The Role of «Novel» Biomarkers of Systemic Inflammation in the Development of Early Hospital Events after Aortic Valve Replacement in Patients with Aortic Stenosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Definitions
2.4. Endpoints
2.5. Surgery
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kopylova, N.S.; Sokol’skaya, N.O.; Skopin, I.I.; Kakhktsyan, P.V.; Asatryan, T.V. Possibilities and results of the method of intraoperative transesophageal echocardiography during Ozaki procedure. Creat. Cardiol. 2022, 16, 394–403. [Google Scholar] [CrossRef]
- Lindman, B.R.; Dweck, M.R.; Lancellotti, P.; Généreux, P.; Piérard, L.A.; O’Gara, P.T.; Bonow, R.O. Management of Asymptomatic Severe Aortic Stenosis: Evolving Concepts in Timing of Valve Replacement. JACC Cardiovasc. Imaging 2020, 13 Pt 1, 481–493. [Google Scholar] [CrossRef]
- Dayawansa, N.H.; Baratchi, S.; Peter, K. Uncoupling the Vicious Cycle of Mechanical Stress and Inflammation in Calcific Aortic Valve Disease. Front. Cardiovasc. Med. 2022, 9, 783543. [Google Scholar] [CrossRef]
- Muhamed, B.; Parks, T.; Sliwa, K. Genetics of rheumatic fever and rheumatic heart disease. Nat. Rev. Cardiol. 2020, 17, 145–154. [Google Scholar] [CrossRef]
- Grimard, B.H.; Safford, R.E.; Burns, E.L. Aortic Stenosis: Diagnosis and Treatment. Am. Fam. Physician 2016, 93, 371–378. [Google Scholar]
- Ambler, G.; Omar, R.Z.; Royston, P.; Kinsman, R.; Keogh, B.E.; Taylor, K.M. Generic, simple risk stratification model for heart valve surgery. Circulation 2005, 112, 224–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, M.; Yamada, T.; Morita, T.; Furukawa, Y.; Tamaki, S.; Iwasaki, Y.; Kawasaki, M.; Kikuchi, A.; Kawai, T.; Ikeda, I.; et al. P589 Prognostic value of systemic immune-inflammation index in patients with chronic heart failure. Eur. Heart J. 2018, 39, 70. [Google Scholar] [CrossRef]
- Hayıroğlu, M.; Çınar, T.; Çinier, G.; Pay, L.; Yumurtaş, A.; Tezen, O.; Eren, S.; Kolak, Z.; Çetin, T.; Çiçek, V.; et al. Evaluating systemic immune-inflammation index in patients with implantable cardioverter defibrillator for heart failure with reduced ejection fraction. Pacing Clin. Electrophysiol. 2022, 45, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Bonaventura, A.; Montecucco, F.; Dallegri, F.; Carbone, F.; Lüscher, T.F.; Camici, G.G.; Liberale, L. Novel findings in neutrophil biology and their impact on cardiovascular disease. Cardiovasc. Res. 2019, 115, 1266–1285. [Google Scholar] [CrossRef]
- Arbănași, E.M.; Mureșan, A.V.; Coșarcă, C.M.; Kaller, R.; Bud, T.I.; Hosu, I.; Voidăzan, S.T.; Arbănași, E.M.; Russu, E. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio Impact on Predicting Outcomes in Patients with Acute Limb Ischemia. Life 2022, 12, 822. [Google Scholar] [CrossRef]
- Melinte, R.M.; Arbănași, E.M.; Blesneac, A.; Zolog, D.N.; Kaller, R.; Mureșan, A.V.; Arbănași, E.M.; Melinte, I.M.; Niculescu, R.; Russu, E. Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty. Medicina 2022, 58, 1502. [Google Scholar] [CrossRef] [PubMed]
- Kaller, R.; Arbănași, E.M.; Mureșan, A.V.; Voidăzan, S.; Arbănași, E.M.; Horváth, E.; Suciu, B.A.; Hosu, I.; Halmaciu, I.; Brinzaniuc, K.; et al. The Predictive Value of Systemic Inflammatory Markers, the Prognostic Nutritional Index, and Measured Vessels’ Diameters in Arteriovenous Fistula Maturation Failure. Life 2022, 12, 1447. [Google Scholar] [CrossRef]
- Shvartz, V.; Sokolskaya, M.; Petrosyan, A.; Ispiryan, A.; Donakanyan, S.; Bockeria, L.; Bockeria, O. Predictors of Mortality Following Aortic Valve Replacement in Aortic Stenosis Patients. Pathophysiology 2022, 29, 106–117. [Google Scholar] [CrossRef]
- Bockeria, L.A.; Bockeria, O.L.; Sanakoev, M.K.; Le, T.G.; Satyukova, A.S.; Ispiryan, A.Y.; Klimchuk, I.Y.; Fatulaev, Z.F.; Petrosyan, A.D.; Shvartz, V.A. Simultaneous surgical correction of atrial fibrillation and aortic valve replacement: Immediate results after surgery. Russ. Open Med. J. 2016, 5, 404. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Chen, Z. Higher systemic immune-inflammation index is associated with higher likelihood of peripheral arterial disease. Ann. Vasc. Surg. 2022, 84, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Xiang, J.; He, L.; Li, D.; Wei, S.; Wu, Z. Value of the systemic immune-inflammation index in predicting poor postoperative outcomes and the short-term prognosis of heart valve diseases: A retrospective cohort study. BMJ Open 2022, 12, e064171. [Google Scholar] [CrossRef]
- Urbanowicz, T.; Olasińska-Wiśniewska, A.; Gładki, M.; Jemielity, M. The Significance of Simple Inflammatory Markers in off Pump Surgery—Review. Rev. Cardiovasc. Med. 2022, 23, 400. [Google Scholar] [CrossRef]
- Russu, E.; Mureșan, A.V.; Arbănași, E.M.; Kaller, R.; Hosu, I.; Voidăzan, S.; Arbănași, E.M.; Coșarcă, C.M. The Predictive Role of NLR and PLR in Outcome and Patency of Lower Limb Revascularization in Patients with Femoropopliteal Disease. J. Clin. Med. 2022, 11, 2620. [Google Scholar] [CrossRef]
- Dey, S.; Kashav, R.; Kohli, J.K.; Magoon, R.; Shri, I.; Walian, A.; Grover, V. Systemic Immune-Inflammation Index Predicts Poor Outcome after Elective off-Pump CABG: A Retrospective, Single-Center Study. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2397–2404. [Google Scholar] [CrossRef]
- Dogdus, M.; Dindas, F.; Yenercag, M.; Yildirim, A.; Abacioglu, O.O.; Kilic, S.; Yavuz, F.; Koyun, E.; Candan, O. The Role of Systemic Immune Inflammation Index for Predicting Saphenous Vein Graft Disease in Patients with Coronary Artery Bypass Grafting. The Role of Systemic Immune Inflammation Index for Predicting Saphenous Vein Graft Disease in Patients with Coronary Artery Bypass Grafting. Angiology 2022, 74, 579–586. [Google Scholar] [CrossRef]
- Hinoue, T.; Yatabe, T.; Nishida, O. Prediction of postoperative atrial fibrillation with the systemic immune-inflammation index in patients undergoing cardiac surgery using cardiopulmonary bypass: A retrospective, single-center study. J. Artif. Organs 2022, 26, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Tosu, A.R.; Kalyoncuoglu, M.; Biter, H.I.; Cakal, S.; Selcuk, M.; Çinar, T.; Belen, E.; Can, M.M. Prognostic value of systemic immune-inflammation index for major adverse cardiac events and mortality in severe aortic stenosis patients after TAVI. Medicina 2021, 57, 588. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xing, Z.; Zhou, K.; Jiang, S. The Predictive Role of Systemic Inflammation Response Index (SIRI) in the Prognosis of Stroke Patients. Clin. Interv. Aging 2021, 16, 1997–2007. [Google Scholar] [CrossRef]
- Han, K.; Shi, D.; Yang, L.; Wang, Z.; Li, Y.; Gao, F.; Liu, Y.; Ma, X.; Zhou, Y. Prognostic value of systemic inflammatory response index in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Ann. Med. 2022, 54, 1667–1677. [Google Scholar] [CrossRef]
- Paliogiannis, P.; Ginesu, G.C.; Tanda, C.; Feo, C.F.; Fancellu, A.; Fois, A.G.; Mangoni, A.A.; Sotgia, S.; Carru, C.; Porcu, A.; et al. Inflammatory cell indexes as preoperative predictors of hospital stay in open elective thoracic surgery. ANZ J. Surg. 2018, 88, 616–620. [Google Scholar] [CrossRef] [PubMed]
- Szymanska, P.; Rozalski, M.; Wilczynski, M.; Golanski, J. Systemic immune-inflammation index (SII) and neutrophil to lymphocyte ratio (NLR) are useful markers for assessing effects of anti-inflammatory diet in patients before coronary artery bypass grafting. Rocz. Państwowego Zakładu Hig. 2021, 72, 327–335. [Google Scholar] [CrossRef]
- Şahin, A.; Sisli, E. Retrospective Evaluation of the Pre- and Postoperative Neutrophil-Lymphocyte Ratio as a Predictor of Mortality in Patients Who Underwent Coronary Artery Bypass Grafting. Heart Surg. Forum 2021, 24, E814–E820. [Google Scholar] [CrossRef]
- Sevuk, U.; Bilgic, A.; Altindag, R.; Baysal, E.; Yaylak, B.; Adiyaman, M.S.; Akkaya, S.; Ay, N.; Alp, V. Value of the neutrophil-to-lymphocyte ratio in predicting post-pericardiotomy syndrome after cardiac surgery. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 906–911. [Google Scholar]
- Urbanowicz, T.; Michalak, M.; Gąsecka, A.; Perek, B.; Rodzki, M.; Bociański, M.; Straburzyńska-Migaj, E.; Jemielity, M. Postoperative Neutrophil to Lymphocyte Ratio as an Overall Mortality Midterm Prognostic Factor following OPCAB Procedures. Clin. Pract. 2021, 11, 587–597. [Google Scholar] [CrossRef]
- Shao, Q.; Chen, K.; Rha, S.; Lim, H.; Li, G.; Liu, T. Usefulness of Neutrophil/Lymphocyte Ratio as a Predictor of Atrial Fibrillation: A Meta-analysis. Arch. Med. Res. 2015, 46, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Moschonas, I.C.; Tselepis, A.D. The pathway of neutrophil extracellular traps towards atherosclerosis and thrombosis. Atherosclerosis 2019, 288, 9–16. [Google Scholar] [CrossRef] [Green Version]
- Döring, Y.; Libby, P.; Soehnlein, O. Neutrophil Extracellular Traps Participate in Cardiovascular Diseases: Recent Experimental and Clinical Insights. Circ. Res. 2020, 126, 1228–1241. [Google Scholar] [CrossRef] [PubMed]
- Jaipersad, A.S.; Lip, G.Y.H.; Silverman, S.; Shantsila, E. The Role of Monocytes in Angiogenesis and Atherosclerosis. J. Am. Coll. Cardiol. 2014, 63, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.W.; Ivanov, S.; Williams, J.W. Monocyte Recruitment, Specification, and Function in Atherosclerosis. Cells 2020, 10, 15. [Google Scholar] [CrossRef]
- Oksuz, F.; Elcik, D.; Yarlioglues, M.; Duran, M.; Ozturk, S.; Celik, I.E.; Kurtul, A.; Kilic, A.; Murat, S.N. The relationship between lymphocyte-to-monocyte ratio and saphenous vein graft patency in patients with coronary artery bypass graft. Biomark. Med. 2017, 11, 867–876. [Google Scholar] [CrossRef] [PubMed]
- Serra, R.; Ielapi, N.; Licastro, N.; Provenzano, M.; Andreucci, M.; Bracale, U.M.; Jiritano, F.; de Franciscis, S.; Mastroroberto, P.; Serraino, G.F. Neutrophil-to-lymphocyte Ratio and Platelet-to-lymphocyte Ratio as Biomarkers for Cardiovascular Surgery Procedures: A Literature Review. Rev. Recent Clin. Trials 2021, 16, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Kurtul, A.; Ornek, E. Platelet to Lymphocyte Ratio in Cardiovascular Diseases: A Systematic Review. Angiology 2019, 70, 802–818. [Google Scholar] [CrossRef]
- Kounis, N.G.; Koniari, I.; Plotas, P.; Soufras, G.D.; Tsigkas, G.; Davlouros, P.; Hahalis, G. Inflammation, Thrombosis, and Platelet-to-Lymphocyte Ratio in Acute Coronary Syndromes. Angiology 2021, 72, 6–8. [Google Scholar] [CrossRef]
- Qiu, Z.; Jiang, Y.; Jiang, X.; Yang, R.; Wu, Y.; Xu, Y.; Cheng, X. Relationship between Platelet to Lymphocyte Ratio and Stable Coronary Artery Disease: Meta-Analysis of Observational Studies. Angiology 2020, 71, 909–915. [Google Scholar] [CrossRef]
- Camilli, M.; Iannaccone, G.; La Vecchia, G.; Cappannoli, L.; Scacciavillani, R.; Minotti, G.; Massetti, M.; Crea, F.; Aspromonte, N. Platelets: The point of interconnection among cancer, inflammation and cardiovascular diseases. Expert Rev. Hematol. 2021, 14, 537–546. [Google Scholar] [CrossRef]
- Ibrahim, H.; Schutt, R.C.; Hannawi, B.; DeLao, T.; Barker, C.M.; Kleiman, N.S. Association of immature platelets with adverse cardiovascular outcomes. J. Am. Coll. Cardiol. 2014, 64, 2122–2129. [Google Scholar] [CrossRef] [Green Version]
- Nording, H.; Baron, L.; Langer, H.F. Platelets as therapeutic targets to prevent atherosclerosis. Atherosclerosis 2020, 307, 97–108. [Google Scholar] [CrossRef]
- Xu, X.R.; Zhang, D.; Oswald, B.E.; Carrim, N.; Wang, X.; Hou, Y.; Zhang, Q.; LaValle, C.; McKeown, T.; Marshall, A.H.; et al. Platelets are versatile cells: New discoveries in hemostasis, thrombosis, immune responses, tumor metastasis and beyond. Crit. Rev. Clin. Lab. Sci. 2016, 53, 409–430. [Google Scholar] [CrossRef]
- Wang, J.; Duan, Y.; Sluijter, J.P.; Xiao, J. Lymphocytic subsets play distinct roles in heart diseases. Theranostics 2019, 9, 4030–4046. [Google Scholar] [CrossRef]
- Duran, M.; Elçik, D.; Murat, S.; Öksüz, F.; Çelik, I.E. Risk factors for coronary artery disease in young patients with stable angina pectoris. Turk. J. Med. Sci. 2019, 49, 993–998. [Google Scholar] [CrossRef] [PubMed]
- De Somer, F. Recent Advances in the Comprehension and the Management of Perioperative Systemic Host Response during Cardiopulmonary Bypass. Recent Pat. Cardiovasc. Drug Discov. 2012, 7, 180–185. [Google Scholar] [CrossRef]
- Gokalp, O.; Yesilkaya, N.K.; Bozok, S.; Besir, Y.; Iner, H.; Durmaz, H.; Gokkurt, Y.; Lafci, B.; Gokalp, G.; Yilik, L.; et al. Effects of age on systemic inflamatory response syndrome and results of coronary bypass surgery. Cardiovasc. J. Afr. 2018, 29, 22–25. [Google Scholar] [CrossRef]
- Giacinto, O.; Satriano, U.; Nenna, A.; Spadaccio, C.; Lusini, M.; Mastroianni, C.; Nappi, F.; Chello, M. Inflammatory Response and Endothelial Dysfunction Following Cardiopulmonary Bypass: Pathophysiology and Pharmacological Targets. Recent Pat. Inflamm. Allergy Drug Discov. 2019, 13, 158–173. [Google Scholar] [CrossRef] [PubMed]
- Tanrıkulu, N.; Ozbek, B. Effects of cardiopulmonary bypass on dialysisdependent patients. Cardiovasc. J. Afr. 2019, 30, 275–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolaczkowska, E.; Kubes, P. Neutrophil recruitment and function in health and inflammation. Nat. Rev. Immunol. 2013, 13, 159–175. [Google Scholar] [CrossRef]
- El-Benna, J.; Dang, P.M.; Gougerot-Pocidalo, M. Priming of the neutrophil NADPH oxidase activation: Role of p47phox phosphorylation and NOX2 mobilization to the plasma membrane. Semin. Immunopathol. 2008, 30, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Warren, O.J.; Smith, A.J.; Alexiou, C.; Rogers, P.L.; Jawad, N.; Vincent, C.; Darzi, A.W.; Athanasiou, T. The Inflammatory Response to Cardiopulmonary Bypass: Part 1—Mechanisms of Pathogenesis. J. Cardiothorac. Vasc. Anesth. 2009, 23, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Ranucci, M.; Baryshnikova, E. Inflammation and coagulation following minimally invasive extracorporeal circulation technologies. J. Thorac. Dis. 2019, 11, S1480–S1488. [Google Scholar] [CrossRef]
- Demirtas, H.; Iriz, E.; Demirtas, C.Y.; Erer, D.; Oktar, L.; Yener, A.; Arslan, M. Investigating the effects of two different pump heads (Centrifugal vs. Roller Pump) on hematological and immunological mechanisms. Niger. J. Clin. Pract. 2018, 21, 847–853. [Google Scholar] [PubMed]

| Parameters | Value (n = 363) |
|---|---|
| Age, years | 58.5 (44; 66.7) |
| Male, % | 221 (61) |
| BMI, kg/m2 | 27.8 (24.5; 30.9) |
| BSA, m2 | 0.2 (0.19; 0.21) |
| Hypertension, % | 134 (37) |
| Smoking, n (%) | 40 (11) |
| CHF NYHA class III-IV, n (%) | 134 (37) |
| Diabetes, n (%) | 25 (7) |
| COPD, n (%) | 7 (2) |
| CKD, n (%) | 14 (4) |
| Initial instrumental data | |
| LVEF, % | 63 (58; 66) |
| iEDD | 2.6 (2.3; 3.0) |
| iESD | 1.7 (1.5; 1.9) |
| iEDV | 67.9 (51.7; 89.4) |
| iESV | 23 (18; 33) |
| Peak gradient, mm Hg | 90 (56; 107) |
| Mean gradient, mm Hg | 52 (42; 67) |
| Fibrous ring of the aortic valve, mm | 24 (22; 26) |
| LA volume, mL3 | 104 (80; 133) |
| Initial laboratory data | |
| Hemoglobin, g/L | 139 (128; 148) |
| Hematocrit, % | 42 (39; 44) |
| WBC, 109/L | 7.1 (5.9; 8.4) |
| Neutrophils, 109/L | 4.4 (3.6; 5.5) |
| Neutrophils, % | 60 (53; 65) |
| Glucose, mmol/L | 5.2 (4.8; 5.6) |
| Fibrinogen, g/L | 4.0 (3.5; 4.5) |
| Creatinine, mkmol/L | 80 (70; 94) |
| eGFR mL/min | 95 (77; 114) |
| eGFR mL/min per 1.73 m2 (MDRD) | 81 (71; 97) |
| Initial drug therapy | |
| Beta-blockers, % | 41 |
| ACE inhibitors, % | 29 |
| ARA, % | 11 |
| Calcium antagonists, % | 9 |
| Statins, % | 20 |
| Nitrates, % | 3 |
| Thiazide diuretics, % | 9 |
| Loop diuretics, % | 12 |
| Potassium-sparing diuretics, % | 15 |
| Parameters | Value (n = 363) |
|---|---|
| Operative data | |
| CPB time, min | 130 (113; 153) |
| ACC time, min | 65 (58; 76) |
| ICU time > 2 days, n (%) | 42 (11.6) |
| Clinical outcomes and complications | |
| Mortality, n (%) | 7 (2) |
| AKI, n (%) | 47 (13) |
| POAF, n (%) | 36 (10) |
| Stroke/ACA, n (%) | 7 (2) |
| Bleeding, n (%) | 3 (0.8) |
| Length of stay, days | 7 (6; 8) |
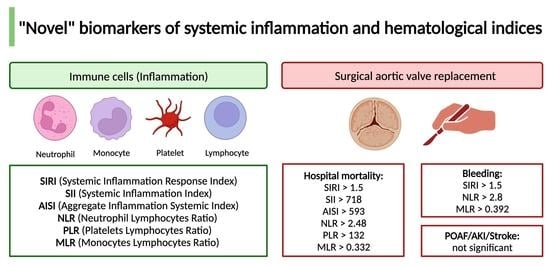
| Parameters | Cut-Off Point | AUC (CI) | Se | Sp | p |
|---|---|---|---|---|---|
| Death | |||||
| SIRI | >1.5 | 0.927 (0.891–0.954) | 100 | 77.8 | <0.001 * |
| SII | >718 | 0.800 (0.750–0.844) | 66.7 | 85.1 | 0.002 * |
| AISI | >593 | 0.857 (0.812–0.896) | 66.7 | 94.3 | <0.001 * |
| NLR | >2.48 | 0.884 (0.841–0.918) | 100 | 73.1 | <0.001 * |
| PLR | >132 | 0.763 (0.716–0.806) | 71.4 | 73.2 | 0.004 * |
| MLR | >0.332 | 0.920 (0.886–0.947) | 100 | 80.3 | <0.001 * |
| Acute kidney injury | |||||
| SIRI | >0.898 | 0.549 (0.483–0.614) | 72.7 | 46.3 | 0.073 |
| SII | >321 | 0.547 (0.481–0.611) | 87.9 | 26 | 0.379 |
| AISI | >243 | 0.568 (0.501–0.632) | 63.6 | 56.5 | 0.202 |
| NLR | >1.77 | 0.532 (0.467–0.597) | 72.7 | 41.5 | 0.535 |
| PLR | <92.6 | 0.489 (0.430–0.547) | 39.5 | 69.8 | 0.833 |
| MLR | <0.133 | 0.498 (0.437–0.558) | 13.5 | 95.4 | 0.966 |
| POAF | |||||
| SIRI | >1.2 | 0.532 (0.473–0.591) | 48.3 | 60.9 | 0.574 |
| SII | >567 | 0.534 (0.475–0.592) | 44.8 | 69.5 | 0.589 |
| AISI | >388 | 0.517 (0.457–0.575) | 31 | 80.8 | 0.784 |
| NLR | >1.9 | 0.563 (0.504–0.620) | 72.4 | 44.9 | 0.281 |
| PLR | >110 | 0.514 (0.461–0.567) | 57.9 | 54 | 0.794 |
| MLR | >0.182 | 0.513 (0.459–0.567) | 86.5 | 23.3 | 0.787 |
| Stroke or ACA | |||||
| SIRI | >1.45 | 0.600 (0.513–0.682) | 66.7 | 72.6 | 0.685 |
| SII | >553 | 0.556 (0.470–0.639) | 66.7 | 67.4 | 0.774 |
| AISI | >337 | 0.593 (0.506–0.675) | 66.7 | 70.4 | 0.668 |
| NLR | >2.43 | 0.531 (0.446–0.616) | 66.7 | 66.7 | 0.892 |
| PLR | <113 | 0.629 (0.556–0.698) | 100 | 44.9 | 0.308 |
| MLR | >0.3 | 0.521 (0.445–0.597) | 66.7 | 68.6 | 0.921 |
| Bleeding | |||||
| SIRI | >1.5 | 0.843 (0.771–0.900) | 100 | 75 | <0.001 * |
| SII | >428 | 0.500 (0.414–0.586) | 100 | 46.7 | 0.999 |
| AISI | >231 | 0.616 (0.528–0.698) | 100 | 48.5 | 0.391 |
| NLR | >2.8 | 0.766 (0.687–0.834) | 100 | 75.9 | <0.001 * |
| PLR | <112 | 0.567 (0.493–0.639) | 100 | 46.2 | 0.540 |
| MLR | >0.392 | 0.904 (0.849–0.943) | 100 | 88.9 | <0.001 * |
| Parameters | Univariate Logistic Regression Analysis OR (95% CI) | p | Multivariate Logistic Regression Analysis OR (95% CI) | p |
|---|---|---|---|---|
| SIRI | 1.143 (1.014–1.289) | 0.029 * | 2.533 (1.001–6.414) | 0.049 * |
| SII | 1.003 (1.001–1006) | 0.015 * | - | - |
| AISI | 1.000 (1.000–1.001) | 0.042 * | - | - |
| NLR | 1.110 (1.025–1.203) | 0.011 * | - | - |
| PLR | 1.001 (1.000–1.002) | 0.068 | - | - |
| MLR | 1.736 (0.980–3.073) | 0.058 | - | - |
| BMI | - | - | - | - |
| Hemoglobin, g/L | 0.957 (0.921–0.995) | 0.041 * | - | - |
| Hematocrit, % | 0.895 (0.795–1.001) | 0.091 | - | - |
| CPB time, min | 1.021 (1.007–1.037) | <0.001 * | - | - |
| ACC time, min | 1.048 (1.029–1.075) | <0.001 * | 1.046 (1.019–1.073) | <0.001 * |
| Diabetes | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shvartz, V.; Sokolskaya, M.; Ispiryan, A.; Basieva, M.; Kazanova, P.; Shvartz, E.; Talibova, S.; Petrosyan, A.; Kanametov, T.; Donakanyan, S.; et al. The Role of «Novel» Biomarkers of Systemic Inflammation in the Development of Early Hospital Events after Aortic Valve Replacement in Patients with Aortic Stenosis. Life 2023, 13, 1395. https://doi.org/10.3390/life13061395
Shvartz V, Sokolskaya M, Ispiryan A, Basieva M, Kazanova P, Shvartz E, Talibova S, Petrosyan A, Kanametov T, Donakanyan S, et al. The Role of «Novel» Biomarkers of Systemic Inflammation in the Development of Early Hospital Events after Aortic Valve Replacement in Patients with Aortic Stenosis. Life. 2023; 13(6):1395. https://doi.org/10.3390/life13061395
Chicago/Turabian StyleShvartz, Vladimir, Maria Sokolskaya, Artak Ispiryan, Madina Basieva, Polina Kazanova, Elena Shvartz, Sayali Talibova, Andrey Petrosyan, Teymuraz Kanametov, Sergey Donakanyan, and et al. 2023. "The Role of «Novel» Biomarkers of Systemic Inflammation in the Development of Early Hospital Events after Aortic Valve Replacement in Patients with Aortic Stenosis" Life 13, no. 6: 1395. https://doi.org/10.3390/life13061395