Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles
Abstract
:1. Introduction
2. Antimicrobial Hydrogels from Natural and Synthetic Polymers
2.1. Antimicrobial Hydrogels from Natural Polymers
2.2. Antimicrobial Hydrogels from Synthetic Polymers
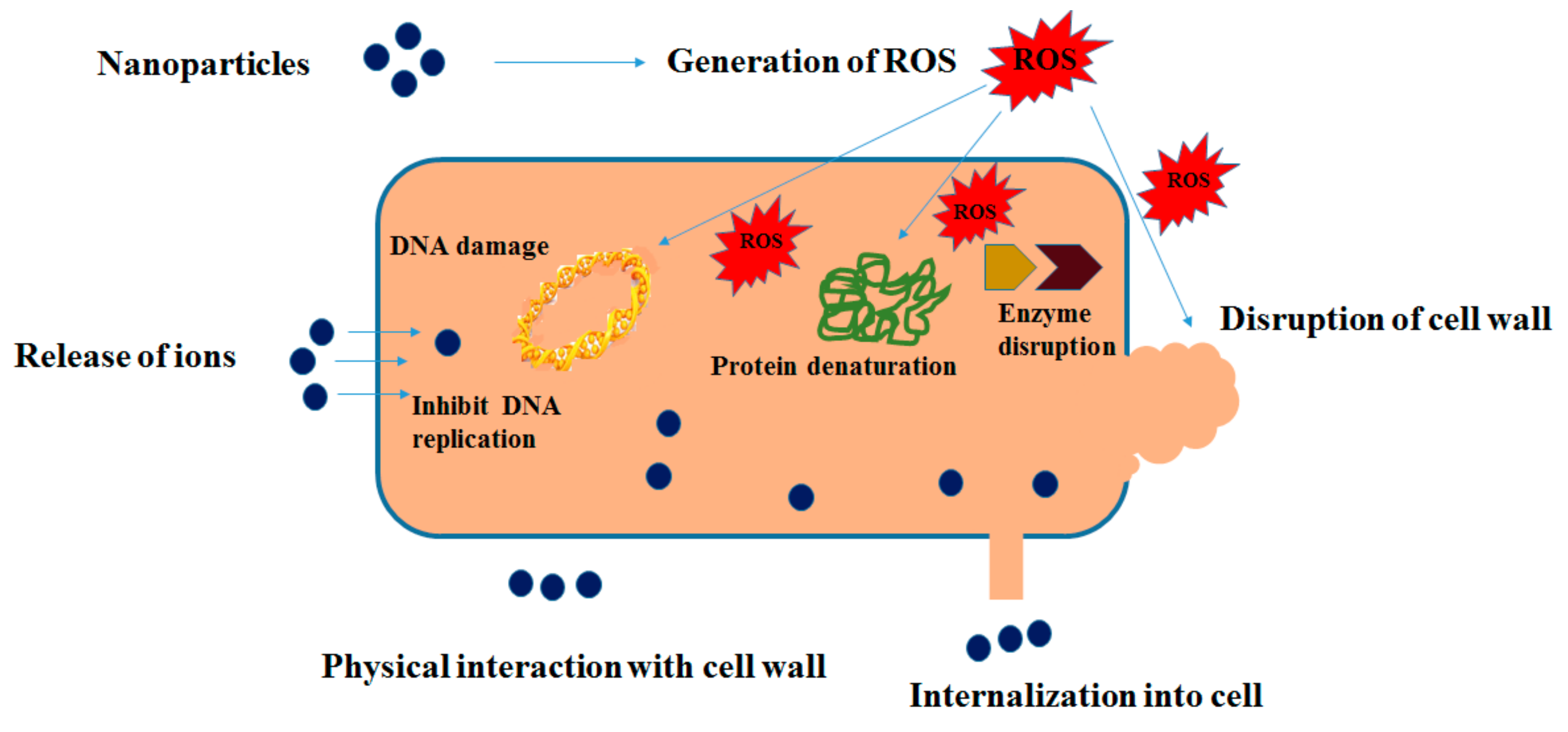
3. Antimicrobial Activity of Metals and Metal Oxide Nanoparticles
4. Designing of Nanocomposite Hydrogels
4.1. Formation of Hydrogel in Nanoparticle Suspension
4.2. Incorporation of Nanoparticles into Pre-Formed Hydrogel
4.3. Formation of Reactive Nanoparticles within a Pre-Formed Hydrogel
4.4. Cross-Linking of Hydrogel Using Nanoparticles
4.5. Hydrogel Formation Using Nanoparticles, Polymers and Cross-Linking Agents
5. Antimicrobial Hydrogels Containing Metal Ions
6. Antimicrobial Hydrogels Containing Metal Nanoparticles
6.1. Antimicrobial Hydrogels Containing Silver Nanoparticles
6.2. Antimicrobial Hydrogels Containing Other Metal Nanoparticles
7. Antimicrobial Hydrogels Containing Metal Oxide Nanoparticles
7.1. Antimicrobial Hydrogels Containing ZnO Nanoparticles
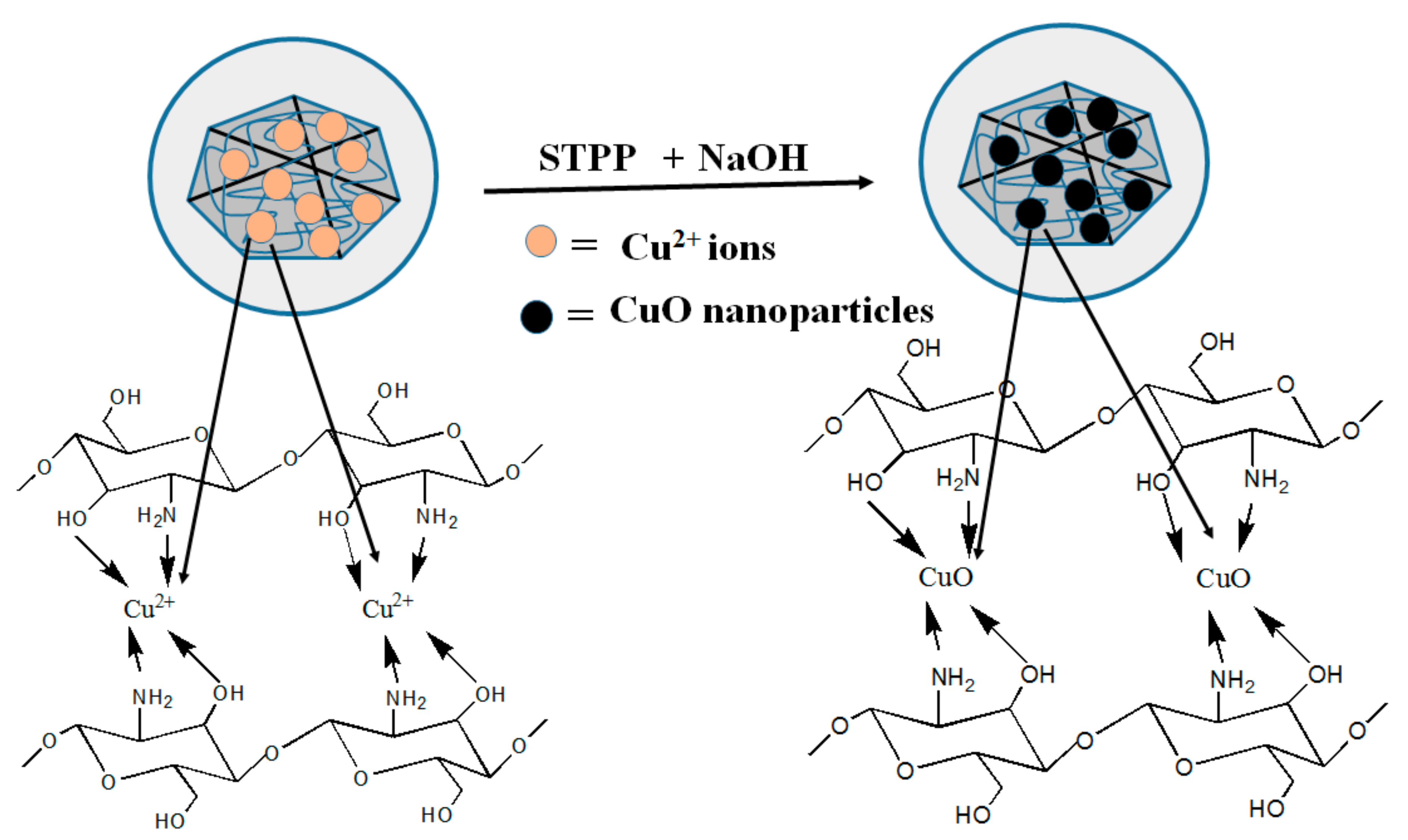
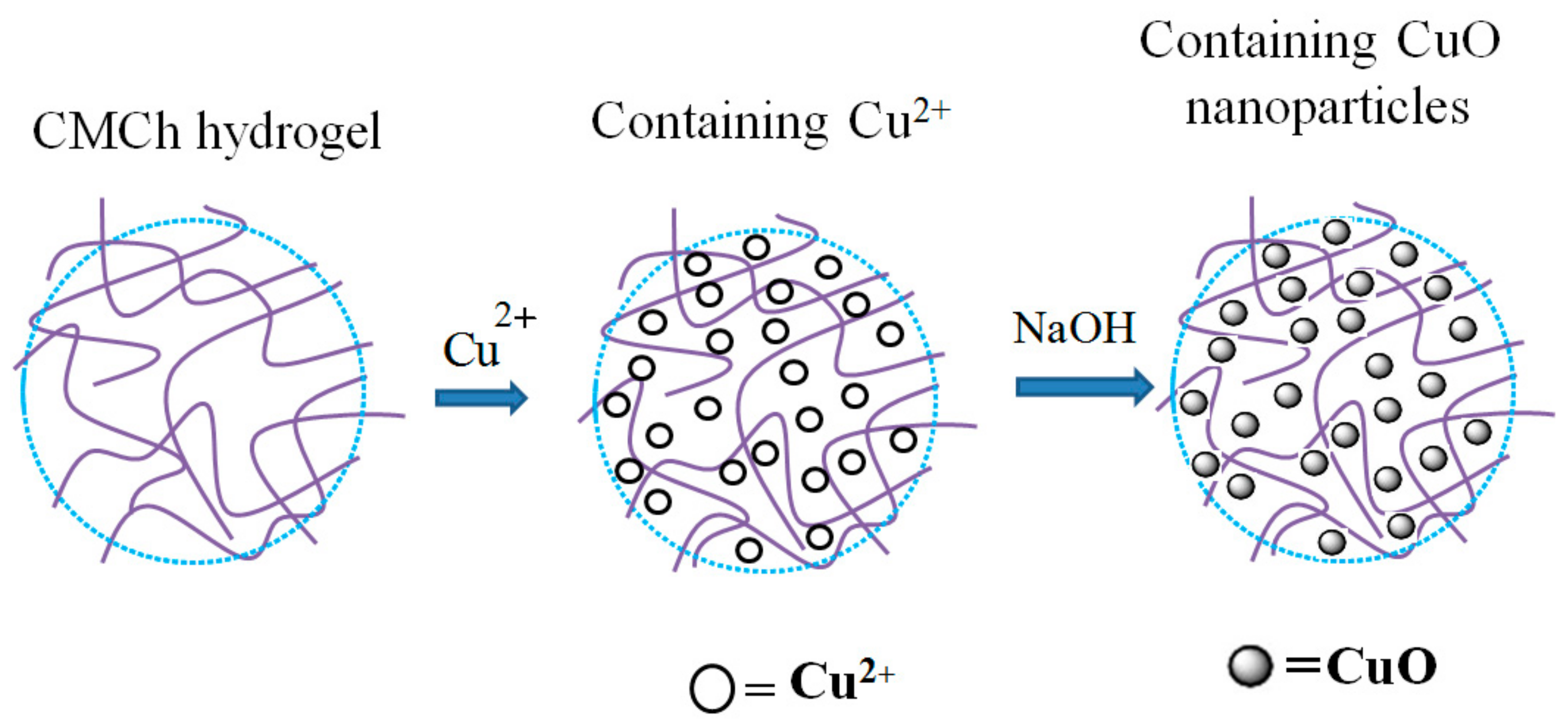
7.2. Antimicrobial Hydrogels Containing CuO Nanoparticles
7.3. Antimicrobial Hydrogels Containing TiO2 Nanoparticles
7.4. Antimicrobial Hydrogels Containing MgO Nanoparticles
8. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| A. baumannii | Acinetobacter baumannii |
| A. flavus | Aspergillus flavus |
| ADSCs | Adipose tissue-derived stem cells |
| Ag-NPs | Silver nanoparticles |
| APS | Ammonium persulfate |
| ATRP | Atom transfer radical polymerization |
| B. subtilis | Bacillus subtilis |
| BTM | Benzotriazole maleimide |
| C. albicans | Candida albicans |
| CMC | Carboxymethyl cellulose |
| CMCh | Carboxymethyl chitosan |
| Cu-NPs | Copper nanoparticles |
| CuO-NPs | Copper oxide nanoparticles |
| DADMAC | Diallyldimethylammonium chloride |
| DAM | Dopamine methacrylamide |
| E. coli | Escherichia coli |
| E. faecalis | Enterococcus faecalis |
| EDTA | Ethylene diamine tetraacetic acid |
| GA | Gum acacia |
| HDF | Human dermal fibroblast |
| K. pneumonia | Klebsiella pneumoniae |
| L. monocytogenes | Listeria monocytogenes |
| LDH | Layered double hydroxide |
| MBA | N,N′-methylene-bis-acrylamide |
| MgO-NPs | Magnesium oxide nanoparticles |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| N. gonorrhoeae | Neisseria gonorrhoeae |
| P. aeruginosa | Pseudomonas aeruginosa |
| PEG | Poly(ethylene glycol) |
| PEGMA | Poly(ethylene glycol) methyl ether methacrylate |
| PEIs | Poly(ethyleneimine)s |
| PMAPA | Poly (methyl methacrylate-co-acryloyl phenylalanine) |
| PNIPAAm | Poly(N-isopropyl acrylamide) |
| PVA | Poly vinyl alcohol |
| RAFT | Reversible addition fragmentation chain-transfer polymerization |
| ROP | Ring-opening polymerization |
| ROS | Reactive oxygen species |
| S. aureus | Staphylococcus aureus |
| S. epidermidis | Staphylococcus epidermidis |
| S. pyogenes | Streptococcus pyogenes |
| S.D. rats | Sprague-Dawley rats |
| SBE | Sulfobetaine |
| TEMED | N,N,N′,N′-tetramethylethylenediamine |
| TiO2-NPs | Titanium dioxide nanoparticles |
| TTO | Tea tree oil |
| XG | Xanthan gum |
| ZnO-NPs | Zinc oxide nanoparticles |
References
- Varaprasad, K.; Raghavendra, G.M.; Jayaramudu, T.; Yallapu, M.M.; Sadiku, R. A mini review on hydrogels classification and recent developments in miscellaneous applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 79, 958–971. [Google Scholar]
- Peppas, N.A.; Bures, P.; Leobandung, W.; Ichikawa, H. Hydrogels in pharmaceutical formulations. Eur. J. Pharm. Biopharm. 2000, 50, 27–46. [Google Scholar]
- Naahidi, S.; Jafari, M.; Logan, M.; Wang, Y.; Yuan, Y.; Bae, H.; Dixon, B.; Chen, P. Biocompatibility of hydrogel-based scaffolds for tissue engineering applications. Biotechnol. Adv. 2017, 35, 530–544. [Google Scholar]
- Wei, W.; Li, J.; Qi, X.; Zhong, Y.; Zuo, G.; Pan, X.; Su, T.; Zhang, J.; Dong, W. Synthesis and characterization of a multi-sensitive polysaccharide hydrogel for drug delivery. Carbohydr. Polym. 2017, 177, 275–283. [Google Scholar]
- Xu, X.; Xu, Z.; Yang, X.; He, Y.; Lin, R. Construction and characterization of a pure protein hydrogel for drug delivery application. Int. J. Biol. Macromol. 2017, 95, 294–298. [Google Scholar]
- Saboktakin, M.R.; Tabatabaei, R.M. Supramolecular hydrogels as drug delivery systems. Int. J. Biol. Macromol. 2015, 75, 426–436. [Google Scholar]
- Luo, Y.; Lou, C.; Zhang, S.; Zhu, Z.; Xing, Q.; Wang, P.; Liu, T.; Liu, H.; Li, C.; Shi, W.; et al. Three-dimensional hydrogel culture conditions promote the differentiation of human induced pluripotent stem cells into hepatocytes. Cytotherapy 2017. [Google Scholar] [CrossRef]
- Annabi, N.; Rana, D.; Shirzaei Sani, E.; Portillo-Lara, R.; Gifford, J.L.; Fares, M.M.; Mithieux, S.M.; Weiss, A.S. Engineering a sprayable and elastic hydrogel adhesive with antimicrobial properties for wound healing. Biomaterials 2017, 139, 229–243. [Google Scholar]
- Xiao, Y.; Gong, T.; Jiang, Y.; Wang, Y.; Wen, Z.T.; Zhou, S.; Bao, C.; Xu, X. Fabrication and characterization of a glucose-sensitive antibacterial chitosan–polyethylene oxide hydrogel. Polymer 2016, 82, 1–10. [Google Scholar]
- Yang, D.H.; Seo, D.I.; Lee, D.-W.; Bhang, S.H.; Park, K.; Jang, G.; Kim, C.H.; Chun, H.J. Preparation and evaluation of visible-light cured glycol chitosan hydrogel dressing containing dual growth factors for accelerated wound healing. J. Ind. Eng. Chem. 2017, 53, 360–370. [Google Scholar]
- Snyder-Talkington, B.N.; Qian, Y.; Castranova, V.; Guo, N.L. New perspectives for in vitro risk assessment of multiwalled carbon nanotubes: Application of coculture and bioinformatics. J. Toxicol. Environ. Health B 2012, 15, 468–492. [Google Scholar]
- Thoniyot, P.; Tan, M.J.; Karim, A.A.; Young, D.J.; Loh, X.J. Nanoparticle-hydrogel composites: Concept, design, and applications of these promising, multi-functional materials. Adv. Sci. 2015, 2. [Google Scholar] [CrossRef]
- Murali Mohan, Y.; Lee, K.; Premkumar, T.; Geckeler, K.E. Hydrogel networks as nanoreactors: A novel approach to silver nanoparticles for antibacterial applications. Polymer 2007, 48, 158–164. [Google Scholar]
- Schexnailder, P.; Schmidt, G. Nanocomposite polymer hydrogels. Colloid Polym. Sci. 2009, 287, 1–11. [Google Scholar]
- Li, L.; Wang, Y.; Pan, L.; Shi, Y.; Cheng, W.; Shi, Y.; Yu, G. A nanostructured conductive hydrogels-based biosensor platform for human metabolite detection. Nano Lett. 2015, 15, 1146–1151. [Google Scholar]
- Yadollahi, M.; Farhoudian, S.; Barkhordari, S.; Gholamali, I.; Farhadnejad, H.; Motasadizadeh, H. Facile synthesis of chitosan/ZnO bio-nanocomposite hydrogel beads as drug delivery systems. Int. J. Biol. Macromol. 2016, 82, 273–278. [Google Scholar]
- Wei, Y.-S.; Chen, K.-S.; Wu, L.-T. In situ synthesis of high swell ratio polyacrylic acid/silver nanocomposite hydrogels and their antimicrobial properties. J. Inorg. Biochem. 2016, 164, 17–25. [Google Scholar]
- Malagurski, I.; Levic, S.; Pantic, M.; Matijasevic, D.; Mitric, M.; Pavlovic, V.; Dimitrijevic-Brankovic, S. Synthesis and antimicrobial properties of Zn-mineralized alginate nanocomposites. Carbohydr. Polym. 2017, 165, 313–321. [Google Scholar]
- Raguvaran, R.; Manuja, B.K.; Chopra, M.; Thakur, R.; Anand, T.; Kalia, A.; Manuja, A. Sodium alginate and gum acacia hydrogels of ZnO nanoparticles show wound healing effect on fibroblast cells. Int. J. Biol. Macromol. 2017, 96, 185–191. [Google Scholar]
- Berdy, J. Thoughts and facts about antibiotics: Where we are now and where we are heading. J. Antibiot. 2012, 65, 385–395. [Google Scholar]
- Engler, A.C.; Wiradharma, N.; Ong, Z.Y.; Coady, D.J.; Hedrick, J.L.; Yang, Y.-Y. Emerging trends in macromolecular antimicrobials to fight multi-drug-resistant infections. Nano Today 2012, 7, 201–222. [Google Scholar]
- Fox, J.L. Antimicrobial peptides stage a comeback. Nat. Biotechnol. 2013, 31, 379–382. [Google Scholar]
- Huh, A.J.; Kwon, Y.J. “Nanoantibiotics”: A new paradigm for treating infectious diseases using nanomaterials in the antibiotics resistant era. J. Control. Release 2011, 156, 128–145. [Google Scholar]
- Brogden, K.A. Antimicrobial peptides: Pore formers or metabolic inhibitors in bacteria? Nat. Rev. Microbiol. 2005, 3, 238–250. [Google Scholar]
- Ng, V.W.; Chan, J.M.; Sardon, H.; Ono, R.J.; Garcia, J.M.; Yang, Y.Y.; Hedrick, J.L. Antimicrobial hydrogels: A new weapon in the arsenal against multidrug-resistant infections. Adv. Drug Deliv. Rev. 2014, 78, 46–62. [Google Scholar]
- Azizi, S.; Mohamad, R.; Abdul Rahim, R.; Mohammadinejad, R.; Bin Ariff, A. Hydrogel beads bio-nanocomposite based on Kappa-Carrageenan and green synthesized silver nanoparticles for biomedical applications. Int. J. Biol. Macromol. 2017, 104, 423–431. [Google Scholar]
- Dizaj, S.M.; Lotfipour, F.; Barzegar-Jalali, M.; Zarrintan, M.H.; Adibkia, K. Antimicrobial activity of the metals and metal oxide nanoparticles. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 44, 278–284. [Google Scholar]
- Dash, M.; Chiellini, F.; Ottenbrite, R.; Chiellini, E. Chitosan—A versatile semi-synthetic polymer in biomedical applications. Prog. Polym. Sci. 2011, 36, 981–1014. [Google Scholar]
- Wedmore, I.; McManus, J.G.; Pusateri, A.E.; Holcomb, J.B. A special report on the chitosan-based hemostatic dressing: Experience in current combat operations. J. Trauma Acute Care Surg. 2006, 60, 655–658. [Google Scholar]
- Ferreira, M.O.G.; Leite, L.L.R.; de Lima, I.S.; Barreto, H.M.; Nunes, L.C.C.; Ribeiro, A.B.; Osajima, J.A.; da Silva Filho, E.C. Chitosan Hydrogel in combination with Nerolidol for healing wounds. Carbohydr. Polym. 2016, 152, 409–418. [Google Scholar]
- Gao, B.; Zhang, X.; Zhu, Y. Studies on the preparation and antibacterial properties of quaternized polyethyleneimine. J. Biomater. Sci. Polym. Ed. 2007, 18, 531–544. [Google Scholar]
- Dohm, M.T.; Mowery, B.P.; Czyzewski, A.M.; Stahl, S.S.; Gellman, S.H.; Barron, A.E. Biophysical mimicry of lung surfactant protein B by random nylon-3 copolymers. J. Am. Chem. Soc. 2010, 132, 7957–7967. [Google Scholar]
- Palermo, E.F.; Kuroda, K. Chemical structure of cationic groups in amphiphilic polymethacrylates modulates the antimicrobial and hemolytic activities. Biomacromolecules 2009, 10, 1416–1428. [Google Scholar]
- Lienkamp, K.; Madkour, A.E.; Musante, A.; Nelson, C.F.; Nusslein, K.; Tew, G.N. Antimicrobial polymers prepared by ROMP with unprecedented selectivity: A molecular construction kit approach. J. Am. Chem. Soc. 2008, 130, 9836–9843. [Google Scholar]
- Som, A.; Navasa, N.; Percher, A.; Scott, R.W.; Tew, G.N.; Anguita, J. Identification of synthetic host defense peptide mimics that exert dual antimicrobial and anti-inflammatory activities. Clin. Vaccine Immunol. 2012, 19, 1784–1791. [Google Scholar]
- Engler, A.C.; Shukla, A.; Puranam, S.; Buss, H.G.; Jreige, N.; Hammond, P.T. Effects of side group functionality and molecular weight on the activity of synthetic antimicrobial polypeptides. Biomacromolecules 2011, 12, 1666–1674. [Google Scholar]
- Fukushima, K.; Tan, J.P.; Korevaar, P.A.; Yang, Y.Y.; Pitera, J.; Nelson, A.; Maune, H.; Coady, D.J.; Frommer, J.E.; Engler, A.C. Broad-spectrum antimicrobial supramolecular assemblies with distinctive size and shape. ACS Nano 2012, 6, 9191–9199. [Google Scholar]
- Bui, V.; Park, D.; Lee, Y.-C. Chitosan Combined with ZnO, TiO2 and Ag Nanoparticles for Antimicrobial Wound Healing Applications: A Mini Review of the Research Trends. Polymers 2017, 9, 21. [Google Scholar]
- Besinis, A.; De Peralta, T.; Handy, R.D. The antibacterial effects of silver, titanium dioxide and silica dioxide nanoparticles compared to the dental disinfectant chlorhexidine on Streptococcus mutans using a suite of bioassays. Nanotoxicology 2014, 8, 1–16. [Google Scholar]
- Ravindranadh, M.R.K.; Mary, T.R. Development of ZnO Nanoparticles for Clinical Applications. J. Chem. Biol. Phys. Sci. 2013, 4, 469. [Google Scholar]
- Leung, Y.H.; Ng, A.M.C.; Xu, X.; Shen, Z.; Gethings, L.A.; Wong, M.T.; Chan, C.M.N.; Guo, M.Y.; Ng, Y.H.; Djurisic, A.B.; et al. Mechanisms of Antibacterial Activity of MgO: Non-ROS Mediated Toxicity of MgO Nanoparticles towards Escherichia coli. Small 2014, 10, 1171–1183. [Google Scholar]
- Azam, A.; Ahmed, A.S.; Oves, M.; Khan, M.S.; Habib, S.S.; Memic, A. Antimicrobial activity of metal oxide nanoparticles against Gram-positive and Gram-negative bacteria: A comparative study. Int. J. Nanomed. 2012, 7, 6003–6009. [Google Scholar]
- Sondi, I.; Salopek-Sondi, B. Silver nanoparticles as antimicrobial agent: A case study on E. coli as a model for Gram-negative bacteria. J. Colloid Interface Sci. 2004, 275, 177–182. [Google Scholar]
- Buzea, C.; Pacheco, I.I.; Robbie, K. Nanomaterials and nanoparticles: Sources and toxicity. Biointerphases 2007, 2, MR17–MR71. [Google Scholar]
- Kim, J.D.; Yun, H.; Kim, G.C.; Lee, C.W.; Choi, H.C. Antibacterial activity and reusability of CNT-Ag and GO-Ag nanocomposites. Appl. Surf. Sci. 2013, 283, 227–233. [Google Scholar]
- Applerot, G.; Lellouche, J.; Lipovsky, A.; Nitzan, Y.; Lubart, R.; Gedanken, A.; Banin, E. Understanding the antibacterial mechanism of CuO nanoparticles: Revealing the route of induced oxidative stress. Small 2012, 8, 3326–3337. [Google Scholar]
- Seil, J.T.; Webster, T.J. Antimicrobial applications of nanotechnology: Methods and literature. Int. J. Nanomed. 2012, 7, 2767. [Google Scholar]
- Mohammadi, G.; Valizadeh, H.; Barzegar-Jalali, M.; Lotfipour, F.; Adibkia, K.; Milani, M.; Azhdarzadeh, M.; Kiafar, F.; Nokhodchi, A. Development of azithromycin–PLGA nanoparticles: Physicochemical characterization and antibacterial effect against Salmonella typhi. Colloids Surf. B Biointerfaces 2010, 80, 34–39. [Google Scholar]
- Fellahi, O.; Sarma, R.K.; Das, M.R.; Saikia, R.; Marcon, L.; Coffinier, Y.; Hadjersi, T.; Maamache, M.; Boukherroub, R. The antimicrobial effect of silicon nanowires decorated with silver and copper nanoparticles. Nanotechnology 2013, 24, 495101. [Google Scholar]
- Mohammadi, G.; Nokhodchi, A.; Barzegar-Jalali, M.; Lotfipour, F.; Adibkia, K.; Ehyaei, N.; Valizadeh, H. Physicochemical and anti-bacterial performance characterization of clarithromycin nanoparticles as colloidal drug delivery system. Colloids Surf. B Biointerfaces 2011, 88, 39–44. [Google Scholar]
- Pal, S.; Tak, Y.K.; Song, J.M. Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the gram-negative bacterium Escherichia coli. Appl. Environ. Microbiol. 2007, 73, 1712–1720. [Google Scholar]
- Bera, R.; Mandal, S.; Raj, C.R. Antimicrobial activity of fluorescent Ag nanoparticles. Lett. Appl. Microbiol. 2014, 58, 520–526. [Google Scholar]
- Janovák, L.; Dékány, I. Optical properties and electric conductivity of gold nanoparticle-containing, hydrogel-based thin layer composite films obtained by photopolymerization. Appl. Surf. Sci. 2010, 256, 2809–2817. [Google Scholar]
- Liu, M.J.; Ishida, Y.; Ebina, Y.; Sasaki, T.; Aida, T. Photolatently modulable hydrogels using unilamellar titania nanosheets as photocatalytic crosslinkers. Nat. Commun. 2013, 4. [Google Scholar] [CrossRef]
- Gogoi, N.; Chowdhury, D. In-Situ and Ex-Situ Chitosan-Silver Nanoparticle Composite: Comparison of Storage/Release and Catalytic Properties. J. Nanosci. Nanotechnol. 2014, 14, 4147–4155. [Google Scholar]
- Hezaveh, H.; Muhamad, II. Effect of MgO nanofillers on burst release reduction from hydrogel nanocomposites. J. Mater. Sci. Mater. Med. 2013, 24, 1443–1453. [Google Scholar]
- Hackenberg, S.; Friehs, G.; Froelich, K.; Ginzkey, C.; Koehler, C.; Scherzed, A.; Burghartz, M.; Hagen, R.; Kleinsasser, N. Intracellular distribution, geno- and cytotoxic effects of nanosized titanium dioxide particles in the anatase crystal phase on human nasal mucosa cells. Toxicol. Lett. 2010, 195, 9–14. [Google Scholar]
- Mohan, Y.M.; Vimala, K.; Thomas, V.; Varaprasad, K.; Sreedhar, B.; Bajpai, S.K.; Raju, K.M. Controlling of silver nanoparticles structure by hydrogel networks. J. Colloid Interface Sci. 2010, 342, 73–82. [Google Scholar]
- Wang, Y.L.; Li, B.Q.; Zhou, Y.; Jia, D.C. Chitosan-induced synthesis of magnetite nanoparticles via iron ions assembly. Polym. Adv. Technol. 2008, 19, 1256–1261. [Google Scholar]
- Xiong, Z.; Sun, Z.B.; Zheng, M.L.; Cao, Y.Y.; Jin, F.; Chen, W.Q.; Zhao, Z.S.; Duan, X.M. A facile method for the room-temperature synthesis of water-soluble magnetic Fe3O4 nanoparticles: Combination of in situ synthesis and decomposition of polymer hydrogel. Mater. Chem. Phys. 2011, 130, 72–78. [Google Scholar]
- Ozay, O.; Aktas, N.; Inger, E.; Sahiner, N. Hydrogel assisted nickel nanoparticle synthesis and their use in hydrogen production from sodium boron hydride. Int. J. Hydrog. Energy 2011, 36, 1998–2006. [Google Scholar]
- Contin, A.; Biffis, A.; Sterchele, S.; Dormbach, K.; Schipmann, S.; Pich, A. Metal nanoparticles inside microgel/clay nanohybrids: Synthesis, characterization and catalytic efficiency in cross-coupling reactions. J. Colloid Interface Sci. 2014, 414, 41–45. [Google Scholar]
- Thomas, V.; Yallapu, M.M.; Sreedhar, B.; Bajpai, S.K. A versatile strategy to fabricate hydrogel-silver nanocomposites and investigation of their antimicrobial activity. J. Colloid Interface Sci. 2007, 315, 389–395. [Google Scholar]
- Bajpai, S.K.; Jadaun, M.; Tiwari, S. Synthesis, characterization and antimicrobial applications of zinc oxide nanoparticles loaded gum acacia/poly(SA) hydrogels. Carbohydr. Polym. 2016, 153, 60–65. [Google Scholar]
- Carlsson, L.; Rose, S.; Hourdet, D.; Marcellan, A. Nano-hybrid self-crosslinked PDMA/silica hydrogels. Soft Matter 2010, 6, 3619–3631. [Google Scholar]
- Haraguchi, K. Synthesis and properties of soft nanocomposite materials with novel organic/inorganic network structures. Polym. J. 2011, 43, 223–241. [Google Scholar]
- Haraguchi, K.; Ebato, M.; Takehisa, T. Polymer-clay nanocomposites exhibiting abnormal necking phenomena accompanied by extremely large reversible elongations and excellent transparency. Adv. Mater. 2006, 18, 2250–2254. [Google Scholar]
- Pasqui, D.; Atrei, A.; Giani, G.; De Cagna, M.; Barbucci, R. Metal oxide nanoparticles as cross-linkers in polymeric hybrid hydrogels. Mater. Lett. 2011, 65, 392–395. [Google Scholar]
- Wang, Q.; Gao, Z. A constitutive model of nanocomposite hydrogels with nanoparticle crosslinkers. J. Mech. Phys. Solids 2016, 94, 127–147. [Google Scholar]
- Wu, H.; Yu, G.H.; Pan, L.J.; Liu, N.A.; McDowell, M.T.; Bao, Z.A.; Cui, Y. Stable Li-ion battery anodes by in-situ polymerization of conducting hydrogel to conformally coat silicon nanoparticles. Nat. Commun. 2013, 4. [Google Scholar] [CrossRef]
- Xing, B.; Choi, M.F.; Xu, B. Design of coordination polymer gels as stable catalytic systems. Chem. Eur. J. 2002, 8, 5028–5032. [Google Scholar]
- Xing, B.; Choi, M.-F.; Xu, B. A stable metal coordination polymer gel based on a calix [4] arene and its “uptake” of non-ionic organic molecules from the aqueous phase. Chem. Commun. 2002, 4, 362–363. [Google Scholar]
- Sangeetha, N.M.; Maitra, U. Supramolecular gels: Functions and uses. Chem. Soc. Rev. 2005, 34, 821–836. [Google Scholar]
- George, M.; Weiss, R.G. Low molecular-mass gelators with diyne functional groups and their unpolymerized and polymerized gel assemblies. Chem. Mater. 2003, 15, 2879–2888. [Google Scholar]
- European Wound Management Association. Position Document: Management of Wound Infection; MEP Ltd.: London, UK, 2006. [Google Scholar]
- Feng, Q.; Wu, J.; Chen, G.; Cui, F.; Kim, T.; Kim, J. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J. Biomed. Mater. Res. 2000, 52, 662–668. [Google Scholar]
- Lansdown, A. Silver. I: Its antibacterial properties and mechanism of action. J. Wound Care 2002, 11, 125–130. [Google Scholar]
- Graham, C. The role of silver in wound healing. Br. J. Nurs. 2005, 14, 22–28. [Google Scholar]
- Hermans, M.H. Silver-Containing Dressings and the Need for Evidence. Am. J. Nurs. 2006, 106, 60–68. [Google Scholar]
- Ansari, M.; Khan, H.; Khan, A. Evaluation of antibacterial activity of silver nanoparticles against MSSA and MSRA on isolates from skin infections. Biol. Med. 2011, 3, 141–146. [Google Scholar]
- Lansdown, A. Silver. 2: Toxicity in mammals and how its products aid wound repair. J. Wound Care 2002, 11, 173–177. [Google Scholar]
- Low, W.; Kenward, M.A.; Amin, M.; Martin, C. Ionically Crosslinked Chitosan Hydrogels for the Controlled Release of Antimicrobial Essential Oils and Metal Ions for Wound Management Applications. Medicines 2016, 3, 8. [Google Scholar]
- Mrlík, M.; Špírek, M.; Al-Khori, J.; Ahmad, A.A.; Mosnaček, J.; AlMaadeed, M.A.; Kasák, P. Mussel-mimicking sulfobetaine-based copolymer with metal tunable gelation, self-healing and antibacterial capability. Arab. J. Chem. 2017. [Google Scholar] [CrossRef]
- Klinkajon, W.; Supaphol, P. Novel copper (II) alginate hydrogels and their potential for use as anti-bacterial wound dressings. Biomed. Mater. 2014, 9, 045008. [Google Scholar] [CrossRef]
- Wahid, F.; Wang, H.-S.; Zhong, C.; Chu, L.-Q. Facile fabrication of moldable antibacterial carboxymethyl chitosan supramolecular hydrogels cross-linked by metal ions complexation. Carbohydr. Polym. 2017, 165, 455–461. [Google Scholar]
- Egger, S.; Lehmann, R.P.; Height, M.J.; Loessner, M.J.; Schuppler, M. Antimicrobial properties of a novel silver-silica nanocomposite material. Appl. Environ. Microbiol. 2009, 75, 2973–2976. [Google Scholar]
- Malarkodi, C.; Rajeshkumar, S.; Paulkumar, K.; Vanaja, M.; Gnanajobitha, G.; Annadurai, G. Biosynthesis and antimicrobial activity of semiconductor nanoparticles against oral pathogens. Bioinorg. Chem. Appl. 2014, 2014, 347167. [Google Scholar] [CrossRef]
- Jo, Y.-K.; Kim, B.H.; Jung, G. Antifungal activity of silver ions and nanoparticles on phytopathogenic fungi. Plant Dis. 2009, 93, 1037–1043. [Google Scholar]
- Allahverdiyev, A.M.; Abamor, E.S.; Bagirova, M.; Rafailovich, M. Antimicrobial effects of TiO2 and Ag2O nanoparticles against drug-resistant bacteria and leishmania parasites. Future Microbiol. 2011, 6, 933–940. [Google Scholar]
- Lok, C.-N.; Ho, C.-M.; Chen, R.; He, Q.-Y.; Yu, W.-Y.; Sun, H.; Tam, P.K.-H.; Chiu, J.-F.; Che, C.-M. Proteomic analysis of the mode of antibacterial action of silver nanoparticles. J. Proteome Res. 2006, 5, 916–924. [Google Scholar]
- Yun, H.; Kim, J.D.; Choi, H.C.; Lee, C.W. Antibacterial activity of CNT-Ag and GO-Ag nanocomposites against gram-negative and gram-positive bacteria. Bull. Korean Chem. Soc. 2013, 34, 3261–3264. [Google Scholar]
- Iavicoli, I.; Fontana, L.; Leso, V.; Bergamaschi, A. The effects of nanomaterials as endocrine disruptors. Int. J. Mol. Sci. 2013, 14, 16732–16801. [Google Scholar]
- Yadollahi, M.; Namazi, H.; Aghazadeh, M. Antibacterial carboxymethyl cellulose/Ag nanocomposite hydrogels cross-linked with layered double hydroxides. Int. J. Biol. Macromol. 2015, 79, 269–277. [Google Scholar]
- Panacek, A.; Kilianova, M.; Prucek, R.; Husickova, V.; Vecerova, R.; Kolar, M.; Kvitek, L.; Zboril, R. Preparation and in vitro bactericidal and fungicidal efficiency of nanosilver/methylcellulose hydrogel. Int. J. Chem. Mol. Nucl. Mater. Metall. Eng. 2014, 8, 493–498. [Google Scholar]
- Pérez-Díaz, M.; Alvarado-Gomez, E.; Magaña-Aquino, M.; Sánchez-Sánchez, R.; Velasquillo, C.; Gonzalez, C.; Ganem-Rondero, A.; Martínez-Castañon, G.; Zavala-Alonso, N.; Martinez-Gutierrez, F. Anti-biofilm activity of chitosan gels formulated with silver nanoparticles and their cytotoxic effect on human fibroblasts. Mater. Sci. Eng. C 2016, 60, 317–323. [Google Scholar]
- González-Sánchez, M.I.; Perni, S.; Tommasi, G.; Morris, N.G.; Hawkins, K.; López-Cabarcos, E.; Prokopovich, P. Silver nanoparticle based antibacterial methacrylate hydrogels potential for bone graft applications. Mater. Sci. Eng. C 2015, 50, 332–340. [Google Scholar]
- García-Astrain, C.; Chen, C.; Burón, M.; Palomares, T.; Eceiza, A.; Fruk, L.; Corcuera, M.Á.; Gabilondo, N. Biocompatible hydrogel nanocomposite with covalently embedded silver nanoparticles. Biomacromolecules 2015, 16, 1301–1310. [Google Scholar]
- Narayanan, K.B.; Han, S.S. Dual-crosslinked poly (vinyl alcohol)/sodium alginate/silver nanocomposite beads–A promising antimicrobial material. Food Chem. 2017, 234, 103–110. [Google Scholar]
- Hussain, I.S.A.; Jaisankar, V. An eco-friendly synthesis, characterization and antibacterial applications of novel almond gum–poly (acrylamide) based hydrogel silver nanocomposite. Polym. Test. 2017, 62, 154–161. [Google Scholar]
- Bozaci, E.; Akar, E.; Ozdogan, E.; Demir, A.; Altinisik, A.; Seki, Y. Application of carboxymethylcellulose hydrogel based silver nanocomposites on cotton fabrics for antibacterial property. Carbohydr. Polym. 2015, 134, 128–135. [Google Scholar]
- Montazer, M.; Keshvari, A.; Kahali, P. Tragacanth gum/nano silver hydrogel on cotton fabric: In-situ synthesis and antibacterial properties. Carbohydr. Polym. 2016, 154, 257–266. [Google Scholar]
- Bhowmick, S.; Koul, V. Assessment of PVA/silver nanocomposite hydrogel patch as antimicrobial dressing scaffold: Synthesis, characterization and biological evaluation. Mater. Sci. Eng. C 2016, 59, 109–119. [Google Scholar]
- Abdel-Halim, E.S.; Al-Deyab, S.S. Antimicrobial activity of silver/starch/polyacrylamide nanocomposite. Int. J. Biol. Macromol. 2014, 68, 33–38. [Google Scholar]
- Tyliszczak, B.; Drabczyk, A.; Kudłacik-Kramarczyk, S.; Bialik-Wąs, K.; Kijkowska, R.; Sobczak-Kupiec, A. Preparation and cytotoxicity of chitosan-based hydrogels modified with silver nanoparticles. Colloids Surf. B Biointerfaces 2017, 160, 325–330. [Google Scholar]
- Rao, K.M.; Kumar, A.; Haider, A.; Han, S.S. Polysaccharides based antibacterial polyelectrolyte hydrogels with silver nanoparticles. Mater. Lett. 2016, 184, 189–192. [Google Scholar]
- Sahraei, R.; Ghaemy, M. Synthesis of modified gum tragacanth/graphene oxide composite hydrogel for heavy metal ions removal and preparation of silver nanocomposite for antibacterial activity. Carbohydr. Polym. 2017, 157, 823–833. [Google Scholar]
- Mohamed, R.R.; Sabaa, M.W. Synthesis and characterization of antimicrobial crosslinked carboxymethyl chitosan nanoparticles loaded with silver. Int. J. Biol. Macromol. 2014, 69, 95–99. [Google Scholar]
- Helaly, F.M.; El-Sawy, S.M.; Hashem, A.I.; Khattab, A.A.; Mourad, R.M. Synthesis and characterization of nanosilver-silicone hydrogel composites for inhibition of bacteria growth. Contact Lens Anterior Eye 2017, 40, 59–66. [Google Scholar]
- Alshehri, S.M.; Aldalbahi, A.; Al-hajji, A.B.; Chaudhary, A.A.; Panhuis, M.I.H.; Alhokbany, N.; Ahamad, T. Development of carboxymethyl cellulose-based hydrogel and nanosilver composite as antimicrobial agents for UTI pathogens. Carbohydr. Polym. 2016, 138, 229–236. [Google Scholar]
- Reddy, P.R.S.; Rao, K.S.V.K.; Rao, K.M.; Reddy, N.S.; Eswaramma, S. pH sensitive poly(methyl methacrylate-co-acryloyl phenylalanine) nanogels and their silver nanocomposites for biomedical applications. J. Drug Deliv. Sci. Technol. 2015, 29, 181–188. [Google Scholar]
- Jayaramudu, T.; Raghavendra, G.M.; Varaprasad, K.; Sadiku, R.; Ramam, K.; Raju, K.M. Iota-Carrageenan-based biodegradable Ag 0 nanocomposite hydrogels for the inactivation of bacteria. Carbohydr. Polym. 2013, 95, 188–194. [Google Scholar]
- Surudžić, R.; Janković, A.; Bibić, N.; Vukašinović-Sekulić, M.; Perić-Grujić, A.; Mišković-Stanković, V.; Park, S.J.; Rhee, K.Y. Physico-chemical and mechanical properties and antibacterial activity of silver/poly(vinyl alcohol)/graphene nanocomposites obtained by electrochemical method. Compos. Part B Eng. 2016, 85, 102–112. [Google Scholar]
- Jiang, D.; Zhang, Y.; Zhang, F.; Liu, Z.; Han, J.; Wu, X. Antimicrobial and antifouling nanocomposite hydrogels containing polythioether dendron: High-loading silver nanoparticles and controlled particle release. Colloid Polym. Sci. 2016, 294, 2021–2028. [Google Scholar]
- Hebeish, A.; Hashem, M.; El-Hady, M.M.A.; Sharaf, S. Development of CMC hydrogels loaded with silver nano-particles for medical applications. Carbohydr. Polym. 2013, 92, 407–413. [Google Scholar]
- Spasojević, J.; Radosavljević, A.; Krstić, J.; Jovanović, D.; Spasojević, V.; Kalagasidis-Krušić, M.; Kačarević-Popović, Z. Dual responsive antibacterial Ag-poly(N-isopropylacrylamide/itaconic acid) hydrogel nanocomposites synthesized by gamma irradiation. Eur. Polym. J. 2015, 69, 168–185. [Google Scholar]
- Bajpai, S.K.; Kumari, M. A green approach to prepare silver nanoparticles loaded gum acacia/poly(acrylate) hydrogels. Int. J. Biol. Macromol. 2015, 80, 177–188. [Google Scholar]
- Stojkovska, J.; Kostić, D.; Jovanović, Ž.; Vukašinović-Sekulić, M.; Mišković-Stanković, V.; Obradović, B. A comprehensive approach to in vitro functional evaluation of Ag/alginate nanocomposite hydrogels. Carbohydr. Polym. 2014, 111, 305–314. [Google Scholar]
- Krishna Rao, K.S.V.; Ramasubba Reddy, P.; Lee, Y.-I.; Kim, C. Synthesis and characterization of chitosan–PEG–Ag nanocomposites for antimicrobial application. Carbohydr. Polym. 2012, 87, 920–925. [Google Scholar]
- Jayaramudu, T.; Varaprasad, K.; Raghavendra, G.M.; Sadiku, E.R.; Mohana Raju, K.; Amalraj, J. Green synthesis of tea Ag nanocomposite hydrogels via mint leaf extraction for effective antibacterial activity. J. Biomater. Sci. Polym. Ed. 2017, 28, 1588–1602. [Google Scholar]
- Obradovic, B.; Stojkovska, J.; Jovanovic, Z.; Miskovic-Stankovic, V. Novel alginate based nanocomposite hydrogels with incorporated silver nanoparticles. J. Mater. Sci. Mater. Med. 2012, 23, 99–107. [Google Scholar]
- Huang, K.-T.; Fang, Y.-L.; Hsieh, P.-S.; Li, C.-C.; Dai, N.-T.; Huang, C.-J. Non-sticky and antimicrobial zwitterionic nanocomposite dressings for infected chronic wounds. Biomater. Sci. 2017, 5, 1072–1081. [Google Scholar]
- Micic, M.; Milic, T.V.; Mitric, M.; Jokic, B.; Suljovrujic, E. Radiation synthesis, characterisation and antimicrobial application of novel copolymeric silver/poly (2-hydroxyethyl methacrylate/itaconic acid) nanocomposite hydrogels. Polym. Bull. 2013, 70, 3347–3357. [Google Scholar]
- Cha, H.-R.; Babu, V.R.; Rao, K.; Kim, Y.-H.; Mei, S.; Joo, W.-H.; Lee, Y.-I. Fabrication of amino acid based silver nanocomposite hydrogels from PVA-poly (acrylamide-co-acryloyl phenylalanine) and their antimicrobial studies. Bull. Korean Chem. Soc. 2012, 33, 3191–3195. [Google Scholar]
- Marsich, E.; Travan, A.; Donati, I.; Di Luca, A.; Benincasa, M.; Crosera, M.; Paoletti, S. Biological response of hydrogels embedding gold nanoparticles. Colloids Surf. B Biointerfaces 2011, 83, 331–339. [Google Scholar]
- Cometa, S.; Iatta, R.; Ricci, M.A.; Ferretti, C.; De Giglio, E. Analytical characterization and antimicrobial properties of novel copper nanoparticle-loaded electrosynthesized hydrogel coatings. J. Bioact. Compat. Polym. 2013, 28, 508–522. [Google Scholar]
- Emilia Villanueva, M.; del Rosario Diez, A.M.; Antonio Gonzalez, J.; Javier Perez, C.; Orrego, M.; Piehl, L.; Teves, S.; Javier Copello, G. Antimicrobial Activity of Starch Hydrogel Incorporated with Copper Nanoparticles. ACS Appl. Mater. Interfaces 2016, 8, 16280–16288. [Google Scholar]
- van den Brom, C.R.; Anac, I.; Roskamp, R.F.; Retsch, M.; Jonas, U.; Menges, B.; Preece, J.A. The swelling behaviour of thermoresponsive hydrogel/silica nanoparticle composites. J. Mater. Chem. 2010, 20, 4827–4839. [Google Scholar]
- Korotych, O.; Samchenko, Y.; Boldeskul, I.; Ulberg, Z.; Zholobak, N.; Sukhodub, L. N-isopropylacrylamide-based fine-dispersed thermosensitive ferrogels obtained via in-situ technique. Mater. Sci. Eng. C 2013, 33, 892–900. [Google Scholar]
- Daniel-da-Silva, A.L.; Carvalho, R.S.; Trindade, T. Magnetic hydrogel nanocomposites and composite nanoparticles—A review of recent patented works. Recent Pat. Nanotechnol. 2013, 7, 153–166. [Google Scholar]
- Sirelkhatim, A.; Mahmud, S.; Seeni, A.; Kaus, N.H.M.; Ann, L.C.; Bakhori, S.K.M.; Hasan, H.; Mohamad, D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nano Micro Lett. 2015, 7, 219–242. [Google Scholar]
- Colon, G.; Ward, B.C.; Webster, T.J. Increased osteoblast and decreased Staphylococcus epidermidis functions on nanophase ZnO and TiO2. J. Biomed. Mater. Res. A 2006, 78, 595–604. [Google Scholar]
- Padmavathy, N.; Vijayaraghavan, R. Enhanced bioactivity of ZnO nanoparticles—An antimicrobial study. Sci. Technol. Adv. Mater. 2008, 9, 035004. [Google Scholar]
- Applerot, G.; Lipovsky, A.; Dror, R.; Perkas, N.; Nitzan, Y.; Lubart, R.; Gedanken, A. Enhanced antibacterial activity of nanocrystalline ZnO due to increased ROS-mediated cell injury. Adv. Funct. Mater. 2009, 19, 842–852. [Google Scholar]
- Xie, Y.; He, Y.; Irwin, P.L.; Jin, T.; Shi, X. Antibacterial activity and mechanism of action of zinc oxide nanoparticles against Campylobacter jejuni. Appl. Environ. Microbiol. 2011, 77, 2325–2331. [Google Scholar]
- Zhang, L.; Ding, Y.; Povey, M.; York, D. ZnO nanofluids—A potential antibacterial agent. Prog. Nat. Sci. 2008, 18, 939–944. [Google Scholar]
- Kumar, P.T.S.; Lakshmanan, V.-K.; Biswas, R.; Nair, S.V.; Jayakumar, R. Synthesis and Biological Evaluation of Chitin Hydrogel/Nano ZnO Composite Bandage as Antibacterial Wound Dressing. J. Biomed. Nanotechnol. 2012, 8, 891–900. [Google Scholar]
- Kumar, S.P.T.; Lakshmanan, V.-K.; Raj, M.; Biswas, R.; Hiroshi, T.; Nair, S.V.; Jayakumar, R. Evaluation of Wound Healing Potential of beta-Chitin Hydrogel/Nano Zinc Oxide Composite Bandage. Pharm. Res. 2013, 30, 523–537. [Google Scholar]
- Păunica-Panea, G.; Ficai, A.; Marin, M.M.; Marin, Ş.; Albu, M.G.; Constantin, V.D.; Dinu-Pîrvu, C.; Vuluga, Z.; Corobea, M.C.; Ghica, M.V. New collagen-dextran-zinc oxide composites for wound dressing. J. Nanomater. 2016, 2016, 34. [Google Scholar] [CrossRef]
- Hashem, M.; Sharaf, S.; Abd El-Hady, M.M.; Hebeish, A. Synthesis and characterization of novel carboxymethylcellulose hydrogels and carboxymethylcellulolse-hydrogel-ZnO-nanocomposites. Carbohydr. Polym. 2013, 95, 421–427. [Google Scholar]
- Yadollahi, M.; Gholamali, I.; Namazi, H.; Aghazadeh, M. Synthesis and characterization of antibacterial carboxymethyl cellulose/ZnO nanocomposite hydrogels. Int. J. Biol. Macromol. 2015, 74, 136–141. [Google Scholar]
- Rakhshaei, R.; Namazi, H. A potential bioactive wound dressing based on carboxymethyl cellulose/ZnO impregnated MCM-41 nanocomposite hydrogel. Mater. Sci. Eng. C 2017, 73, 456–464. [Google Scholar]
- Wahid, F.; Yin, J.-J.; Xue, D.-D.; Xue, H.; Lu, Y.-S.; Zhong, C.; Chu, L.-Q. Synthesis and characterization of antibacterial carboxymethyl Chitosan/ZnO nanocomposite hydrogels. Int. J. Biol. Macromol. 2016, 88, 273–279. [Google Scholar]
- Chaturvedi, A.; Bajpai, A.K.; Bajpai, J.; Singh, S.K. Evaluation of poly (vinyl alcohol) based cryogel–zinc oxide nanocomposites for possible applications as wound dressing materials. Mater. Sci. Eng. C 2016, 65, 408–418. [Google Scholar]
- Schwartz, V.B.; Thétiot, F.; Ritz, S.; Pütz, S.; Choritz, L.; Lappas, A.; Förch, R.; Landfester, K.; Jonas, U. Antibacterial Surface Coatings from Zinc Oxide Nanoparticles Embedded in Poly(N-isopropylacrylamide) Hydrogel Surface Layers. Adv. Funct. Mater. 2012, 22, 2376–2386. [Google Scholar]
- Wang, J.; Hu, H.; Yang, Z.; Wei, J.; Li, J. IPN hydrogel nanocomposites based on agarose and ZnO with antifouling and bactericidal properties. Mater. Sci. Eng. C 2016, 61, 376–386. [Google Scholar]
- Kumar, P.T.S.; Lakshmanan, V.K.; Anilkumar, T.V.; Ramya, C.; Reshmi, P.; Unnikrishnan, A.G.; Nair, S.V.; Jayakumar, R. Flexible and Microporous Chitosan Hydrogel/Nano ZnO Composite Bandages for Wound Dressing: In Vitro and In Vivo Evaluation. ACS Appl. Mater. Interfaces 2012, 4, 2618–2629. [Google Scholar]
- Liu, Y.; Kim, H.I. Characterization and antibacterial properties of genipin-crosslinked chitosan/poly(ethylene glycol)/ZnO/Ag nanocomposites. Carbohydr. Polym. 2012, 89, 111–116. [Google Scholar]
- Filipic, G.; Cvelbar, U. Copper oxide nanowires: A review of growth. Nanotechnology 2012, 23. [Google Scholar] [CrossRef]
- Li, J.; Sun, F.; Gu, K.; Wu, T.; Zhai, W.; Li, W.; Huang, S. Preparation of spindly CuO micro-particles for photodegradation of dye pollutants under a halogen tungsten lamp. Appl. Catal. A Gen. 2011, 406, 51–58. [Google Scholar]
- Ren, G.; Hu, D.; Cheng, E.W.C.; Vargas-Reus, M.A.; Reip, P.; Allaker, R.P. Characterisation of copper oxide nanoparticles for antimicrobial applications. Int. J. Antimicrob. Agents 2009, 33, 587–590. [Google Scholar]
- Meghana, S.; Kabra, P.; Chakraborty, S.; Padmavathy, N. Understanding the pathway of antibacterial activity of copper oxide nanoparticles. RSC Adv. 2015, 5, 12293–12299. [Google Scholar]
- Gabbay, J.; Borkow, G.; Mishal, J.; Magen, E.; Zatcoff, R.; Shemer-Avni, Y. Copper oxide impregnated textiles with potent biocidal activities. J. Ind. Text. 2006, 35, 323–335. [Google Scholar]
- Llorens, A.; Lloret, E.; Picouet, P.; Fernandez, A. Study of the antifungal potential of novel cellulose/copper composites as absorbent materials for fruit juices. Int. J. Food Microbiol. 2012, 158, 113–119. [Google Scholar]
- Gopal, A.; Kant, V.; Gopalakrishnan, A.; Tandan, S.K.; Kumar, D. Chitosan-based copper nanocomposite accelerates healing in excision wound model in rats. Eur. J. Pharmacol. 2014, 731, 8–19. [Google Scholar]
- Li, B.; Li, Y.; Wu, Y.; Zhao, Y. Synthesis of water-soluble Cu/PAA composite flowers and their antibacterial activities. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 35, 205–211. [Google Scholar]
- Delgado, K.; Quijada, R.; Palma, R.; Palza, H. Polypropylene with embedded copper metal or copper oxide nanoparticles as a novel plastic antimicrobial agent. Lett. Appl. Microbiol. 2011, 53, 50–54. [Google Scholar]
- Hebeish, A.; Sharaf, S. Novel nanocomposite hydrogel for wound dressing and other medical applications. RSC Adv. 2015, 5, 103036–103046. [Google Scholar]
- Yadollahi, M.; Gholamali, I.; Namazi, H.; Aghazadeh, M. Synthesis and characterization of antibacterial carboxymethylcellulose/CuO bio-nanocomposite hydrogels. Int. J. Biol. Macromol. 2015, 73, 109–114. [Google Scholar]
- Farhoudian, S.; Yadollahi, M.; Namazi, H. Facile synthesis of antibacterial chitosan/CuO bio-nanocomposite hydrogel beads. Int. J. Biol. Macromol. 2016, 82, 837–843. [Google Scholar]
- Wahid, F.; Wang, H.S.; Lu, Y.S.; Zhong, C.; Chu, L.Q. Preparation, characterization and antibacterial applications of carboxymethyl chitosan/CuO nanocomposite hydrogels. Int. J. Biol. Macromol. 2017, 101, 690–695. [Google Scholar]
- Oun, A.A.; Rhim, J.-W. Carrageenan-based hydrogels and films: Effect of ZnO and CuO nanoparticles on the physical, mechanical, and antimicrobial properties. Food Hydrocoll. 2017, 67, 45–53. [Google Scholar]
- Liu, C.; Guo, J.; Yan, X.; Tang, Y.; Mazumder, A.; Wu, S.; Liang, Y. Antimicrobial nanomaterials against biofilms: An alternative strategy. Environ. Rev. 2017, 25, 225–244. [Google Scholar]
- Roy, A.S.; Parveen, A.; Koppalkar, A.R.; Prasad, M.V.N.A. Effect of Nano-Titanium Dioxide with Different Antibiotics against Methicillin-Resistant Staphylococcus Aureus. J. Biomater. Nanobiotechnol. 2010, 1, 37–41. [Google Scholar]
- Carre, G.; Hamon, E.; Ennahar, S.; Estner, M.; Lett, M.C.; Horvatovich, P.; Gies, J.P.; Keller, V.; Keller, N.; Andre, P. TiO2 Photocatalysis Damages Lipids and Proteins in Escherichia coli. Appl. Environ. Microbiol. 2014, 80, 2573–2581. [Google Scholar]
- Saqib, N.U.; Adnan, R.; Shah, I. A mini-review on rare earth metal-doped TiO2 for photocatalytic remediation of wastewater. Environ. Sci. Pollut. Res. 2016, 23, 15941–15951. [Google Scholar]
- Cerrada, M.L.; Serrano, C.; Sanchez-Chaves, M.; Fernandez-Garcia, M.; Fernandez-Martin, F.; de Andres, A.; Jimenez Rioboo, R.J.; Kubacka, A.; Ferrer, M.; Fernandez-Garcia, M. Self-sterilized EVOH-TiO2 nanocomposites: Interface effects on biocidal properties. Adv. Funct. Mater. 2008, 18, 1949–1960. [Google Scholar]
- Cerrada, M.L.; Serrano, C.; Sanchez-Chaves, M.; Fernandez-Garcia, M.; De Andres, A.; Rioboo, R.J.; Fernandez-Martin, F.; Kubacka, A.; Ferrer, M.; Fernandez-Garcia, M. Biocidal Capability Optimization in Organic-Inorganic Nanocomposites Based on Titania. Environ. Sci. Technol. 2009, 43, 1630–1634. [Google Scholar]
- Kong, H.; Song, J.; Jang, J. Photocatalytic Antibacterial Capabilities of TiO2-Biocidal Polymer Nanocomposites Synthesized by a Surface-Initiated Photopolymerization. Environ. Sci. Technol. 2010, 44, 5672–5676. [Google Scholar]
- Si, S.; Zhou, R.; Xing, Z.; Xu, H.; Cai, Y.; Zhang, Q. A Study of Hybrid Organic/Inorganic Hydrogel Films Based on in Situ-generated TiO2 Nanoparticles and Methacrylated Gelatin. Fibers Polym. 2013, 14, 982–989. [Google Scholar]
- Li, Y.-S.; Han, Y.; Qin, J.-T.; Song, Z.-Y.; Cai, H.-H.; Du, J.-F.; Sun, S.-F.; Liu, Y. Photosensitive antibacterial and cytotoxicity performances of a TiO2/carboxymethyl chitosan/poly(vinyl alcohol) nanocomposite hydrogel by in situ radiation construction. J. Appl. Polym. Sci. 2016, 133. [Google Scholar] [CrossRef]
- Yamamoto, O.; Ohira, T.; Alvarez, K.; Fukuda, M. Antibacterial characteristics of CaCO3-MgO composites. Mater. Sci. Eng. B Adv. Funct. Solid State Mater. 2010, 173, 208–212. [Google Scholar]
- Jin, T.; He, Y.P. Antibacterial activities of magnesium oxide (MgO) nanoparticles against foodborne pathogens. J. Nanopart. Res. 2011, 13, 6877–6885. [Google Scholar]
- Sawai, J.; Kojima, H.; Igarashi, H.; Hashimoto, A.; Shoji, S.; Sawaki, T.; Hakoda, A.; Kawada, E.; Kokugan, T.; Shimizu, M. Antibacterial characteristics of magnesium oxide powder. World J. Microbiol. Biotechnol. 2000, 16, 187–194. [Google Scholar]
- Muhamad, I.I.; Asgharzadehahmadi, S.A.A.; Zaidel, D.N.A.; Supriyanto, E. Characterization and Evaluation of Antibacterial Properties of Polyacrylamide Based Hydrogel Containing Magnesium Oxide Nanoparticles. Int. J. Biol. Biomed. Eng. 2013, 7, 108–113. [Google Scholar]



| Nanocomposite Hydrogel | Loading of Ag Nanoparticles | Antimicrobial Activity against | Applications | Ref. |
|---|---|---|---|---|
| Poly(vinyl alcohol)/sodium alginate/silver | Entrapment during physical cross-linking | E. coli | Food packaging | [98] |
| Almond gum-poly(acrylamide)/Ag | In situ preparation of Ag-NPs in hydrogel | S. aureus, E. coli, P. aeroginosa | Antibacterial material | [99] |
| Acrylic acid/Ag | UV-irradiation | S. aureus, C. albicans, P. aeruginosa, S. epidermidis, E. coli, A. baumannii, K. pneumonia | Super absorbent antimicrobial material for pharmaceutical applications | [17] |
| Kappa-Carrageenan (κ-Carrageenan)/Ag | Biosynthesis of Ag-NPs in Citrullus colocynthis seed extract | S. aureus, MRSA, P. aeruginosa, E. coli | Pharmaceutical applications | [26] |
| Carboxymethyl cellulose/Ag | In situ preparation of Ag-NPs with synthesis of hydrogel. | S. aureus K. pneumonia | Treatment of cotton fabrics for medical applications | [100] |
| Tragacanth gum/Ag | In situ of nano silver in hydrogel | S. aureus, E. coli | For cotton fabrics to improve its properties | [101] |
| Polyvinyl alcohol/Ag | Loading of Ag-NPs to polymeric hydrogel | S. aureus, E.coli, P. aeruginosa | Antimicrobial dressing scaffold | [102] |
| Silver/starch/polyacrylamide nanocomposites | In situ preparation of Ag-NPs inside hydrogel network | S. aureus, E. coli, A. flavus, C. albicans | Antimicrobial applications | [103] |
| Chitosan based hydrogel/Ag nanocomposites | UV-radiation | S. aureus, E. faecalis | Biomedical applications | [104] |
| Polysaccharides such as xanthan gum (XG) and chitosan (CS)/Ag nanocomposite hydrogel | In situ formation of Ag-NPs within hydrogel. | S. aureus, E. coli | Antibacterial wound dressing | [105] |
| Tragacanth gum and graphene oxide/Ag | In situ reduction of Ag+ to Ag0 flower extract of Achillea millefolium | S. aureus | Bio-absorbent for removal of heavy metals from water, with antimicrobial activity. | [106] |
| Carboxymethyl chitosan/Ag nanocomposite hydrogel | Synthesis of Ag-NPs with the formation of hydrogel. | S. aureus, S. faecalis, B. subtilis, P. aeruginosa, E.coli, N. gonorrhoeae, C. albicans | Antimicrobial hydrogels | [107] |
| Silicone/Ag nanocomposite hydrogel film | In situ chemical reduction of Ag+ by NaBH4 | B. subtilis, S. aureus, E. coli, P. aeruginosa | Contact lenses | [108] |
| Carboxymethyl cellulose (CMC), polyvinyl alcohol (PVA)/Ag | Incorporation of Ag-NPs by microwave radiations | E. coli, P. aeruginosa, K. pneumoniae, P. vulgaris, S. aureus P. mirabilis | Antibacterial applications | [109] |
| Poly (methyl methacrylate-co-acryloyl phenylalanine) (PMAPA)/Ag | Chemical reduction of Ag+ by NaBH4 | Bacilli, E. coli | Antibacterial applications | [110] |
| Iota-Carrageenan/Ag nanocomposite hydrogel | Biochemical reduction of Ag+ by leaf extract of Azadirachta indica | Bacillus, E. coli | Antimicrobial applications | [111] |
| Silver/poly(vinyl alcohol)/graphene nanocomposite hydrogel film | Electrochemical reduction of Ag+ ions. | E. coli, S. aureus | Wound dressing | [112] |
| Polythioether dendron/Ag | In situ chemical reduction of Ag+ by NaBH4 | E. coli and anti-algae | Antifouling coating of biomaterials. | [113] |
| Carboxymethyl cellulose/Ag nanocomposite hydrogel | In situ preparation of Ag-NPs in hydrogel as well as incorporation of Ag-NPs into hydrogel | P. aeruginosa, E. coli, S. aureus, B. subtilis. | Antibacterial applications | [114] |
| Ag-poly(N-isopropylacrylamide/itaconic acid) hydrogel | In situ reduction of Ag+ with gamma irradiation | S. aureus, E. coli | Antibacterial applications | [115] |
| Gum acacia (GA)/poly(sodium acrylate)/Ag semi-interpenetrating polymeric hydrogel | In situ reduction of Ag+ with extract of Syzygium aromaticum (clove) | E. coli | Antibacterial applications | [116] |
| Ag/Alginate nanocomposite hydrogel | Electrochemical production of Ag-NPs in hydrogel. | S. aureus, E. coli | Wound dressing | [117] |
| Chitosan-polyethylene glycol/Ag nanocomposite hydrogel | In situ reduction of Ag+ as well as incorporation of Ag-NPs into hydrogel | E. coli | Antimicrobial | [118] |
| Tea/polyacrylamide/Ag nanocomposite hydrogel | In situ reduction of Ag+ by mint leaf extract within hydrogel | S. aureus, E. coli | Antimicrobial | [119] |
| Alginate/polyvinyl alcohol/ poly(N-vinyl-2-pyrrolidone)/ Ag nanocomposite hydrogel | Electrochemical synthesis of Ag-NPs in hydrogel | E. coli | Wound dressing | [120] |
| Poly(sulfobetaine acrylamide)/Ag | In situ formation of Ag-NPs within hydrogel | S. epidermidis, P. aeruginosa | Treatment of infected chronic wounds | [121] |
| 2-hydroxyethyl methacrylate/itaconic acid/Ag | In situ reduction of silver nitrate by gamma radiations | E. coli, S. aureus, C. albicans | Wound dressing | [122] |
| Poly(acryl amide-co-acryloyl phenyl alanine)/Ag | In situ chemical reduction of Ag+ by NaBH4 | S. aureus, E. coli | Artificial burn dressing | [123] |
| Nanocomposite Hydrogel | Loading of ZnO Nanoparticles | Antimicrobial Activity against | Applications | Ref. |
|---|---|---|---|---|
| Gum acacia/poly sodium acrylate/ZnO | In situ preparation by hydrothermal method | E. coli | Antimicrobial | [64] |
| Alginate/gum acacia/ZnO | Addition of ZnO-NPs during the synthesis of hydrogel | P. aeruginosa, B. cereus | Wound dressing | [19] |
| Poly(ethylene glycol) methyl ether methacrylate modified ZnO (ZnO-PEGMA)/4-azidobenzoic agarose (AG-N3) IPN hydrogel | Addition of ZnO-NPs to PEGMA | S. aureus, E. coli | Wound dressing | [145] |
| Chitosan/ZnO flexible, microporous hydrogel | Incorporation of ZnO-NPs into hydrogel | S. aureus, E.coli | Wound dressing | [146] |
| Genipin-crosslinked chitosan (GC), poly(ethylene glycol) (PEG)/ZnO/Ag | Incorporation of ZnO and Ag nanoparticles into hydrogel matrix | E. coli, P. aeruginosa, S. aureus, B. subtilis | Wound dressing | [147] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wahid, F.; Zhong, C.; Wang, H.-S.; Hu, X.-H.; Chu, L.-Q. Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles. Polymers 2017, 9, 636. https://doi.org/10.3390/polym9120636
Wahid F, Zhong C, Wang H-S, Hu X-H, Chu L-Q. Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles. Polymers. 2017; 9(12):636. https://doi.org/10.3390/polym9120636
Chicago/Turabian StyleWahid, Fazli, Cheng Zhong, Hai-Song Wang, Xiao-Hui Hu, and Li-Qiang Chu. 2017. "Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles" Polymers 9, no. 12: 636. https://doi.org/10.3390/polym9120636
APA StyleWahid, F., Zhong, C., Wang, H.-S., Hu, X.-H., & Chu, L.-Q. (2017). Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles. Polymers, 9(12), 636. https://doi.org/10.3390/polym9120636





