Challenging Occam’s Razor: Dual Molecular Diagnoses Explain Entangled Clinical Pictures
Abstract
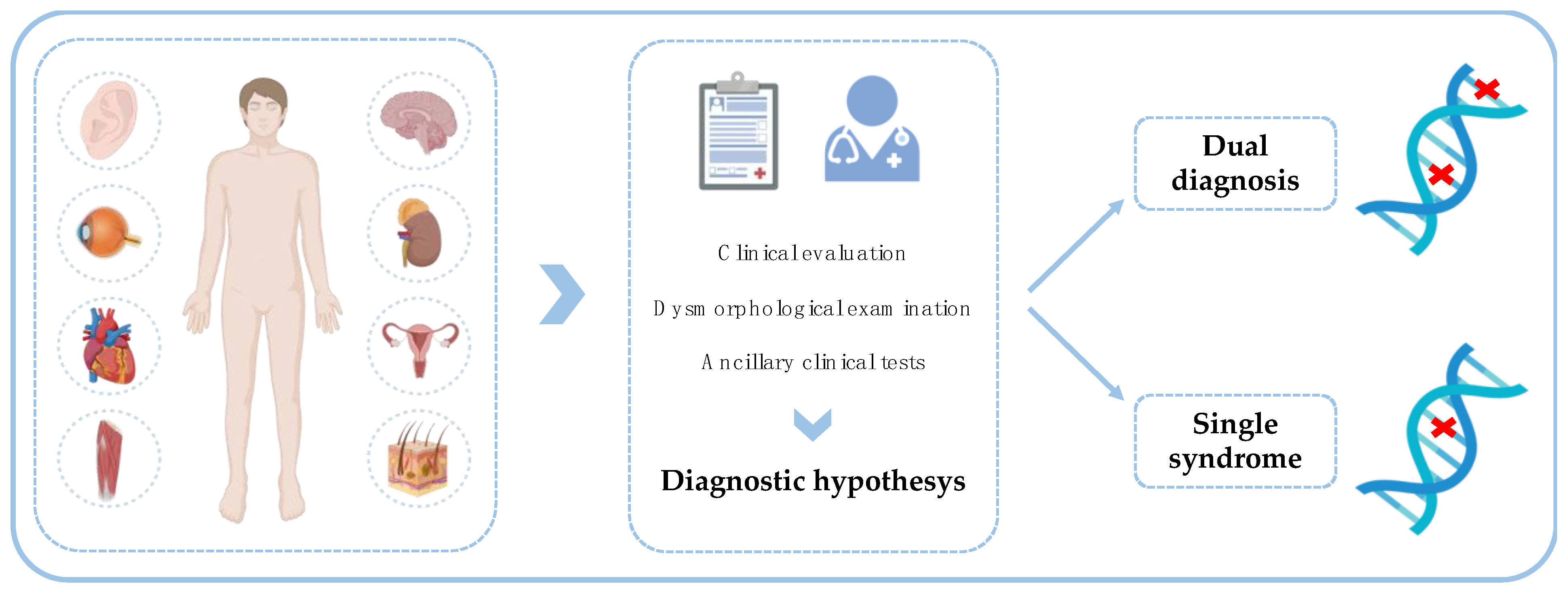
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Clinical Evaluation
2.3. DNA Extraction and Quality Control
2.4. WES and Data Analysis
2.5. Protein-Protein Interaction Analysis
3. Results
- A.
- Patients who present distinct phenotypes, due to each of the two different underlying genetic diseases. Five patients belong to this category (i.e., Patients 1, 2, 3, 4 and 5).
- B.
- Patients with overlapping clinical features that may be underpinned by both the identified genetic variations. Two patients belong to this group (i.e., Patients 6 and 7).
3.1. Patients Who Present Distinct Phenotypes Due to Two Different Underlying Genetic Diseases
3.1.1. Patient 1: Syndromic Craniosynostosis and Xerosis Cutis
3.1.2. Patient 2: Epilepsy and Congenital Heart Disease
3.1.3. Patient 3: Syndromic Intellectual Disability and Hypertrophic Cardiomyopathy
3.1.4. Patient 4: Syndromic Intellectual Disability and Congenital Heart Disease
3.1.5. Patient 5: Multiple Congenital Malformations and Autism Spectrum Disorder
3.2. Patients Who Present Overlapping Phenotypes Due to the Contribution of Two Different Loci
3.2.1. Patient 6: Drug-Resistant Epilepsy
3.2.2. Patient 7: Epileptic Encephalopathy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nguengang Wakap, S.; Lambert, D.M.; Olry, A.; Rodwell, C.; Gueydan, C.; Lanneau, V.; Murphy, D.; Le Cam, Y.; Rath, A. Estimating Cumulative Point Prevalence of Rare Diseases: Analysis of the Orphanet Database. Eur. J. Hum. Genet. 2020, 28, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Posey, J.E.; Harel, T.; Liu, P.; Rosenfeld, J.A.; James, R.A.; Coban Akdemir, Z.H.; Walkiewicz, M.; Bi, W.; Xiao, R.; Ding, Y.; et al. Resolution of Disease Phenotypes Resulting from Multilocus Genomic Variation. N. Engl. J. Med. 2016, 376, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Muzny, D.M.; Reid, J.G.; Bainbridge, M.N.; Willis, A.; Ward, P.A.; Braxton, A.; Beuten, J.; Xia, F.; Niu, Z.; et al. Clinical Whole-Exome Sequencing for the Diagnosis of Mendelian Disorders. N. Engl. J. Med. 2013, 369, 1502–1511. [Google Scholar] [CrossRef]
- Posey, J.E.; Rosenfeld, J.A.; James, R.A.; Bainbridge, M.; Niu, Z.; Wang, X.; Dhar, S.; Wiszniewski, W.; Akdemir, Z.H.C.; Gambin, T.; et al. Molecular Diagnostic Experience of Whole-Exome Sequencing in Adult Patients. Genet. Med. 2016, 18, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Matis, T.; Michaud, V.; Van-Gils, J.; Raclet, V.; Plaisant, C.; Fergelot, P.; Lasseaux, E.; Arveiler, B.; Trimouille, A. Triple Diagnosis of Wiedemann-Steiner, Waardenburg and DLG3-Related Intellectual Disability Association Found by WES: A Case Report. J. Gene Med. 2020, 22, e3197. [Google Scholar] [CrossRef] [PubMed]
- Vona, B.; Maroofian, R.; Mendiratta, G.; Croken, M.; Peng, S.; Ye, X.; Rezazadeh, J.; Bahena, P.; Lekszas, C.; Haaf, T.; et al. Dual Diagnosis of Ellis-van Creveld Syndrome and Hearing Loss in a Consanguineous Family. Mol. Syndromol. 2018, 9, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.L.; Crowley, T.B.; McGinn, D.E.; McDougall, C.; Unolt, M.; Lambert, M.P.; Emanuel, B.S.; Zackai, E.H.; McDonald-McGinn, D.M. 22q and Two: 22q11.2 Deletion Syndrome and Coexisting Conditions. Am. J. Med. Genet. Part A 2018, 176, 2203–2214. [Google Scholar] [CrossRef] [PubMed]
- Severi, G.; Bonora, E.; Perri, A.; Scarano, E.; Mazzanti, L.; Isidori, F.; Zuntini, R.; Menabò, S.; Graziano, C. HDAC8 Loss of Function and SHOX Haploinsufficiency: Two Independent Genetic Defects Responsible for a Complex Phenotype. Cytogenet. Genome Res. 2019, 157, 135–140. [Google Scholar] [CrossRef]
- Lahbib, S.; Trabelsi, M.; Dallali, H.; Sakka, R.; Bourourou, R.; Kefi, R.; Mrad, R.; Abdelhak, S.; Gaddour, N. Novel MED12 Variant in a Multiplex Fragile X Syndrome Family: Dual Molecular Etiology of Two X-Linked Intellectual Disabilities with Autism in the Same Family. Mol. Biol. Rep. 2019, 46, 4185–4193. [Google Scholar] [CrossRef]
- Priolo, M.; Mancini, C.; Pizzi, S.; Chiriatti, L.; Radio, F.C.; Cordeddu, V.; Pintomalli, L.; Mammì, C.; Dallapiccola, B.; Tartaglia, M. Complex Presentation of Hao-Fountain Syndrome Solved by Exome Sequencing Highlighting Co-Occurring Genomic Variants. Genes 2022, 13, 889. [Google Scholar] [CrossRef]
- Ye, X.; Fang, D.; He, Y.; Yan, H.; Qiu, W.; Sun, Y. Dual Diagnosis of Osteogenesis Imperfecta (OI) and Short Stature and Advanced Bone Age with or without Early-Onset Osteoarthritis and/or Osteochondritis Dissecans (SSOAOD) Reveals a Cumulative Effect on Stature Caused by Mutations in COL1A1 and ACAN Genes. Eur. J. Med. Genet. 2020, 63, 104074. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and Guidelines for the Interpretation of Sequence Variants: A Joint Consensus Recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–423. [Google Scholar] [CrossRef] [PubMed]
- Adzhubei, I.; Jordan, D.M.; Sunyaev, S.R. Predicting Functional Effect of Human Missense Mutations Using PolyPhen-2. Curr. Protoc. Hum. Genet. 2013, 76, 7.20.1–7.20.41. [Google Scholar] [CrossRef] [PubMed]
- Ng, P.C.; Henikoff, S. SIFT: Predicting Amino Acid Changes That Affect Protein Function. Nucleic Acids Res. 2003, 31, 3812–3814. [Google Scholar] [CrossRef]
- Limongelli, I.; Marini, S.; Bellazzi, R. PaPI: Pseudo Amino Acid Composition to Score Human Protein-Coding Variants. BMC Bioinform. 2015, 16, 123. [Google Scholar] [CrossRef]
- Quang, D.; Chen, Y.; Xie, X. DANN: A Deep Learning Approach for Annotating the Pathogenicity of Genetic Variants. Bioinformatics 2015, 31, 761–763. [Google Scholar] [CrossRef]
- Jian, X.; Boerwinkle, E.; Liu, X. In Silico Prediction of Splice-Altering Single Nucleotide Variants in the Human Genome. Nucleic Acids Res. 2014, 42, 13534–13544. [Google Scholar] [CrossRef]
- Steinberger, D.; Vriend, G.; Mulliken, J.B.; Müller, U. The Mutations in FGFR2-Associated Craniosynostoses Are Clustered in Five Structural Elements of Immunoglobulin-like Domain III of the Receptor. Hum. Genet. 1998, 102, 145–150. [Google Scholar] [CrossRef]
- Sandilands, A.; Terron-Kwiatkowski, A.; Hull, P.R.; O’Regan, G.M.; Clayton, T.H.; Watson, R.M.; Carrick, T.; Evans, A.T.; Liao, H.; Zhao, Y.; et al. Comprehensive Analysis of the Gene Encoding Filaggrin Uncovers Prevalent and Rare Mutations in Ichthyosis Vulgaris and Atopic Eczema. Nat. Genet. 2007, 39, 650–654. [Google Scholar] [CrossRef]
- van Leersum, F.S.; Nagtzaam, I.F.; van Oosterhoud, C.N.; Ghesquiere, S.A.I.; Brandts, R.R.H.F.J.; Gostyński, A.; Steijlen, P.M.; van Geel, M. Improving the Diagnostic Yield for Filaggrin: Concealed Mutations in the Dutch Population. J. Allergy Clin. Immunol. 2020, 145, 1704–1706.e2. [Google Scholar] [CrossRef]
- Turkyilmaz, A.; Sager, G. A Novel ELP2 Compound Heterozygous Mutation in a Boy with Severe Intellectual Disability, Spastic Diplegia, Stereotypic Behavior and Review of the Current Literature. Mol. Syndromol. 2020, 11, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Olivotto, I.; Girolami, F.; Ackerman, M.J.; Nistri, S.; Bos, J.M.; Zachara, E.; Ommen, S.R.; Theis, J.L.; Vaubel, R.A.; Re, F.; et al. Myofilament Protein Gene Mutation Screening and Outcome of Patients with Hypertrophic Cardiomyopathy. Mayo Clin. Proc. 2008, 83, 630–638. [Google Scholar] [CrossRef]
- van Lint, F.H.M.; Murray, B.; Tichnell, C.; Zwart, R.; Amat, N.; Lekanne Deprez, R.H.; Dittmann, S.; Stallmeyer, B.; Calkins, H.; van der Smagt, J.J.; et al. Arrhythmogenic Right Ventricular Cardiomyopathy-Associated Desmosomal Variants Are Rarely De Novo. Circ. Genomic Precis. Med. 2019, 12, e002467. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.Y.; Gonzaga-Jauregui, C.; Bhoj, E.J.; Strauss, K.A.; Brigatti, K.; Puffenberger, E.; Li, D.; Xie, L.; Das, N.; Skubas, I.; et al. Monoallelic BMP2 Variants Predicted to Result in Haploinsufficiency Cause Craniofacial, Skeletal, and Cardiac Features Overlapping Those of 20p12 Deletions. Am. J. Hum. Genet. 2017, 101, 985–994. [Google Scholar] [CrossRef]
- Al-Mubarak, B.; Abouelhoda, M.; Omar, A.; AlDhalaan, H.; Aldosari, M.; Nester, M.; Alshamrani, H.A.; El-Kalioby, M.; Goljan, E.; Albar, R.; et al. Whole Exome Sequencing Reveals Inherited and de Novo Variants in Autism Spectrum Disorder: A Trio Study from Saudi Families. Sci. Rep. 2017, 7, 5679. [Google Scholar] [CrossRef]
- Martin, H.C.; Gardner, E.J.; Samocha, K.E.; Kaplanis, J.; Akawi, N.; Sifrim, A.; Eberhardt, R.Y.; Tavares, A.L.T.; Neville, M.D.C.; Niemi, M.E.K.; et al. The Contribution of X-Linked Coding Variation to Severe Developmental Disorders. Nat. Commun. 2021, 12, 627. [Google Scholar] [CrossRef]
- Tian, X.J.; Zhang, Y.H.; Liu, A.J.; Yang, X.L.; Zeng, Q.; Yang, Z.X.; Ye, J.T.; Liu, X.Y.; Jiang, Y.W.; Wu, X.R. Clinical and neuroimaging features of acute encephalopathy after status epilepticus in Dravet syndrome. Zhonghua Er Ke Za Zhi Chin. J. Pediatr. 2017, 55, 277–282. [Google Scholar] [CrossRef]
- Orsini, A.; Santangelo, A.; Bravin, F.; Bonuccelli, A.; Peroni, D.; Battini, R.; Foiadelli, T.; Bertini, V.; Valetto, A.; Iacomino, M.; et al. Expanding Phenotype of Poirier-Bienvenu Syndrome: New Evidence from an Italian Multicentrical Cohort of Patients. Genes 2022, 13, 276. [Google Scholar] [CrossRef]
- Klee, E.W.; Cousin, M.A.; Pinto e Vairo, F.; Morales-Rosado, J.A.; Macke, E.L.; Jenkinson, W.G.; Ferrer, A.; Schultz-Rogers, L.E.; Olson, R.J.; Oliver, G.R.; et al. Impact of Integrated Translational Research on Clinical Exome Sequencing. Genet. Med. 2021, 23, 498–507. [Google Scholar] [CrossRef]
- Ishihara, N.; Yamada, K.; Yamada, Y.; Miura, K.; Kato, J.; Kuwabara, N.; Hara, Y.; Kobayashi, Y.; Hoshino, K.; Nomura, Y.; et al. Clinical and Molecular Analysis of Mowat-Wilson Syndrome Associated with ZFHX1B Mutations and Deletions at 2q22–Q24.1. J. Med. Genet. 2004, 41, 387–393. [Google Scholar] [CrossRef][Green Version]
- Lindy, A.S.; Stosser, M.B.; Butler, E.; Downtain-Pickersgill, C.; Shanmugham, A.; Retterer, K.; Brandt, T.; Richard, G.; McKnight, D.A. Diagnostic Outcomes for Genetic Testing of 70 Genes in 8565 Patients with Epilepsy and Neurodevelopmental Disorders. Epilepsia 2018, 59, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Fung, J.L.F.; Yu, M.H.C.; Huang, S.; Chung, C.C.Y.; Chan, M.C.Y.; Pajusalu, S.; Mak, C.C.Y.; Hui, V.C.C.; Tsang, M.H.Y.; Yeung, K.S.; et al. A Three-Year Follow-up Study Evaluating Clinical Utility of Exome Sequencing and Diagnostic Potential of Reanalysis. NPJ Genom. Med. 2020, 5, 37. [Google Scholar] [CrossRef] [PubMed]
- Karaca, E.; Posey, J.E.; Coban Akdemir, Z.; Pehlivan, D.; Harel, T.; Jhangiani, S.N.; Bayram, Y.; Song, X.; Bahrambeigi, V.; Yuregir, O.O.; et al. Phenotypic Expansion Illuminates Multilocus Pathogenic Variation. Genet. Med. 2018, 20, 1528–1537. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.X.; Buckingham, K.J.; Jhangiani, S.N.; Boehm, C.; Sobreira, N.; Smith, J.D.; Harrell, T.M.; McMillin, M.J.; Wiszniewski, W.; Gambin, T.; et al. The Genetic Basis of Mendelian Phenotypes: Discoveries, Challenges, and Opportunities. Am. J. Hum. Genet. 2015, 97, 199–215. [Google Scholar] [CrossRef]
- Shashi, V.; Pena, L.D.M.; Kim, K.; Burton, B.; Hempel, M.; Schoch, K.; Walkiewicz, M.; McLaughlin, H.M.; Cho, M.; Stong, N.; et al. De Novo Truncating Variants in ASXL2 Are Associated with a Unique and Recognizable Clinical Phenotype. Am. J. Hum. Genet. 2016, 99, 991–999. [Google Scholar] [CrossRef]
- Smith, E.D.; Blanco, K.; Sajan, S.A.; Hunter, J.M.; Shinde, D.N.; Wayburn, B.; Rossi, M.; Huang, J.; Stevens, C.A.; Muss, C.; et al. A Retrospective Review of Multiple Findings in Diagnostic Exome Sequencing: HalF.A.Re Distinct and HalF.A.Re Overlapping Diagnoses. Genet. Med. 2019, 21, 2199–2207. [Google Scholar] [CrossRef]
- Jehee, F.S.; de Oliveira, V.T.; Gurgel-Giannetti, J.; Pietra, R.X.; Rubatino, F.V.M.; Carobin, N.V.; Vianna, G.S.; de Freitas, M.L.; Fernandes, K.S.; Ribeiro, B.S.V.; et al. Dual Molecular Diagnosis Contributes to Atypical Prader–Willi Phenotype in Monozygotic Twins. Am. J. Med. Genet. Part A 2017, 173, 2451–2455. [Google Scholar] [CrossRef]
- Saettini, F.; L’Imperio, V.; Fazio, G.; Cazzaniga, G.; Mazza, C.; Moroni, I.; Badolato, R.; Biondi, A.; Corti, P. More than an ‘Atypical’ Phenotype: Dual Molecular Diagnosis of Autoimmune Lymphoproliferative Syndrome and Becker Muscular Dystrophy. Br. J. Haematol. 2020, 191, 291–294. [Google Scholar] [CrossRef]
- Xu, S.; Lian, Q.; Wu, J.; Li, L.; Song, J. Dual Molecular Diagnosis of Tricho-Rhino-Phalangeal Syndrome Type I and Okur-Chung Neurodevelopmental Syndrome in One Chinese Patient: A Case Report. BMC Med. Genet. 2020, 21, 158. [Google Scholar] [CrossRef]
- Kelly, J. The Diagnostic Approach in Complex Patients: Parsimony or Plenitude? Am. J. Med. 2021, 134, 11–12. [Google Scholar] [CrossRef]
- Wang, J.; Lin, Z.-J.; Liu, L.; Xu, H.-Q.; Shi, Y.-W.; Yi, Y.-H.; He, N.; Liao, W.-P. Epilepsy-Associated Genes. Seizure 2017, 44, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Mina, E.D.; Ciccone, R.; Brustia, F.; Bayindir, B.; Limongelli, I.; Vetro, A.; Iascone, M.; Pezzoli, L.; Bellazzi, R.; Perotti, G.; et al. Improving Molecular Diagnosis in Epilepsy by a Dedicated High-Throughput Sequencing Platform. Eur. J. Hum. Genet. 2015, 23, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Krenn, M.; Wagner, M.; Hotzy, C.; Graf, E.; Weber, S.; Brunet, T.; Lorenz-Depiereux, B.; Kasprian, G.; Aull-Watschinger, S.; Pataraia, E.; et al. Diagnostic Exome Sequencing in Non-Acquired Focal Epilepsies Highlights a Major Role of GATOR1 Complex Genes. J. Med. Genet. 2020, 57, 624–633. [Google Scholar] [CrossRef] [PubMed]
- Jakovcevski, M.; Ruan, H.; Shen, E.Y.; Dincer, A.; Javidfar, B.; Ma, Q.; Peter, C.J.; Cheung, I.; Mitchell, A.C.; Jiang, Y.; et al. Neuronal Kmt2a/Mll1 Histone Methyltransferase Is Essential for Prefrontal Synaptic Plasticity and Working Memory. J. Neurosci. Off. J. Soc. Neurosci. 2015, 35, 5097–5108. [Google Scholar] [CrossRef]
- Li, J.; Zhang, W.; Yang, H.; Howrigan, D.P.; Wilkinson, B.; Souaiaia, T.; Evgrafov, O.V.; Genovese, G.; Clementel, V.A.; Tudor, J.C.; et al. Spatiotemporal Profile of Postsynaptic Interactomes Integrates Components of Complex Brain Disorders. Nat. Neurosci. 2017, 20, 1150–1161. [Google Scholar] [CrossRef]
- Hodges, S.L.; Lugo, J.N. Wnt/β-Catenin Signaling as a Potential Target for Novel Epilepsy Therapies. Epilepsy Res. 2018, 146, 9–16. [Google Scholar] [CrossRef]
- Lupski, J.R.; Belmont, J.W.; Boerwinkle, E.; Gibbs, R.A. Clan Genomics and the Complex Architecture of Human Disease. Cell 2011, 147, 32–43. [Google Scholar] [CrossRef]


| Patient | Clinical Features | Molecular Diagnosis | Gene | cDNA Change | Protein Change | Genotype | Inheritance | ACMG/AMP Classification | References |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Syndromic craniosynostosis and Xerosis cutis | First | FGFR2 (NM_000141.4) | c.940G>T | p.(Ala314Ser) | Heterozygous | de novo | Likely pathogenic | PMID: 9521581 |
| Second | FLG (NM_002016.1) | c.7339C>T c.3191G>A | p.(Arg2447*) p.(Trp1064*) | Compound heterozygous | Paternal Maternal | Pathogenic Uncertain significance | PMID: 17417636 PMID: 32018027 | ||
| 2 | Drug-resistant epilepsy and Congenital heart defect | First | SCN1A (NM_001165963.1) | c.2591_2593 delTGC | p.(Leu864del) | Heterozygous | de novo | Pathogenic | NA |
| Second | MMP21 (NM_147191.1) | c.903G>A | p.(Met301Ile) | Homozygous | Paternal and Maternal | Uncertain significance | NA | ||
| 3 | Intellectual disability and Hypertrophic cardiomyopathy | First | ELP2 (NM_001242875.1) | c.1580G>A | p.(Arg527Gln) | Homozygous | Paternal and Maternal | Likely pathogenic | PMID: 33510603 |
| Second | MYBPC3 (NM_000256.3) | c.913_914 delTT | p.(Phe305Pro fs*27) | Heterozygous | Paternal | Pathogenic | PMID: 18533079 | ||
| 4 | Syndromic intellectual disability | First | ZMIZI (NM_020338.3) | c.1984A>G | p.(Asn662Asp) | Heterozygous | Maternal | Uncertain significance | NA |
| Second | DSG2 (NM_001943.3) | c.621_626 delTCCTCC | p.(Tyr207_Pro209 delinsTer) | Heterozygous | Maternal | Pathogenic | NA | ||
| 5 | Multiple malformations and Autism spectrum disorder | First | BMP2 (NM_001200.2) | c.460C>T | p.(Arg154*) | Heterozygous | Paternal mosaicism | Pathogenic | PMID: 29198724 |
| Second | INTS6L (NM_182540.4) | c.2552_2554 delACA | p.(Asn851del) | Hemizygous | Maternal | Uncertain significance | NA | ||
| 6 | Drug resistantepilepsy | First | SCN1A (NM_001202435.1) | c.695-1G>A | NA | Heterozygous | de novo | Pathogenic | PMID: 28441824 |
| Second | CSNK2B (NM_001320.5) | c.384_394del AGGTGAAGCCA | p.(Pro128fs) | Heterozygous | de novo | Pathogenic | PMID: 35205321 | ||
| 7 | Epileptic encephalopathy | First | CACNB4 (NM_000726.5) | c.1418G>A | p.(Arg473His) | Heterozygous | NA | Uncertain significance | PMID: 33144682 |
| Second | ZEB2 (NM_014795.4) | c.905G>A | p.(Arg302Gln) | Heterozygous | NA | Likely pathogenic | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spedicati, B.; Morgan, A.; Pianigiani, G.; Musante, L.; Rubinato, E.; Santin, A.; Nardone, G.G.; Faletra, F.; Girotto, G. Challenging Occam’s Razor: Dual Molecular Diagnoses Explain Entangled Clinical Pictures. Genes 2022, 13, 2023. https://doi.org/10.3390/genes13112023
Spedicati B, Morgan A, Pianigiani G, Musante L, Rubinato E, Santin A, Nardone GG, Faletra F, Girotto G. Challenging Occam’s Razor: Dual Molecular Diagnoses Explain Entangled Clinical Pictures. Genes. 2022; 13(11):2023. https://doi.org/10.3390/genes13112023
Chicago/Turabian StyleSpedicati, Beatrice, Anna Morgan, Giulia Pianigiani, Luciana Musante, Elisa Rubinato, Aurora Santin, Giuseppe Giovanni Nardone, Flavio Faletra, and Giorgia Girotto. 2022. "Challenging Occam’s Razor: Dual Molecular Diagnoses Explain Entangled Clinical Pictures" Genes 13, no. 11: 2023. https://doi.org/10.3390/genes13112023
APA StyleSpedicati, B., Morgan, A., Pianigiani, G., Musante, L., Rubinato, E., Santin, A., Nardone, G. G., Faletra, F., & Girotto, G. (2022). Challenging Occam’s Razor: Dual Molecular Diagnoses Explain Entangled Clinical Pictures. Genes, 13(11), 2023. https://doi.org/10.3390/genes13112023









