Clinical Feasibility of a High-Resolution Thermal Monitoring Sheet for Superficial Hyperthermia in Breast Cancer Patients
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Amsterdam UMC Standard of Care Thermometry
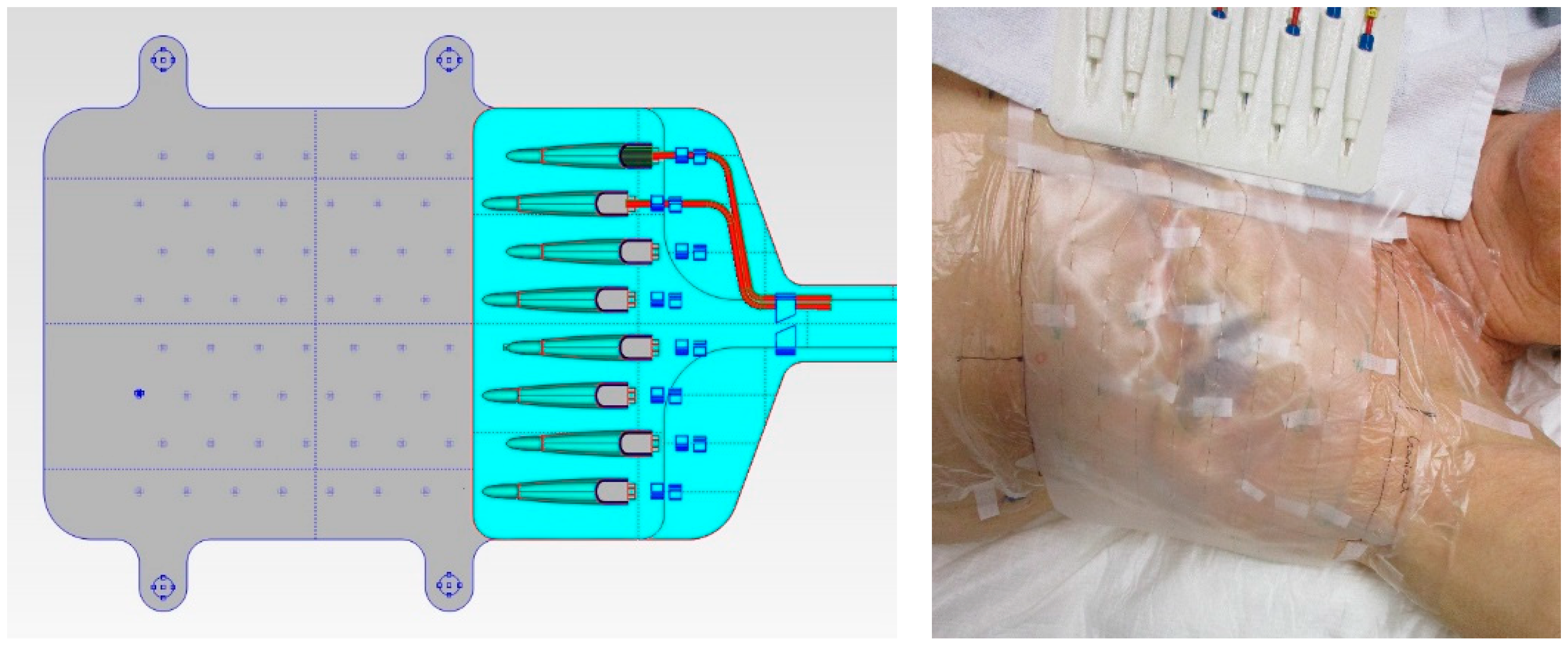
2.2. Thermal Monitoring Sheet (TMS)
2.3. Phantom Experiments
2.3.1. Applicator Efficiency
2.3.2. Power Deposition Pattern
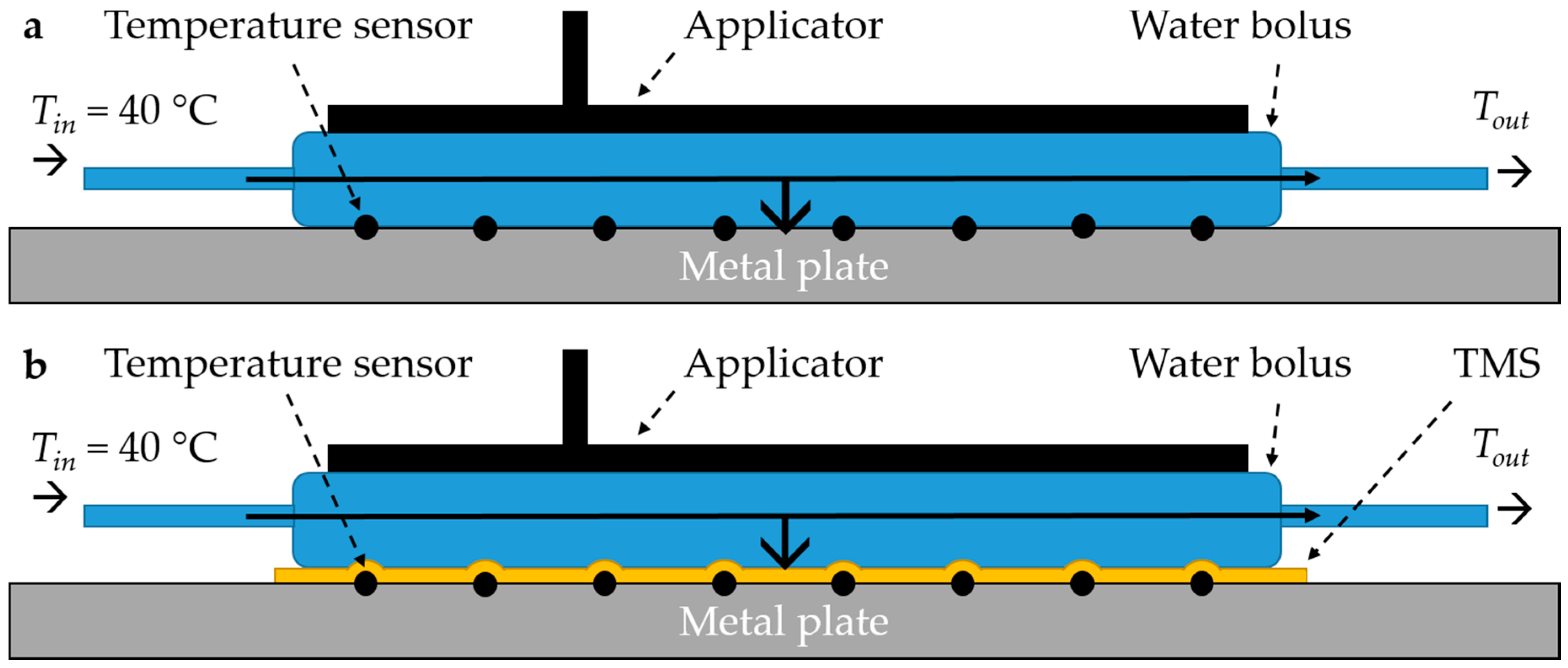
2.3.3. Heat Transfer of the Water Bolus
2.4. Clinical Feasibility Study
Statistical Analysis
3. Results
3.1. Phantom Experiments
3.1.1. Applicator Efficiency
3.1.2. Power Deposition Pattern
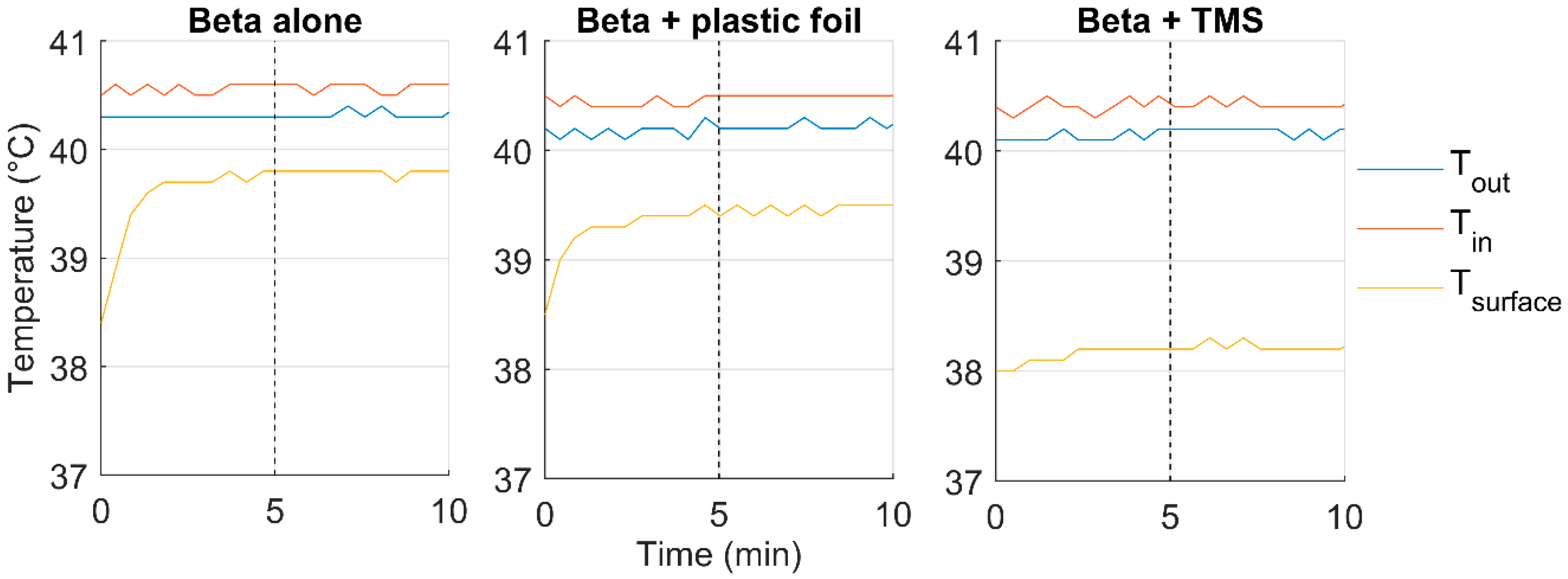
3.1.3. Heat Transfer of the Water Bolus
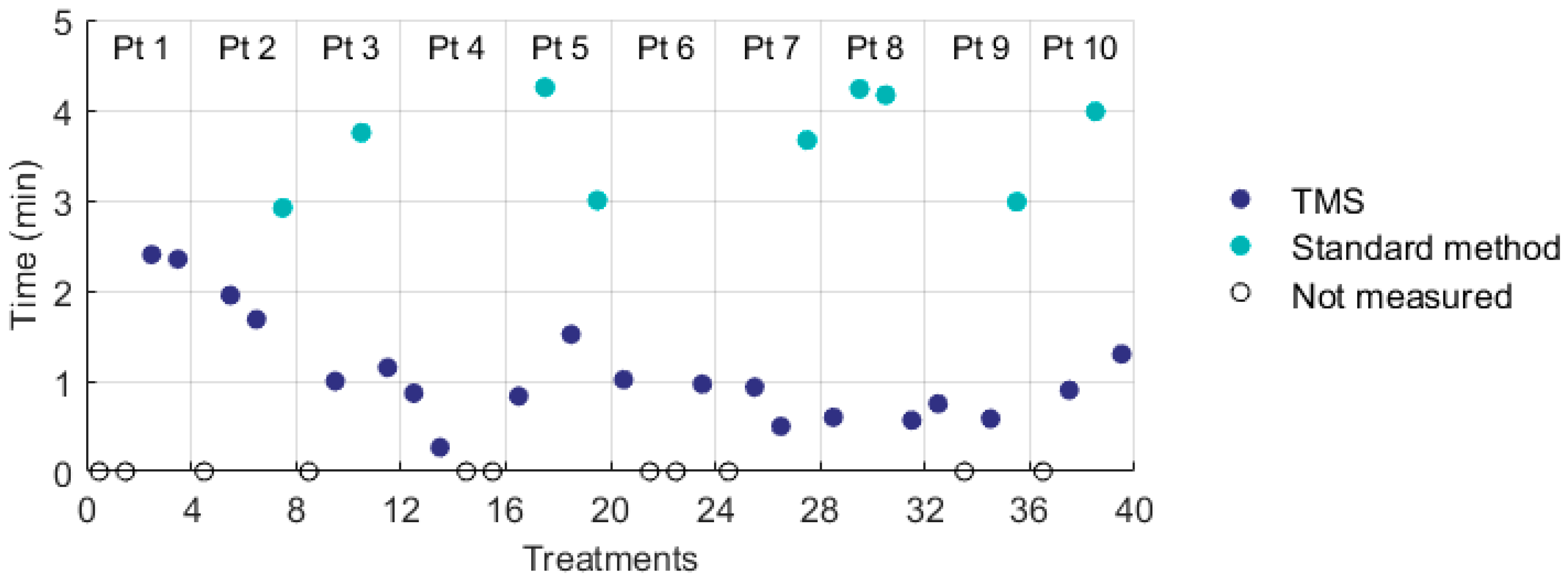
3.2. Clinical Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Overgaard, J.; Gonzalez, D.G.; Hulshof, M.C.C.H.; Arcangeli, G.; Dahl, O.; Mella, O.; Bentzen, S.M. Hyperthermia as an adjuvant to radiation therapy of recurrent or metastatic malignant melanoma. A multicentre randomized trial by the European Society for Hyperthermic Oncology. Int. J. Hyperth. 1996, 12, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Vernon, C.C.; Hand, J.W.; Field, S.B.; Machin, D.; Whaley, J.B.; van der Zee, J.; Van Putten, W.; Van Rhoon, G.; Van Dijk, J.; Gonzalez Gonzalez, D.; et al. Radiotherapy with or without hyperthermia in the treatment of superficial localized breast cancer: Results from five randomized controlled trials. International Collaborative Hyperthermia Group. Int. J. Radiat. Oncol. Biol. Phys. 1996, 3, 731–744. [Google Scholar] [CrossRef] [Green Version]
- Jones, E.L.; Oleson, J.R.; Prosnitz, L.R.; Samulski, T.V.; Vujaskovic, Z.; Yu, D.; Sanders, L.L.; Dewhirst, M.W. Randomized Trial of Hyperthermia and Radiation for Superficial Tumors. J. Clin. Oncol. 2005, 23, 3079–3085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakker, A.; Van Der Zee, J.; Van Tienhoven, G.; Kok, H.P.; Rasch, C.R.N.; Crezee, H. Temperature and thermal dose during radiotherapy and hyperthermia for recurrent breast cancer are related to clinical outcome and thermal toxicity: A systematic review. Int. J. Hyperth. 2019, 36, 1023–1038. [Google Scholar] [CrossRef] [Green Version]
- Notter, M.; Thomsen, A.; Nitsche, M.; Hermann, R.M.; Wolff, H.A.; Habl, G.; Münch, K.; Grosu, A.-L.; Vaupel, P. Combined wIRA-hyperthermia and hypofractionated re-irradiation in the treatment of locally recurrent breast cancer: Evaluation of therapeutic outcome based on a novel size classification. Cancers 2020, 12, 606. [Google Scholar] [CrossRef] [Green Version]
- Van Der Gaag, M.L.; De Bruijne, M.; Samaras, T.; Van Der Zee, J.; Van Rhoon, G.C. Development of a guideline for the water bolus temperature in superficial hyperthermia. Int. J. Hyperth. 2006, 22, 637–656. [Google Scholar] [CrossRef]
- Bakker, A.; Kolff, M.W.; Holman, R.; Van Leeuwen, C.M.; Straten, L.K.-V.; De Kroon-Oldenhof, R.; Rasch, C.R.; Van Tienhoven, G.; Crezee, H. Thermal skin damage during reirradiation and hyperthermia is time-temperature dependent. Int. J. Radiat. Oncol. 2017, 98, 392–399. [Google Scholar] [CrossRef]
- Trefná, H.D.; Crezee, H.; Schmidt, M.; Marder, D.; Lamprecht, U.; Ehmann, M.; Hartmann, J.; Nadobny, J.; Gellermann, J.; Van Holthe, N.; et al. Quality assurance guidelines for superficial hyperthermia clinical trials: I. Clinical requirements. Int. J. Hyperth. 2017, 33, 471–482. [Google Scholar] [CrossRef] [Green Version]
- Bakker, A.; Holman, R.; Rodrigues, D.B.; Dobšíček Trefná, H.; Stauffer, P.R.; Van Tienhoven, G. Analysis of the required number of sensors for adequate monitoring of skin temperature distribution during superficial microwave hyperthermia treatment. Int. J. Hyperth. 2018, 34, 910–917. [Google Scholar] [CrossRef]
- Stauffer, P.R.; Maccarini, P.; Arunachalam, K.; Craciunescu, O.; Diederich, C.; Juang, T.; Rossetto, F.; Schlorff, J.; Milligan, A.; Hsu, J.; et al. Conformal microwave array (CMA) applicators for hyperthermia of diffuse chest wall recurrence. Int. J. Hyperth. 2010, 26, 686–698. [Google Scholar] [CrossRef] [Green Version]
- Arunachalam, K.; Maccarini, P.F.; Stauffer, P.R. A thermal monitoring sheet with low influence from adjacent waterbolus for tissue surface thermometry during clinical hyperthermia. IEEE Trans. Biomed. Eng. 2008, 55, 2397–2406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arunachalam, K.; Maccarini, P.; Juang, T.; Gaeta, C.; Stauffer, P.R. Performance evaluation of a conformal thermal monitoring sheet sensor array for measurement of surface temperature distributions during superficial hyperthermia treatments. Int. J. Hyperth. 2009, 24, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Trefná, H.D.; Crezee, J.; Schmidt, M.; Marder, D.; Lamprecht, U.; Ehmann, M.; Nadobny, J.; Hartmann, J.; Lomax, N.; Abdel-Rahman, S.; et al. Quality assurance guidelines for superficial hyperthermia clinical trials: II. Technical requirements for heating devices. Strahlenther. Onkol. 2017, 193, 351–366. [Google Scholar] [CrossRef] [Green Version]
- De Leeuw, A.A.C.; Crezee, J.; Lagendijk, J.J.W. Temperature and SAR measurements in deep-body hyperthermia with thermocouple thermometry. Int. J. Hyperth. 1993, 9, 685–697. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.; Zweije, R.; Van Tienhoven, G.; Kok, H.P.; Sijbrands, J.; Bongard, H.J.G.D.V.D.; Rasch, C.R.N.; Crezee, H. Two high-resolution thermal monitoring sheets for clinical superficial hyperthermia. Phys. Med. Biol. 2020, 65, 175021. [Google Scholar] [CrossRef] [PubMed]
- Kok, H.P.; Cressman, E.N.K.; Ceelen, W.; Brace, C.L.; Ivkov, R.; Grüll, H.; Ter Haar, G.; Wust, P.; Crezee, J. Heating technology for malignant tumors: A review. Int. J. Hyperth. 2020, 37, 711–741. [Google Scholar] [CrossRef]
- Medlogix. ALBA 4000 Double ON. 2020. Available online: http://www.albahyperthermia.com/hyperthermia-ON4000-Double.html (accessed on 28 September 2020).
- Pyrexar. BSD-500. 2020. Available online: https://www.pyrexar.com/hyperthermia/bsd-500 (accessed on 28 September 2020).
- Gelvich, E.A.; Mazokhin, V. Contact flexible microstrip applicators (CFMA) in a range from microwaves up to short waves. IEEE Trans. Biomed. Eng. 2002, 49, 1015–1023. [Google Scholar] [CrossRef]
- Kok, H.P.; De Greef, M.; Correia, D.; Vörding, P.J.Z.V.S.; Van Stam, G.; Gelvich, E.A.; Bel, A.; Crezee, J. FDTD simulations to assess the performance of CFMA-434 applicators for superficial hyperthermia. Int. J. Hyperth. 2009, 25, 462–476. [Google Scholar] [CrossRef]
- Van Stam, G.; Kok, H.P.; Hulshof, M.C.C.M.; Kolff, M.W.; Van Tienhoven, G.; Sijbrands, J.; Bakker, A.; Vörding, P.J.Z.V.S.; Oldenborg, S.; De Greef, M.; et al. A flexible 70 MHz phase-controlled double waveguide system for hyperthermia treatment of superficial tumours with deep infiltration. Int. J. Hyperth. 2017, 33, 796–809. [Google Scholar] [CrossRef] [Green Version]
- Kok, H.P.; Berg, C.A.T.V.D.; A Van Haaren, P.M.; Crezee, J. Artefacts in intracavitary temperature measurements during regional hyperthermia. Phys. Med. Biol. 2007, 52, 5157–5171. [Google Scholar] [CrossRef]
- Schneider, C.; Olmi, R.; van Dijk, J. Phantom design: Applicability and physical properties. In Thermoradiotherapy Thermochem; Seegenschmiedt, M., Fessenden, P., Vernon, C., Eds.; Springer: Berlin/Heidelberg, Germany, 1994; pp. 381–397. [Google Scholar]
- Guy, A. Analyses of electromagnetic fields induced in biological tissues by thermographic studies on equivalent phantom models. IEEE Trans. Microw. Theory Tech. 1971, 19, 205–214. [Google Scholar] [CrossRef]
- Gabriele, P.; Ferrara, T.; Baiotto, B.; Garibaldi, E.; Marini, P.; Penduzzu, G.; Giovannini, V.; Bardati, F.; Guiot, C. Radio hyperthermia for re-treatment of superficial tumours. Int. J. Hyperth. 2009, 25, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Sherar, M.; Liu, F.; Newcombe, D.; Cooper, B.; Levin, W.; Taylor, W.; Hunt, J. Beam shaping for microwave waveguide hyperthermia applicators. Int. J. Radiat. Oncol. 1993, 25, 849–857. [Google Scholar] [CrossRef]
- Rodrigues, D.B.; Hurwitz, M.D.; Maccarini, P.F.; Stauffer, P.R. Optimization of chest wall hyperthermia treatment using a virtual human chest model. In Proceedings of the 9th European Conference on Antennas and Propagation (EuCAP), Lisbon, Portugal, 12–17 April 2015. [Google Scholar]
- Stauffer, P.R.; Rodrigues, D.B.; Sinahon, R.; Sbarro, L.; Beckhoff, V.; Hurwitz, M.D. Using a conformal water bolus to adjust heating patterns of microwave waveguide applicators. In Energy-Based Treatment of Tissue and Assessment IX; Ryan, T., Ed.; International Society for Optics and Photonics: Bellingham, WA, USA, 2017; Volume 10066, p. 100660N. [Google Scholar] [CrossRef] [Green Version]
- Chou, C.-K. Use of heating rate and specific absorption rate in the hyperthermia clinic. Int. J. Hyperth. 1990, 6, 367–370. [Google Scholar] [CrossRef]
- Lagendijk, J.J.W. Heat transfer in tissues. In Physics and Technology of Hyperthermia; Field, S.B., Franconi, C., Eds.; Springer: Dordrecht, The Netherlands, 1987; pp. 517–552. [Google Scholar] [CrossRef]
- Engin, K.; Tupchong, L.; Waterman, F.M.; Komarnicky, L.; Mansfield, C.M.; Leeper, D.B. ?Patchwork? fields in thermoradiotherapy for extensive chest wall recurrences of breast carcinoma. Breast Cancer Res. Treat. 1993, 27, 263–270. [Google Scholar] [CrossRef]
- Lindholm, C.-E.; Kjellén, E.; Nilsson, P.; Weber, L.; Hill, S. Prognostic factors for tumour response and skin damage to combined radiotherapy and hyperthermia in superficial recurrent breast carcinomas. Int. J. Hyperth. 1995, 11, 337–355. [Google Scholar] [CrossRef]
- Linthorst, M.; Van Geel, A.N.; Baaijens, M.; Ameziane, A.; Ghidey, W.; Van Rhoon, G.C.; Van Der Zee, J. Re-irradiation and hyperthermia after surgery for recurrent breast cancer. Radiother. Oncol. 2013, 109, 188–193. [Google Scholar] [CrossRef]
- Linthorst, M.; Baaijens, M.; Wiggenraad, R.; Creutzberg, C.L.; Ghidey, W.; Van Rhoon, G.C.; Van Der Zee, J. Local control rate after the combination of re-irradiation and hyperthermia for irresectable recurrent breast cancer: Results in 248 patients. Radiother. Oncol. 2015, 117, 217–222. [Google Scholar] [CrossRef]
- Seegenschmiedt, H.M.; Karlsson, U.L.; Sauer, R.; Brady, L.W.; Herbst, M.; E Amendola, B.; Markoe, A.M.; A Fisher, S.; Micaily, B. Superficial chest wall recurrences of breast cancer: Prognostic treatment factors for combined radiation therapy and hyperthermia. Radiology 1989, 173, 551–558. [Google Scholar] [CrossRef]
- Notter, M.; Piazena, H.; Vaupel, M.P. Hypofractionated re-irradiation of large-sized recurrent breast cancer with thermography-controlled, contact-free water-filtered infra-red-A hyperthermia: A retrospective study of 73 patients. Int. J. Hyperth. 2016, 33, 227–236. [Google Scholar] [CrossRef] [Green Version]
- Overgaard, J. Simultaneous and sequential hyperthermia and radiation treatment of an experimental tumor and its surrounding normal tissue in vivo. Int. J. Radiat. Oncol. 1980, 6, 1507–1517. [Google Scholar] [CrossRef]
- Van Leeuwen, C.M.; Oei, A.L.; Chin, K.W.T.K.; Crezee, J.; Bel, A.; Westermann, A.M.; Buist, M.R.; Franken, N.A.P.; Stalpers, L.J.A.; Kok, H.P. A short time interval between radiotherapy and hyperthermia reduces in-field recurrence and mortality in women with advanced cervical cancer. Radiat. Oncol. 2017, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]




| Specifications | Phantom Experiments | Clinical Study | |
|---|---|---|---|
| Beta Applicator | MA-100 Applicator | 3H Applicator | |
| Frequency | 434 MHz | 915 MHz | 434 MHz |
| Applicator (main direction EM-field ↕) |  |  |  |
| Aperture dimensions | 150 × 160 mm [17] | 100 × 130 mm [18] | 290 × 210 mm [19] |
| Aperture shape | Fixed curvature | Flat | Bendable |
| Water bolus dimensions | 170 × 175 mm | 130 × 130 mm | 300 × 220 mm |
| Effective field size (50% SAR) | 80 × 120 mm [17] | 80 × 100 mm [18] | 177 × 175 mm [20] |
| Effective heating depth (25% SAR) | 23–33 mm [17] | 25 mm [18] | 30 mm [19] |
| Experiment | Method | Phantom | Comparison |
|---|---|---|---|
| Applicator efficiency | Calorimetric method (Figure 3) | Insulated saline water bag Dimensions: 350 × 250 × 90 mm (l × w × h) Content: 6.426 kg; 0.6% NaCl |
|
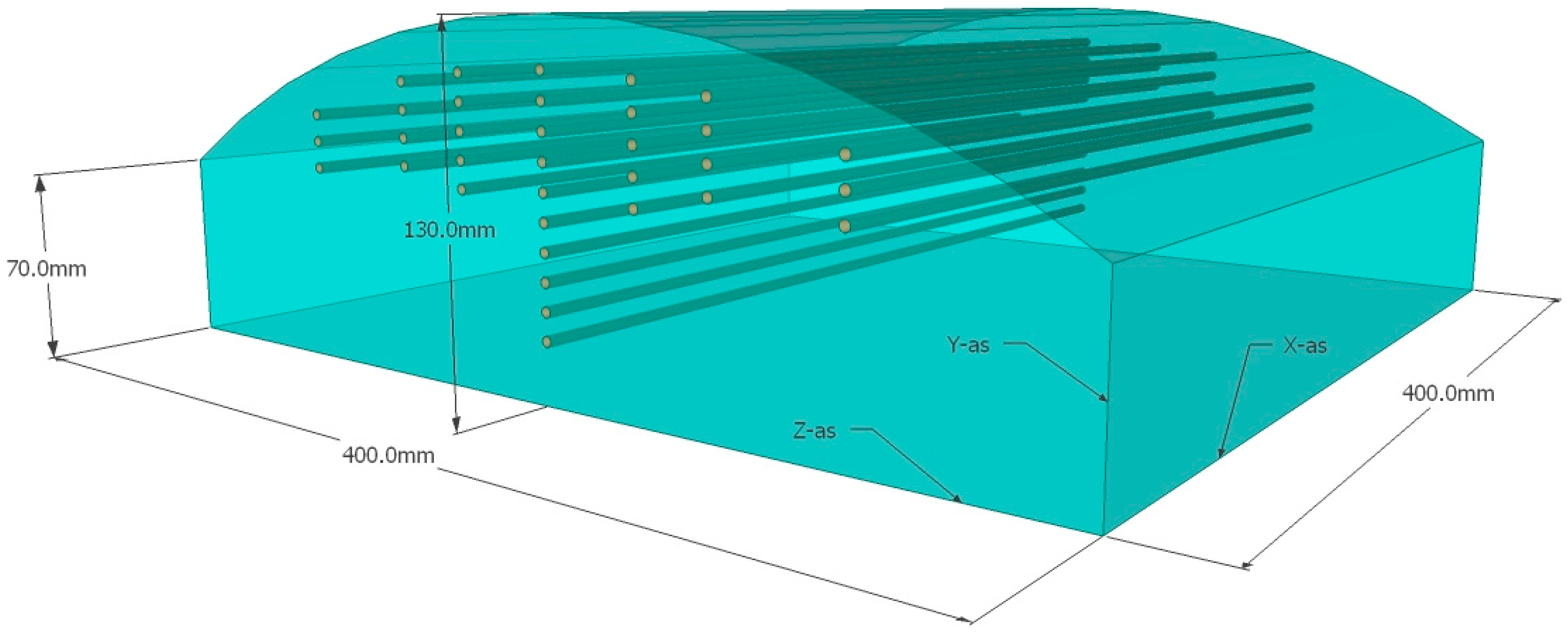
| Power deposition pattern | IR camera (Figure 4) | Curved muscle-equivalent phantom with on top a removable 10 mm fat-equivalent layer Muscle-equivalent phantom: Dimensions: 400 × 400 × 70–130 (top) mm Content: wallpaper paste [21,22,23] Fat-equivalent layer: Dimensions: 400 × 400 × 10–70 (top) mm Content: acetylene black mixed with aluminum powder and laminac polyester resin [24] |
|
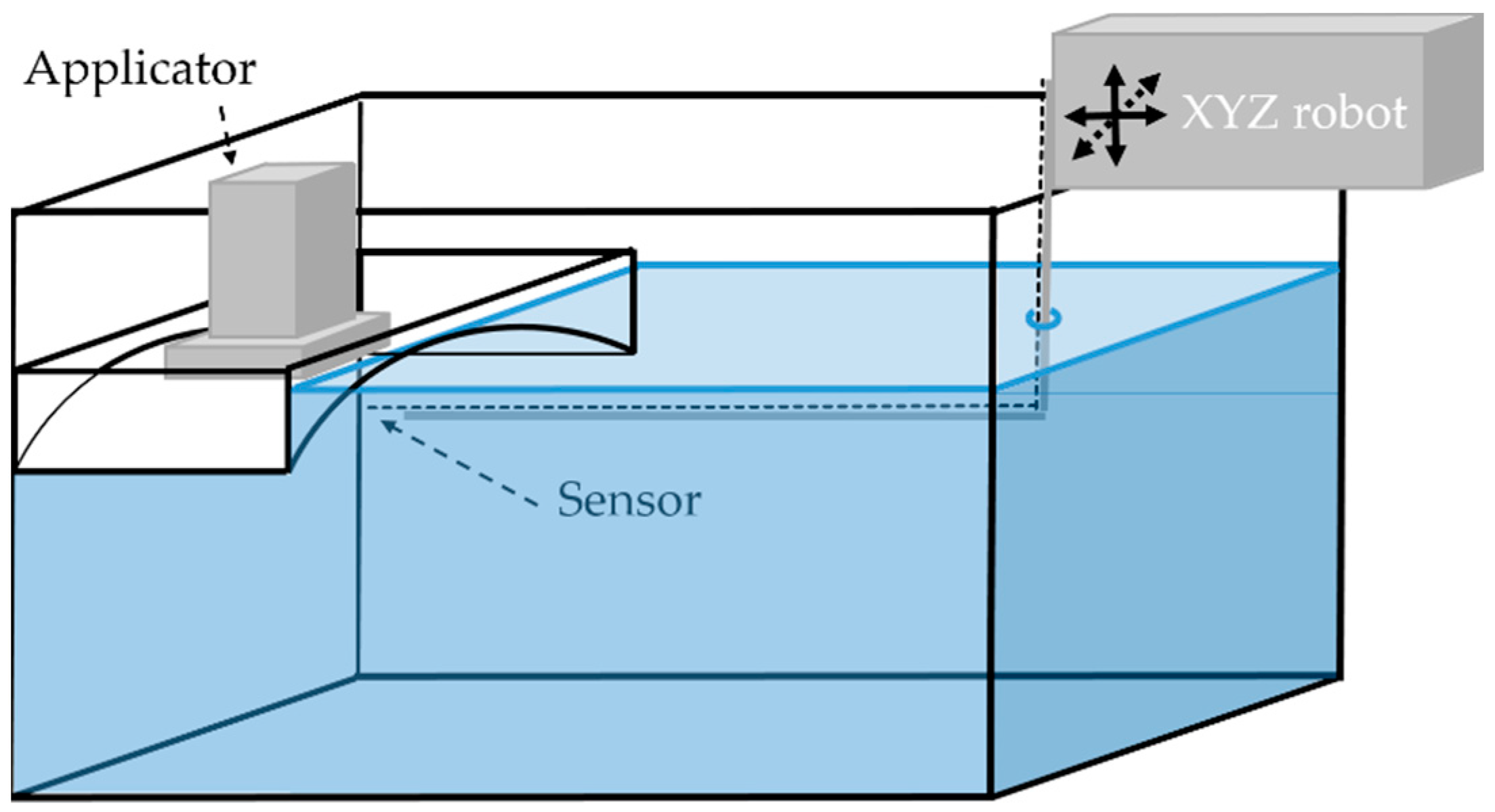
| E-field (Figure 5) | Tank filled with liquid muscle-equivalent phantom with a curved top Dimensions: 1000 × 400 × 400 mm Content: ca. 80 L; 0.6% NaCl; σ = 1.26–1.27 S m−1 |
| |
| Heat transfer of the water bolus | (Figure 6) | Metal plate Dimensions: 440 × 280 × 1 mm |
|
| Parameter | Quantity (Unit) | Beta Applicator | MA-100 Applicator | ||||
|---|---|---|---|---|---|---|---|
| Alone | +Plastic Foil | +TMS | Alone | +Plastic Foil | +TMS | ||
| Applicator efficiency (%) | Mean ± SD | 94.4 ± 2.9 | 91.2 ± 2.1 | 92.7 ± 1.1 | 89.4 ± 1.5 | 88.5 ± 1.7 | 88.0 ± 1.5 |
| Reduction (%) | 3.2 | 1.7 | 1.0 | 1.4 | |||
| Power distribution pattern | Effective field size E-field probe (mm) | 43 × 58 | 47 × 58 | 80 × 105 | 76 × 105 | ||
| Heat transfer coefficient h (W m−2 °C−1) | Mean ± SD | 2288 ± 123 | 1680 ± 160 | 997 ± 32 | 2717 ± 406 | 2417 ± 199 | 1345 ± 241 |
| Reduction (%) | 26.6 | 56.4 | 11.1 | 50.5 | |||
| Treatment Characteristic | Standard Method | TMS | (Generalized) Linear Mixed Models | ||
|---|---|---|---|---|---|
| Parameter Estimate | 95% CI | ||||
| Treatments | 20 | 20 | |||
| Power (W) | 44.5 ± 11.4 | 48.4 ± 12.3 | |||
| Water bolus temperature (°C) | 42.5 ± 0.6 | 42.6 ± 0.7 | |||
| Invasive temperature (°C) 1 | T0 | 41.6 ± 1.1 | 42.0 ± 1.5 | ||
| T10 | 41.0 ± 0.9 | 41.3 ± 1.3 | |||
| T50 | 39.8 ± 1.1 | 39.8 ± 1.3 | |||
| T90 | 38.8 ± 1.0 | 38.8 ± 1.1 | |||
| T100 | 38.1 ± 0.6 | 38.1 ± 0.9 | |||
| T0 − 100 | 3.5 ± 1.0 | 3.9 ± 1.5 | |||
| Skin temperature (°C) | T0 | 43.2 ± 0.4 | 43.4 ± 0.5 | ||
| T10 | 41.9 ± 0.3 | 41.9 ± 0.2 | |||
| T50 | 40.9 ± 0.3 | 40.8 ± 0.3 | |||
| T90 | 39.8 ± 0.3 | 39.6 ± 0.5 | |||
| T100 | 38.4 ± 0.9 | 37.3 ± 1.4 | −0.8 | −1.5 to −0.1 | |
| T0 − T100 | 4.8 ± 1.0 | 5.7 ± 1.7 | 1.0 | 0.1 to 1.8 | |
| Time to place the sensors (s) 2 | 220 ± 34 | 66 ± 36 | −159 | −184 to −134 | |
| Treatments with thermal toxicity | 0 | 0 | |||
| Treatments with complaints | 3 | 6 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bakker, A.; Zweije, R.; Kok, H.P.; Kolff, M.W.; van den Bongard, H.J.G.D.; Schmidt, M.; van Tienhoven, G.; Crezee, H. Clinical Feasibility of a High-Resolution Thermal Monitoring Sheet for Superficial Hyperthermia in Breast Cancer Patients. Cancers 2020, 12, 3644. https://doi.org/10.3390/cancers12123644
Bakker A, Zweije R, Kok HP, Kolff MW, van den Bongard HJGD, Schmidt M, van Tienhoven G, Crezee H. Clinical Feasibility of a High-Resolution Thermal Monitoring Sheet for Superficial Hyperthermia in Breast Cancer Patients. Cancers. 2020; 12(12):3644. https://doi.org/10.3390/cancers12123644
Chicago/Turabian StyleBakker, Akke, Remko Zweije, Henny Petra Kok, Merel Willemijn Kolff, H. J. G. Desiree van den Bongard, Manfred Schmidt, Geertjan van Tienhoven, and Hans Crezee. 2020. "Clinical Feasibility of a High-Resolution Thermal Monitoring Sheet for Superficial Hyperthermia in Breast Cancer Patients" Cancers 12, no. 12: 3644. https://doi.org/10.3390/cancers12123644






