Adrenal Vein Sampling for Conn’s Syndrome: Diagnosis and Clinical Outcomes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedure
2.3. Imaging
2.4. Outcomes and Data Analysis
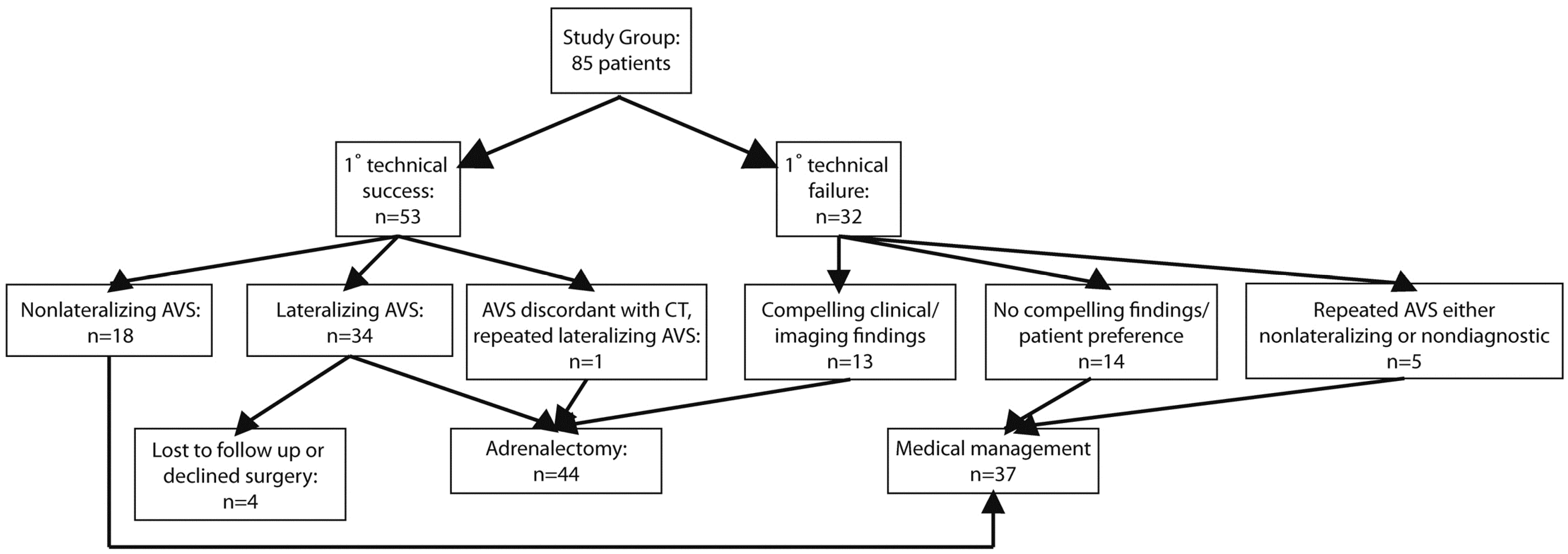
3. Results
3.1. Patient Demographics
| Demographic and Clinical Variable | Surgical | Medical | p value |
|---|---|---|---|
| Mean Age (SE) | 51.2 (1.5) | 50 (1.6) | 0.7 |
| % Male | 45% | 70% | 0.04 |
| Pre-AVS Systolic BP (SE) | 167 (4) | 150 (4) | 0.009 |
| Pre-AVS Diastolic BP (SE) | 96 (2) | 89 (3) | 0.03 |
| Pre-AVS BP meds (range) | 3 (1–6) | 2 (0–5) | 0.02 |
| % Hypokalemic | 86% | 54% | 0.003 |
| Pre-AVS Potassium (SE) | 3.3 (0.1) | 3.6 (0.1) | 0.006 |
| Pre-AVS Aldosterone:Renin Ratio (SE) | 69 (14) | 94 (19) | 0.3 |
3.2. AVS Findings and Concordance to Imaging and Pathology
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBP pre | DBP pre | SBP Post | DBP Post | Preop Meds | Postop Meds | HypoK Resolved | Adrenal Resected | Pathology |
| Lateralizing AVS, Adrenalectomy (n = 31) | |||||||||||||
| Left adrenal adenoma | 9.5 | 51.3 | 127.8 | 0.01 | 204 | 102 | - | - | 2 | - | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 32.7 | 30.8 | 58.0 | 0.02 | 170 | 90 | 150 | 92 | 4 | 0 | yes | Left | Adrenocortical adenoma |
| Left adrenal lesion too small to characterize | 108.5 | 100.2 | 54.1 | 0.02 | 174 | 108 | 120 | 70 | 4 | 3 | yes | Left | Adrenocortical adenoma |
| Normal | 19.3 | 48.8 | 28.3 | 0.04 | 144 | 90 | 118 | 68 | 4 | 1 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 52.6 | 70.8 | 27.2 | 0.04 | 130 | 80 | 107 | 73 | 6 | 0 | yes | Left | Adrenocortical adenoma |
| Normal | 38.9 | 54.9 | 26.0 | 0.04 | 130 | 80 | 118 | 78 | 2 | 0 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 12.0 | 19.7 | 22.9 | 0.04 | 170 | 98 | 140 | 60 | 2 | 1 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 23.3 | 31.1 | 22.6 | 0.04 | 154 | 96 | 102 | 78 | 5 | 1 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 18.6 | 48.7 | 13.6 | 0.1 | 158 | 108 | 120 | 70 | 2 | 0 | yes | Left | Adrenocortical adenoma |
| Left adrenal | 44.7 | 50.8 | 13.6 | 0.1 | 164 | 98 | 109 | 67 | 1 | 1 | yes | Left | Adrenocortical adenoma |
| adenoma *** | |||||||||||||
| Left adrenal adenoma | 50.6 | 39.8 | 10.1 | 0.1 | 155 | 90 | 110 | 60 | 2 | 0 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 5.8 | 5.5 | 9.4 | 0.1 | 130 | 85 | 130 | 85 | 4 | 2 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 30.5 | 8.0 | 5.0 | 0.2 | 200 | 115 | 134 | 90 | 2 | 1 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 35.4 | 22.1 | 3.9 | 0.3 | 200 | 100 | 120 | 70 | 2 | 1 | yes | Left | Adrenocortical adenoma |
| Left adrenal thickening | 6.1 | 10.6 | 33.0 | 0.0 | - | - | - | - | 5 | 2 | yes | Left | Adrenal cortical hyperplasia with mixed macro- and micronodular pattern |
| Left adrenal adenoma | 49.2 | 39.1 | 11.8 | 0.1 | 160 | 88 | 117 | 76 | 3 | 0 | yes | Left | Adrenocortical adenoma with a background of nodular cortical hyperplasia |
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBP pre | DBP pre | SBP Post | DBP Post | Preop meds | Postop meds | HypoK Resolved | Adrenal Resected | Pathology |
| Left adrenal lesion too small to characterize | 18.5 | 35.2 | 12.6 | 0.1 | 150 | 100 | 102 | 72 | 3 | 2 | yes | Left | Adrenocortical adenoma with a background of nodular cortical hyperplasia |
| Right adrenal adenoma | 9.4 | 21.9 | 0.04 | 23.6 | 188 | 90 | 140 | 100 | 3 | 3 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 16.2 | 18.8 | 0.2 | 4.5 | 168 | 88 | 140 | 100 | 3 | yes | Right | Adrenocortical adenoma | |
| Right adrenal adenoma | 42.0 | 65.6 | 0.2 | 4.7 | 166 | 90 | 138 | 68 | 5 | 2 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 9.3 | 38.7 | 0.2 | 5.1 | 160 | 98 | 148 | 88 | 2 | 1 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 22.1 | 39.2 | 0.1 | 10.3 | 200 | 110 | 130 | 82 | 4 | 2 | yes | Right | Adrenocortical adenoma |
| Normal | 39.3 | 31.7 | 0.1 | 11.6 | 180 | 110 | 118 | 80 | 2 | 2 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 17.5 | 11.7 | 0.1 | 14.3 | 150 | 90 | 130 | 80 | 5 | 4 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 85.6 | 49.7 | 0.1 | 14.7 | - | - | - | - | 2 | yes | Right | Adrenocortical adenoma | |
| Right adrenal adenoma | 16.5 | 39.7 | 0.1 | 17.9 | 226 | 141 | 140 | 84 | 2 | 0 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 8.5 | 23.3 | 0.03 | 36.3 | 162 | 85 | 122 | 76 | 4 | 1 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 50.3 | 9.1 | 0.1 | 16.5 | 170 | 90 | 134 | 80 | 1 | 1 | yes | Right | Adrenocortical adenoma with a background of nodular cortical hyperplasia |
| Right adrenal adenoma | 11.7 | 25.6 | 0.04 | 22.7 | 140 | 90 | 117 | 83 | 1 | 1 | yes | Right | Adrenocortical adenoma with a background of nodular cortical hyperplasia |
| Right adrenal adenoma | 10.7 | 10.7 | 0.1 | 14.1 | 190 | 110 | 120 | 90 | 3 | 1 | yes | Right | Adrenocortical adenoma with a background of nodular cortical hyperplasia |
| Bilateral adrenal thickening | 16.9 | 10.8 | 0.03 | 31.7 | 160 | 90 | - | - | 2 | 1 | yes | Right | Multinodular adrenal cortical hyperplasia |
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBP pre | DBP pre | SBP Post | DBP Post | Preop meds | Postop meds | HypoK Resolved | Adrenal Resected | Pathology |
| Nondiagnostic AVS, Adrenalectomy (n = 13) | |||||||||||||
| Bilateral adrenal adenomas | 4.8 | 1.2 | 2.9 | 0.3 | - | - | 136 | 90 | 3 | 1 | yes | Bilateral (subtotal right) | Bilateral nodular cortical hyperplasia |
| Left adrenal adenoma | 13.6 | 0.8 | 34.9 | 0.0 | 150 | 90 | 119 | 77 | 3 | 1 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 17.2 | 0.9 | 31.4 | 0.0 | 142 | 71 | 123 | 68 | 4 | 2 | yes | Left | Adrenocortical adenoma |
| Bilateral adrenal adenomas | 7.6 | 1.2 | 6.1 | 0.2 | - | - | 121 | 66 | 3 | 0 | yes | Left | Adrenocortical adenoma |
| Left adrenal adenoma | 33.1 | 2.6 | 12.4 | 0.1 | 177 | 117 | 100 | 70 | 3 | 0 | yes | Left | Cortical nodular hyperplasia with two dominant nodules |
| Normal | 2.3 | 1.0 | 4.4 | 0.2 | - | - | 115 | 66 | - | 4 | no | Left | Not documented |
| Left adrenal adenoma | 7.3 | 1.5 | 2.1 | 0.5 | 148 | 96 | 130 | 80 | 2 | 1 | yes | Left | Nodular hyperplasia with a dominant adrenocortical adenoma |
| Bilateral adrenal adenomas | 3.1 | 1.5 | 48.9 | 0.0 | 150 | 87 | 124 | 76 | 3 | 3 | yes | Right | Adrenal cortical hyperplasia with a dominant nodule |
| Right adrenal adenoma | 17.4 | 1.0 | 1.4 | 0.7 | 120 | 73 | 116 | 70 | 3 | 2 | - | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 7.1 | 1.5 | 0.5 | 2.1 | 154 | 92 | 155 | 105 | 2 | 0 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 43.9 | 1.0 | 0.3 | 3.7 | 240 | 120 | 122 | 86 | 2 | 1 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 23.6 | 1.2 | 0.1 | 12.8 | 240 | 120 | 138 | 68 | 5 | 2 | yes | Right | Adrenocortical adenoma |
| Right adrenal adenoma | 16.8 | 1.8 | 0.0 | 47.7 | 133 | 77 | 124 | 78 | 3 | 0 | no | Right | Adrenocortical adenoma |
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBP pre | DBP pre | SBP post | DBP post | PreAVS meds | PostAVS meds | - | ||
| Nonlateralizing Diagnostic AVS, Medically Managed (n = 21) | |||||||||||||
| Normal | 27.3 | 41.9 | 0.3 | 3.6 | 110 | 78 | 128 | 90 | 4 | 6 | - | ||
| Normal | 39.5 | 76.2 | 0.5 | 2.1 | 163 | 108 | 120 | 90 | 3 | 3 | - | ||
| Normal | 48.7 | 33.7 | 0.5 | 2.0 | 154 | 100 | 118 | 88 | 0 | 2 | - | ||
| Normal | 84.3 | 92.9 | 0.5 | 1.9 | 158 | 80 | 116 | 64 | 2 | 3 | - | ||
| Normal | 24.7 | 101.9 | 0.5 | 1.8 | 144 | 100 | 154 | 89 | 2 | 4 | - | ||
| Normal | 35.1 | 43.0 | 1.6 | 0.6 | 130 | 72 | 150 | 95 | 1 | 3 | - | ||
| Normal | 30.1 | 22.9 | 3.5 | 0.3 | 140 | 100 | 140 | 105 | 1 | 2 | - | ||
| Bilateral adrenal adenomas | 78.2 | 53.6 | 0.5 | 2.0 | 146 | 70 | 124 | 76 | 3 | 5 | - | ||
| Bilateral adrenal adenomas | 70.1 | 87.7 | 0.9 | 1.1 | 155 | 96 | 132 | 77 | 3 | 4 | - | ||
| Bilateral adrenal thickening | 11.9 | 22.0 | 0.8 | 1.3 | 150 | 80 | 148 | 75 | 1 | 4 | - | ||
| Right adrenal adenoma | 23.5 | 27.9 | 0.4 | 2.3 | 150 | 97 | 128 | 71 | 3 | 4 | - | ||
| Right adrenal adenoma | 7.0 | 7.0 | 1.0 | 1.0 | 150 | 74 | 140 | 74 | 3 | 6 | - | ||
| Right adrenal adenoma | 23.1 | 35.5 | 1.0 | 1.0 | 240 | 120 | 100 | 80 | 1 | 3 | - | ||
| Right adrenal thickening | 52.3 | 59.2 | 0.4 | 2.6 | 155 | 88 | 140 | 70 | 1 | 4 | - | ||
| Left adrenal adenoma | 37.7 | 46.4 | 0.3 | 3.4 | 160 | 90 | 2 | - | |||||
| Left adrenal adenoma | 75.2 | 74.4 | 2.0 | 0.5 | 137 | 86 | 134 | 82 | 3 | 4 | - | ||
| Left adrenal adenoma | 23.4 | 38.0 | 3.2 | 0.3 | 140 | 86 | 158 | 100 | 4 | 4 | - | ||
| Left adrenal adenoma and right adrenal thickening | 40.2 | 39.5 | 0.3 | 3.3 | 148 | 102 | 136 | 84 | 2 | 7 | - | ||
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBPpre | DBPpre | SBPpost | DBPpost | PreAVS meds | PostAVS meds | - | ||
| Left adrenal | 23.7 | 1.1 | 2.0 | 0.5 | 170 | 90 | 125 | 74 | 2 | 4 | - | ||
| adenoma *** | |||||||||||||
| Left adrenal | 8.6 | 0.9 | 0.6 | 1.6 | 171 | 117 | 142 | 91 | 3 | 4 | - | ||
| thickening *** | |||||||||||||
| Left adrenal | 1.4 | 35.1 | 6.2 | 0.2 | 158 | 94 | 140 | 76 | 2 | 4 | - | ||
| adenoma *** | |||||||||||||
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBPpre | DBPpre | SBPpost | DBPpost | PreAVS meds | PostAVS meds | Rationale for Medical Management | ||
| Lateralizing AVS, no Follow Up or Medically Managed (n = 4) | |||||||||||||
| Not documented | 28.2 | 32.0 | 9.4 | 0.1 | 154 | 88 | - | - | 0 | - | Lost to follow up | ||
| Not documented | 47.1 | 50.7 | 37.2 | 0.0 | - | - | - | - | - | - | Lost to follow up | ||
| Bilateral adrenal adenomas | 15.0 | 27.3 | 0.2 | 4.1 | 152 | 90 | 180 | 72 | 3 | 3 | Patient deferring surgery | ||
| Not documented | 17.8 | 60.9 | 10.2 | 0.1 | - | - | - | 112 | 68 | 1 | Patient deferring surgery | ||
| Nondiagnostic AVS, Medically Managed (n = 16) | |||||||||||||
| Bilateral adrenal thickening | 21.4 | 0.9 | 0.2 | 6.1 | 201 | 124 | 140 | 90 | 0 | 3 | Clinical/imaging data not compelling, AVS not repeated | ||
| Left adrenal adenoma | 87.6 | 1.5 | 0.2 | 6.4 | 158 | 103 | 130 | 71 | - | - | Clinical/imaging data not compelling, AVS not repeated | ||
| Left adrenal thickening | 31.8 | 0.9 | 1.0 | 1.0 | 134 | 70 | 150 | 88 | 2 | 4 | Clinical/imaging data not compelling, AVS not repeated | ||
| Left adrenal thickening | 1.5 | 11.2 | 5.2 | 0.2 | 118 | 83 | 110 | 78 | 2 | 2 | Clinical/imaging data not compelling, AVS not repeated | ||
| Normal | 1.4 | 2.3 | 2.8 | 0.4 | 120 | 72 | 106 | 70 | 2 | 3 | Clinical/imaging data not compelling, AVS not repeated | ||
| CT Findings | SI (L) | SI (R) | LI (L) | LI (R) | SBPpre | DBPpre | SBPpost | DBPpost | PreAVS meds | PostAVS meds | Rationale for Medical Management | ||
| Lateralizing AVS, no Follow Up or Medically Managed (n = 4) | |||||||||||||
| Normal | 35.4 | 0.9 | 2.6 | 0.4 | 144 | 96 | 135 | 85 | 2 | 2 | Clinical/imaging data not compelling, AVS not repeated | ||
| Normal | 27.2 | 1.5 | 1.1 | 0.9 | 140 | 80 | 134 | 70 | 2 | 3 | Clinical/imaging data not compelling, AVS not repeated | ||
| Normal | 53.4 | 1.0 | 1.3 | 0.7 | 120 | 80 | 140 | 78 | 4 | 4 | Clinical/imaging data not compelling, AVS not repeated | ||
| Right adrenal adenoma | 10.0 | 0.9 | 2.9 | 0.3 | 100 | 70 | 114 | 70 | 2 | 3 | Clinical/imaging data not compelling, AVS not repeated | ||
| Right adrenal adenoma | 25.6 | 1.5 | 0.6 | 1.5 | 160 | 70 | 133 | 74 | 5 | 6 | Clinical/imaging data not compelling, AVS not repeated | ||
| Right adrenal adenoma | 2.5 | 2.5 | 0.1 | 7.7 | 150 | 80 | 131 | 62 | 5 | 6 | Clinical/imaging data not compelling, AVS not repeated | ||
| Right adrenal thickening | 42.0 | 1.4 | 0.3 | 3.3 | 140 | 96 | 134 | 84 | 2 | 3 | Clinical/imaging data not compelling, AVS not repeated | ||
| Right adrenal thickening | 1.0 | 1.0 | 0.9 | 1.1 | 144 | 64 | - | - | 5 | - | Clinical/imaging data not compelling, AVS not repeated | ||
| Right adrenal adenoma | 49.2 | 1.3 | 0.1 | 10.3 | 210 | 114 | 165 | 95 | 2 | 3 | Refused repeat AVS or further workup | ||
| Right adrenal adenoma *** | 15.8 | 2.5 | 3.3 | 0.3 | 136 | 80 | 129 | 78 | 2 | 1 | Repeated AVS also failed; no compelling imaging/clinical | ||
| Normal *** | 35.0 | 2.4 | 0.2 | 5.9 | 160 | 80 | - | - | 3 | 2 | Failed AVS twice, refused further AVS | ||
3.3. Response to Therapy
| Outcome Measure | Before Surgery | After Surgery | p value |
|---|---|---|---|
| Potassium (SE) | 3.3 (0.1) | 4.1 (0.1) | p < 0.0001 |
| Systolic BP (SE) | 167 (5) | 124 (2) | p < 0.0001 |
| Diastolic BP (SE) | 97 (2) | 79 (2) | p < 0.0001 |
| # BP meds (range) | 3 (1–6) | 1 (0–4) | p < 0.0001 |
4. Discussion and Conclusion
Author Contributions
Conflicts of Interest
References
- Milliez, P.; Girerd, X.; Plouin, P.F.; Blacher, J.; Safar, M.E.; Mourad, J.J. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J. Am. Coll. Cardiol. 2005, 45, 1243–1248. [Google Scholar] [CrossRef] [PubMed]
- Mosso, L.; Carvajal, C.; Gonzalez, A.; Barraza, A.; Avila, F.; Montero, J.; Huete, A.; Gederlini, A.; Fardella, C.E. Primary aldosteronism and hype rtensive disease. Hypertension 2003, 42, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Plouin, P.F.; Amar, L.; Chatellier, G. Trends in the prevalence of primary aldosteronism, aldosterone-producing adenomas, and surgically correctable aldosterone-dependent hypertension. Nephrol. Dial. Transplant. 2004, 19, 774–777. [Google Scholar] [CrossRef] [PubMed]
- Briet, M.; Schiffrin, E.L. Vascular actions of aldosterone. J. Vasc. Res. 2012, 50, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Xanthakis, V.; Vasan, R.S. Aldosterone and the risk of hypertension. Curr. Hypertens. Rep. 2013, 15, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Vonend, O.; Ockenfels, N.; Gao, X.; Allolio, B.; Lang, K.; Mai, K.; Quack, I.; Saleh, A.; Degenhart, C.; Seufert, J. Adrenal venous sampling: Evaluation of the German Conn’s registry. Hypertension 2011, 57, 990–995. [Google Scholar] [CrossRef] [PubMed]
- Kempers, M.J.; Lenders, J.W.; van Outheusden, L.; van der Wilt, G.J.; Schultze Kool, L.J.; Hermus, A.R.; Deinum, J. Systematic review: Diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann. Intern. Med. 2009, 151, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Nwariaku, F.E.; Miller, B.S.; Auchus, R.; Holt, S.; Watumull, L.; Dolmatch, B.; Nesbitt, S.; Vongpatanasin, W.; Victor, R.; Wians, F.; et al. Primary hyperaldosteronism: Effect of adrenal vein sampling on surgical outcome. Arch. Surg. 2006, 141, 497–502. [Google Scholar] [CrossRef]
- Schwab, C.W., 2nd; Vingan, H.; Fabrizio, M.D. Usefulness of adrenal vein sampling in the evaluation of aldosteronism. J. Endourol. 2008, 22, 1247–1250. [Google Scholar] [CrossRef] [PubMed]
- Seiler, L.; Rump, L.C.; Schulte-Monting, J.; Slawik, M.; Borm, K.; Pavenstädt, H.; Beuschlein, F.; Reincke, M. Diagnosis of primary aldosteronism: Value of different screening parameters and influence of antihypertensive medication. Eur. J. Endocrinol. 2004, 150, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Vonend, O.; Stegbauer, J.; Kokulinsky, P.; Adams, S.; Liermann, D.; Hahn, K.; Rump, L.C. [Comparison of adrenal imaging and selective adrenal vein sampling in primary hyperaldosteronism]. Dtsch. Med. Wochenschr. 2007, 132, 2436–2441. [Google Scholar] [CrossRef] [PubMed]
- Young, W.F.; Stanson, A.W.; Thompson, G.B.; Grant, C.S.; Farley, D.R.; van Heerden, J.A. Role for adrenal venous sampling in primary aldosteronism. Surgery 2004, 136, 1227–1235. [Google Scholar] [CrossRef] [PubMed]
- Riester, A.; Fischer, E.; Degenhart, C.; Reiser, M.F.; Bidlingmaier, M.; Beuschlein, F.; Reincke, M.; Quinkler, M. Age below 40 or a recently proposed clinical prediction score cannot bypass adrenal venous sampling in primary aldosteronism. J. Clin. Endocrinol. Metab. 2014, 99, E1035–E1039. [Google Scholar] [CrossRef] [PubMed]
- Reznek, R.H.; Armstrong, P. The adrenal gland. Clin. Endocrinol. 1994, 40, 561–576. [Google Scholar] [CrossRef]
- Young, W.F., Jr.; Klee, G.G. Primary aldosteronism. Diagnostic evaluation. Endocrinol. Metab. Clin. North Am. 1988, 17, 367–395. [Google Scholar] [PubMed]
- Magill, S.B.; Raff, H.; Shaker, J.L.; Brickner, R.C.; Knechtges, T.E.; Kehoe, M.E.; Findling, J.W. Comparison of adrenal vein sampling and computed tomography in the differentiation of primary aldosteronism. J. Clin. Endocrinol. Metab. 2001, 86, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- Doppman, J.L.; Gill, J.R., Jr.; Miller, D.L.; Chang, R.; Gupta, R.; Friedman, T.C.; Choyke, P.L.; Feuerstein, I.M.; Dwyer, A.J.; Jicha, D.L.; et al. Distinction between hyperaldosteronism due to bilateral hyperplasia and unilateral aldosteronoma: Reliability of CT. Radiology 1992, 184, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Espiner, E.A.; Ross, D.G.; Yandle, T.G.; Richards, A.M.; Hunt, P.J. Predicting surgically remedial primary aldosteronism: Role of adrenal scanning, posture testing, and adrenal vein sampling. J. Clin. Endocrinol. Metab. 2003, 88, 3637–3644. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Sacchetto, A.; Chiesura-Corona, M.; de Toni, R.; Gallina, M.; Feltrin, G.P.; Pessina, A.C. Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: Results in 104 consecutive cases. J. Clin. Endocrinol. Metab. 2001, 86, 1083–1090. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Auchus, R.J.; Brown, M.; Lenders, J.W.; Naruse, M.; Plouin, P.F.; Satoh, F.; Young, W.F., Jr. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension 2014, 63, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Blumenfeld, J.D.; Sealey, J.E.; Schlussel, Y.; Vaughan, E.D.; Sos, T.A.; Atlas, S.A.; Muller, F.B.; Acevedo, R.; Ulick, S.; Laragh, J.H. Diagnosis and treatment of primary hyperaldosteronism. Ann. Intern. Med. 1994, 121, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Young, W.F., Jr.; Hogan, M.J.; Klee, G.G.; Grant, C.S.; van Heerden, J.A. Primary aldosteronism: Diagnosis and treatment. Mayo Clin. Proc. 1990, 65, 96–110. [Google Scholar] [CrossRef]
- Kline, G.A.; Pasieka, J.L.; Harvey, A.; So, B.; Dias, V.C. High-probability features of primary aldosteronism may obviate the need for confirmatory testing without increasing false-positive diagnoses. J. Clin. Hypertens. 2014, 16, 488–496. [Google Scholar] [CrossRef] [PubMed]
- Raman, S.P.; Lessne, M.; Kawamoto, S.; Chen, Y.; Salvatori, R.; Prescott, J.D.; Fishman, E.K. Diagnostic Performance of Multidetector Computed Tomography in Distinguishing Unilateral From Bilateral Abnormalities in Primary Hyperaldosteronism: Comparison of Multidetector Computed Tomography With Adrenal Vein Sampling. J. Comput. Assist. Tomogr. 2015, 39, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Bovio, S.; Cataldi, A.; Reimondo, G.; Sperone, P.; Novello, S.; Berruti, A.; Borasio, P.; Fava, C.; Dogliotti, L.; Scagliotti, G.V.; et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J. Endocrinol. Investig. 2006, 29, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Hedeland, H.; Ostberg, G.; Hokfelt, B. On the prevalence of adrenocortical adenomas in an autopsy material in relation to hypertension and diabetes. Acta Med. Scand. 1968, 184, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Lim, V.; Guo, Q.; Grant, C.S.; Thompson, G.B.; Richards, M.L.; Farley, D.R.; Young, W.F., Jr. Accuracy of adrenal imaging and adrenal venous sampling in predicting surgical cure of primary aldosteronism. J. Clin. Endocrinol. Metab. 2014, 99, 2712–2719. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.H.; Sze, W.C.; Reznek, R.H.; Matson, M.; Sahdev, A.; Carpenter, R.; Berney, D.M.; Akker, S.A.; Chew, S.L.; Grossman, A.B.; et al. A prospective evaluation of postural stimulation testing, computed tomography and adrenal vein sampling in the differential diagnosis of primary aldosteronism. Clin. Endocrinol. 2012, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Trerotola, S.O.; Asmar, M.; Yan, Y.; Fraker, D.L.; Cohen, D.L. Failure mode analysis in adrenal vein sampling: A single-center experience. J. Vasc. Interv. Radiol. 2014, 25, 1611–1619. [Google Scholar] [CrossRef] [PubMed]
- Melby, J.C.; Spark, R.F.; Dale, S.L.; Egdahl, R.H.; Kahn, P.C. Diagnosis and localization of aldosterone-producing adenomas by adrenal-vein cateterization. N. Engl. J. Med. 1967, 277, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Umakoshi, H.; Tanase-Nakao, K.; Wada, N.; Ichijo, T.; Sone, M.; Inagaki, N.; Katabami, T.; Kamemura, K.; Matsuda, Y.; Fujii, Y.; et al. Importance of contralateral aldosterone suppression during adrenal vein sampling in the subtype evaluation of primary aldosteronism. Clin. Endocrinol. 2015. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deipolyi, A.R.; Bailin, A.; Wicky, S.; Alansari, S.; Oklu, R. Adrenal Vein Sampling for Conn’s Syndrome: Diagnosis and Clinical Outcomes. Diagnostics 2015, 5, 254-271. https://doi.org/10.3390/diagnostics5020254
Deipolyi AR, Bailin A, Wicky S, Alansari S, Oklu R. Adrenal Vein Sampling for Conn’s Syndrome: Diagnosis and Clinical Outcomes. Diagnostics. 2015; 5(2):254-271. https://doi.org/10.3390/diagnostics5020254
Chicago/Turabian StyleDeipolyi, Amy R., Alexander Bailin, Stephan Wicky, Shehab Alansari, and Rahmi Oklu. 2015. "Adrenal Vein Sampling for Conn’s Syndrome: Diagnosis and Clinical Outcomes" Diagnostics 5, no. 2: 254-271. https://doi.org/10.3390/diagnostics5020254
APA StyleDeipolyi, A. R., Bailin, A., Wicky, S., Alansari, S., & Oklu, R. (2015). Adrenal Vein Sampling for Conn’s Syndrome: Diagnosis and Clinical Outcomes. Diagnostics, 5(2), 254-271. https://doi.org/10.3390/diagnostics5020254





