Surgical Management of Hepatoblastoma and Recent Advances
Abstract
:1. Introduction
2. Preoperative Planning
3. The PRETEXT and POST-TEXT System
4. Upfront Versus Delayed Surgery
5. Advancement in Techniques to Make Tumors Resectable
6. Advances Intraoperative Techniques and Approaches to Local Control
7. Resection of Lung Metastasis
8. Management of Disease Relapse
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Darbari, A.; Sabin, K.M.; Shapiro, C.N.; Schwarz, K.B. Epidemiology of primary hepatic malignancies in U.S. children. Hepatology 2003, 38, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Allan, B.J.; Parikh, P.P.; Diaz, S.; Perez, E.A.; Neville, H.L.; Sola, J.E. Predictors of survival and incidence of hepatoblastoma in the paediatric population. HPB 2013, 15, 741–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linabery, A.M.; Ross, J.A. Trends in childhood cancer incidence in the U.S. (1992–2004). Cancer 2008, 112, 416–432. [Google Scholar] [CrossRef] [PubMed]
- Hung, G.-Y.; Lin, L.-Y.; Yu, T.-Y.; Lee, C.-Y.; Yen, H.-J.; Horng, J.-L. Hepatoblastoma incidence in Taiwan: A population-based study. J. Chin. Med. Assoc. 2018, 81, 541–547. [Google Scholar] [CrossRef]
- Spector, L.G.; Birch, J. The epidemiology of hepatoblastoma. Pediatr. Blood Cancer 2012, 59, 776–779. [Google Scholar] [CrossRef]
- Czauderna, P.; Haeberle, B.; Hiyama, E.; Rangaswami, A.; Krailo, M.; Maibach, R.; Rinaldi, E.; Feng, Y.; Aronson, D.; Malogolowkin, M.; et al. The Children’s Hepatic tumors International Collaboration (CHIC): Novel global rare tumor database yields new prognostic factors in hepatoblastoma and becomes a research model. Eur. J. Cancer 2016, 52, 92–101. [Google Scholar] [CrossRef] [Green Version]
- Aronson, D.C.; Meyers, R.L. Malignant tumors of the liver in children. Semin. Pediatr. Surg. 2016, 25, 265–275. [Google Scholar] [CrossRef]
- Malogolowkin, M.H.; Katzenstein, H.M.; Meyers, R.L.; Krailo, M.D.; Rowland, J.M.; Haas, J.; Finegold, M.J. Complete Surgical Resection Is Curative for Children with Hepatoblastoma with Pure Fetal Histology: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2011, 29, 3301–3306. [Google Scholar] [CrossRef] [Green Version]
- Meyers, R.L.; Maibach, R.; Hiyama, E.; Haberle, B.; Krailo, M.; Rangaswami, A.; Aronson, D.C.; Malogolowkin, M.H.; Perilongo, G.; von Schweinitz, D.; et al. Risk-stratified staging in paediatric hepatoblastoma: A unified analysis from the Children’s Hepatic tumors International Collaboration. Lancet Oncol. 2017, 18, 122–131. [Google Scholar] [CrossRef] [Green Version]
- Trobaugh-Lotrario, A.D.; Meyers, R.L.; Tiao, G.M.; Feusner, J.H. Pediatric liver transplantation for hepatoblastoma. Transl. Gastroenterol. Hepatol. 2016, 1, 44. [Google Scholar] [CrossRef] [Green Version]
- Lim, I.I.P.; Bondoc, A.J.; Geller, J.I.; Tiao, G.M. Hepatoblastoma-The Evolution of Biology, Surgery, and Transplantation. Children 2018, 6, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCarville, M.B.; Roebuck, D.J. Diagnosis and staging of hepatoblastoma: Imaging aspects. Pediatr. Blood Cancer 2012, 59, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Towbin, A.J.; Meyers, R.L.; Woodley, H.; Miyazaki, O.; Weldon, C.B.; Morland, B.; Hiyama, E.; Czauderna, P.; Roebuck, D.J.; Tiao, G.M. 2017 PRETEXT: Radiologic staging system for primary hepatic malignancies of childhood revised for the Paediatric Hepatic International Tumour Trial (PHITT). Pediatr. Radiol. 2018, 48, 536–554. [Google Scholar] [CrossRef] [PubMed]
- Seale, M.K.; Catalano, O.A.; Saini, S.; Hahn, P.F.; Sahani, D.V. Hepatobiliary-specific MR contrast agents: Role in imaging the liver and biliary tree. Radiographics 2009, 29, 1725–1748. [Google Scholar] [CrossRef]
- Meyers, A.B.; Towbin, A.J.; Serai, S.; Geller, J.I.; Podberesky, D.J. Characterization of pediatric liver lesions with gadoxetate disodium. Pediatr. Radiol. 2011, 41, 1183–1197. [Google Scholar] [CrossRef]
- Chavhan, G.B.; Shelmerdine, S.; Jhaveri, K.; Babyn, P.S. Liver MR Imaging in Children: Current Concepts and Technique. Radiographics 2016, 36, 1517–1532. [Google Scholar] [CrossRef] [Green Version]
- Perilongo, G.; Brown, J.; Shafford, E.; Brock, P.; De Camargo, B.; Keeling, J.W.; Vos, A.; Philips, A.; Pritchard, J.; Plaschkes, J.; et al. Hepatoblastoma presenting with lung metastases—Treatment results of the first cooperative, prospective study of the International Society of Paediatric Oncology on Childhood Liver Tumors. Cancer 2000, 89, 1845–1853. [Google Scholar] [CrossRef]
- Bottcher, J.; Hansch, A.; Pfeil, A.; Schmidt, P.; Malich, A.; Schneeweiss, A.; Maurer, M.H.; Streitparth, F.; Teichgraber, U.K.; Renz, D.M. Detection and classification of different liver lesions: Comparison of Gd-EOB-DTPA-enhanced MRI versus multiphasic spiral CT in a clinical single centre investigation. Eur. J. Radiol. 2013, 82, 1860–1869. [Google Scholar] [CrossRef]
- Sironi, S.; Messa, C.; Cistaro, A.; Landoni, C.; Provenzi, M.; Giraldi, E.; Sonzogni, A.; Fazio, F. Recurrent hepatoblastoma in orthotopic transplanted liver: Detection with FDG positron emission tomography. AJR Am. J. Roentgenol. 2004, 182, 1214–1216. [Google Scholar] [CrossRef] [Green Version]
- Figarola, M.S.; McQuiston, S.A.; Wilson, F.; Powell, R. Recurrent hepatoblastoma with localization by PET-CT. Pediatr. Radiol. 2005, 35, 1254–1258. [Google Scholar] [CrossRef]
- Philip, I.; Shun, A.; McCowage, G.; Howman-Giles, R. Positron emission tomography in recurrent hepatoblastoma. Pediatr. Surg. Int. 2005, 21, 341–345. [Google Scholar] [CrossRef]
- Pritchard, J.; Brown, J.; Shafford, E.; Perilongo, G.; Brock, P.; Dicks-Mireaux, C.; Keeling, J.; Phillips, A.; Vos, A.; Plaschkes, J. Cisplatin, doxorubicin, and delayed surgery for childhood hepatoblastoma: A successful approach—Results of the first prospective study of the international society of pediatric oncology. J. Clin. Oncol. 2000, 18, 3819–3828. [Google Scholar] [CrossRef]
- Roebuck, D.J.; Aronson, D.; Clapuyt, P.; Czauderna, P.; de Ville de Goyet, J.; Gauthier, F.; Mackinlay, G.; Maibach, R.; McHugh, K.; Olsen, O.E.; et al. 2005 PRETEXT: A revised staging system for primary malignant liver tumours of childhood developed by the SIOPEL group. Pediatr. Radiol. 2007, 37, 123–132, quiz 249–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aronson, D.C.; Schnater, J.M.; Staalman, C.R.; Weverling, G.J.; Plaschkes, J.; Perilongo, G.; Brown, J.; Phillips, A.; Otte, J.B.; Czauderna, P.; et al. Predictive value of the pretreatment extent of disease system in hepatoblastoma: Results from the International Society of Pediatric Oncology Liver Tumor Study Group SIOPEL-1 study. J. Clin. Oncol. 2005, 23, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
- Perilongo, G.; Shafford, E.; Plaschkes, J.; Liver Tumour Study Group of the International Society of Paediatric Oncology. SIOPEL trials using preoperative chemotherapy in hepatoblastoma. Lancet Oncol. 2000, 1, 94–100. [Google Scholar] [CrossRef]
- Perilongo, G.; Maibach, R.; Shafford, E.; Brugieres, L.; Brock, P.; Morland, B.; de Camargo, B.; Zsiros, J.; Roebuck, D.; Zimmermann, A.; et al. Cisplatin versus cisplatin plus doxorubicin for standard-risk hepatoblastoma. N. Engl. J. Med. 2009, 361, 1662–1670. [Google Scholar] [CrossRef] [Green Version]
- Schnater, J.M.; Aronson, D.C.; Plaschkes, J.; Perilongo, G.; Brown, J.; Otte, J.B.; Brugieres, L.; Czauderna, P.; MacKinlay, G.; Vos, A. Surgical view of the treatment of patients with hepatoblastoma—Results from the first prospective trial of the International Society of Pediatric Oncology Liver Tumor Study Group (SIOPEL-1). Cancer 2002, 94, 1111–1120. [Google Scholar] [CrossRef]
- Zsiros, J.; Maibach, R.; Shafford, E.; Brugieres, L.; Brock, P.; Czauderna, P.; Roebuck, D.; Childs, M.; Zimmermann, A.; Laithier, V.; et al. Successful treatment of childhood high-risk hepatoblastoma with dose-intensive multiagent chemotherapy and surgery: Final results of the SIOPEL-3HR study. J. Clin. Oncol. 2010, 28, 2584–2590. [Google Scholar] [CrossRef]
- Ortega, J.A.; Douglass, E.C.; Feusner, J.H.; Reynolds, M.; Quinn, J.J.; Finegold, M.J.; Haas, J.E.; King, D.R.; Liu-Mares, W.; Sensel, M.G.; et al. Randomized comparison of cisplatin/vincristine/fluorouracil and cisplatin/continuous infusion doxorubicin for treatment of pediatric hepatoblastoma: A report from the Children’s Cancer Group and the Pediatric Oncology Group. J. Clin. Oncol. 2000, 18, 2665–2675. [Google Scholar] [CrossRef]
- Lopez-Terrada, D.; Alaggio, R.; de Davila, M.T.; Czauderna, P.; Hiyama, E.; Katzenstein, H.; Leuschner, I.; Malogolowkin, M.; Meyers, R.; Ranganathan, S.; et al. Towards an international pediatric liver tumor consensus classification: Proceedings of the Los Angeles COG liver tumors symposium. Mod. Pathol. 2014, 27, 472–491. [Google Scholar] [CrossRef] [Green Version]
- Murphy, A.J.; Ayers, G.D.; Hilmes, M.A.; Mukherjee, K.; Wilson, K.J.; Allen, W.M.; Fernandez-Pineda, I.; Shinall, M.C., Jr.; Zhao, Z.; Furman, W.L.; et al. Imaging analysis of hepatoblastoma resectability across neoadjuvant chemotherapy. J. Pediatr. Surg. 2013, 48, 1239–1248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venkatramani, R.; Stein, J.E.; Sapra, A.; Genyk, Y.; Jhaveri, V.; Malogolowkin, M.; Mascarenhas, L. Effect of neoadjuvant chemotherapy on resectability of stage III and IV hepatoblastoma. Br. J. Surg. 2015, 102, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Lovvorn, H.N., 3rd; Ayers, D.; Zhao, Z.; Hilmes, M.; Prasad, P.; Shinall, M.C., Jr.; Berch, B.; Neblett, W.W., 3rd; O’Neill, J.A., Jr. Defining hepatoblastoma responsiveness to induction therapy as measured by tumor volume and serum alpha-fetoprotein kinetics. J. Pediatr. Surg. 2010, 45, 121–128, discussion 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hery, G.; Franchi-Abella, S.; Habes, D.; Brugieres, L.; Martelli, H.; Fabre, M.; Pariente, D.; Gauthier, F.; Jacquemin, E.; Branchereau, S. Initial liver transplantation for unresectable hepatoblastoma after chemotherapy. Pediatr. Blood Cancer 2011, 57, 1270–1275. [Google Scholar] [CrossRef]
- Barrena, S.; Hernandez, F.; Miguel, M.; de la Torre, C.A.; Moreno, A.M.; Encinas, J.L.; Leal, N.; Murcia, J.; Martinez, L.; Gamez, M.; et al. High-risk hepatoblastoma: Results in a pediatric liver transplantation center. Eur. J. Pediatr. Surg. 2011, 21, 18–20. [Google Scholar] [CrossRef]
- Czauderna, P.; Zbrzezniak, G.; Narozanski, W.; Korzon, M.; Wyszomirska, M.; Stoba, C. Preliminary experience with arterial chemoembolization for hepatoblastoma and hepatocellular carcinoma in children. Pediatr. Blood Cancer 2006, 46, 825–828. [Google Scholar] [CrossRef]
- Wang, S.; Yang, C.; Zhang, J.; Kong, X.R.; Zhu, H.; Wu, F.; Wang, Z. First experience of high-intensity focused ultrasound combined with transcatheter arterial embolization as local control for hepatoblastoma. Hepatology 2014, 59, 170–177. [Google Scholar] [CrossRef]
- Hirakawa, M.; Nishie, A.; Asayama, Y.; Fujita, N.; Ishigami, K.; Tajiri, T.; Taguchi, T.; Honda, H. Efficacy of preoperative transcatheter arterial chemoembolization combined with systemic chemotherapy for treatment of unresectable hepatoblastoma in children. Jpn. J. Radiol. 2014, 32, 529–536. [Google Scholar] [CrossRef]
- Pham, T.A.; Gallo, A.M.; Concepcion, W.; Esquivel, C.O.; Bonham, C.A. Effect of Liver Transplant on Long-term Disease-Free Survival in Children with Hepatoblastoma and Hepatocellular Cancer. JAMA Surg. 2015, 150, 1150–1158. [Google Scholar] [CrossRef] [Green Version]
- Aguado, A.; Ristagno, R.; Towbin, A.J.; Gupta, A.; Haberle, S.; Qi, Z.; Patel, M.N.; Kukreja, K.U.; Tiao, G.M.; Geller, J.I. Transarterial radioembolization with yttrium-90 of unresectable primary hepatic malignancy in children. Pediatr. Blood Cancer 2019, 66, e27510. [Google Scholar] [CrossRef]
- Glantzounis, G.K.; Tokidis, E.; Basourakos, S.P.; Ntzani, E.E.; Lianos, G.D.; Pentheroudakis, G. The role of portal vein embolization in the surgical management of primary hepatobiliary cancers. A systematic review. Eur. J. Surg. Oncol. 2017, 43, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Terraz, S.; Ronot, M.; Breguet, R.; Anooshiravani, M.; Rubbia-Brandt, L.; Becker, C.D.; Wildhaber, B.E. Portal Vein Embolization Before Extended Hepatectomy in a Toddler with Mesenchymal Hamartoma. Pediatrics 2015, 136, e1055–e1059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, J.C.; Kim, J.; Browning, M.; Wagner, A.; Lerret, S.; Segura, A.D.; Zimmerman, M.A. Modified Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy for Hepatoblastoma in a Small Infant How Far Can We Push the Envelope? Ann. Surg. 2017, 266, E16–E17. [Google Scholar] [CrossRef] [PubMed]
- Schnitzbauer, A.A.; Lang, S.A.; Goessmann, H.; Nadalin, S.; Baumgart, J.; Farkas, S.A.; Fichtner-Feigl, S.; Lorf, T.; Goralcyk, A.; Horbelt, R.; et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann. Surg. 2012, 255, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Wiederkehr, J.C.; Avilla, S.G.; Mattos, E.; Coelho, I.M.; Ledesma, J.A.; Conceicao, A.F.; Wiederkehr, H.A.; Wiederkehr, B.A. Associating liver partition with portal vein ligation and staged hepatectomy (ALPPS) for the treatment of liver tumors in children. J. Pediatr. Surg. 2015, 50, 1227–1231. [Google Scholar] [CrossRef] [PubMed]
- Torzilli, G.; Procopio, F. State of the Art of Intraoperative Ultrasound in Liver Surgery: Current Use for Resection-guidance. Chirurgia 2017, 112, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Felsted, A.E.; Shi, Y.; Masand, P.M.; Nuchtern, J.G.; Goss, J.A.; Vasudevan, S.A. Intraoperative ultrasound for liver tumor resection in children. J. Surg. Res. 2015, 198, 418–423. [Google Scholar] [CrossRef]
- Mise, Y.; Tani, K.; Aoki, T.; Sakamoto, Y.; Hasegawa, K.; Sugawara, Y.; Kokudo, N. Virtual liver resection: Computer-assisted operation planning using a three-dimensional liver representation. J. Hepato-Biliary-Pancreat. Sci. 2013, 20, 157–164. [Google Scholar] [CrossRef]
- Zhang, G.; Zhou, X.J.; Zhu, C.Z.; Dong, Q.; Su, L. Usefulness of three-dimensional(3D) simulation software in hepatectomy for pediatric hepatoblastoma. Surg. Oncol. 2016, 25, 236–243. [Google Scholar] [CrossRef]
- Nakayama, K.; Oshiro, Y.; Miyamoto, R.; Kohno, K.; Fukunaga, K.; Ohkohchi, N. The effect of three-dimensional preoperative simulation on liver surgery. World. J. Surg. 2017, 41, 1840–1847. [Google Scholar] [CrossRef] [Green Version]
- Fuchs, J.; Warmann, S.W.; Szavay, P.; Kirschner, H.J.; Schäfer, J.F.; Hennemuth, A.; Scheel-Walter, H.G.; Bourquain, H.; Peitgen, H.O. Three-dimensional visualization and virtual simulation of resections in pediatric solid tumors. J. Pediatr. Surg. 2005, 40, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Warmann, S.W.; Schenk, A.; Schaefer, J.F.; Ebinger, M.; Blumenstock, G.; Tsiflikas, I.; Fuchs, J. Computer-assisted surgery planning in children with complex liver tumors identifies variability of the classical Couinaud classification. J. Pediatr. Surg. 2016, 51, 1801–1806. [Google Scholar] [CrossRef] [PubMed]
- Souzaki, R.; Kinoshita, Y.; Ieiri, S.; Hayashida, M.; Koga, Y.; Shirabe, K.; Hara, T.; Maehara, Y.; Hashizume, M.; Taguchi, T. Three-dimensional liver model based on preoperative CT images as a tool to assist in surgical planning for hepatoblastoma in a child. Pediatr. Surg. Int. 2015, 31, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Lin, S.; Xie, Q.; Ouyang, W.; Tan, T.; Li, J.; Chen, Z.; Yang, J.; Wu, H.; Pan, J.; et al. Impact of 3D printing technology on the comprehension of surgical liver anatomy. Surg. Endosc. 2019, 33, 411–417. [Google Scholar] [CrossRef]
- Zein, N.N.; Hanouneh, I.A.; Bishop, P.D.; Samaan, M.; Eghtesad, B.; Quintini, C.; Miller, C.; Yerian, L.; Klatte, R. Three-Dimensional Print of a Liver for Preoperative Planning in Living Donor Liver Transplantation. Liver Transplant. 2013, 19, 1304–1310. [Google Scholar] [CrossRef]
- Keating, J.; Newton, A.; Venegas, O.; Nims, S.; Zeh, R.; Predina, J.; Deshpande, C.; Kucharczuk, J.; Nie, S.; Delikatny, E.J.; et al. Near-Infrared Intraoperative Molecular Imaging Can Locate Metastases to the Lung. Ann. Thorac. Surg. 2017, 103, 390–398. [Google Scholar] [CrossRef] [Green Version]
- Schwarz, C.; Plass, I.; Fitschek, F.; Punzengruber, A.; Mittlbock, M.; Kampf, S.; Asenbaum, U.; Starlinger, P.; Stremitzer, S.; Bodingbauer, M.; et al. The value of indocyanine green clearance assessment to predict postoperative liver dysfunction in patients undergoing liver resection. Sci. Rep. 2019, 9, 8421. [Google Scholar] [CrossRef] [Green Version]
- Vlek, S.L.; van Dam, D.A.; Rubinstein, S.M.; de Lange-de Klerk, E.S.M.; Schoonmade, L.J.; Tuynman, J.B.; Meijerink, W.; Ankersmit, M. Biliary tract visualization using near-infrared imaging with indocyanine green during laparoscopic cholecystectomy: Results of a systematic review. Surg. Endosc. 2017, 31, 2731–2742. [Google Scholar] [CrossRef] [Green Version]
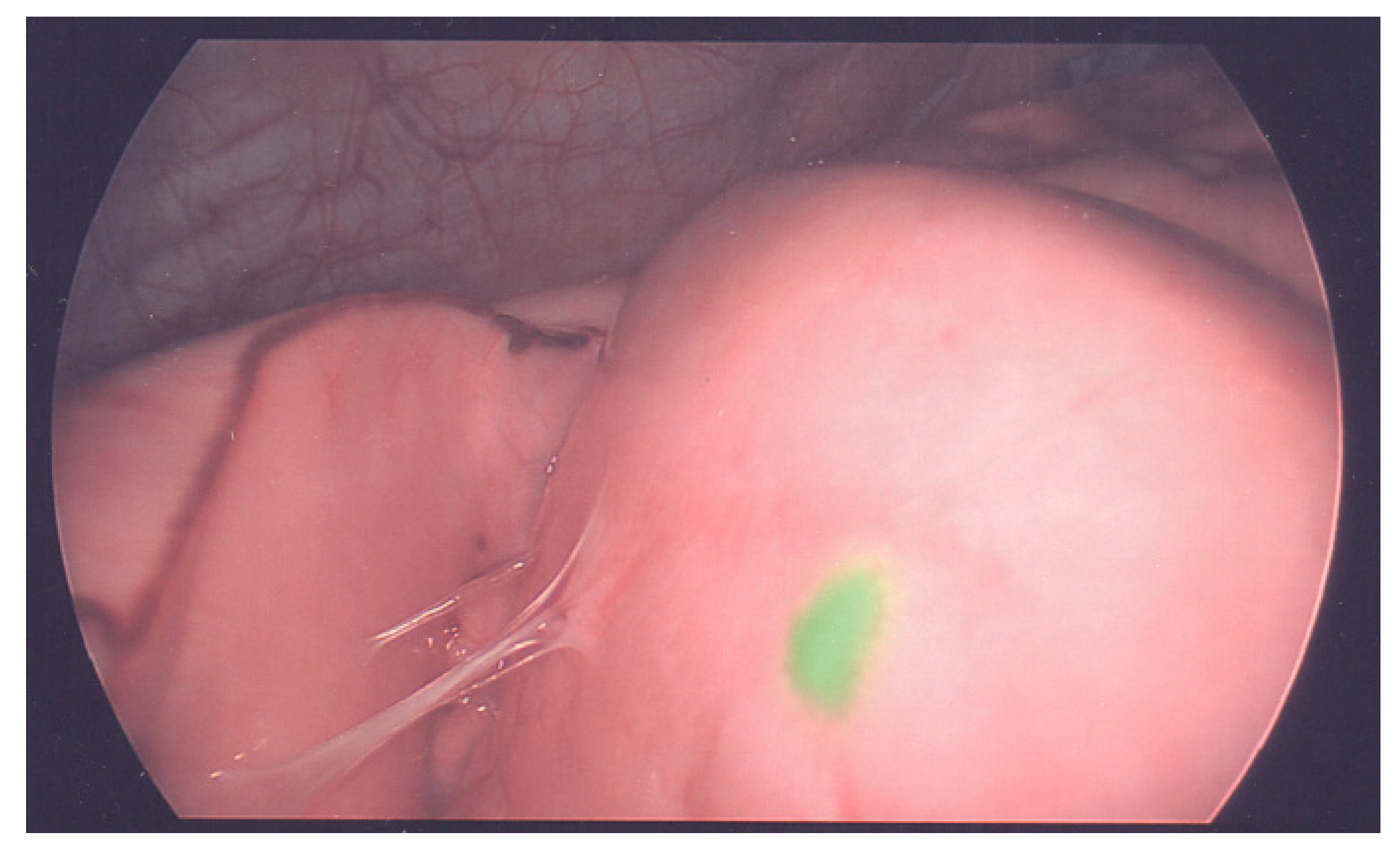
- Nakaseko, Y.; Ishizawa, T.; Saiura, A. Fluorescence-guided surgery for liver tumors. J. Surg. Oncol. 2018, 118, 324–331. [Google Scholar] [CrossRef]
- Kokudo, N.; Ishizawa, T. Clinical application of fluorescence imaging of liver cancer using indocyanine green. Liver Cancer 2012, 1, 15–21. [Google Scholar] [CrossRef]
- Ishizawa, T.; Saiura, A.; Kokudo, N. Clinical application of indocyanine green-fluorescence imaging during hepatectomy. Hepatobiliary Surg. Nutr. 2016, 5, 322–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Souzaki, R.; Kawakubo, N.; Matsuura, T.; Yoshimaru, K.; Koga, Y.; Takemoto, J.; Shibui, Y.; Kohashi, K.; Hayashida, M.; Oda, Y.; et al. Navigation surgery using indocyanine green fluorescent imaging for hepatoblastoma patients. Pediatr. Surg. Int. 2019, 35, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Hoshino, K.; Mori, T.; Kawaida, M.; Abe, K.; Takahashi, N.; Fujimura, T.; Kameyama, K.; Kuroda, T. Metastasectomy of Hepatoblastoma Utilizing a Novel Overlay Fluorescence Imaging System. J. Laparoendosc. Adv. Surg. Tech. A 2018, 28, 1152–1155. [Google Scholar] [CrossRef]
- Yamamichi, T.; Oue, T.; Yonekura, T.; Owari, M.; Nakahata, K.; Umeda, S.; Nara, K.; Ueno, T.; Uehara, S.; Usui, N. Clinical application of indocyanine green (ICG) fluorescent imaging of hepatoblastoma. J. Pediatr. Surg. 2015, 50, 833–836. [Google Scholar] [CrossRef]
- Nguyen, K.T.; Gamblin, T.C.; Geller, D.A. World review of laparoscopic liver resection-2,804 patients. Ann. Surg. 2009, 250, 831–841. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Buell, J.F.; Kaneko, H.; Han, H.S.; Asbun, H.; O’Rourke, N.; Tanabe, M.; Koffron, A.J.; et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann. Surg. 2015, 261, 619–629. [Google Scholar] [CrossRef]
- Cherqui, D.; Lin, C.-W.; Kluger, M. Chapter 105—Minimally invasive techniques in hepatic resection. In Blumgart’s Surgery of the Liver, Biliary Tract and Pancreas, 2-Volume Set, 6th ed.; Jarnagin, W.R., Ed.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 1597–1611. [Google Scholar]
- Kim, T.; Kim, D.Y.; Cho, M.J.; Kim, S.C.; Seo, J.J.; Kim, I.K. Surgery for hepatoblastoma: From laparoscopic resection to liver transplantation. Hepatogastroenterology 2011, 58, 896–899. [Google Scholar]
- Yada, K.; Ishibashi, H.; Mori, H.; Shimada, M. Laparoscopic resection of hepatoblastoma: Report of a case. Asian J. Endosc. Surg. 2014, 7, 267–270. [Google Scholar] [CrossRef]
- Dutta, S.; Nehra, D.; Woo, R.; Cohen, I. Laparoscopic resection of a benign liver tumor in a child. J. Pediatr. Surg. 2007, 42, 1141–1145. [Google Scholar] [CrossRef]
- Fuchs, J. The role of minimally invasive surgery in pediatric solid tumors. Pediatr. Surg. Int. 2015, 31, 213–228. [Google Scholar] [CrossRef]
- Fonseca, A.; Gupta, A.; Shaikh, F.; Ramphal, R.; Ng, V.; McGilvray, I.; Gerstle, J.T. Extreme hepatic resections for the treatment of advanced hepatoblastoma: Are planned close margins an acceptable approach? Pediatr. Blood Cancer 2018, 65. [Google Scholar] [CrossRef] [PubMed]
- Lautz, T.B.; Ben-Ami, T.; Tantemsapya, N.; Gosiengfiao, Y.; Superina, R.A. Successful nontransplant resection of POST-TEXT III and IV hepatoblastoma. Cancer 2011, 117, 1976–1983. [Google Scholar] [CrossRef] [PubMed]
- El-Gendi, A.; Fadel, S.; El-Shafei, M.; Shawky, A. Avoiding liver transplantation in post-treatment extent of disease III and IV hepatoblastoma. Pediatr. Int. 2018, 60, 862–868. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Li, H.; Diao, M.; Chen, L.; Xu, H.; Li, L. Results of surgical resections with positive margins for children with hepatoblastoma: Case series from a single Asian center. Pediatr. Blood Cancer 2019, 66. [Google Scholar] [CrossRef]
- Aronson, D.C.; Weeda, V.B.; Maibach, R.; Czauderna, P.; Dall’Igna, P.; de Ville de Goyet, J.; Branchereau, S.; Perilongo, G.; Brock, P.; Zsiros, J.; et al. Microscopically positive resection margin after hepatoblastoma resection: What is the impact on prognosis? A Childhood Liver Tumours Strategy Group (SIOPEL) report. Eur. J. Cancer 2019, 106, 126–132. [Google Scholar] [CrossRef]
- Hishiki, T.; Watanabe, K.; Ida, K.; Hoshino, K.; Iehara, T.; Aoki, Y.; Kazama, T.; Kihira, K.; Takama, Y.; Taguchi, T.; et al. The role of pulmonary metastasectomy for hepatoblastoma in children with metastasis at diagnosis: Results from the JPLT-2 study. J. Pediatr. Surg. 2017, 52, 2051–2055. [Google Scholar] [CrossRef]
- Wanaguru, D.; Shun, A.; Price, N.; Karpelowsky, J. Outcomes of pulmonary metastases in hepatoblastoma--is the prognosis always poor? J. Pediatr. Surg. 2013, 48, 2474–2478. [Google Scholar] [CrossRef]
- Meyers, R.L.; Katzenstein, H.M.; Krailo, M.; McGahren, E.D., 3rd; Malogolowkin, M.H. Surgical resection of pulmonary metastatic lesions in children with hepatoblastoma. J. Pediatr. Surg. 2007, 42, 2050–2056. [Google Scholar] [CrossRef]
- McDaniel, J.D.; Racadio, J.M.; Patel, M.N.; Johnson, N.D.; Kukreja, K. CT-guided localization of pulmonary nodules in children prior to video-assisted thoracoscopic surgical resection utilizing a combination of two previously described techniques. Pediatr. Radiol. 2018, 48, 626–631. [Google Scholar] [CrossRef]
- Kitagawa, N.; Shinkai, M.; Mochizuki, K.; Usui, H.; Miyagi, H.; Nakamura, K.; Tanaka, M.; Tanaka, Y.; Kusano, M.; Ohtsubo, S. Navigation using indocyanine green fluorescence imaging for hepatoblastoma pulmonary metastases surgery. Pediatr. Surg. Int. 2015, 31, 407–411. [Google Scholar] [CrossRef]
- Semeraro, M.; Branchereau, S.; Maibach, R.; Zsiros, J.; Casanova, M.; Brock, P.; Domerg, C.; Aronson, D.C.; Zimmermann, A.; Laithier, V.; et al. Relapses in hepatoblastoma patients: Clinical characteristics and outcome—Experience of the International Childhood Liver Tumour Strategy Group (SIOPEL). Eur. J. Cancer 2013, 49, 915–922. [Google Scholar] [CrossRef]
- Matsunaga, T.; Sasaki, F.; Ohira, M.; Hashizume, K.; Hayashi, A.; Hayashi, Y.; Mugishima, H.; Ohnuma, N.; Japanese Study Group for Pediatric Liver, T. Analysis of treatment outcome for children with recurrent or metastatic hepatoblastoma. Pediatr. Surg. Int. 2003, 19, 142–146. [Google Scholar] [CrossRef]
- Liberale, G.; Vankerckhove, S.; Caldon, M.G.; Ahmed, B.; Moreau, M.; Nakadi, I.E.; Larsimont, D.; Donckier, V.; Bourgeois, P.; Group, R.; et al. Fluorescence Imaging After Indocyanine Green Injection for Detection of Peritoneal Metastases in Patients Undergoing Cytoreductive Surgery for Peritoneal Carcinomatosis From Colorectal Cancer: A Pilot Study. Ann. Surg. 2016, 264, 1110–1115. [Google Scholar] [CrossRef]
- Takahashi, N.; Yamada, Y.; Hoshino, K.; Kawaida, M.; Mori, T.; Abe, K.; Fujimura, T.; Matsubara, K.; Hibi, T.; Shinoda, M.; et al. Living Donor Liver Re-Transplantation for Recurrent Hepatoblastoma in the Liver Graft following Complete Eradication of Peritoneal Metastases under Indocyanine Green Fluorescence Imaging. Cancers 2019, 11, 730. [Google Scholar] [CrossRef] [Green Version]
- Otte, J.B.; Pritchard, J.; Aronson, D.C.; Brown, J.; Czauderna, P.; Maibach, R.; Perilongo, G.; Shafford, E.; Plaschkes, J. Liver transplantation for hepatoblastoma: Results from the International Society of Pediatric Oncology (SIOP) study SIOPEL-1 and review of the world experience. Pediatr. Blood Cancer 2004, 42, 74–83. [Google Scholar] [CrossRef]
- Sakamoto, S.; Kasahara, M.; Mizuta, K.; Kuroda, T.; Yagi, T.; Taguchi, T.; Inomata, Y.; Umeshita, K.; Uemoto, S. Nationwide survey of the outcomes of living donor liver transplantation for hepatoblastoma in Japan. Liver Transplant. 2014, 20, 333–346. [Google Scholar] [CrossRef]
- Liu, B.; Zhou, L.; Huang, G.; Zhong, Z.; Jiang, C.; Shan, Q.; Xu, M.; Kuang, M.; Xie, X. First Experience of Ultrasound-guided Percutaneous Ablation for Recurrent Hepatoblastoma after Liver Resection in Children. Sci. Rep. 2015, 5. [Google Scholar] [CrossRef] [Green Version]
- Matthew Hawkins, C.; Towbin, A.J.; Roebuck, D.J.; Monroe, E.J.; Gill, A.E.; Thakor, A.S.; Towbin, R.B.; Cahill, A.M.; Lungren, M.P. Role of interventional radiology in managing pediatric liver tumors: Part 2: Percutaneous interventions. Pediatr. Radiol. 2018, 48, 565–580. [Google Scholar] [CrossRef]
- Shi, Y.; Geller, J.I.; Ma, I.T.; Chavan, R.S.; Masand, P.M.; Towbin, A.J.; Chintagumpala, M.; Nuchtern, J.G.; Tiao, G.M.; Thompson, P.A.; et al. Relapsed hepatoblastoma confined to the lung is effectively treated with pulmonary metastasectomy. J. Pediatr. Surg. 2016, 51, 525–529. [Google Scholar] [CrossRef]

| Stage | Definition |
|---|---|
| PRETEXT I | Three contiguous hepatic sections are free of tumor |
| PRETEXT II | One or two sections have tumor involvement, but two adjoining sections are tumor-free |
| PRETEXT III | Two or three sections have tumor involvement, but no two adjoining sections are tumor-free |
| PRETEXT IV | All four sections have tumor involvement |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, T.; Whitlock, R.S.; Vasudevan, S.A. Surgical Management of Hepatoblastoma and Recent Advances. Cancers 2019, 11, 1944. https://doi.org/10.3390/cancers11121944
Yang T, Whitlock RS, Vasudevan SA. Surgical Management of Hepatoblastoma and Recent Advances. Cancers. 2019; 11(12):1944. https://doi.org/10.3390/cancers11121944
Chicago/Turabian StyleYang, Tianyou, Richard S. Whitlock, and Sanjeev A. Vasudevan. 2019. "Surgical Management of Hepatoblastoma and Recent Advances" Cancers 11, no. 12: 1944. https://doi.org/10.3390/cancers11121944





