Impacts of F18+ Escherichia coli on Intestinal Health of Nursery Pigs and Dietary Interventions
Abstract
:Simple Summary
Abstract
1. Introduction
2. Virulence Factors of F18+ Escherichia coli
2.1. Fimbriae
2.2. Adhesin Involved in Diffuse Adherence
2.3. Lipopolysaccharides
2.4. Enterotoxins
2.4.1. STa
2.4.2. STb
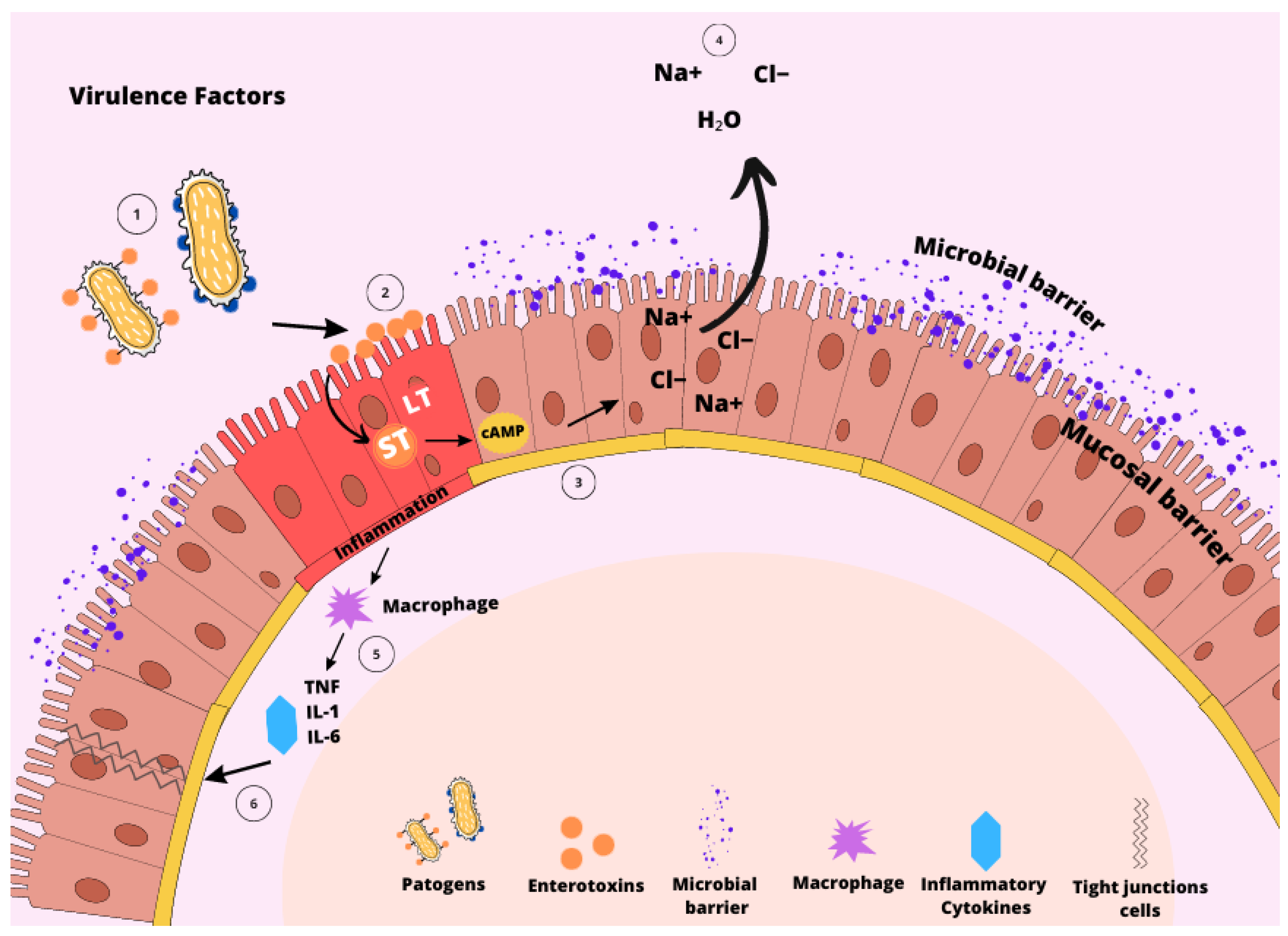
3. Pathogenesis of F18+ Escherichia coli
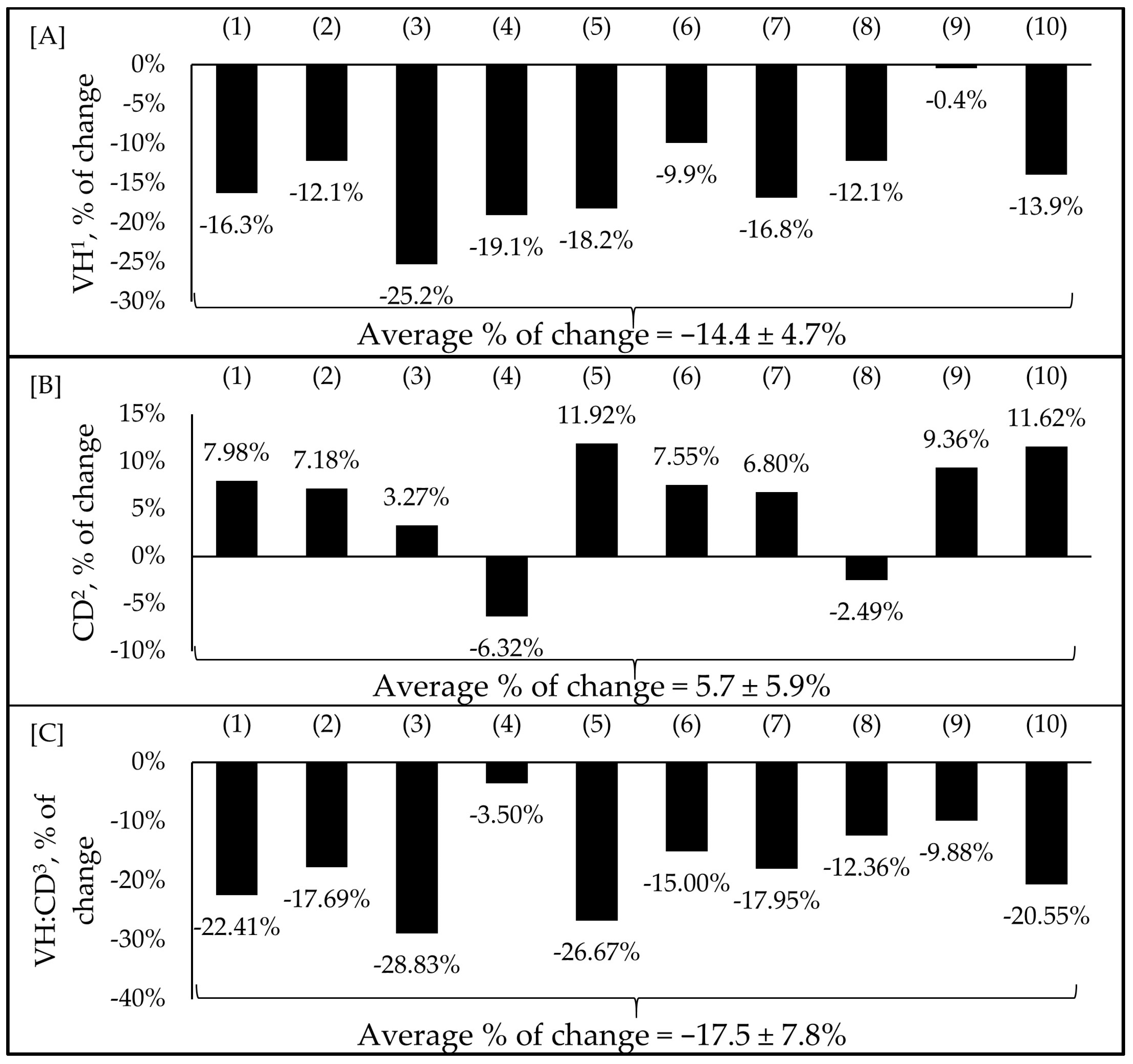
4. Physiological, Clinical, Immunological, and Growth Responses of Pigs
5. Nutritional Interventions
5.1. Low Crude Protein Diets
5.2. Zinc
5.3. Copper
5.4. Probiotics
5.5. Prebiotics
5.6. Postbiotics
5.7. Phytobiotics
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lallès, J.-P.; Boudry, G.; Favier, C.; Le Floc’h, N.; Luron, I.; Montagne, L.; Oswald, I.P.; Pié, S.; Piel, C.; Sève, B. Gut Function and Dysfunction in Young Pigs: Physiology. Anim. Res. 2004, 53, 301–316. [Google Scholar] [CrossRef]
- Zheng, L.; Duarte, M.E.; Sevarolli Loftus, A.; Kim, S.W. Intestinal Health of Pigs upon Weaning: Challenges and Nutritional Intervention. Front. Vet. Sci. 2021, 8, 628258. [Google Scholar] [CrossRef]
- Hampson, D.J. Alterations in Piglet Small Intestinal Structure at Weaning. Res. Vet. Sci. 1986, 40, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Frydendahl, K. Prevalence of Serogroups and Virulence Genes in Escherichia coli Associated with Postweaning Diarrhoea and Edema Disease in Pigs and a Comparison of Diagnostic Approaches. Vet. Microbiol. 2002, 85, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Luppi, A.; Gibellini, M.; Gin, T.; Vangroenweghe, F.; Vandenbroucke, V.; Bauerfeind, R.; Bonilauri, P.; Labarque, G.; Hidalgo, Á. Prevalence of Virulence Factors in Enterotoxigenic Escherichia coli Isolated from Pigs with Post-Weaning Diarrhoea in Europe. Porc. Health Manag. 2016, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Post, K.W.; Bosworth, B.T.; Knoth, J.L. Frequency of Virulence Factors in Escherichia coli Isolated from Pigs with Postweaning Diarrhea and Edema Disease in North Carolina. J. Swine Health Prod. 2000, 8, 119–120. [Google Scholar]
- Xu, X.; Duarte, M.E.; Kim, S.W. Postbiotic Effects of Lactobacillus Fermentate on Intestinal Health, Mucosa-Associated Microbiota, and Growth Efficiency of Nursery Pigs Challenged with F18+ Escherichia coli. J. Anim. Sci. 2022, 100, skac210. [Google Scholar] [CrossRef]
- Duarte, M.E.; Kim, S.W. Significance of Mucosa-Associated Microbiota and Its Impacts on Intestinal Health of Pigs Challenged with F18+ E. coli. Pathogens 2022, 11, 589. [Google Scholar] [CrossRef]
- He, Y.; Jinno, C.; Kim, K.; Wu, Z.; Tan, B.; Li, X.; Whelan, R.; Liu, Y. Dietary Bacillus spp. Enhanced Growth and Disease Resistance of Weaned Pigs by Modulating Intestinal Microbiota and Systemic Immunity. J. Anim. Sci. Biotechnol. 2020, 11, 101. [Google Scholar] [CrossRef]
- Fairbrother, J.M.; Nadeau, É. Colibacillosis. In Diseases of Swine; Zimmerman, J.J., Karriker, L.A., Ramirez, A., Schwartz, K.J., Stevenson, G.W., Zhang, J., Eds.; Wiley: Hoboken, NJ, USA, 2019; pp. 807–834. ISBN 9781119350927. [Google Scholar]
- Nielsen, S.S.; Bicout, D.J.; Calistri, P.; Canali, E.; Drewe, J.A.; Garin-Bastuji, B.; Gonzales Rojas, J.L.; Gortázar, C.; Herskin, M.; Michel, V.; et al. Assessment of Listing and Categorisation of Animal Diseases within the Framework of the Animal Health Law (Regulation (EU) No 2016/429): Antimicrobial-resistant Escherichia coli in Dogs and Cats, Horses, Swine, Poultry, Cattle, Sheep and Goats. EFSA J. 2022, 20, e07311. [Google Scholar] [CrossRef]
- Amezcua, R.; Friendship, R.M.; Dewey, C.E.; Gyles, C.; Fairbrother, J.M. Presentation of Postweaning Escherichia coli Diarrhea in Southern Ontario, Prevalence of Hemolytic E. coli Serogroups Involved, and Their Antimicrobial Resistance Patterns. Can. J. Vet. Res. 2002, 66, 73–78. [Google Scholar] [PubMed]
- Luppi, A. Swine Enteric Colibacillosis: Diagnosis, Therapy and Antimicrobial Resistance. Porc. Health Manag. 2017, 3, 16. [Google Scholar] [CrossRef] [PubMed]
- Curcio, L.; Luppi, A.; Bonilauri, P.; Gherpelli, Y.; Pezzotti, G.; Pesciaroli, M.; Magistrali, C.F. Detection of the Colistin Resistance Gene Mcr-1 in Pathogenic Escherichia coli from Pigs Affected by Post-Weaning Diarrhoea in Italy. J. Glob. Antimicrob. Resist. 2017, 10, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Castro, J.; Barros, M.M.; Araújo, D.; Campos, A.M.; Oliveira, R.; Silva, S.; Almeida, C. Swine Enteric Colibacillosis: Current Treatment Avenues and Future Directions. Front. Vet. Sci. 2022, 9, 981207. [Google Scholar] [CrossRef]
- Duarte, M.E.; Stahl, C.H.; Kim, S.W. Intestinal Damages by F18+ Escherichia coli and Its Amelioration with an Antibacterial Bacitracin Fed to Nursery Pigs. Antioxidants 2023, 12, 1040. [Google Scholar] [CrossRef]
- Zhang, W.; Zhao, M.; Ruesch, L.; Omot, A.; Francis, D. Prevalence of Virulence Genes in Escherichia Coli Strains Recently Isolated from Young Pigs with Diarrhea in the US. Vet. Microbiol. 2007, 123, 145–152. [Google Scholar] [CrossRef]
- Fairbrother, J.M.; Nadeau, É.; Gyles, C.L. Escherichia coli in Postweaning Diarrhea in Pigs: An Update on Bacterial Types, Pathogenesis, and Prevention Strategies. Anim. Health Res. Rev. 2005, 6, 17–39. [Google Scholar] [CrossRef]
- Rippinger, P.; Bertschinger, H.U.; Imberechts, H.; Nagy, B.; Sorg, I.; Stamm, M.; Wild, P.; Wittig, W. Designations F18ab and F18ac for the Related Fimbrial Types F107, 2134P and 8813 of Escherichia coli Isolated from Porcine Postweaning Diarrhoea and from Oedema Disease. Vet. Microbiol. 1995, 45, 281–295. [Google Scholar] [CrossRef]
- Nagy, B.; Whipp, S.C.; Imberechts, H.; Bertschinger, H.U.; Dean-Nystrom, E.A.; Casey, T.A.; Salajka, E. Biological Relationship between F18ab and F18ac Fimbriae of Enterotoxigenic and Verotoxigenic Escherichia coli from Weaned Pigs with Oedema Disease or Diarrhoea. Microb. Pathog. 1997, 22, 1–11. [Google Scholar] [CrossRef]
- Kim, Y.J.; Kim, J.H.; Hur, J.; Lee, J.H. Isolation of Escherichia coli from Piglets in South Korea with Diarrhea and Characteristics of the Virulence Genes. Can. J. Vet. Res. 2010, 74, 59–64. [Google Scholar]
- Weber, N.; Nielsen, J.P.; Jakobsen, A.S.; Pedersen, L.L.; Hansen, C.F.; Pedersen, K.S. Occurrence of Diarrhoea and Intestinal Pathogens in Non-Medicated Nursery Pigs. Acta Vet. Scand. 2015, 57, 64. [Google Scholar] [CrossRef] [PubMed]
- Bessone, F.A.; Bessone, G.; Marini, S.; Conde, M.B.; Alustiza, F.E.; Zielinski, G. Presence and Characterization of Escherichia coli Virulence Genes Isolated from Diseased Pigs in the Central Region of Argentina. Vet. World 2017, 10, 939–945. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Zhao, X.; Li, J.; Yang, C. Post-Weaning Diarrhea and Use of Feedstuffs in Pigs. Anim. Front. 2022, 12, 41–52. [Google Scholar] [CrossRef]
- Pedersen, K.S.; Okholm, E.; Johansen, M.; Angen, Ø.; Jorsal, S.E.; Nielsen, J.P.; Bækbo, P. Clinical Utility and Performance of Sock Sampling in Weaner Pig Diarrhoea. Prev. Vet. Med. 2015, 120, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Frömmel, U.; Lehmann, W.; Rödiger, S.; Böhm, A.; Nitschke, J.; Weinreich, J.; Groß, J.; Roggenbuck, D.; Zinke, O.; Ansorge, H.; et al. Adhesion of Human and Animal Escherichia coli Strains in Association with Their Virulence-Associated Genes and Phylogenetic Origins. Appl. Environ. Microbiol. 2013, 79, 5814–5829. [Google Scholar] [CrossRef]
- Mohlatlole, R.P.; Madoroba, E.; Muchadeyi, F.C.; Chimonyo, M.; Kanengoni, A.T.; Dzomba, E.F. Virulence Profiles of Enterotoxigenic, Shiga Toxin and Enteroaggregative Escherichia coli in South African Pigs. Trop. Anim. Health Prod. 2013, 45, 1399–1405. [Google Scholar] [CrossRef]
- Rueter, C.; Bielaszewska, M. Secretion and Delivery of Intestinal Pathogenic Escherichia coli Virulence Factors via Outer Membrane Vesicles. Front. Cell Infect. Microbiol. 2020, 10, 91. [Google Scholar] [CrossRef]
- Osek, J. Prevalence of Virulence Factors of Escherichia coli Strains Isolated from Diarrheic and Healthy Piglets after Weaning. Vet. Microbiol. 1999, 68, 209–217. [Google Scholar] [CrossRef]
- Yang, F.; Wang, A.; Zeng, X.; Hou, C.; Liu, H.; Qiao, S. Lactobacillus Reuteri I5007 Modulates Tight Junction Protein Expression in IPEC-J2 Cells with LPS Stimulation and in Newborn Piglets under Normal Conditions. BMC Microbiol. 2015, 15, 32. [Google Scholar] [CrossRef]
- Ravi, M.; Ngeleka, M.; Kim, S.-H.; Gyles, C.; Berthiaume, F.; Mourez, M.; Middleton, D.; Simko, E. Contribution of AIDA-I to the Pathogenicity of a Porcine Diarrheagenic Escherichia coli and to Intestinal Colonization through Biofilm Formation in Pigs. Vet. Microbiol. 2007, 120, 308–319. [Google Scholar] [CrossRef]
- Duarte, M.E.; Kim, S.W. Intestinal Microbiota and Its Interaction to Intestinal Health in Nursery Pigs. Anim. Nutr. 2022, 8, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Francis, D.H. Enterotoxigenic Escherichia coli Infection in Pigs and Its Diagnosis. J. Swine Health Prod. 2002, 10, 171–175. [Google Scholar]
- Imberechts, H.; Wild, P.; Charlier, G.; De Greve, H.; Lintermans, P.; Pohl, P. Characterization of F18 Fimbrial Genes fedE andfedF involved in Adhesion and Length of Enterotoxemic Escherichia coli strain 107/86. Microb. Pathog. 1996, 21, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Coddens, A.; Verdonck, F.; Tiels, P.; Rasschaert, K.; Goddeeris, B.M.; Cox, E. The Age-Dependent Expression of the F18+ E. coli Receptor on Porcine Gut Epithelial Cells Is Positively Correlated with the Presence of Histo-Blood Group Antigens. Vet. Microbiol. 2007, 122, 332–341. [Google Scholar] [CrossRef]
- Nagy, B.; Fekete, P.Z. Enterotoxigenic Escherichia coli in Veterinary Medicine. Int. J. Med. Microbiol. 2005, 295, 443–454. [Google Scholar] [CrossRef]
- Rehman, T.; Yin, L.; Latif, M.B.; Chen, J.; Wang, K.; Geng, Y.; Huang, X.; Abaidullah, M.; Guo, H.; Ouyang, P. Adhesive Mechanism of Different Salmonella Fimbrial Adhesins. Microb. Pathog. 2019, 137, 103748. [Google Scholar] [CrossRef]
- Dai, C.; Yang, L.; Jin, J.; Wang, H.; Wu, S.; Bao, W. Regulation and Molecular Mechanism of TLR5 on Resistance to Escherichia coli F18 in Weaned Piglets. Animals 2019, 9, 735. [Google Scholar] [CrossRef]
- Barros, M.M.; Castro, J.; Araújo, D.; Campos, A.M.; Oliveira, R.; Silva, S.; Outor-Monteiro, D.; Almeida, C. Swine Colibacillosis: Global Epidemiologic and Antimicrobial Scenario. Antibiotics 2023, 12, 682. [Google Scholar] [CrossRef]
- Ngeleka, M.; Pritchard, J.; Appleyard, G.; Middleton, D.M.; Fairbrother, J.M. Isolation and Association of Escherichia Coli AIDA-I/STb, Rather than EAST1 Pathotype, with Diarrhea in Piglets and Antibiotic Sensitivity of Isolates. J. Vet. Diagn. Investig. 2003, 15, 242–252. [Google Scholar] [CrossRef]
- Niewerth, U.; Frey, A.; Voss, T.; Le Bouguénec, C.; Baljer, G.; Franke, S.; Schmidt, M.A. The AIDA Autotransporter System Is Associated with F18 and Stx2e in Escherichia coli Isolates from Pigs Diagnosed with Edema Disease and Postweaning Diarrhea. Clin. Diagn. Lab. Immunol. 2001, 8, 143–149. [Google Scholar] [CrossRef]
- Tieng, V.; Le Bouguénec, C.; du Merle, L.; Bertheau, P.; Desreumaux, P.; Janin, A.; Charron, D.; Toubert, A. Binding of Escherichia coli adhesin AfaE to CD55 triggers cell-surface expression of the MHC class I-related molecule MICA. Proc. Natl. Acad. Sci. USA 2002, 99, 2977–2982. [Google Scholar] [CrossRef]
- Hawkins, P.T.; Stephens, L.R. PI3K signalling in inflammation. Biochim. Biophys. Acta—Mol. Cell Biol. Lipids 2015, 1851, 882–897. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Feye, K.M.; Nguyen, Y.T.; Rakhshandeh, A.; Loving, C.L.; Dekkers, J.C.M.; Gabler, N.K.; Tuggle, C.K. Acute Systemic Inflammatory Response to Lipopolysaccharide Stimulation in Pigs Divergently Selected for Residual Feed Intake. BMC Genom. 2019, 20, 728. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Qin, L.; Du, R.; Chen, Y.; Lei, M.; Deng, M.; Wang, J. Lipopolysaccharide Upregulated Intestinal Epithelial Cell Expression of Fn14 and Activation of Fn14 Signaling Amplify Intestinal TLR4-Mediated Inflammation. Front. Cell Infect. Microbiol. 2017, 7, 315. [Google Scholar] [CrossRef] [PubMed]
- Kaper, J.B.; Nataro, J.P.; Mobley, H.L.T. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2004, 2, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Nighot, M.; Al-Sadi, R.; Alhmoud, T.; Nighot, P.; Ma, T.Y. Lipopolysaccharide Regulation of Intestinal Tight Junction Permeability Is Mediated by TLR4 Signal Transduction Pathway Activation of FAK and MyD88. J. Immunol. 2015, 195, 4999–5010. [Google Scholar] [CrossRef]
- Hartadi, E.B.; Effendi, M.H.; Plumeriastuti, H.; Sofiana, E.D.; Wibisono, F.M.; Hidayatullah, A.R. A Review of Enterotoxigenic Escherichia coli Infection in Piglets: Public Health Importance. Syst. Rev. Pharm. 2020, 11, 687–698. [Google Scholar]
- Read, L.T.; Hahn, R.W.; Thompson, C.C.; Bauer, D.L.; Norton, E.B.; Clements, J.D. Simultaneous Exposure to Escherichia coli Heat-Labile and Heat-Stable Enterotoxins Increases Fluid Secretion and Alters Cyclic Nucleotide and Cytokine Production by Intestinal Epithelial Cells. Infect. Immun. 2014, 82, 5308–5316. [Google Scholar] [CrossRef]
- Dubreuil, J.D.; Isaacson, R.E.; Schifferli, D.M. Animal Enterotoxigenic Escherichia coli. EcoSal Plus 2016, 7, 1–47. [Google Scholar] [CrossRef]
- Liu, W.; Yuan, C.; Meng, X.; Du, Y.; Gao, R.; Tang, J.; Shi, D. Frequency of Virulence Factors in Escherichia coli Isolated from Suckling Pigs with Diarrhoea in China. Vet. J. 2014, 199, 286–289. [Google Scholar] [CrossRef]
- Wang, H.; Zhong, Z.; Luo, Y.; Cox, E.; Devriendt, B. Heat-Stable Enterotoxins of Enterotoxigenic Escherichia coli and Their Impact on Host Immunity. Toxins 2019, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Bölin, I.; Wiklund, G.; Qadri, F.; Torres, O.; Bourgeois, A.L.; Savarino, S.; Svennerholm, A.-M. Enterotoxigenic Escherichia coli with STh and STp Genotypes Is Associated with Diarrhea Both in Children in Areas of Endemicity and in Travelers. J. Clin. Microbiol. 2006, 44, 3872–3877. [Google Scholar] [CrossRef] [PubMed]
- Nair, G.; Takeda, Y. The Heat-Stable Enterotoxins. Microb. Pathog. 1998, 24, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Dubreuil, J.D. Escherichia coli Heat-Stable Enterotoxins. In The Comprehensive Sourcebook of Bacterial Protein Toxins; Elsevier: Amsterdam, The Netherlands, 2015; pp. 874–910. ISBN 9780128005897. [Google Scholar]
- Sun, Y.; Kim, S.W. Intestinal Challenge with Enterotoxigenic Escherichia coli in Pigs, and Nutritional Intervention to Prevent Postweaning Diarrhea. Anim. Nutr. 2017, 3, 322–330. [Google Scholar] [CrossRef]
- Dubreuil, J.D. Enterotoxigenic Escherichia coli Targeting Intestinal Epithelial Tight Junctions: An Effective Way to Alter the Barrier Integrity. Microb. Pathog. 2017, 113, 129–134. [Google Scholar] [CrossRef]
- Rousset, E.; Harel, J.; Dubreuil, J.D. Sulfatide from the Pig Jejunum Brush Border Epithelial Cell Surface Is Involved in Binding of Escherichia coli Enterotoxin b. Infect. Immun. 1998, 66, 5650–5658. [Google Scholar] [CrossRef]
- Chao, K.L.; Dreyfus, L.A. Interaction of Escherichia coli Heat-Stable Enterotoxin B with Cultured Human Intestinal Epithelial Cells. Infect. Immun. 1997, 65, 3209–3217. [Google Scholar] [CrossRef]
- Beausoleil, H.-E.; Labrie, V.; Dubreuil, J.D.; Harel, J. Binding to Sulfatide and Enterotoxicity of Various Escherichia coli STb Mutants. Microbiology 2001, 147, 3141–3148. [Google Scholar] [CrossRef]
- Gonçalves, C.; Berthiaume, F.; Mourez, M.; Dubreuil, J.D. Escherichia coli STb Toxin Binding to Sulfatide and Its Inhibition by Carragenan. FEMS Microbiol. Lett. 2008, 281, 30–35. [Google Scholar] [CrossRef]
- Fujii, Y.; Kondo, Y.; Okamoto, K. Involvement of Prostaglandin E 2 Synthesis in the Intestinal Secretory Action of Escherichia coli Heat-Stable Enterotoxin II. FEMS Microbiol. Lett. 1995, 130, 259–265. [Google Scholar] [CrossRef]
- Ngendahayo Mukiza, C.; Dubreuil, J.D. Escherichia coli Heat-Stable Toxin b Impairs Intestinal Epithelial Barrier Function by Altering Tight Junction Proteins. Infect. Immun. 2013, 81, 2819–2827. [Google Scholar] [CrossRef] [PubMed]
- Dubreuil, J.D. Escherichia Coli STb Enterotoxin: A Multifaceted Molecule. In Microbial Toxins; Springer: Dordrecht, The Netherlands, 2016; pp. 1–18. ISBN 978-94-007-6725-6. [Google Scholar]
- Coddens, A.; Loos, M.; Vanrompay, D.; Remon, J.P.; Cox, E. Cranberry Extract Inhibits In Vitro Adhesion of F4 and F18+ Escherichia coli to Pig Intestinal Epithelium and Reduces In Vivo Excretion of Pigs Orally Challenged with F18+ Verotoxigenic E. coli. Vet. Microbiol. 2017, 202, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; He, Y.; Xiong, X.; Ehrlich, A.; Li, X.; Raybould, H.; Atwill, E.R.; Maga, E.A.; Jørgensen, J.; Liu, Y. Dietary Supplementation of Bacillus Subtilis Influenced Intestinal Health of Weaned Pigs Experimentally Infected with a Pathogenic E. coli. J. Anim. Sci. Biotechnol. 2019, 10, 52. [Google Scholar] [CrossRef]
- Duarte, M.E.; Tyus, J.; Kim, S.W. Synbiotic Effects of Enzyme and Probiotics on Intestinal Health and Growth of Newly Weaned Pigs Challenged with Enterotoxigenic F18+ Escherichia coli. Front. Vet. Sci. 2020, 7, 573. [Google Scholar] [CrossRef] [PubMed]
- Jang, K.B.; Moita, V.H.C.; Martinez, N.; Sokale, A.; Kim, S.W. Efficacy of Zinc Glycinate Reducing Zinc Oxide on Intestinal Health and Growth of Nursery Pigs Challenged with F18+ Escherichia coli. J. Anim. Sci. 2023, 101, skad035. [Google Scholar] [CrossRef]
- McLamb, B.L.; Gibson, A.J.; Overman, E.L.; Stahl, C.; Moeser, A.J. Early Weaning Stress in Pigs Impairs Innate Mucosal Immune Responses to Enterotoxigenic E. coli Challenge and Exacerbates Intestinal Injury and Clinical Disease. PLoS ONE 2013, 8, e59838. [Google Scholar] [CrossRef]
- Gomez de Agüero, M.; Ganal-Vonarburg, S.C.; Fuhrer, T.; Rupp, S.; Uchimura, Y.; Li, H.; Steinert, A.; Heikenwalder, M.; Hapfelmeier, S.; Sauer, U.; et al. The Maternal Microbiota Drives Early Postnatal Innate Immune Development. Science 2016, 351, 1296–1302. [Google Scholar] [CrossRef]
- Pluske, J.R.; Pethick, D.W.; Hopwood, D.E.; Hampson, D.J. Nutritional Influences on Some Major Enteric Bacterial Diseases of Pig. Nutr. Res. Rev. 2002, 15, 333–371. [Google Scholar] [CrossRef]
- Katouli, M.; Lund, A.; Wallgren, P.; Kühn, I.; Söderlind, O.; Möllby, R. Phenotypic Characterization of Intestinal Escherichia coli of Pigs during Suckling, Postweaning, and Fattening Periods. Appl. Environ. Microbiol. 1995, 61, 778–783. [Google Scholar] [CrossRef]
- Moredo, F.A.; Piñeyro, P.E.; Márquez, G.C.; Sanz, M.; Colello, R.; Etcheverría, A.; Padola, N.L.; Quiroga, M.A.; Perfumo, C.J.; Galli, L.; et al. Enterotoxigenic Escherichia coli Subclinical Infection in Pigs: Bacteriological and Genotypic Characterization and Antimicrobial Resistance Profiles. Foodborne Pathog. Dis. 2015, 12, 704–711. [Google Scholar] [CrossRef]
- Herath, M.; Hosie, S.; Bornstein, J.C.; Franks, A.E.; Hill-Yardin, E.L. The Role of the Gastrointestinal Mucus System in Intestinal Homeostasis: Implications for Neurological Disorders. Front. Cell Infect. Microbiol. 2020, 10, 248. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Khan, W. Goblet Cells and Mucins: Role in Innate Defense in Enteric Infections. Pathogens 2013, 2, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Duarte, M.E.; Kim, S.W. Dietary Inclusion of Multispecies Probiotics to Reduce the Severity of Post-Weaning Diarrhea Caused by Escherichia coli F18+ in Pigs. Anim. Nutr. 2021, 7, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Wong, B.T.; Park, S.; Kovanda, L.; He, Y.; Kim, K.; Xu, S.; Lingga, C.; Hejna, M.; Wall, E.; Sripathy, R.; et al. Dietary Supplementation of Botanical Blends Enhanced Performance and Disease Resistance of Weaned Pigs Experimentally Infected with Enterotoxigenic Escherichia coli F18. J. Anim. Sci. 2022, 100, skac353. [Google Scholar] [CrossRef]
- Li, Q.; Peng, X.; Burrough, E.R.; Sahin, O.; Gould, S.A.; Gabler, N.K.; Loving, C.L.; Dorman, K.S.; Patience, J.F. Dietary Soluble and Insoluble Fiber with or Without Enzymes Altered the Intestinal Microbiota in Weaned Pigs Challenged With Enterotoxigenic E. coli F18. Front. Microbiol. 2020, 11, 1110. [Google Scholar] [CrossRef]
- Li, Q.; Burrough, E.R.; Gabler, N.K.; Loving, C.L.; Sahin, O.; Gould, S.A.; Patience, J.F. A Soluble and Highly Fermentable Dietary Fiber with Carbohydrases Improved Gut Barrier Integrity Markers and Growth Performance in F18 ETEC Challenged Pigs. J. Anim. Sci. 2019, 97, 2139–2153. [Google Scholar] [CrossRef]
- Jinno, C.; Li, X.; Liu, Y. Dietary Supplementation of Bacillus Subtilis or Antibiotics Modified Intestinal Microbiome of Weaned Pigs under Enterotoxigenic Escherichia coli Infection. Front. Microbiol. 2022, 13, 1064328. [Google Scholar] [CrossRef]
- Liu, Y.; Song, M.; Che, T.M.; Almeida, J.A.S.; Lee, J.J.; Bravo, D.; Maddox, C.W.; Pettigrew, J.E. Dietary Plant Extracts Alleviate Diarrhea and Alter Immune Responses of Weaned Pigs Experimentally Infected with a Pathogenic Escherichia coli. J. Anim. Sci. 2013, 91, 5294–5306. [Google Scholar] [CrossRef]
- Loos, M.; Geens, M.; Schauvliege, S.; Gasthuys, F.; van der Meulen, J.; Dubreuil, J.D.; Goddeeris, B.M.; Niewold, T.; Cox, E. Role of Heat-Stable Enterotoxins in the Induction of Early Immune Responses in Piglets after Infection with Enterotoxigenic Escherichia coli. PLoS ONE 2012, 7, e41041. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.L.; Li, Q.; Burrough, E.R.; Kenne, D.; Sahin, O.; Gould, S.A.; Patience, J.F. Effects of an F18 Enterotoxigenic Escherichia coli Challenge on Growth Performance, Immunological Status, and Gastrointestinal Structure of Weaned Pigs and the Potential Protective Effect of Direct-Fed Microbial Blends. J. Anim. Sci. 2020, 98, skaa113. [Google Scholar] [CrossRef]
- Bomba, L.; Minuti, A.; Moisá, S.J.; Trevisi, E.; Eufemi, E.; Lizier, M.; Chegdani, F.; Lucchini, F.; Rzepus, M.; Prandini, A.; et al. Gut Response Induced by Weaning in Piglet Features Marked Changes in Immune and Inflammatory Response. Funct. Integr. Genom. 2014, 14, 657–671. [Google Scholar] [CrossRef]
- Chang, S.Y.; Lee, J.H.; Oh, H.J.; An, J.W.; Song, D.C.; Cho, H.A.; Park, S.H.; Jeon, K.H.; Cho, S.Y.; Kim, D.J.; et al. Effect of Different Ratios of Phytogenic Feed Additives on Growth Performance, Nutrient Digestibility, Intestinal Barrier Integrity, and Immune Response in Weaned Pigs Challenged with a Pathogenic Escherichia coli. J. Anim. Sci. 2023, 101, skad148. [Google Scholar] [CrossRef]
- He, Y.; Kim, K.; Kovanda, L.; Jinno, C.; Song, M.; Chase, J.; Li, X.; Tan, B.; Liu, Y. Bacillus Subtilis: A Potential Growth Promoter in Weaned Pigs in Comparison to Carbadox. J. Anim. Sci. 2020, 98, skaa290. [Google Scholar] [CrossRef]
- Jerez-Bogota, K.; Jensen, M.; Højberg, O.; Cormican, P.; Lawlor, P.G.; Gardiner, G.E.; Canibe, N. Antibacterial Plant Combinations Prevent Postweaning Diarrhea in Organically Raised Piglets Challenged with Enterotoxigenic Escherichia coli F18. Front. Vet. Sci. 2023, 10, 1095160. [Google Scholar] [CrossRef]
- Caprarulo, V.; Turin, L.; Hejna, M.; Reggi, S.; Dell’Anno, M.; Riccaboni, P.; Trevisi, P.; Luise, D.; Baldi, A.; Rossi, L. Protective Effect of Phytogenic plus Short and Medium-Chain Fatty Acids-Based Additives in Enterotoxigenic Escherichia coli Challenged Piglets. Vet. Res. Commun. 2023, 47, 217–231. [Google Scholar] [CrossRef]
- Smith, B.N.; Hannas, M.; Orso, C.; Martins, S.M.M.K.; Wang, M.; Donovan, S.M.; Dilger, R.N. Dietary Osteopontin-Enriched Algal Protein as Nutritional Support in Weaned Pigs Infected with F18-Fimbriated Enterotoxigenic Escherichia coli. J. Anim. Sci. 2020, 98, skaa314. [Google Scholar] [CrossRef]
- Rist, V.T.S.; Weiss, E.; Sauer, N.; Mosenthin, R.; Eklund, M. Effect of Dietary Protein Supply Originating from Soybean Meal or Casein on the Intestinal Microbiota of Piglets. Anaerobe 2014, 25, 72–79. [Google Scholar] [CrossRef]
- Marchetti, R.; Faeti, V.; Gallo, M.; Pindo, M.; Bochicchio, D.; Buttazzoni, L.; Della Casa, G. Protein Content in the Diet Influences Growth and Diarrhea in Weaning Piglets. Animals 2023, 13, 795. [Google Scholar] [CrossRef]
- Lynegaard, J.C.; Kjeldsen, N.J.; Bache, J.K.; Weber, N.R.; Hansen, C.F.; Nielsen, J.P.; Amdi, C. Low Protein Diets without Medicinal Zinc Oxide for Weaned Pigs Reduced Diarrhoea Treatments and Average Daily Gain. Animal 2021, 15, 100075. [Google Scholar] [CrossRef]
- Bhunia, A.K. Foodborne Microbial Pathogens; Springer: New York, NY, USA, 2008; ISBN 9781493973477. [Google Scholar]
- Luise, D.; Chalvon-Demersay, T.; Lambert, W.; Bosi, P.; Trevisi, P. Meta-Analysis to Evaluate the Impact of the Reduction of Dietary Crude Protein on the Gut Health of Post-Weaning Pigs. Ital. J. Anim. Sci. 2021, 20, 1386–1397. [Google Scholar] [CrossRef]
- Rocha, G.C.; Duarte, M.E.; Kim, S.W. Advances, Implications, and Limitations of Low-Crude-Protein Diets in Pig Production. Animals 2022, 12, 3478. [Google Scholar] [CrossRef] [PubMed]
- Kociova, S.; Dolezelikova, K.; Horky, P.; Skalickova, S.; Baholet, D.; Bozdechova, L.; Vaclavkova, E.; Belkova, J.; Nevrkla, P.; Skladanka, J.; et al. Zinc Phosphate-Based Nanoparticles as Alternatives to Zinc Oxide in Diet of Weaned Piglets. J. Anim. Sci. Biotechnol. 2020, 11, 59. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, H.D. Zinc Oxide for Weanling Piglets. Acta Agric. Scand. A Anim. Sci. 1995, 45, 159–167. [Google Scholar] [CrossRef]
- Wang, W.; Van Noten, N.; Degroote, J.; Romeo, A.; Vermeir, P.; Michiels, J. Effect of Zinc Oxide Sources and Dosages on Gut Microbiota and Integrity of Weaned Piglets. J. Anim. Physiol. Anim. Nutr. 2019, 103, 231–241. [Google Scholar] [CrossRef]
- Grilli, E.; Tugnoli, B.; Vitari, F.; Domeneghini, C.; Morlacchini, M.; Piva, A.; Prandini, A. Low doses of microencapsulated zinc oxide improve performance and modulate the ileum architecture, inflammatory cytokines and tight junctions expression of weaned pigs. Animal 2015, 9, 1760–1768. [Google Scholar] [CrossRef] [PubMed]
- Jang, I.; Kwon, C.; Ha, D.; Jung, D.; Kang, S.; Park, M.; Han, J.; Park, B.-C.; Lee, C. Effects of a lipid-encapsulated zinc oxide supplement on growth performance and intestinal morphology and digestive enzyme activities in weanling pigs. J. Anim. Sci. Technol. 2014, 56, 29. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Ma, N.; Qi, Z.; Han, M.; Ma, X. Coated Zinc Oxide Improves Growth Performance of Weaned Piglets via Gut Microbiota. Front. Nutr. 2022, 9, 819722. [Google Scholar] [CrossRef]
- Shen, J.; Chen, Y.; Wang, Z.; Zhou, A.; He, M.; Mao, L.; Zou, H.; Peng, Q.; Xue, B.; Wang, L.; et al. Coated zinc oxide improves intestinal immunity function and regulates microbiota composition in weaned piglets. Br. J. Nutr. 2014, 111, 2123–2134. [Google Scholar] [CrossRef]
- Kim, S.j.; Kwon, C.H.; Park, B.C.; Lee, C.Y.; Han, J.H. Effects of a lipid-encapsulated zinc oxide dietary supplement, on growth parameters and intestinal morphology in weanling pigs artificially infected with enterotoxigenic Escherichia coli. J. Anim. Sci. Technol. 2015, 57, 4. [Google Scholar] [CrossRef]
- Cromwell, G.L.; Lindemann, M.D.; Monegue, H.J.; Hall, D.D.; Orr, D.E. Tribasic Copper Chloride and Copper Sulfate as Copper Sources for Weanling Pigs. J. Anim. Sci. 1998, 76, 118–123. [Google Scholar] [CrossRef]
- Huang, Y.L.; Ashwell, M.S.; Fry, R.S.; Lloyd, K.E.; Flowers, W.L.; Spears, J.W. Effect of Dietary Copper Amount and Source on Copper Metabolism and Oxidative Stress of Weanling Pigs in Short-Term Feeding1. J. Anim. Sci. 2015, 93, 2948–2955. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Hu, L.; Liu, Y.; Yan, C.; Fang, Z.F.; Lin, Y.; Xu, S.Y.; Li, J.; Wu, C.M.; Chen, D.W.; et al. Effects of Low-Protein Diets Supplemented with Indispensable Amino Acids on Growth Performance, Intestinal Morphology and Immunological Parameters in 13 to 35 Kg Pigs. Animal 2016, 10, 1812–1820. [Google Scholar] [CrossRef] [PubMed]
- Mathews, S.; Kumar, R.; Solioz, M. Copper Reduction and Contact Killing of Bacteria by Iron Surfaces. Appl. Environ. Microbiol. 2015, 81, 6399–6403. [Google Scholar] [CrossRef] [PubMed]
- Pérez, V.G.; Waguespack, A.M.; Bidner, T.D.; Southern, L.L.; Fakler, T.M.; Ward, T.L.; Steidinger, M.; Pettigrew, J.E. Additivity of Effects from Dietary Copper and Zinc on Growth Performance and Fecal Microbiota of Pigs after Weaning. J. Anim. Sci. 2011, 89, 414–425. [Google Scholar] [CrossRef]
- Saphier, M.; Silberstein, E.; Shotland, Y.; Popov, S.; Saphier, O. Prevalence of Monovalent Copper Over Divalent in Killing Escherichia coli and Staphylococcus Aureus. Curr. Microbiol. 2018, 75, 426–430. [Google Scholar] [CrossRef]
- Popov, S.; Saphier, O.; Popov, M.; Shenker, M.; Entus, S.; Shotland, Y.; Saphier, M. Factors Enhancing the Antibacterial Effect of Monovalent Copper Ions. Curr. Microbiol. 2020, 77, 361–368. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, J.; Dong, Z.; Li, G.; Wang, J.; Li, Y.; Wan, D.; Yang, H.; Yin, Y. Effect of Dietary Copper on Intestinal Microbiota and Antimicrobial Resistance Profiles of Escherichia coli in Weaned Piglets. Front. Microbiol. 2019, 10, 2808. [Google Scholar] [CrossRef]
- Su, W.; Gong, T.; Jiang, Z.; Lu, Z.; Wang, Y. The Role of Probiotics in Alleviating Postweaning Diarrhea in Piglets from the Perspective of Intestinal Barriers. Front. Cell Infect. Microbiol. 2022, 12, 883107. [Google Scholar] [CrossRef]
- Lewton, J.R.; Woodward, A.D.; Moser, R.L.; Thelen, K.M.; Moeser, A.J.; Trottier, N.L.; Tempelman, R.J.; Rozeboom, D.W. Effects of a Multi-Strain Bacillus Subtilis-Based Direct-Fed Microbial on Immunity Markers and Intestinal Morphology in Diets Fed to Weanling Pigs. Transl. Anim. Sci. 2022, 6, txac083. [Google Scholar] [CrossRef]
- Kogan, G.; Kocher, A. Role of Yeast Cell Wall Polysaccharides in Pig Nutrition and Health Protection. Livest. Sci. 2007, 109, 161–165. [Google Scholar] [CrossRef]
- Guo, M.; Wu, F.; Hao, G.; Qi, Q.; Li, R.; Li, N.; Wei, L.; Chai, T. Bacillus Subtilis Improves Immunity and Disease Resistance in Rabbits. Front. Immunol. 2017, 8, 354. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.H.T.; Everaert, N.; Bindelle, J. Review on the Effects of Potential Prebiotics on Controlling Intestinal Enteropathogens Salmonella and Escherichia coli in Pig Production. J. Anim. Physiol. Anim. Nutr. 2018, 102, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.R.; Probert, H.M.; Van Loo, J.; Rastall, R.A.; Roberfroid, M.B. Dietary Modulation of the Human Colonic Microbiota: Updating the Concept of Prebiotics. Nutr. Res. Rev. 2004, 17, 259–275. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.; Chen, D.; Yu, B.; Luo, Y.; Zheng, P.; Yin, H.; Mao, X.; Huang, Z.; Yu, J.; Luo, J.; et al. Amelioration of Enterotoxigenic Escherichia coli-Induced Disruption of Intestinal Epithelium by Manno-Oligosaccharide in Weaned Pigs. J. Funct. Foods 2021, 82, 104492. [Google Scholar] [CrossRef]
- Choi, H.; Kim, S.W. Characterization of β-Glucans from Cereal and Microbial Sources and Their Roles in Feeds for Intestinal Health and Growth of Nursery Pigs. Animals 2023, 13, 2236. [Google Scholar] [CrossRef]
- Hopwood, D.E.; Pethick, D.W.; Pluske, J.R.; Hampson, D.J. Addition of pearl barley to a rice-based diet for newly weaned piglets increases the viscosity of the intestinal contents, reduces starch digestibility and exacerbates post-weaning colibacillosis. Br. J. Nutr. 2004, 92, 419–427. [Google Scholar] [CrossRef]
- Li, J.; Li, D.F.; Xing, J.J.; Cheng, Z.B.; Lai, C.H. Effects of β-glucan extracted from Saccharomyces cerevisiae on growth performance, and immunological and somatotropic responses of pigs challenged with Escherichia coli lipopolysaccharide1. J. Anim. Sci. 2006, 84, 2374–2381. [Google Scholar] [CrossRef]
- Shen, Y.B.; Piao, X.S.; Kim, S.W.; Wang, L.; Liu, P.; Yoon, I.; Zhen, Y.G. Effects of yeast culture supplementation on growth performance, intestinal health, and immune response of nursery pigs1. J. Anim. Sci. 2009, 87, 2614–2624. [Google Scholar] [CrossRef]
- Liang, B.; Xing, D. The Current and Future Perspectives of Postbiotics. Probiotics Antimicrob. Proteins 2023, 10, 1–18. [Google Scholar] [CrossRef]
- Vinderola, G.; Sanders, M.E.; Salminen, S. The Concept of Postbiotics. Foods 2022, 11, 1077. [Google Scholar] [CrossRef]
- Wenk, C. Herbs and Botanicals as Feed Additives in Monogastric Animals. Asian-Australas. J. Anim. Sci. 2003, 16, 282–289. [Google Scholar] [CrossRef]
- Nazzaro, F.; Fratianni, F.; De Martino, L.; Coppola, R.; De Feo, V. Effect of Essential Oils on Pathogenic Bacteria. Pharmaceuticals 2013, 6, 1451–1474. [Google Scholar] [CrossRef]
- Duarte, M.E.; Kim, S.W. Phytobiotics from Oregano Extracts Enhance the Intestinal Health and Growth Performance of Pigs. Antioxidants 2022, 11, 2066. [Google Scholar] [CrossRef] [PubMed]
- Kommera, S.K.; Mateo, R.D.; Neher, F.J.; Kim, S.W. Phytobiotics and Organic Acids as Potential Alternatives to the Use of Antibiotics in Nursery Pig Diets. Asian-Australas. J. Anim. Sci. 2006, 19, 1784–1789. [Google Scholar] [CrossRef]
- Moita, V.H.C.; Duarte, M.E.; da Silva, S.N.; Kim, S.W. Supplemental Effects of Functional Oils on the Modulation of Mucosa-Associated Microbiota, Intestinal Health, and Growth Performance of Nursery Pigs. Animals 2021, 11, 1591. [Google Scholar] [CrossRef] [PubMed]


| Interventions | Observation | Reference | |
|---|---|---|---|
| F18+ E. coli (NC vs. PC) | Treatment (PC vs. Treatment) | ||
| Zinc glycinate | Increased fecal score, enterocyte proliferation (44%), TNF-α (27%), protein carbonyl (67%), and MDA (42%) in jejunum; reduced ADG (23%). | Reduced fecal score, IL8 (39%), TNF-α (26%), MDA (31%), and protein carbonyl (45%); increased ADG (39%) | [68] |
| B. subtilis | Increased frequency of diarrhea and neutrophils (33%) in serum; reduced BW (21%), ADG (35%), ADFI (17.8%), and G:F (24%) | Reduced diarrhea, fecal β-hemolytic coliforms, and neutrophils (16%) in serum; increased BW (20%), and G:F (13%) and expression of tight junction protein in the jejunum | [66] |
| Bacillus sp. + xylanase | Reduced BW (7%), ADG (19%), and G:F (18%) and villus height (18%); increased fecal score, Proteobacteria (37%), IL6 (58%), and MDA (215%) in the jejunal mucosa. | Reduced fecal score, IL6 (27%) in the jejunal mucosa; increased BW (3%) and villus height (23%). | [67] |
| Lactic acid bacteria 1 | Increased frequency of diarrhea, TNF-α (27%), and villus height (17%). | Improved ADG (51%) and ADFI (44%); reduced TNF-α (36%). | [7] |
| Lactobacillus postbiotic | Reduced BW (12%), ADG (22%), ADFI (17%), increased IL8 (83%), and abundance of harmful bacteria. | Improved BW (14%), ADFI (20%), and increased diversity and abundance of beneficial bacteria | [7] |
| Garlic and apple pomace or garlic and blackcurrant | Reduced ADG (4%), G:F (4%), increased inflammation, diarrhea, and the abundance of ETEC and other harmful bacteria in the feces. | Improved G:F (51%), inhibited the proliferation of pathogens, and increased the abundance of beneficial bacteria. | [87] |
| Capsicum oleoresin, garlic botanical, or turmeric oleoresin | Reduced BW (15%), ADG (46%), G:F (53%), and villus height (18%); increased neutrophils (114%) and TNF-α (36%). | Reduced inflammation and fecal score; reduced neutrophils (43%), | [83] |
| Thymol and carvacrol or a blend of botanicals 2 | Reduced BW (9%), ADG (26%), ADFI (5%); increased diarrhea, TNF-α (36%), and IL6 (20%) in serum. | Increased BW (8%), ADG (49%), ADFI (5%), G:F (44%), decreased diarrhea, TNF-α (23%), and IL6 (21%) in serum. | [85] |
| Blend of botanicals + fatty acids 3 | Reduced G:F (38%) and increased fecal consistency. | Improved G:F (29%) and fecal consistency. | [88] |
| Osteopontin | Reduced BW (26%), ADG (56%), and G:F (58%); increased blood helper T-cells, total leukocyte counts, and TNF-α (29%). | Increased TNF-α (141%) and restored microbiota composition. | [89] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duarte, M.E.; Garavito-Duarte, Y.; Kim, S.W. Impacts of F18+ Escherichia coli on Intestinal Health of Nursery Pigs and Dietary Interventions. Animals 2023, 13, 2791. https://doi.org/10.3390/ani13172791
Duarte ME, Garavito-Duarte Y, Kim SW. Impacts of F18+ Escherichia coli on Intestinal Health of Nursery Pigs and Dietary Interventions. Animals. 2023; 13(17):2791. https://doi.org/10.3390/ani13172791
Chicago/Turabian StyleDuarte, Marcos Elias, Yesid Garavito-Duarte, and Sung Woo Kim. 2023. "Impacts of F18+ Escherichia coli on Intestinal Health of Nursery Pigs and Dietary Interventions" Animals 13, no. 17: 2791. https://doi.org/10.3390/ani13172791






