Contribution of the Skin–Gut Axis to Immune-Related Adverse Events with Multi-System Involvement
Abstract
:Simple Summary
Abstract
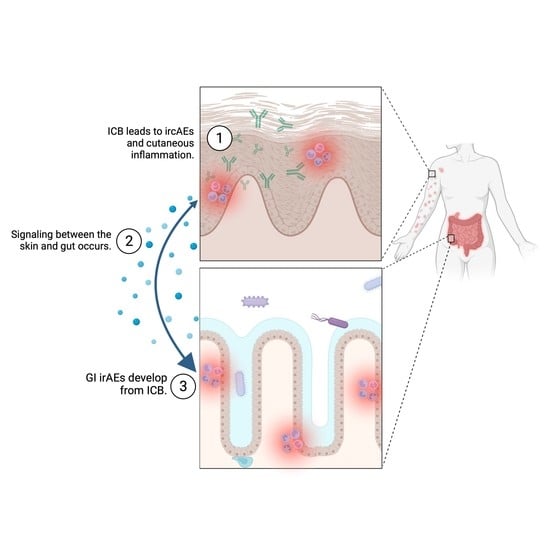
1. Introduction
2. Patients and Methods
3. Results
3.1. Cohort 1
3.2. Cohort 2
3.3. Patients with Both ircAEs and GI irAEs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barrios, D.M.; Do, M.H.; Phillips, G.S.; Postow, M.A.; Akaike, T.; Nghiem, P.; Lacouture, M.E. Immune checkpoint inhibitors to treat cutaneous malignancies. J. Am. Acad. Dermatol. 2020, 83, 1239–1253. [Google Scholar] [CrossRef] [PubMed]
- Ascierto, P.A.; McArthur, G.A. Checkpoint inhibitors in melanoma and early phase development in solid tumors: What’s the future? J. Transl. Med. 2017, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Seo, H.K. Immune checkpoint inhibitors for urothelial carcinoma. Investig. Clin. Urol. 2018, 59, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Memon, H.; Patel, B.M. Immune checkpoint inhibitors in non-small cell lung cancer: A bird’s eye view. Life Sci. 2019, 233, 116713. [Google Scholar] [CrossRef]
- Postow, M.A.; Sidlow, R.; Hellmann, M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018, 378, 158–168. [Google Scholar] [CrossRef]
- Foster, C.C.; Couey, M.A.; Ba, S.E.K.; Khattri, A.; Ms, R.K.A.; Tan, Y.C.; Brisson, R.J.; Leidner, R.S.; Seiwert, T.Y. Immune-related adverse events are associated with improved response, progression-free survival, and overall survival for patients with head and neck cancer receiving immune checkpoint inhibitors. Cancer 2021, 127, 4565–4573. [Google Scholar] [CrossRef]
- Tang, K.; Seo, J.; Tiu, B.C.; Le, T.K.; Pahalyants, V.; Raval, N.S.; Ugwu-Dike, P.O.; Zubiri, L.; Naranbhai, V.; Carrington, M.; et al. Association of Cutaneous Immune-Related Adverse Events With Increased Survival in Patients Treated With Anti–Programmed Cell Death 1 and Anti–Programmed Cell Death Ligand 1 Therapy. JAMA Dermatol. 2022, 158, 189. [Google Scholar] [CrossRef]
- Muntyanu, A.; Netchiporouk, E.; Gerstein, W.; Gniadecki, R.; Litvinov, I.V. Cutaneous Immune-Related Adverse Events (irAEs) to Immune Checkpoint Inhibitors: A Dermatology Perspective on Management. J. Cutan. Med. Surg. 2020, 25, 59–76. [Google Scholar] [CrossRef]
- Collins, L.K.; Chapman, M.S.; Carter, J.B.; Samie, F.H. Cutaneous adverse effects of the immune checkpoint inhibitors. Curr. Probl. Cancer 2017, 41, 125–128. [Google Scholar] [CrossRef]
- Geisler, A.N.; Phillips, G.S.; Barrios, D.M.; Wu, J.; Leung, D.Y.M.; Moy, A.P.; Kern, J.A.; Lacouture, M.E. Immune checkpoint inhibitor–related dermatologic adverse events. J. Am. Acad. Dermatol. 2020, 83, 1255–1268. [Google Scholar] [CrossRef]
- Wang, E.; Kraehenbuehl, L.; Ketosugbo, K.; Kern, J.A.; Lacouture, M.E.; Leung, D.Y. Immune-related cutaneous adverse events due to checkpoint inhibitors. Ann. Allergy Asthma Immunol. 2021, 126, 613–622. [Google Scholar] [CrossRef]
- O’Reilly, A.; Hughes, P.; Mann, J.; Lai, Z.; Teh, J.J.; Mclean, E.; Edmonds, K.; Lingard, K.; Chauhan, D.; Lynch, J.; et al. An immunotherapy survivor population: Health-related quality of life and toxicity in patients with metastatic melanoma treated with immune checkpoint inhibitors. Support. Care Cancer 2019, 28, 561–570. [Google Scholar] [CrossRef] [Green Version]
- Lacouture, M.; Sibaud, V. Toxic Side Effects of Targeted Therapies and Immunotherapies Affecting the Skin, Oral Mucosa, Hair, and Nails. Am. J. Clin. Dermatol. 2018, 19, 31–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sznol, M.; Ferrucci, P.F.; Hogg, D.; Atkins, M.B.; Wolter, P.; Guidoboni, M.; Lebbé, C.; Kirkwood, J.M.; Schachter, J.; Daniels, G.A.; et al. Pooled Analysis Safety Profile of Nivolumab and Ipilimumab Combination Therapy in Patients With Advanced Melanoma. J. Clin. Oncol. 2017, 35, 3815–3822. [Google Scholar] [CrossRef] [Green Version]
- Kröner, P.T.; Mody, K.; Farraye, F.A. Immune checkpoint inhibitor–related luminal GI adverse events. Gastrointest. Endosc. 2019, 90, 881–892. [Google Scholar] [CrossRef]
- Soularue, E.; Lepage, P.; Colombel, J.F.; Coutzac, C.; Faleck, D.; Marthey, L.; Collins, M.; Chaput, N.; Robert, C.; Carbonnel, F. Enterocolitis due to immune checkpoint inhibitors: A systematic review. Gut 2018, 67, 2056–2067. [Google Scholar] [CrossRef]
- Michot, J.; Bigenwald, C.; Champiat, S.; Collins, M.; Carbonnel, F.; Postel-Vinay, S.; Berdelou, A.; Varga, A.; Bahleda, R.; Hollebecque, A.; et al. Immune-related adverse events with immune checkpoint blockade: A comprehensive review. Eur. J. Cancer 2016, 54, 139–148. [Google Scholar] [CrossRef]
- Yanai, S.; Toya, Y.; Sugai, T.; Matsumoto, T. Gastrointestinal Adverse Events Induced by Immune-Checkpoint Inhibitors. Digestion 2021, 102, 965–973. [Google Scholar] [CrossRef]
- Molina, G.E.; Allen, I.M.; Hughes, M.S.; Zubiri, L.; Lee, H.; Mooradian, M.J.; Reynolds, K.L.; Dougan, M.; Chen, S.T. Prognostic implications of co-occurring dermatologic and gastrointestinal toxicity from immune checkpoint inhibition therapy for advanced malignancies: A retrospective cohort study. J. Am. Acad. Dermatol. 2019, 82, 743–746. [Google Scholar] [CrossRef] [Green Version]
- Thompson, L.L.; Krasnow, N.A.; Chang, M.S.; Yoon, J.; Li, E.B.; Polyakov, N.J.; Molina, G.E.; Said, J.T.; Huang, K.; Kuchroo, J.R.; et al. Patterns of Cutaneous and Noncutaneous Immune-Related Adverse Events Among Patients With Advanced Cancer. JAMA Dermatol. 2021, 157, 577. [Google Scholar] [CrossRef]
- Weber, J.S.; Hodi, F.S.; Wolchok, J.D.; Topalian, S.L.; Schadendorf, D.; Larkin, J.; Sznol, M.; Long, G.; Li, H.; Waxman, I.M.; et al. Safety Profile of Nivolumab Monotherapy: A Pooled Analysis of Patients With Advanced Melanoma. J. Clin. Oncol. 2017, 35, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Carbone, D.P.; Reck, M.; Paz-Ares, L.; Creelan, B.; Horn, L.; Steins, M.; Felip, E.; van den Heuvel, M.M.; Ciuleanu, T.-E.; Badin, F.; et al. First-Line Nivolumab in Stage IV or Recurrent Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 376, 2415–2426. [Google Scholar] [CrossRef] [PubMed]
- Garon, E.B.; Rizvi, N.A.; Hui, R.; Leighl, N.; Balmanoukian, A.S.; Eder, J.P.; Patnaik, A.; Aggarwal, C.; Gubens, M.; Horn, L.; et al. Pembrolizumab for the Treatment of Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 372, 2018–2028. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, M.D.; Paz-Ares, L.; Bernabe Caro, R.; Zurawski, B.; Kim, S.-W.; Carcereny Costa, E.; Park, K.; Alexandru, A.; Lupinacci, L.; de la Mora Jimenez, E.; et al. Nivolumab plus Ipilimumab in Advanced Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2019, 381, 2020–2031. [Google Scholar] [CrossRef]
- Togashi, Y.; Shitara, K.; Nishikawa, H. Regulatory T cells in cancer immunosuppression — implications for anticancer therapy. Nat. Rev. Clin. Oncol. 2019, 16, 356–371. [Google Scholar] [CrossRef]
- Repnik, K.; Potočnik, U. CTLA4 CT60 Single-Nucleotide Polymorphism Is Associated with Slovenian Inflammatory Bowel Disease Patients and Regulates Expression of CTLA4 Isoforms. DNA Cell Biol. 2010, 29, 603–610. [Google Scholar] [CrossRef]
- Zhao, J.-J.; Wang, D.; Yao, H.; Sun, D.-W.; Li, H.-Y. CTLA-4andMDR1polymorphisms increase the risk for ulcerative colitis: A meta-analysis. World J. Gastroenterol. 2015, 21, 10025–10040. [Google Scholar] [CrossRef]
- Anderson, R.; Rapoport, B.L. Immune Dysregulation in Cancer Patients Undergoing Immune Checkpoint Inhibitor Treatment and Potential Predictive Strategies for Future Clinical Practice. Front. Oncol. 2018, 8, 80. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Yao, Z.; Zhou, X.; Zhang, W.; Zhang, X.; Zhang, F. Immune-related adverse events of checkpoint inhibitors: Insights into immunological dysregulation. Clin. Immunol. 2020, 213, 108377. [Google Scholar] [CrossRef]
- Quach, H.T.; Johnson, D.B.; LeBoeuf, N.R.; Zwerner, J.P.; Dewan, A.K. Cutaneous adverse events caused by immune checkpoint inhibitors. J. Am. Acad. Dermatol. 2021, 85, 956–966. [Google Scholar] [CrossRef]
- Kumagai, S.; Togashi, Y.; Kamada, T.; Sugiyama, E.; Nishinakamura, H.; Takeuchi, Y.; Vitaly, K.; Itahashi, K.; Maeda, Y.; Matsui, S.; et al. The PD-1 expression balance between effector and regulatory T cells predicts the clinical efficacy of PD-1 blockade therapies. Nat. Immunol. 2020, 21, 1346–1358. [Google Scholar] [CrossRef]
- Gallo, R.L.; Hooper, L.V. Epithelial antimicrobial defence of the skin and intestine. Nat. Rev. Immunol. 2012, 12, 503–516. [Google Scholar] [CrossRef] [Green Version]
- Ghevariya, V.; Singhal, S.; Anand, S. The skin: A mirror to the gut. Int. J. Color. Dis. 2013, 28, 889–913. [Google Scholar] [CrossRef]
- Salem, I.; Ramser, A.; Isham, N.; Ghannoum, M.A. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front. Microbiol. 2018, 9, 1459. [Google Scholar] [CrossRef] [Green Version]
- Arck, P.; Handjiski, B.; Hagen, E.; Pincus, M.; Bruenahl, C.; Bienenstock, J.; Paus, R. Is there a ‘gut-brain-skin axis’? Exp. Dermatol. 2010, 19, 401–405. [Google Scholar] [CrossRef]
- De Pessemier, B.; Grine, L.; Debaere, M.; Maes, A.; Paetzold, B.; Callewaert, C. Gut–Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms 2021, 9, 353. [Google Scholar] [CrossRef]
- Mager, L.F.; Burkhard, R.; Pett, N.; Cooke, N.C.A.; Brown, K.; Ramay, H.; Paik, S.; Stagg, J.; Groves, R.A.; Gallo, M.; et al. Microbiome-derived inosine modulates response to checkpoint inhibitor immunotherapy. Science 2020, 369, 1481–1489. [Google Scholar] [CrossRef]
- Dokoshi, T.; Seidman, J.S.; Cavagnero, K.J.; Li, F.; Liggins, M.C.; Taylor, B.C.; Olvera, J.; Knight, R.; Chang, J.T.; Salzman, N.H.; et al. Skin inflammation activates intestinal stromal fibroblasts and promotes colitis. J. Clin. Investig. 2021, 131, e147614. [Google Scholar] [CrossRef]
- Juzot, C.; Sibaud, V.; Amatore, F.; Mansard, S.; Seta, V.; Jeudy, G.; Pham-Ledard, A.; Benzaquen, M.; Peuvrel, L.; Le Corre, Y.; et al. Clinical, biological and histological characteristics of bullous pemphigoid associated with anti-PD-1/PD-L1 therapy: A national retrospective study. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e511–e514. [Google Scholar] [CrossRef]
- Siegel, J.; Totonchy, M.; Damsky, W.; Berk-Krauss, J.; Castiglione, F.; Sznol, M.; Petrylak, D.P.; Fischbach, N.; Goldberg, S.B.; Decker, R.H.; et al. Bullous disorders associated with anti–PD-1 and anti–PD-L1 therapy: A retrospective analysis evaluating the clinical and histopathologic features, frequency, and impact on cancer therapy. J. Am. Acad. Dermatol. 2018, 79, 1081–1088. [Google Scholar] [CrossRef]
- Ba, A.T.L.; Khanna, T.; Antonov, N.; Audrey-Bayan, C.; Geskin, L. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int. J. Dermatol. 2018, 57, 664–669. [Google Scholar] [CrossRef]
- Phillips, G.S.; Wu, J.; Hellmann, M.D.; Postow, M.A.; Rizvi, N.A.; Freites-Martinez, A.; Chan, D.; Dusza, S.; Motzer, R.J.; Rosenberg, J.E.; et al. Treatment Outcomes of Immune-Related Cutaneous Adverse Events. J. Clin. Oncol. 2019, 37, 2746–2758. [Google Scholar] [CrossRef]
- Apalla, Z.; Nikolaou, V.; Fattore, D.; Fabbrocini, G.; Freites-Martinez, A.; Sollena, P.; Lacouture, M.; Kraehenbuehl, L.; Stratigos, A.; Peris, K.; et al. European recommendations for management of immune checkpoint inhibitors-derived dermatologic adverse events. The EADV task force ‘Dermatology for cancer patients’ position statement. J. Eur. Acad. Dermatol. Venereol. 2021, 36, 332–350. [Google Scholar] [CrossRef]
- Bellaguarda, E.; Hanauer, S. Checkpoint Inhibitor–Induced Colitis. Am. J. Gastroenterol. 2020, 115, 202–210. [Google Scholar] [CrossRef]
- Darnell, E.P.; Mooradian, M.J.; Baruch, E.N.; Yilmaz, M.; Reynolds, K.L. Immune-Related Adverse Events (irAEs): Diagnosis, Management, and Clinical Pearls. Curr. Oncol. Rep. 2020, 22, 1–11. [Google Scholar] [CrossRef]
- Friedman, C.; Proverbs-Singh, T.A.; Postow, M.A. Treatment of the Immune-Related Adverse Effects of Immune Checkpoint Inhibitors. JAMA Oncol. 2016, 2, 1346–1353. [Google Scholar] [CrossRef]
- Luo, J.; Beattie, J.A.; Fuentes, P.; Rizvi, H.; Egger, J.V.; Kern, J.A.; Leung, D.Y.; Lacouture, M.E.; Kris, M.G.; Gambarin, M.; et al. Beyond Steroids: Immunosuppressants in Steroid-Refractory or Resistant Immune-Related Adverse Events. J. Thorac. Oncol. 2021, 16, 1759–1764. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Management of Immunotherapy-Associated Toxicities Version 3.2021; National Comprehensive Cancer Network: Plymouth Meeting, PA, USA, 2021. [Google Scholar]




| Variables | Cohort 1 (n = 152) | Cohort 2 (n = 246) | p-Value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Age (mean) | 64.3 | 62.4 | p = 0.255 | |||
| Sex | Female | 59 | 38.8 | 97 | 39.4 | p = 0.903 |
| Male | 93 | 61.2 | 149 | 60.6 | ||
| Race | Asian | 11 | 7.2 | 10 | 4.1 | p = 0.150 |
| Black | 4 | 2.6 | 2 | 0.8 | ||
| Native American | 2 | 1.3 | 0 | 0 | ||
| White | 126 | 82.9 | 221 | 89.8 | ||
| Other | 4 | 2.6 | 4 | 1.7 | ||
| N/A | 5 | 3.3 | 9 | 3.7 | ||
| Ethnicity | Hispanic | 9 | 5.9 | 13 | 5.3 | p = 0.963 |
| Not Hispanic | 137 | 90.1 | 223 | 90.7 | ||
| N/A | 6 | 4.0 | 10 | 4.1 | ||
| Tumor Type | Breast | 1 | 0.7 | 2 | 0.8 | p < 0.001 |
| Cervical | 2 | 1.3 | 2 | 0.8 | ||
| CNS | 3 | 2.0 | 5 | 2.03 | ||
| Colorectal | 5 | 3.3 | 3 | 1.2 | ||
| Endometrial | 10 | 6.6 | 3 | 1.2 | ||
| Gastrointestinal/Hepatobiliary | 9 | 5.9 | 30 | 12.2 | ||
| Genitourinary | 47 | 30.9 | 39 | 15.9 | ||
| Head and Neck/ Endocrine | 4 | 2.6 | 9 | 3.7 | ||
| Hematologic | 0 | 0.0 | 8 | 3.3 | ||
| Lung | 31 | 20.1 | 46 | 18.7 | ||
| Melanoma | 25 | 16.5 | 76 | 30.9 | ||
| Merkel Cell Carcinoma | 4 | 2.6 | 4 | 1.6 | ||
| Ovarian | 2 | 1.3 | 4 | 1.6 | ||
| Prostate | 3 | 2.0 | 14 | 5.7 | ||
| Sarcoma | 6 | 4.0 | 1 | 0.4 | ||
| ICB Type | Atezolizumab (anti-PDL1) | 11 | 7.2 | 9 | 3.7 | p < 0.001 |
| Avelumab (anti-PDL1) | 8 | 5.3 | 2 | 0.8 | ||
| Cemiplimab (anti-PD1) | 0 | 0.0 | 1 | 0.4 | ||
| Durvalumab (anti-PDL1) | 7 | 4.6 | 7 | 2.9 | ||
| Durvalumab (anti-PDL1)/ Tremelimumab (anti-CTLA4) | 0 | 0.0 | 7 | 2.9 | ||
| Ipilimumab (anti-CTLA4) | 0 | 0.0 | 35 | 14.2 | ||
| Ipilimumab (anti-CTLA4)/ Nivolumab (anti-PD1) | 38 | 25.0 | 71 | 28.9 | ||
| Nivolumab (anti-PD1) | 30 | 19.7 | 35 | 14.2 | ||
| Pembrolizumab (anti-PD1) | 58 | 38.2 | 76 | 30.9 | ||
| Tremelimumab (anti-CTLA4) | 0 | 0.0 | 2 | 0.8 | ||
| Variable | Developed Only ircAEs | Developed ircAEs + GI irAEs | p-Value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| All Patients with ircAE | 126 | 82.9 | 26 | 17.1 | ||
| ircAE Phenotype | Bullous | 4 | 80.0 | 1 | 20.0 | p = 0.768 |
| Eczema | 6 | 100.0 | 0 | 0.0 | ||
| Lichenoid | 2 | 100.0 | 0 | 0.0 | ||
| Maculopapular | 26 | 83.9 | 5 | 16.1 | ||
| Pruritus | 64 | 79.0 | 17 | 21.0 | ||
| Psoriasis | 5 | 100.0 | 0 | 0.0 | ||
| Urticaria | 10 | 90.9 | 1 | 9.1 | ||
| Vitiligo | 9 | 81.8 | 2 | 18.2 | ||
| ircAE Grade | 1 | 76 | 81.7 | 17 | 18.3 | p = 0.106 |
| 2 | 43 | 89.6 | 5 | 10.4 | ||
| 3 | 7 | 63.6 | 4 | 36.4 | ||
| ICB Target | Anti-PD1/PDL1 | 96 | 84.2 | 18 | 15.8 | p = 0.456 |
| Anti-CTLA4 + Anti-PD1 | 30 | 79.0 | 8 | 21.1 | ||
| ICB Antibody | Atezolizumab | 9 | 81.8 | 2 | 18.2 | p = 0.121 |
| Avelumab | 4 | 50.0 | 4 | 50.0 | ||
| Durvalumab | 7 | 100.0 | 0 | 0.0 | ||
| Nivolumab | 26 | 86.7 | 4 | 13.3 | ||
| Pembrolizumab | 50 | 86.2 | 8 | 13.8 | ||
| Ipilimumab/ Nivolumab | 30 | 79.0 | 8 | 21.1 | ||
| Best Response to ICB | Complete Response | 7 | 77.8 | 2 | 22.2 | p = 0.880 |
| Partial Response | 30 | 85.7 | 5 | 14.3 | ||
| POD | 29 | 85.3 | 5 | 14.7 | ||
| Stable | 60 | 81.1 | 14 | 18.9 | ||
| Patients with Both irColitis and ircAE | n | % | p-value | |||
| GI irAE Grade | 1 | 15 | 57.7 | - | ||
| 2 | 9 | 34.6 | ||||
| 3 | 2 | 7.7 | ||||
| Relationship to ircAE | GI irAE Before ircAE | 8 | 30.8 | p = 0.014 | ||
| GI irAE After ircAE | 18 | 69.2 | ||||
| Variable | Developed only irColitis | Developed irColitis + ircAEs | p-Value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| All Patients with Biopsy-Proven Colitis | 211 | 85.8 | 35 | 14.2 | p = 0.010 | |
| ICB Target | Anti-PD-1/PD-L1 | 114 | 87.7 | 16 | 12.3 | |
| Anti-CTLA4 | 36 | 97.3 | 1 | 2.7 | ||
| Anti-PD-1/PD-L1 + Anti-CTLA4 | 61 | 77.2 | 18 | 22.8 | ||
| ICB Antibody | Atezolizumab | 9 | 100.0 | 0 | 0.0 | p = 0.125 |
| Avelumab | 1 | 50.0 | 1 | 50.0 | ||
| Cemiplimab | 1 | 100.0 | 0 | 0.0 | ||
| Durvalumab | 6 | 87.7 | 1 | 14.3 | ||
| Nivolumab | 32 | 91.4 | 3 | 8.6 | ||
| Pembrolizumab | 65 | 85.5 | 11 | 14.5 | ||
| Ipilimumab | 34 | 97.1 | 1 | 2.9 | ||
| Tremelimumab | 2 | 100.0 | 0 | 0.0 | ||
| Ipilimumab/ Nivolumab | 55 | 76.4 | 17 | 23.6 | ||
| Tremelimumab/ Durvalumab | 6 | 85.7 | 1 | 14.3 | ||
| Patients with Biopsy-Proven irColitis AND ircAE | n | % | p-Value | |||
| ircAE Phenotype | Lichenoid | 4 | 11.4 | - | ||
| Maculopapular | 13 | 37.1 | - | |||
| Pruritus | 5 | 14.3 | - | |||
| Psoriasis | 1 | 2.9 | - | |||
| Urticaria | 4 | 11.4 | - | |||
| Vitiligo | 2 | 5.7 | - | |||
| Other | 6 | 17.1 | - | |||
| ircAE and GI irAE Relationship | ircAE Before irColitis | 26 | 74.3 | p = 0.0001 | ||
| irColitis Before ircAE | 9 | 25.7 | ||||
| ircAE Grade | General Recommendations | Phenotype-Specific Recommendations |
|---|---|---|
| 1 | Start moderate- to high-potency topical corticosteroids Continue ICB | - |
| 2 | Consider adding systemic corticosteroids (prednisone 0.5–1 mg/kg daily) Continue ICB | Psoriasiform rash: Consider narrow-band UVB phototherapy or apremilast Pruritus: Consider GABA analogs Bullous Pemphigoid: Hold ICB until grade 0 or 1 |
| 3+ | Start systemic corticosteroids (prednisone 0.5–2 mg/kg daily) Hold ICB until grades 0–1 | Maculopapular or lichenoid rash: Consider infliximab or tocilizumab Psoriasiform rash: Consider ustekinumab, guselkumab, infliximab, adalimumab, apremilast, or retinoids Pruritus: Consider GABA analogs, omalizumab, or dupilumab Bullous Pemphigoid: Consider rituximab SJS/TEN: Hospitalization |
| Step | General Recommendations | Specific Recommendations |
|---|---|---|
| 1 | Supportive treatment Continue ICB | Diarrhea: Loperamide, hydration, dietary modifications |
| 2–3 | Early endoscopic evaluation Administer systemic corticosteroids (prednisone 1–2 mg/kg daily) Hold ICB | Systemic symptoms (fever, tachycardia, etc.): Hospitalization Steroid-refractory cases: Consider biologics such as infliximab or vedolizumab Biologics-refractory cases: Consider stool transplant |
| 4 | Hospitalization Intravenous corticosteroids (methylprednisolone 1–2 mg/kg daily) Permanently discontinue ICB | Systemic symptoms (fever, tachycardia, etc.): Hospitalization Steroid-refractory cases: Consider biologics such as infliximab or vedolizumab Biologics-refractory cases: Consider stool transplant |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, A.M.; Kraehenbuehl, L.; King, S.; Leung, D.Y.M.; Goleva, E.; Moy, A.P.; Lacouture, M.E.; Shah, N.J.; Faleck, D.M. Contribution of the Skin–Gut Axis to Immune-Related Adverse Events with Multi-System Involvement. Cancers 2022, 14, 2995. https://doi.org/10.3390/cancers14122995
Kuo AM, Kraehenbuehl L, King S, Leung DYM, Goleva E, Moy AP, Lacouture ME, Shah NJ, Faleck DM. Contribution of the Skin–Gut Axis to Immune-Related Adverse Events with Multi-System Involvement. Cancers. 2022; 14(12):2995. https://doi.org/10.3390/cancers14122995
Chicago/Turabian StyleKuo, Alyce M., Lukas Kraehenbuehl, Stephanie King, Donald Y. M. Leung, Elena Goleva, Andrea P. Moy, Mario E. Lacouture, Neil J. Shah, and David M. Faleck. 2022. "Contribution of the Skin–Gut Axis to Immune-Related Adverse Events with Multi-System Involvement" Cancers 14, no. 12: 2995. https://doi.org/10.3390/cancers14122995