Management and Outcome of Young Women (≤40 Years) with Breast Cancer in Switzerland
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Population and Data Source
2.2. Variables
- Triple-negative: estrogen receptor (ER) and progesterone receptor (PR) staining <1% and HER2 immunohistochemical score classified as 0 or 1+. In case of equivocal HER2 status (2+), tumors were considered HER2− if fluorescence in situ hybridization (FISH) showed an HER2-to-probe ratio < 2.0.
- HER2+: ER/PR < 1% and HER2 immunohistochemical score of 3+ or HER2-to-probe FISH ratio ≥ 2.0.
- Luminal A-like: ER/PR > 1% HER2- and Ki-67 < 14% or ER/PR > 1% HER2- and well or moderately differentiated tumors.
- Luminal-B-like: ER/PR > 1% HER2+ or ER/PR > 1% HER2- and Ki-67 ≥ 14%, or ER/PR > 1% HER2- and poorly differentiated tumors.
2.3. Covariate Measures
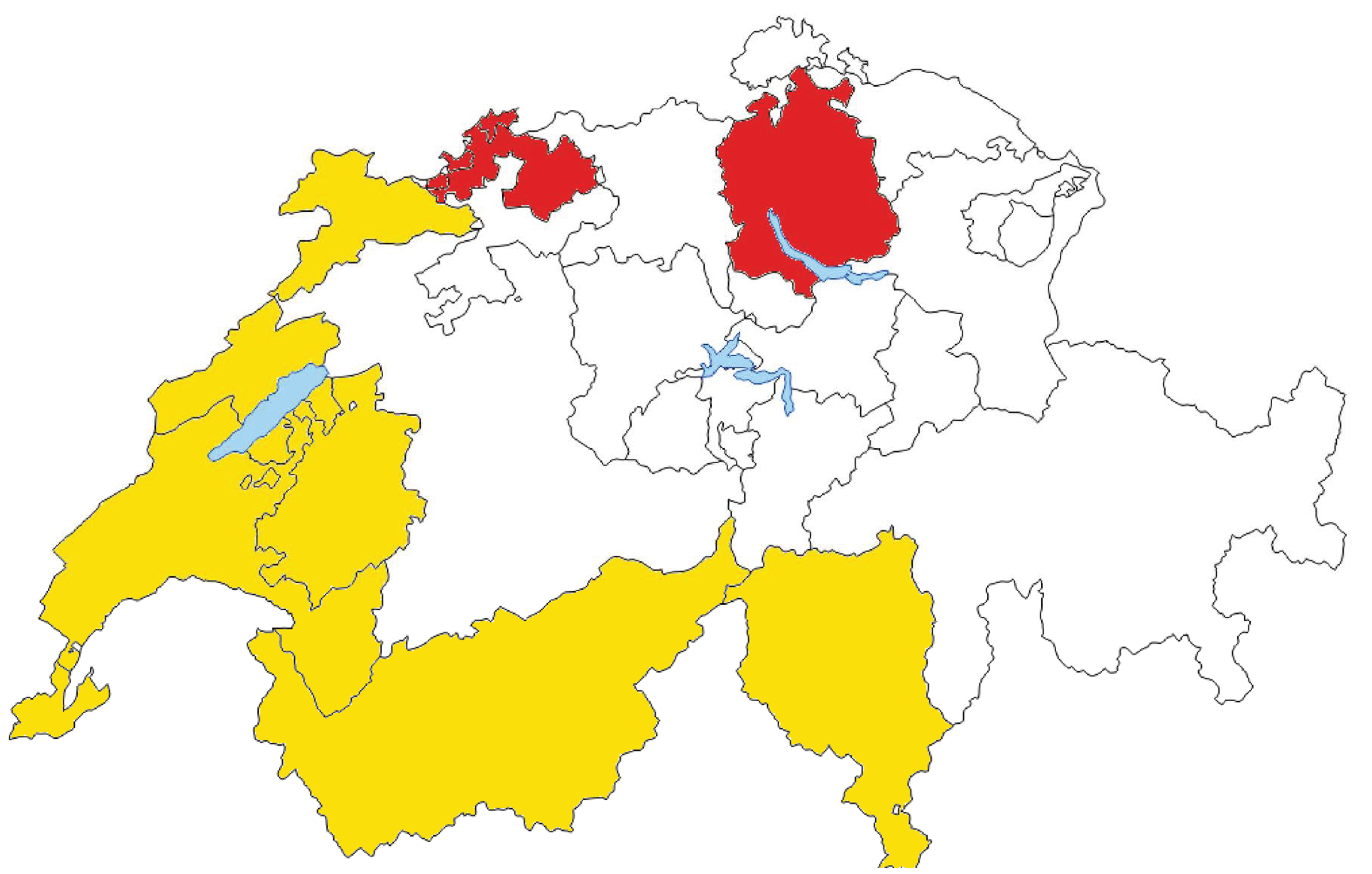
2.4. Linguistic-Geographic Region
2.5. Quality-of-Care Score
- For clinical management: method of diagnosis, time to start of treatment of <6 weeks from diagnosis, complete pathology report (pT, pN, tumor grade, ER%, and PR%);
- For locoregional treatment: negative final margins, 1 surgical procedure only, ≥10 lymph nodes removed if axillary lymph node dissection (ALND) performed, radiotherapy (RT) following breast-conserving surgery (BCS), RT boost if BCS, and RT after mastectomy when indicated;
- For systemic therapy: receipt of (neo)adjuvant chemotherapy, receipt of (neo)adjuvant anti-HER2 therapy, and prescription of endocrine therapy.
2.6. Outcome Measures
2.7. Statistical Analysis
2.8. Ethics
3. Results
3.1. Quality-of-Care Score
3.2. Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Agency for Cancer Registration. Le Cancer en Suisse—Rapport 2021. Available online: https://www.onec.ch/fr/statistiques-atlas/les-statistiques-national-sur-la-survie-au-cancer/2022 (accessed on 22 February 2022).
- DeSantis, C.E.; Ma, J.; Gaudet, M.M.; Newman, L.A.; Miller, K.D.; Goding Sauer, A.; Jemal, A.; Siegel, R.L. Breast cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 438–451. [Google Scholar] [CrossRef] [PubMed]
- Bodmer, A.; Feller, A.; Bordoni, A.; Bouchardy, C.; Dehler, S.; Ess, S.; Levi, F.; Konzelmann, I.; Rapiti, E.; Steiner, A.; et al. Breast cancer in younger women in Switzerland 1996–2009: A longitudinal population-based study. Breast 2015, 24, 112–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merlo, D.F.; Ceppi, M.; Filiberti, R.; Bocchini, V.; Znaor, A.; Gamulin, M.; Primic-Zakelj, M.; Bruzzi, P.; Bouchardy, C.; Fucic, A.; et al. Breast cancer incidence trends in European women aged 20–39 years at diagnosis. Breast Cancer Res. Treat. 2012, 134, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Cathcart-Rake, E.J.; Ruddy, K.J.; Bleyer, A.; Johnson, R.H. Breast Cancer in Adolescent and Young Adult Women Under the Age of 40 Years. JCO Oncol. Pract. 2021, 17, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Bharat, A.; Aft, R.L.; Gao, F.; Margenthaler, J.A. Patient and tumor characteristics associated with increased mortality in young women (< or =40 years) with breast cancer. J. Surg. Oncol. 2009, 100, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Partridge, A.H.; Hughes, M.E.; Warner, E.T.; Ottesen, R.A.; Wong, Y.N.; Edge, S.B.; Theriault, R.L.; Blayney, D.W.; Niland, J.C.; Winer, E.P.; et al. Subtype-Dependent Relationship Between Young Age at Diagnosis and Breast Cancer Survival. J. Clin. Oncol. 2016, 34, 3308–3314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Partridge, A.H.; Pagani, O.; Abulkhair, O.; Aebi, S.; Amant, F.; Azim, H.A., Jr.; Costa, A.; Delaloge, S.; Freilich, G.; Gentilini, O.D.; et al. First international consensus guidelines for breast cancer in young women (BCY1). Breast 2014, 23, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Paluch-Shimon, S.; Pagani, O.; Partridge, A.H.; Bar-Meir, E.; Fallowfield, L.; Fenlon, D.; Friedman, E.; Gelmon, K.; Gentilini, O.; Geraghty, J.; et al. Second international consensus guidelines for breast cancer in young women (BCY2). Breast 2016, 26, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Paluch-Shimon, S.; Pagani, O.; Partridge, A.H.; Abulkhair, O.; Cardoso, M.J.; Dent, R.A.; Gelmon, K.; Gentilini, O.; Harbeck, N.; Margulies, A.; et al. ESO-ESMO 3rd international consensus guidelines for breast cancer in young women (BCY3). Breast 2017, 35, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Paluch-Shimon, S.; Cardoso, F.; Partridge, A.H.; Abulkhair, O.; Azim, H.A., Jr.; Bianchi-Micheli, G.; Cardoso, M.J.; Curigliano, G.; Gelmon, K.A.; Harbeck, N.; et al. ESO-ESMO 4th International Consensus Guidelines for Breast Cancer in Young Women (BCY4). Ann. Oncol. 2020, 31, 674–696. [Google Scholar] [CrossRef]
- De Pietro, C.; Camenzind, P.; Sturny, I.; Crivelli, L.; Edwards-Garavoglia, S.; Spranger, A.; Wittenbecher, F.; Quentin, W. Switzerland: Health System Review. Health Syst. Transit. 2015, 17, 1–288.xix. [Google Scholar]
- Ess, S.; Savidan, A.; Frick, H.; Rageth, C.; Vlastos, G.; Lutolf, U.; Thurlimann, B. Geographic variation in breast cancer care in Switzerland. Cancer Epidemiol. 2010, 34, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Fisch, T.; Pury, P.; Probst, N.; Bordoni, A.; Bouchardy, C.; Frick, H.; Jundt, G.; De Weck, D.; Perret, E.; Lutz, J.M. Variation in survival after diagnosis of breast cancer in Switzerland. Ann. Oncol. 2005, 16, 1882–1888. [Google Scholar] [CrossRef] [PubMed]
- Bulliard, J.L.; La Vecchia, C.; Levi, F. Diverging trends in breast cancer mortality within Switzerland. Ann. Oncol. 2006, 17, 57–59. [Google Scholar] [CrossRef]
- NICER. Swiss Cancer Prevalance and Language Region. 2018. Available online: https://www.nicer.org/assets/files/publications/others/skb_01_2018_swiss_cancer_prevalence_and_language_region.pdf (accessed on 20 December 2021).
- Del Turco, M.R.; Ponti, A.; Bick, U.; Biganzoli, L.; Cserni, G.; Cutuli, B.; Decker, T.; Dietel, M.; Gentilini, O.; Kuehn, T.; et al. Quality indicators in breast cancer care. Eur. J. Cancer 2010, 46, 2344–2356. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Loibl, S.; Pagani, O.; Graziottin, A.; Panizza, P.; Martincich, L.; Gentilini, O.; Peccatori, F.; Fourquet, A.; Delaloge, S.; et al. The European Society of Breast Cancer Specialists recommendations for the management of young women with breast cancer. Eur. J. Cancer 2012, 48, 3355–3377. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Glick, J.H.; Gelber, R.D.; Coates, A.S.; Senn, H.J. Meeting highlights: International Consensus Panel on the Treatment of Primary Breast Cancer. Seventh International Conference on Adjuvant Therapy of Primary Breast Cancer. J. Clin. Oncol. 2001, 19, 3817–3827. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Wood, W.C.; Gelber, R.D.; Coates, A.S.; Thurlimann, B.; Senn, H.J. Meeting highlights: Updated international expert consensus on the primary therapy of early breast cancer. J. Clin. Oncol. 2003, 21, 3357–3365. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Glick, J.H.; Gelber, R.D.; Coates, A.S.; Thurlimann, B.; Senn, H.J.; Panel, M. Meeting highlights: International expert consensus on the primary therapy of early breast cancer 2005. Ann. Oncol. 2005, 16, 1569–1583. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Wood, W.C.; Gelber, R.D.; Coates, A.S.; Thurlimann, B.; Senn, H.J.; Members, P. Progress and promise: Highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann. Oncol. 2007, 18, 1133–1144. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Ingle, J.N.; Gelber, R.D.; Coates, A.S.; Thurlimann, B.; Senn, H.J.; Panel, M. Thresholds for therapies: Highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann. Oncol. 2009, 20, 1319–1329. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Wood, W.C.; Coates, A.S.; Gelber, R.D.; Thurlimann, B.; Senn, H.J.; Panel, M. Strategies for subtypes—Dealing with the diversity of breast cancer: Highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 2011, 22, 1736–1747. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Winer, E.P.; Coates, A.S.; Gelber, R.D.; Piccart-Gebhart, M.; Thurlimann, B.; Senn, H.J.; Panel, M. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann. Oncol. 2013, 24, 2206–2223. [Google Scholar] [CrossRef]
- Royston, P.; Parmar, M.K. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat. Med. 2002, 21, 2175–2197. [Google Scholar] [CrossRef]
- White, D.P.; Kurian, A.W.; Stevens, J.L.; Liu, B.; Brest, A.E.; Petkov, V.I. Receipt of guideline-concordant care among young adult women with breast cancer. Cancer 2021, 127, 3325–3333. [Google Scholar] [CrossRef] [PubMed]
- Wockel, A.; Kurzeder, C.; Geyer, V.; Novasphenny, I.; Wolters, R.; Wischnewsky, M.; Kreienberg, R.; Varga, D. Effects of guideline adherence in primary breast cancer—A 5-year multi-center cohort study of 3976 patients. Breast 2010, 19, 120–127. [Google Scholar] [CrossRef]
- Copson, E.R.; Maishman, T.C.; Tapper, W.J.; Cutress, R.I.; Greville-Heygate, S.; Altman, D.G.; Eccles, B.; Gerty, S.; Durcan, L.T.; Jones, L.; et al. Germline BRCA mutation and outcome in young-onset breast cancer (POSH): A prospective cohort study. Lancet Oncol. 2018, 19, 169–180. [Google Scholar] [CrossRef] [Green Version]
- Billena, C.; Wilgucki, M.; Flynn, J.; Modlin, L.; Tadros, A.; Razavi, P.; Braunstein, L.Z.; Gillespie, E.; Cahlon, O.; McCormick, B.; et al. 10-Year Breast Cancer Outcomes in Women </=35 Years of Age. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 1007–1018. [Google Scholar] [CrossRef]
- Colleoni, M.; Sun, Z.; Price, K.N.; Karlsson, P.; Forbes, J.F.; Thurlimann, B.; Gianni, L.; Castiglione, M.; Gelber, R.D.; Coates, A.S.; et al. Annual Hazard Rates of Recurrence for Breast Cancer During 24 Years of Follow-Up: Results From the International Breast Cancer Study Group Trials I to V. J. Clin. Oncol. 2016, 34, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Ruddy, K.J.; Gelber, S.; Tamimi, R.M.; Schapira, L.; Come, S.E.; Meyer, M.E.; Winer, E.P.; Partridge, A.H. Breast cancer presentation and diagnostic delays in young women. Cancer 2014, 120, 20–25. [Google Scholar] [CrossRef]
- Montagna, G.; Schneeberger, A.R.; Rossi, L.; Bianchi Micheli, G.; Meani, F.; Imperiali, M.; Spitale, A.; Pagani, O. Can we make a portrait of women with inoperable locally advanced breast cancer? Breast 2017, 33, 83–90. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total n = 2477 | Latin n = 1469 | German n = 1008 | p-Value |
|---|---|---|---|---|
| Median, years (IQR) | 37.3 (34.0–39.4) | 37.3 (34.1–39.4) | 37.3 (33.9–39.5) | 0.880 |
| Age, n (%) | 0.811 | |||
| <25 | 22 (0.9) | 15 (1.0) | 7 (0.7) | |
| 25–29 | 160 (6.5) | 93 (6.3) | 67 (6.6) | |
| 30–34 | 584 (23.6) | 338 (23.0) | 246 (24.4) | |
| 35–40 | 1709 (69) | 1021 (69.6) | 688 (68.3) | |
| Unknown | 2 | 2 | 0 | |
| Period of Diagnosis | 0.006 | |||
| 2000–2004 | 731 (29.5) | 409 (27.9) | 322 (31.9) | |
| 2005–2009 | 864 (34.9) | 500 (34.1) | 364 (36.1) | |
| 2010–2014 | 880 (35.6) | 558 (38.0) | 322 (31.9) | |
| Missing | 2 | 2 | 0 | |
| Stage | 0.013 | |||
| I | 789 (34.1) | 507 (36.5) | 282 (30.5) | |
| II | 1165 (50.3) | 673 (48.3) | 492 (53.2) | |
| III | 362 (15.6) | 212 (15.2) | 150 (16.2) | |
| Unknown | 161 | 77 | 84 | |
| Tumor differentiation | <0.0001 | |||
| Well | 207 (8.7) | 143 (10.1) | 64 (6.5) | |
| Moderately | 1019 (42.6) | 630 (44.6) | 389 (39.7) | |
| Poorly | 1166 (48.7) | 639 (45.3) | 527 (53.8) | |
| Unknown | 85 | 57 | 28 | |
| Tumor subtype | 0.034 | |||
| Triple negative | 432 (20.3) | 244 (19.1) | 188 (22.0) | |
| HER2+ | 150 (7.0) | 86 (6.7) | 64 (7.5) | |
| Luminal B-like | 1019 (47.8) | 644 (50.4) | 375 (43.9) | |
| Luminal A-like | 531 (24.9) | 304 (23.8) | 227 (26.6) | |
| Unknown * | 345 | 191 | 154 | |
| Family history | 0.005 | |||
| Negative | 1058 (60.2) | 768 (62.3) | 290 (55.1) | |
| Positive ** | 700 (39.8) | 464 (37.7) | 236 (44.9) | |
| Unknown | 719 | 237 | 482 | |
| Treatment setting | <0.0001 | |||
| Public | 1238 (69.4) | 809 (68.0) | 429 (72.2) | |
| Private | 546 (30.6) | 381 (32.0) | 165 (27.8) | |
| Unknown | 693 | 279 | 414 | |
| Clinical Management | Latin Region (n = 1469) | German Region (n = 1008) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| 1 Point n (%) | No Point n (%) | Missing n | 1 Point n (%) | No Point n (%) | Missing n | ||
| Pretreatment diagnostic biopsy/FNA (n = 2477) | 1464 (99.9) | 1 (0.1) | 4 | 1008 (100) | - | - | 0.407 |
| Time to start of treatment <6 weeks (n = 2477) | 1289 (93.5) | 89 (6.5) | 91 | 931 (95.9) | 40 (4.1) | 37 | 0.014 |
| Pathology report indicating ER%, PR%, tumor size and tumor differentiation (n = 2477) | 1330 (90.5) All features present | 139 (9.5) 1–3 features missing | - | 927 (92.0) All features present | 81 (8.0) 1–3 features missing | - | 0.220 |
| Locoregional therapy | |||||||
| “No ink on tumor” on final margin (n = 2477) | 1042 (80.3) | 256 (19.7) | 171 | 772 (84.5) | 142 (15.5) | 94 | 0.012 |
| Only 1 surgical procedure (n = 2477) | 1004 (70.9) | 412 (29.1) | 53 | 716 (72.5) | 271 (27.5) | 21 | 0.381 |
| Removal of > 10 LN when undergoing ALND (n = 1507) Not applicable (n = 771) Missing (n = 199) | 689 (75.8) | 220 (24.2) | 8 | 485 (82.5) | 103 (17.5) | 2 | 0.002 |
| RT following BCS (n = 1430) Not applicable (n = 974) Missing (n = 73) | 739 (92.5) | 60 (7.5) | - | 473 (75.0) | 158 (25.0) | - | <0.0001 |
| RT boost on tumor bed if BCS (n = 1430) Not applicable (n = 974) Missing (n = 73) | 659 (95.8) | 29 (4.2) | 111 | 318 (88.6) | 41 (11.4) | 272 | <0.0001 |
| Post Mastectomy RT (n = 343) Not applicable (n = 2049) Missing (n = 85) | 140 (68.6) | 64 (31.4) | - | 97 (69.8) | 42 (30.2) | - | 0.820 |
| Systemic therapy | |||||||
| Adjuvant chemotherapy if appropriate (n = 1190) Not applicable (n = 1004) Missing (n = 283) | 648 (92.8) | 50 (7.2) | - | 364 (74.0) | 128 (26.0) | - | <0.0001 |
| Adjuvant anti-HER2 therapy if HER2+ (n = 571) Not applicable (n = 1675) Missing (n = 231) | 220 (96.1) | 9 (3.9) | 130 | 107 (89.2) | 13 (10.8) | 92 | 0.012 |
| Endocrine therapy prescribed (n = 1670) Not applicable (n = 707) Missing (n = 100) | 855 (84.5) | 157 (15.5) | - | 431 (65.5) | 227 (34.5) | - | <0.0001 |
| Score | Latin Region | German Region | ||
|---|---|---|---|---|
| n = 1469 | % | n = 1008 | % | |
| 100% | 554 | 37.71% | 334 | 18.65% |
| 89–99% | 194 | 13.21% | 92 | 9.13% |
| 79–88% | 322 | 21.92% | 213 | 21.13% |
| 68–78% | 191 | 13.00% | 181 | 17.96% |
| <67% | 208 | 14.16% | 188 | 18.65% |
| Univariable | Multivariable * | |||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p | Hazard Ratio (95% CI) | p | |
| Linguistic-geographic region | ||||
| German region | Ref | Ref | ||
| Latin region | 0.72 (0.59–0.89) | 0.003 | 0.84 (0.68–1.03) | 0.097 |
| Age group | ||||
| ≤35 | Ref | Ref | ||
| >35 | 0.79 (0.63–0.98) | 0.031 | 0.87 (0.7–1.09) | 0.228 |
| Quality-of-care score | ||||
| 1st tertile | Ref | |||
| 2nd tertile | 0.84 (0.61–1.16) | 0.280 | ||
| 3rd tertile | 0.94 (0.70–1.26) | 0.670 | ||
| 100% | 0.83 (0.64–1.08) | 0.168 | ||
| Period of diagnosis | ||||
| 2000–2004 | Ref | Ref | ||
| 2005–2009 | 0.68 (0.54–0.87) | 0.002 | 0.59 (0.46–0.76) | <0.0001 |
| 2010–2014 | 0.66 (0.48–0.89) | 0.008 | 0.59 (0.43–0.81) | 0.001 |
| Tumor differentiation | ||||
| Well | Ref | Ref | ||
| Moderately | 3.11 (1.58–6.12) | <0.0001 | 2.36 (1.19–4.67) | 0.014 |
| Poorly | 5.22 (2.68–10.17) | <0.0001 | 3.20 (1.59–6.42) | 0.001 |
| Missing | 4.72 (2.09–10.69) | <0.0001 | 2.90 (1.24–6.76) | 0.014 |
| Tumor stage | ||||
| I | Ref | Ref | ||
| II | 2.75 (1.97–3.83) | <0.0001 | 2.42 (1.73–3.38) | <0.0001 |
| III | 6.34 (4.46–9.02) | <0.0001 | 5.55 (3.98–7.93) | <0.0001 |
| Missing | 4.91 (3.18–7.58) | <0.0001 | 4.32 (2.77–6.75) | <0.0001 |
| Tumor subtype | ||||
| Triple negative | Ref | |||
| Luminal A like | 0.41 (0.28–0.58) | <0.0001 | 0.62 (0.41–0.95) | 0.028 |
| Luminal B like | 0.77 (0.59–1.02) | 0.067 | 0.83 (0.63–1.11) | 0.213 |
| HER2+ | 1.12 (0.73–1.73) | 0.598 | 0.95 (0.61–1.47) | 0.810 |
| Unknown | 0.67 (0.48–0.94) | 0.019 | 0.66 (0.46–0.96) | 0.031 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montagna, G.; Schaffar, R.; Bordoni, A.; Spitale, A.; Terribile, D.A.; Rossi, L.; Bergeron, Y.; van der Linden, B.W.A.; Konzelmann, I.; Rohrmann, S.; et al. Management and Outcome of Young Women (≤40 Years) with Breast Cancer in Switzerland. Cancers 2022, 14, 1328. https://doi.org/10.3390/cancers14051328
Montagna G, Schaffar R, Bordoni A, Spitale A, Terribile DA, Rossi L, Bergeron Y, van der Linden BWA, Konzelmann I, Rohrmann S, et al. Management and Outcome of Young Women (≤40 Years) with Breast Cancer in Switzerland. Cancers. 2022; 14(5):1328. https://doi.org/10.3390/cancers14051328
Chicago/Turabian StyleMontagna, Giacomo, Robin Schaffar, Andrea Bordoni, Alessandra Spitale, Daniela A. Terribile, Lorenzo Rossi, Yvan Bergeron, Bernadette W. A. van der Linden, Isabelle Konzelmann, Sabine Rohrmann, and et al. 2022. "Management and Outcome of Young Women (≤40 Years) with Breast Cancer in Switzerland" Cancers 14, no. 5: 1328. https://doi.org/10.3390/cancers14051328






