AMIC for Focal Osteochondral Defect of the Talar Shoulder
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Surgical Technique
2.4. Outcomes of Interest
2.5. Statistical Analysis
3. Results
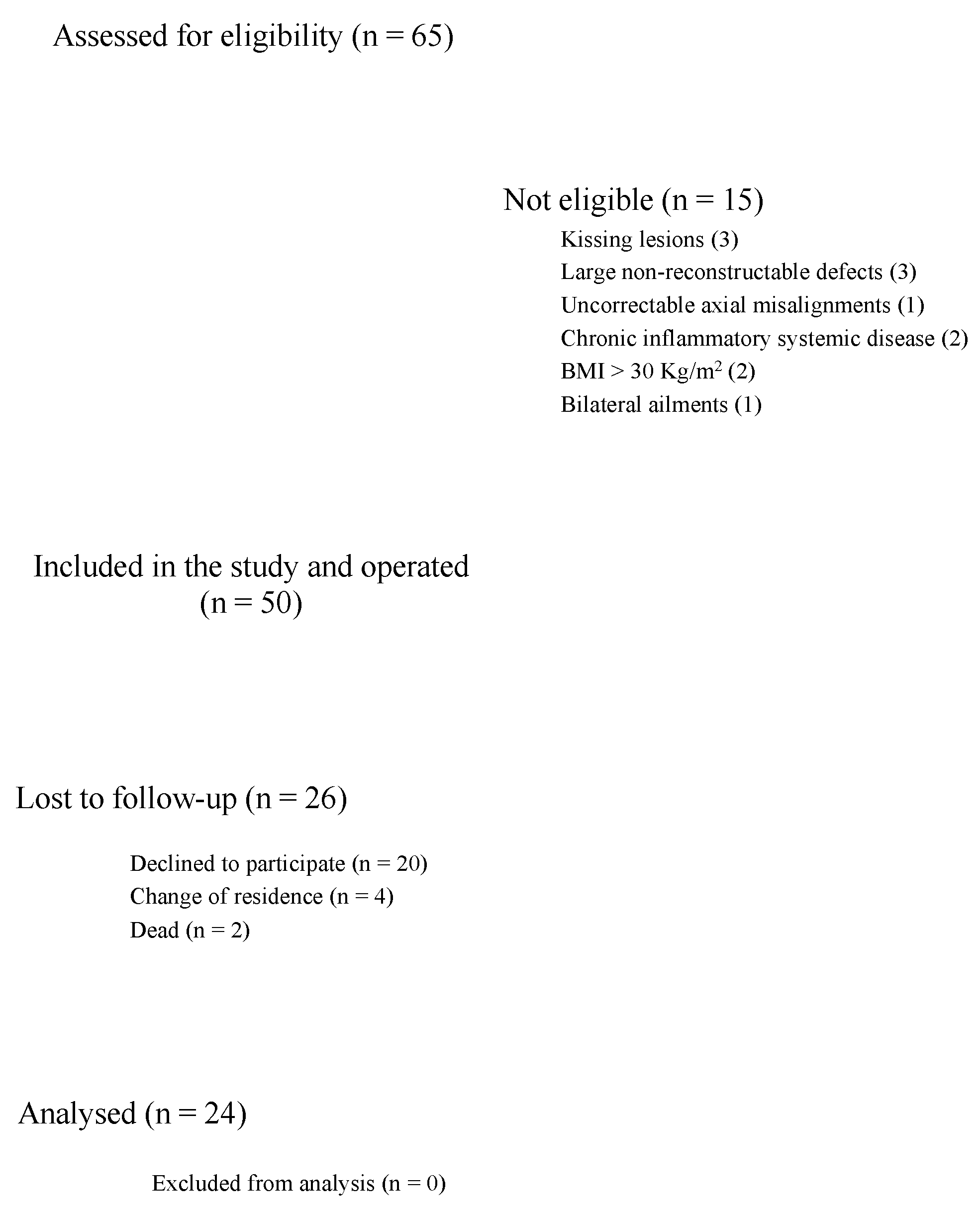
3.1. Recruitment Process
3.2. Patient Demographics
3.3. Outcomes of Interest
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Uozumi, H.; Sugita, T.; Aizawa, T.; Takahashi, A.; Ohnuma, M.; Itoi, E. Histologic findings and possible causes of osteochondritis dissecans of the knee. Am. J. Sports Med. 2009, 37, 2003–2008. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Berton, A.; Salvatore, G.; Candela, V.; Khan, W.; Longo, U.G.; Denaro, V. Autologous Chondrocyte Implantation and Mesenchymal Stem Cells for the Treatments of Chondral Defects of The Knee- A Systematic Review. Curr. Stem Cell Res. Ther. 2020, 15, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, R.A.; Struijs, P.A.; Bossuyt, P.M.; van Dijk, C.N. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003, 8, 233–242. [Google Scholar] [CrossRef]
- Abu-Shakra, M.; Buskila, D.; Shoenfeld, Y. Osteonecrosis in patients with SLE. Clin. Rev. Allergy Immunol. 2003, 25, 13–24. [Google Scholar] [CrossRef]
- Van Dijk, C.N.; Reilingh, M.L.; Zengerink, M.; van Bergen, C.J. Osteochondral defects in the ankle: Why painful? Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 570–580. [Google Scholar] [CrossRef] [Green Version]
- Korner, D.; Gueorguiev, B.; Niemeyer, P.; Bangert, Y.; Zinser, W.; Aurich, M.; Walther, M.; Becher, C.; Ateschrang, A.; Schroter, S. Parameters influencing complaints and joint function in patients with osteochondral lesions of the ankle-an investigation based on data from the German Cartilage Registry (KnorpelRegister DGOU). Arch. Orthop. Trauma Surg. 2017, 137, 367–373. [Google Scholar] [CrossRef]
- Bruns, J.; Habermann, C.R.; Petersen, J.P. Osteochondritis Dissecans of the Talus—A Critical Review. Z. Orthop. Unfall. 2016, 154, 199–216. [Google Scholar] [CrossRef]
- Vannini, F.; Costa, G.G.; Caravelli, S.; Pagliazzi, G.; Mosca, M. Treatment of osteochondral lesions of the talus in athletes: What is the evidence? Joints 2016, 4, 111–120. [Google Scholar] [CrossRef] [Green Version]
- Pettine, K.A.; Morrey, B.F. Osteochondral fractures of the talus. A long-term follow-up. J. Bone Jt. Surg. 1987, 69, 89–92. [Google Scholar] [CrossRef]
- Amendola, A.; Panarella, L. Osteochondral lesions: Medial versus lateral, persistent pain, cartilage restoration options and indications. Foot Ankle Clin. 2009, 14, 215–227. [Google Scholar] [CrossRef]
- Dahmen, J.; Lambers, K.T.A.; Reilingh, M.L.; van Bergen, C.J.A.; Stufkens, S.A.S.; Kerkhoffs, G. Reply to the letter to the editor: Comment on “No superior treatment for primary osteochondral defects of the talus”. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3984–3986. [Google Scholar] [CrossRef] [PubMed]
- Zengerink, M.; Struijs, P.A.; Tol, J.L.; van Dijk, C.N. Treatment of osteochondral lesions of the talus: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 238–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.H.; Suzer, F.; Thermann, H. Autologous Matrix-Induced Chondrogenesis in the Knee: A Review. Cartilage 2014, 5, 145–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gille, J.; Schuseil, E.; Wimmer, J.; Gellissen, J.; Schulz, A.P.; Behrens, P. Mid-term results of Autologous Matrix-Induced Chondrogenesis for treatment of focal cartilage defects in the knee. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1456–1464. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [Green Version]
- Wiewiorski, M.; Barg, A.; Valderrabano, V. Autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Foot Ankle Clin. 2013, 18, 151–158. [Google Scholar] [CrossRef]
- Marlovits, S.; Singer, P.; Zeller, P.; Mandl, I.; Haller, J.; Trattnig, S. Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: Determination of interobserver variability and correlation to clinical outcome after 2 years. Eur. J. Radiol. 2006, 57, 16–23. [Google Scholar] [CrossRef]
- Budiman-Mak, E.; Conrad, K.J.; Roach, K.E. The Foot Function Index: A measure of foot pain and disability. J. Clin. Epidemiol. 1991, 44, 561–570. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Galla, M.; Duensing, I.; Kahn, T.L.; Barg, A. Open reconstruction with autologous spongiosa grafts and matrix-induced chondrogenesis for osteochondral lesions of the talus can be performed without medial malleolar osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2789–2795. [Google Scholar] [CrossRef]
- Gottschalk, O.; Altenberger, S.; Baumbach, S.; Kriegelstein, S.; Dreyer, F.; Mehlhorn, A.; Horterer, H.; Topfer, A.; Roser, A.; Walther, M. Functional Medium-Term Results After Autologous Matrix-Induced Chondrogenesis for Osteochondral Lesions of the Talus: A 5-Year Prospective Cohort Study. J. Foot Ankle Surg. 2017, 56, 930–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valderrabano, V.; Miska, M.; Leumann, A.; Wiewiorski, M. Reconstruction of osteochondral lesions of the talus with autologous spongiosa grafts and autologous matrix-induced chondrogenesis. Am. J. Sports Med. 2013, 41, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Weigelt, L.; Hartmann, R.; Pfirrmann, C.; Espinosa, N.; Wirth, S.H. Autologous Matrix-Induced Chondrogenesis for Osteochondral Lesions of the Talus: A Clinical and Radiological 2- to 8-Year Follow-up Study. Am. J. Sports Med. 2019, 47, 1679–1686. [Google Scholar] [CrossRef] [PubMed]
- Oussedik, S.; Tsitskaris, K.; Parker, D. Treatment of articular cartilage lesions of the knee by microfracture or autologous chondrocyte implantation: A systematic review. Arthroscopy 2015, 31, 732–744. [Google Scholar] [CrossRef] [PubMed]
- VanTienderen, R.J.; Dunn, J.C.; Kusnezov, N.; Orr, J.D. Osteochondral Allograft Transfer for Treatment of Osteochondral Lesions of the Talus: A Systematic Review. Arthroscopy 2017, 33, 217–222. [Google Scholar] [CrossRef]
- Hangody, L. The mosaicplasty technique for osteochondral lesions of the talus. Foot Ankle Clin. 2003, 8, 259–273. [Google Scholar] [CrossRef]
- Imhoff, A.B.; Paul, J.; Ottinger, B.; Wortler, K.; Lammle, L.; Spang, J.; Hinterwimmer, S. Osteochondral transplantation of the talus: Long-term clinical and magnetic resonance imaging evaluation. Am. J. Sports Med. 2011, 39, 1487–1493. [Google Scholar] [CrossRef] [PubMed]
- Raikin, S.M. Fresh osteochondral allografts for large-volume cystic osteochondral defects of the talus. J. Bone Jt. Surg. Am. 2009, 91, 2818–2826. [Google Scholar] [CrossRef]
- Clar, C.; Cummins, E.; McIntyre, L.; Thomas, S.; Lamb, J.; Bain, L.; Jobanputra, P.; Waugh, N. Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: Systematic review and economic evaluation. Health Technol. Assess. 2005, 9, 1–82. [Google Scholar] [CrossRef] [Green Version]
- Usuelli, F.G.; de Girolamo, L.; Grassi, M.; D’Ambrosi, R.; Montrasio, U.A.; Boga, M. All-Arthroscopic Autologous Matrix-Induced Chondrogenesis for the Treatment of Osteochondral Lesions of the Talus. Arthrosc. Tech. 2015, 4, e255–e259. [Google Scholar] [CrossRef]
- Wiewiorski, M.; Werner, L.; Paul, J.; Anderson, A.E.; Barg, A.; Valderrabano, V. Sports Activity After Reconstruction of Osteochondral Lesions of the Talus With Autologous Spongiosa Grafts and Autologous Matrix-Induced Chondrogenesis. Am. J. Sports Med. 2016, 44, 2651–2658. [Google Scholar] [CrossRef] [PubMed]
- Barg, A.; Pagenstert, G.; Leumann, A.; Valderrabano, V. Malleolar osteotomy—Osteotomy as approach. Orthopade 2013, 42, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Perdisa, F.; Filardo, G.; Sessa, A.; Busacca, M.; Zaffagnini, S.; Marcacci, M.; Kon, E. One-Step Treatment for Patellar Cartilage Defects With a Cell-Free Osteochondral Scaffold: A Prospective Clinical and MRI Evaluation. Am. J. Sports Med. 2017, 45, 1581–1588. [Google Scholar] [CrossRef] [PubMed]
- Kon, E.; Delcogliano, M.; Filardo, G.; Pressato, D.; Busacca, M.; Grigolo, B.; Desando, G.; Marcacci, M. A novel nano-composite multi-layered biomaterial for treatment of osteochondral lesions: Technique note and an early stability pilot clinical trial. Injury 2010, 41, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Kon, E.; Delcogliano, M.; Filardo, G.; Fini, M.; Giavaresi, G.; Francioli, S.; Martin, I.; Pressato, D.; Arcangeli, E.; Quarto, R.; et al. Orderly osteochondral regeneration in a sheep model using a novel nano-composite multilayered biomaterial. J. Orthop. Res. 2010, 28, 116–124. [Google Scholar] [CrossRef]
- Filardo, G.; Kon, E.; Berruto, M.; Di Martino, A.; Patella, S.; Marcheggiani Muccioli, G.M.; Zaffagnini, S.; Marcacci, M. Arthroscopic second generation autologous chondrocytes implantation associated with bone grafting for the treatment of knee osteochondritis dissecans: Results at 6 years. Knee 2012, 19, 658–663. [Google Scholar] [CrossRef]
- Filardo, G.; Kon, E.; Andriolo, L.; Di Martino, A.; Zaffagnini, S.; Marcacci, M. Treatment of “patellofemoral” cartilage lesions with matrix-assisted autologous chondrocyte transplantation: A comparison of patellar and trochlear lesions. Am. J. Sports Med. 2014, 42, 626–634. [Google Scholar] [CrossRef]
- Behrens, P.; Ehlers, E.M.; Kochermann, K.U.; Rohwedel, J.; Russlies, M.; Plotz, W. New therapy procedure for localized cartilage defects. Encouraging results with autologous chondrocyte implantation. MMW Fortschr. Med. 1999, 141, 49–51. [Google Scholar]
- Li, X.; Ding, J.; Wang, J.; Zhuang, X.; Chen, X. Biomimetic biphasic scaffolds for osteochondral defect repair. Regen. Biomater. 2015, 2, 221–228. [Google Scholar] [CrossRef] [Green Version]
- Albano, D.; Martinelli, N.; Bianchi, A.; Messina, C.; Malerba, F.; Sconfienza, L.M. Clinical and imaging outcome of osteochondral lesions of the talus treated using autologous matrix-induced chondrogenesis technique with a biomimetic scaffold. BMC Musculoskelet. Disord. 2017, 18, 306. [Google Scholar] [CrossRef]
- Kubosch, E.J.; Erdle, B.; Izadpanah, K.; Kubosch, D.; Uhl, M.; Sudkamp, N.P.; Niemeyer, P. Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int. Orthop. 2016, 40, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.T.; Choi, Y.S.; Lee, Y.K.; Cha, S.D.; Koo, H.M. Comparison of MRI and arthroscopy in modified MOCART scoring system after autologous chondrocyte implantation for osteochondral lesion of the talus. Orthopedics 2011, 34, e356–e362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aurich, M.; Bedi, H.S.; Smith, P.J.; Rolauffs, B.; Muckley, T.; Clayton, J.; Blackney, M. Arthroscopic treatment of osteochondral lesions of the ankle with matrix-associated chondrocyte implantation: Early clinical and magnetic resonance imaging results. Am. J. Sports Med. 2011, 39, 311–319. [Google Scholar] [CrossRef]
- Trattnig, S.; Ohel, K.; Mlynarik, V.; Juras, V.; Zbyn, S.; Korner, A. Morphological and compositional monitoring of a new cell-free cartilage repair hydrogel technology—GelrinC by MR using semi-quantitative MOCART scoring and quantitative T2 index and new zonal T2 index calculation. Osteoarthr. Cartil. 2015, 23, 2224–2232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samosky, J.T.; Burstein, D.; Eric Grimson, W.; Howe, R.; Martin, S.; Gray, M.L. Spatially-localized correlation of dGEMRIC-measured GAG distribution and mechanical stiffness in the human tibial plateau. J. Orthop. Res. 2005, 23, 93–101. [Google Scholar] [CrossRef]
- Potter, H.G.; Black, B.R.; Chong le, R. New techniques in articular cartilage imaging. Clin. Sports Med. 2009, 28, 77–94. [Google Scholar] [CrossRef]
- Ukai, T.; Sato, M.; Yamashita, T.; Imai, Y.; Mitani, G.; Takagaki, T.; Serigano, K.; Mochida, J. Diffusion tensor imaging can detect the early stages of cartilage damage: A comparison study. BMC Musculoskelet. Disord. 2015, 16, 35. [Google Scholar] [CrossRef] [Green Version]
- Kretzschmar, M.; Bieri, O.; Miska, M.; Wiewiorski, M.; Hainc, N.; Valderrabano, V.; Studler, U. Characterization of the collagen component of cartilage repair tissue of the talus with quantitative MRI: Comparison of T2 relaxation time measurements with a diffusion-weighted double-echo steady-state sequence (dwDESS). Eur. Radiol. 2015, 25, 980–986. [Google Scholar] [CrossRef]
- Al-Bashaireh, A.M.; Haddad, L.G.; Weaver, M.; Kelly, D.L.; Chengguo, X.; Yoon, S. The Effect of Tobacco Smoking on Musculoskeletal Health: A Systematic Review. J. Environ. Public Health 2018, 2018, 4184190. [Google Scholar] [CrossRef]
| Endpoint | Value at Baseline |
|---|---|
| Number of procedures | 24 |
| Mean age | 46.8 ± 14.8 |
| Female gender | 50% (12/24) |
| Right side | 62.5% (15/24) |
| Mean BMI | 26.92 ± 5.7 |
| Mean defect size (mm2) | 6.95 ± 2.9 |
| Mean duration of prior symptoms (months) | 24.77 ± 32.1 |
| Mean length of follow up (months) | 25.17 ± 13.1 |
| Endpoint | Pre-OP | Post-OP | MD | p |
|---|---|---|---|---|
| MOCART | 39.29 ± 19.4 | 67.62 ± 19.7 | 28.33 | <0.0001 |
| AOFAS | 61.83 ± 15.6 | 80.58 ± 15.8 | 19.28 | <0.0001 |
| FFI | 47.8 ± 19.4 | 22.5 ± 21.6 | −25.3 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Götze, C.; Nieder, C.; Felder, H.; Migliorini, F. AMIC for Focal Osteochondral Defect of the Talar Shoulder. Life 2020, 10, 328. https://doi.org/10.3390/life10120328
Götze C, Nieder C, Felder H, Migliorini F. AMIC for Focal Osteochondral Defect of the Talar Shoulder. Life. 2020; 10(12):328. https://doi.org/10.3390/life10120328
Chicago/Turabian StyleGötze, Christian, Christian Nieder, Hanna Felder, and Filippo Migliorini. 2020. "AMIC for Focal Osteochondral Defect of the Talar Shoulder" Life 10, no. 12: 328. https://doi.org/10.3390/life10120328






