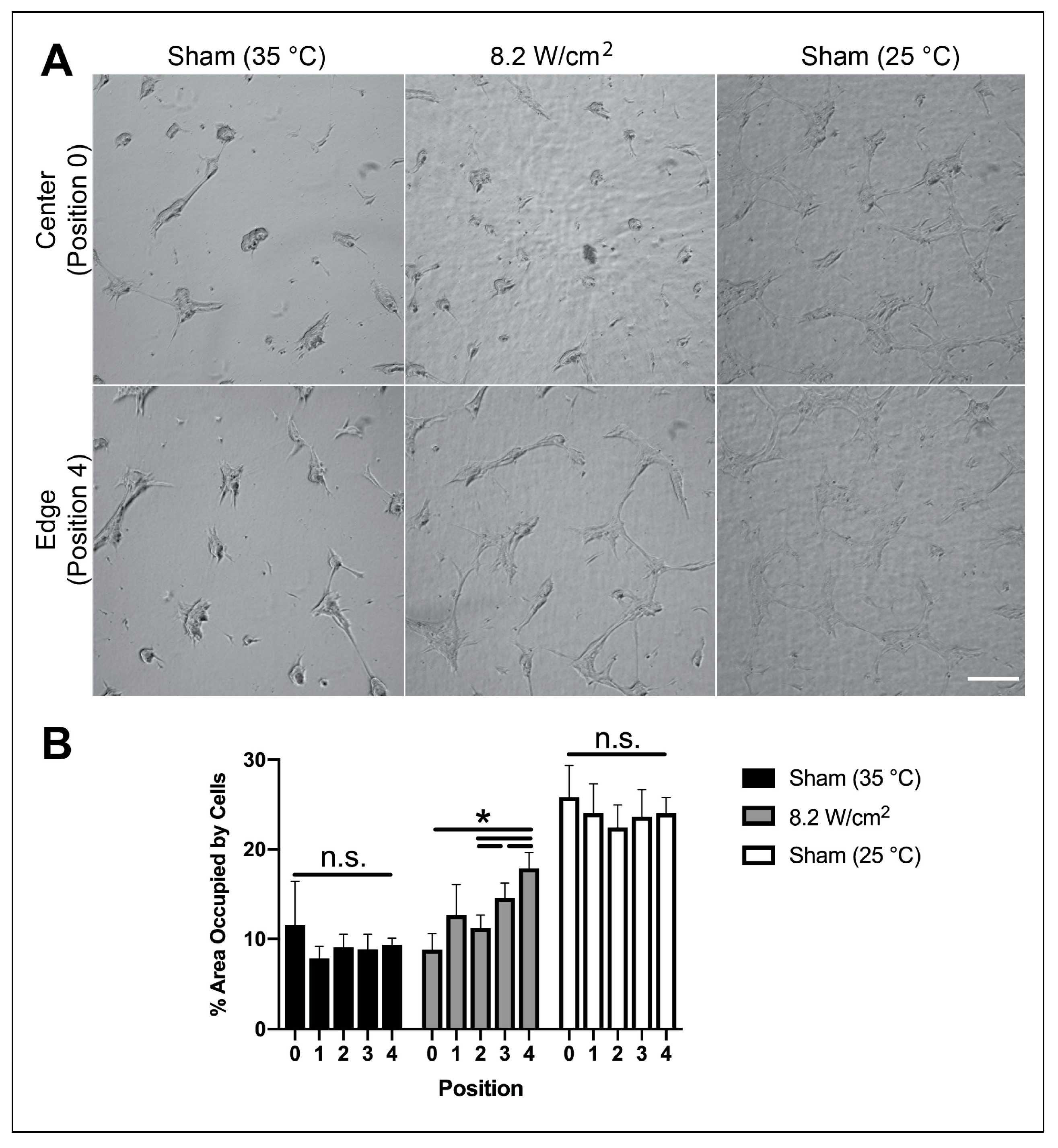
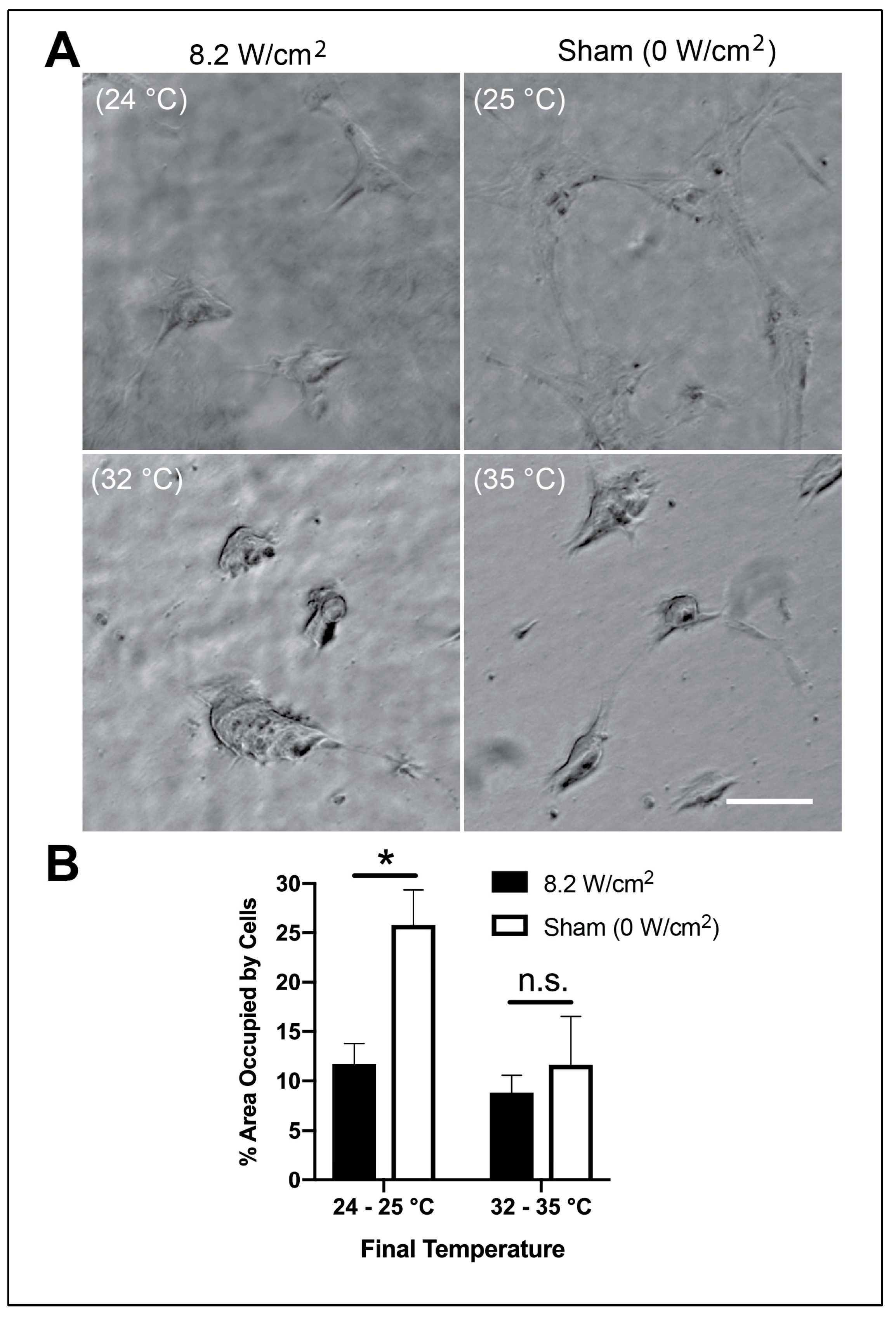
3.2. Effects of Ultrasound on Microtissue Assembly are Temperature-Dependent and Spatially Localized
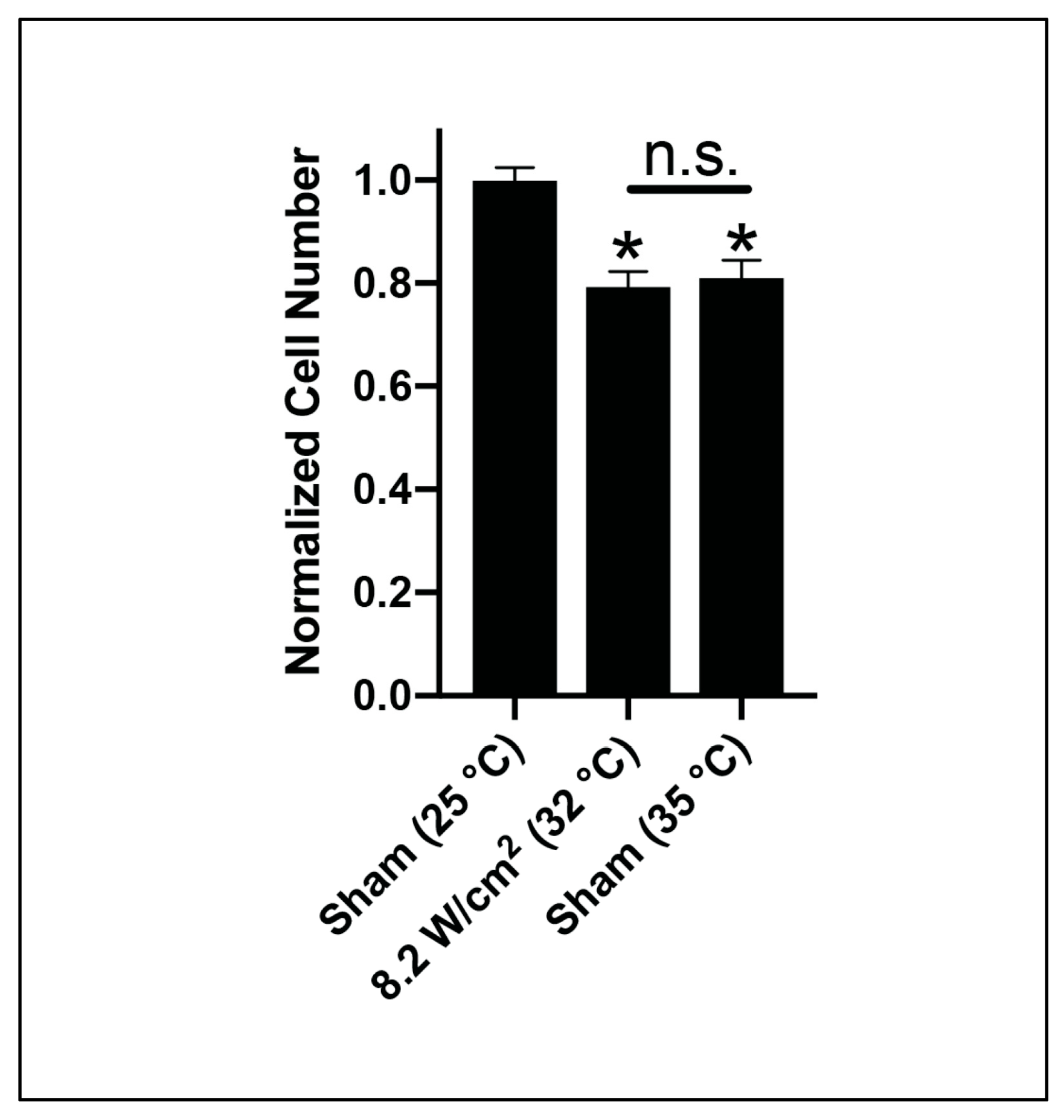
3.3. Acoustic Modification Reduces Initial Adhesion to Collagen–Fibronectin Hydrogels
3.4. Mechanical Effects of Ultrasound on Fibronectin Structure are Observed at Reduced Polymerization Temperature
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A

References
- Langer, R.; Vacanti, J.P. Tissue engineering. Science 1993, 260, 920–926. [Google Scholar] [CrossRef] [Green Version]
- Clark, R.A.; Ghosh, K.; Tonnesen, M.G. Tissue engineering for cutaneous wounds. J. Investig. Dermatol. 2007, 127, 1018–1029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singer, A.J.; Clark, R.A. Cutaneous wound healing. N. Engl. J. Med. 1999, 341, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Falanga, V. Wound healing and its impairment in the diabetic foot. Lancet 2005, 366, 1736–1743. [Google Scholar] [CrossRef]
- Demidova-Rice, T.N.; Hamblin, M.R.; Herman, I.M. Acute and impaired wound healing: Pathophysiology and current methods for drug delivery, part 1: Normal and chronic wounds: Biology, causes, and approaches to care. Adv. Skin Wound Care 2012, 25, 304–314. [Google Scholar] [CrossRef] [Green Version]
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human skin wounds: A major and snowballing threat to public health and the economy. Wound Repair Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [Green Version]
- Fife, C.E.; Eckert, K.A.; Carter, M.J. Publicly reported wound healing rates: The fantasy and the reality. Adv. Wound Care (New Rochelle) 2018, 7, 77–94. [Google Scholar] [CrossRef] [Green Version]
- Shoulders, M.D.; Raines, R.T. Collagen structure and stability. Annu. Rev. Biochem. 2009, 78, 929–958. [Google Scholar] [CrossRef] [Green Version]
- Abou Neel, E.A.; Bozec, L.; Knowles, J.C.; Syed, O.; Mudera, V.; Day, R.; Keun Hyun, J. Collagen - emerging collagen based therapies hit the patient. Adv. Drug Deliv. Rev. 2013, 65, 429–456. [Google Scholar] [CrossRef]
- Wood, G.C. The formation of fibrils from collagen solutions. 2. A mechanism of collagen-fibril formation. Biochem. J. 1960, 75, 598–605. [Google Scholar] [CrossRef] [Green Version]
- Antoine, E.E.; Vlachos, P.P.; Rylander, M.N. Review of collagen I hydrogels for bioengineered tissue microenvironments: Characterization of mechanics, structure, and transport. Tissue Eng. Part. B Rev. 2014, 20, 683–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Place, E.S.; Evans, N.D.; Stevens, M.M. Complexity in biomaterials for tissue engineering. Nat. Mater. 2009, 8, 457–470. [Google Scholar] [CrossRef]
- Singh, P.; Carraher, C.; Schwarzbauer, J.E. Assembly of fibronectin extracellular matrix. Annu. Rev. Cell Dev. Biol. 2010, 26, 397–419. [Google Scholar] [CrossRef] [Green Version]
- Dzamba, B.J.; Wu, H.; Jaenisch, R.; Peters, D.M. Fibronectin binding site in type I collagen regulates fibronectin fibril formation. J. Cell Biol. 1993, 121, 1165–1172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sottile, J.; Hocking, D.C. Fibronectin polymerization regulates the composition and stability of extracellular matrix fibrils and cell-matrix adhesions. Mol. Biol. Cell 2002, 13, 3546–3559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velling, T.; Risteli, J.; Wennerberg, K.; Mosher, D.F.; Johansson, S. Polymerization of type I and III collagens is dependent on fibronectin and enhanced by integrins alpha 11beta 1 and alpha 2beta 1. J. Biol. Chem. 2002, 277, 37377–37381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sottile, J.; Shi, F.; Rublyevska, I.; Chiang, H.Y.; Lust, J.; Chandler, J. Fibronectin-dependent collagen I deposition modulates the cell response to fibronectin. Am. J. Physiol. Cell Physiol. 2007, 293, C1934–C1946. [Google Scholar] [CrossRef] [Green Version]
- Sevilla, C.A.; Dalecki, D.; Hocking, D.C. Regional fibronectin and collagen fibril co-assembly directs cell proliferation and microtissue morphology. PLoS ONE 2013, 8, e77316. [Google Scholar] [CrossRef] [Green Version]
- Gildner, C.D.; Lerner, A.L.; Hocking, D.C. Fibronectin matrix polymerization increases the tensile strength of a model tissue. Am. J. Physiol. Heart Circ. Physiol. 2004, 287, H46–H53. [Google Scholar] [CrossRef] [Green Version]
- Hocking, D.C.; Sottile, J.; Langenbach, K.J. Stimulation of integrin-mediated cell contractility by fibronectin polymerization. J. Biol.Chem. 2000, 275, 10673–10682. [Google Scholar] [CrossRef] [Green Version]
- Dalecki, D. Mechanical bioeffects of ultrasound. Annu. Rev. Biomed. Eng. 2004, 6, 229–248. [Google Scholar] [CrossRef] [PubMed]
- Ingham, K.C.; Brew, S.A.; Isaacs, B.S. Interaction of fibronectin and its gelatin-binding domains with fluorescent-labeled chains of Type I collagen. J. Biol.Chem. 1988, 263, 4624–4628. [Google Scholar] [PubMed]
- Leikina, E.; Mertts, M.V.; Kuznetsova, N.; Leikin, S. Type I collagen is thermally unstable at body temperature. Proc. Natl. Acad. Sci. USA 2002, 99, 1314–1318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kubow, K.E.; Vukmirovic, R.; Zhe, L.; Klotzsch, E.; Smith, M.L.; Gourdon, D.; Luna, S.; Vogel, V. Mechanical forces regulate the interactions of fibronectin and collagen I in extracellular matrix. Nat. Commun. 2015, 6, 8026. [Google Scholar] [CrossRef] [Green Version]
- Smith, M.L.; Gourdon, D.; Little, W.C.; Kubow, K.E.; Eguiluz, R.A.; Luna-Morris, S.; Vogel, V. Force-induced unfolding of fibronectin in the extracellular matrix of living cells. PLoS Biol. 2007, 5, e268. [Google Scholar] [CrossRef]
- Paten, J.A.; Siadat, S.M.; Susilo, M.E.; Ismail, E.N.; Stoner, J.L.; Rothstein, J.P.; Ruberti, J.W. Flow-induced crystallization of collagen: A potentially critical mechanism in early tissue formation. ACS Nano 2016, 10, 5027–5040. [Google Scholar] [CrossRef]
- Garvin, K.A.; VanderBurgh, J.; Hocking, D.C.; Dalecki, D. Controlling collagen fiber microstructure in three-dimensional hydrogels using ultrasound. J. Acoust. Soc. Am. 2013, 134, 1491–1502. [Google Scholar] [CrossRef] [Green Version]
- Norris, E.G.; Dalecki, D.; Hocking, D.C. Acoustic modification of collagen hydrogels facilitates cellular remodeling. Mater. Today Bio. 2019, 3, 100018. [Google Scholar] [CrossRef]
- Norris, E.G.; Majeski, J.; Wayson, S.E.; Coleman, H.; Choe, R.; Dalecki, D.; Hocking, D.C. Non-invasive acoustic fabrication methods to enhance collagen hydrogel bioactivity. Mater. Res. Express 2019, 6. [Google Scholar] [CrossRef]
- Roy, D.C.; Hocking, D.C. Recombinant fibronectin matrix mimetics specify integrin adhesion and extracellular matrix assembly. Tissue Eng. Part. A 2013, 19, 558–570. [Google Scholar] [CrossRef] [Green Version]
- Sottile, J.; Hocking, D.C.; Swiatek, P.J. Fibronectin matrix assembly enhances adhesion-dependent cell growth. J. Cell Sci. 1998, 111, 2933–2943. [Google Scholar] [PubMed]
- Humphries, M.J. Cell-Substrate Adhesion Assays. Curr. Protoc. Cell Biol. 1998, 9.1.1–9.1.11. [Google Scholar] [CrossRef] [PubMed]
- Grinnell, F.; Zhu, M. Fibronectin degradation in chronic wounds depends on the relative levels of elastase, alpha1-proteinase inhibitor, and alpha2-macroglobulin. J. Investig. Dermatol. 1996, 106, 335–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Rocha-Azevedo, B.; Ho, C.H.; Grinnell, F. Fibroblast cluster formation on 3D collagen matrices requires cell contraction dependent fibronectin matrix organization. Exp. Cell Res. 2013, 319, 546–555. [Google Scholar] [CrossRef] [Green Version]
- Brennan, J.R.; Hocking, D.C. Cooperative effects of fibronectin matrix assembly and initial cell-substrate adhesion strength in cellular self-assembly. Acta Biomater. 2016, 32, 198–209. [Google Scholar] [CrossRef] [Green Version]
- Young, T.H.; Lee, C.Y.; Chiu, H.C.; Hsu, C.J.; Lin, S.J. Self-assembly of dermal papilla cells into inductive spheroidal microtissues on poly(ethylene-co-vinyl alcohol) membranes for hair follicle regeneration. Biomaterials 2008, 29, 3521–3530. [Google Scholar] [CrossRef]
- Engvall, E.; Ruoslahti, E.; Miller, E.J. Affinity of fibronectin to collagens of different genetic types and to fibrinogen. J. Exp. Med. 1978, 147, 1584–1595. [Google Scholar] [CrossRef] [Green Version]
- Ejim, O.S.; Blunn, G.W.; Brown, R.A. Production of artificial-orientated mats and strands from plasma fibronectin: A morphological study. Biomaterials 1993, 14, 743–748. [Google Scholar] [CrossRef]
- Baneyx, G.; Vogel, V. Self-assembly of fibronectin into fibrilar networks underneath dipalmitoyl phosphatidylcholine monolayers: Role of lipid matrix and tensile forces. Proc. Natl. Acad. Sci. USA 1999, 96, 12518–12523. [Google Scholar] [CrossRef] [Green Version]
- Paten, J.A.; Martin, C.L.; Wanis, J.T.; Siadat, S.M.; Figueroa-Navedo, A.M.; Ruberti, J.W.; Deravi, L.F. Molecular interactions between collagen and fibronectin: A reciprocal relationship that regulates de novo fibrillogenesis. Chem 2019, 5, 2126–2145. [Google Scholar] [CrossRef]
- Zhong, C.; Chrzanowska-Wodnicka, M.; Brown, J.; Shaub, A.; Belkin, A.M.; Burridge, K. Rho-mediated contractility exposes a cryptic site in fibronecitn and induces fibronectin matrix assembly. J. Cell Biol. 1998, 141, 539–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Water Tank Temperature | Acoustic Intensity (ISPPA) | Peak Positive Pressure | Peak Negative Pressure | Final Temperature |
|---|---|---|---|---|
| 18 °C | 8.2 ± 0.1 W/cm2 | 0.76 ± 0.02 MPa | 0.44 ± 0.02 MPa | 24.2 ± 0.3 °C |
| 25 °C | Sham (0 W/cm2) | - | - | 24.6 ± 0.1 °C |
| 25 °C | 3.8 ± 0.1 W/cm2 | 0.48 ± 0.02 MPa | 0.28 ± 0.02 MPa | 27.7 ± 0.1 °C |
| 25 °C | 8.2 ± 0.1 W/cm2 | 0.76 ± 0.02 MPa | 0.44 ± 0.02 MPa | 32.3 ± 0.2 °C |
| 37 °C | Sham (0 W/cm2) | - | - | 34.5 ± 0.1 °C |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Norris, E.G.; Dalecki, D.; Hocking, D.C. Acoustic Fabrication of Collagen–Fibronectin Composite Gels Accelerates Microtissue Formation. Appl. Sci. 2020, 10, 2907. https://doi.org/10.3390/app10082907
Norris EG, Dalecki D, Hocking DC. Acoustic Fabrication of Collagen–Fibronectin Composite Gels Accelerates Microtissue Formation. Applied Sciences. 2020; 10(8):2907. https://doi.org/10.3390/app10082907
Chicago/Turabian StyleNorris, Emma G., Diane Dalecki, and Denise C. Hocking. 2020. "Acoustic Fabrication of Collagen–Fibronectin Composite Gels Accelerates Microtissue Formation" Applied Sciences 10, no. 8: 2907. https://doi.org/10.3390/app10082907





