Botulinum Neurotoxins and Botulism: A Novel Therapeutic Approach
Abstract
:1. Introduction
1.1. Botulinum Neurotoxins (BoNTs)
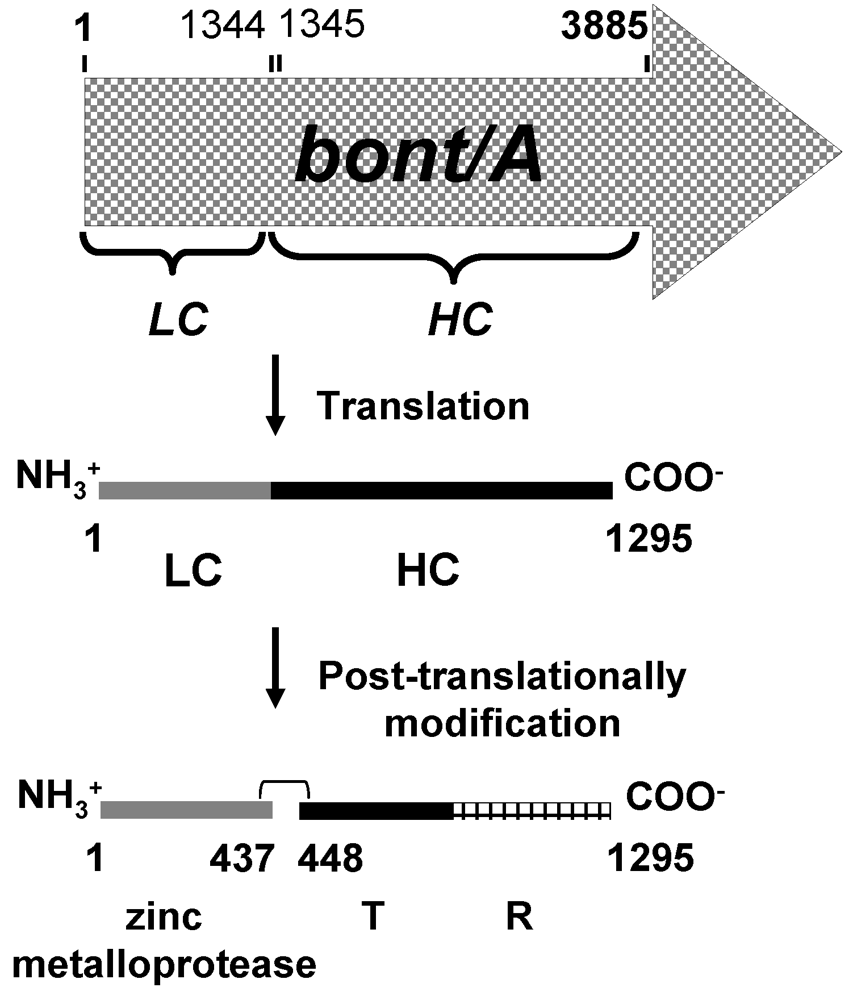
1.2. Synthesis and Molecular Structure of BoNTs
1.3. Mechanism of Action of BoNTs
| BoNT Serotype | SNARE Substrate(s) | Susceptible Scissile Bond | Reference(s) |
|---|---|---|---|
| A | SNAP25 | Gln197-Arg198 | [27,28,29] |
| C | SNAP25 | Arg198-Ala199 | [30,31] |
| Syntaxin | Lys253-Ala254 and Lys260-Ala261 | [25,30,31] | |
| E | SNAP25 | Arg180-Ile181 | [28,29] |
| B | VAMP | Gln76-Phe77 | [32] |
| D | VAMP | Lys59-Leu60 | [28,34] |
| F | VAMP | Gln58-Lys59 | [33,34] |
| G | VAMP | Ala81-Ala82 | [35] |
1.4. Botulism
1.5. Clinical Manifestations of Human Botulism [5,36]
2. Treatment of Botulism
| Preparation | Target BoNT Serotype | Enterpreneur | Status | Reference(s) |
|---|---|---|---|---|
| 1. Trivalent equine antitoxin | A, B, and E | CDC/USA | FDA approved | [36,40] |
| 2. Bivalent equine antitoxin (BAT-AB) | A and B | Sanofi Pasteur Limited | FDA approved | [41,42] |
| 3. Human botulism immune globulin (BabyBIG or BIG-IV) | A,B,C,D, and E | California Department of Public Health | FDA approved | [41,42,43,44] |
| 4. Monovalent equine antitoxin (BAT-E) | E | Sanofi Pasteur Limited | Investigational | [41] |
| 5. Heptavalent equine antitoxin (HBAT) | A to G | Cangene Corporation | Investigational | [41] |
| 6. Recombinant antitoxin | A | University of California, San Francisco | Investigational | [36,45,46,47] |
3. Therapeutic Antibody
3.1. Serum Therapy
3.2. Mouse Monoclonal Antibody
3.3. Chimeric-, Humanized- and Single Chain Antibodies
3.4. Fully Human Monoclonal Antibody
3.5. Single Domain Antibody (sdAb)
4. Molecular Insertion of a Single Domain Antibody (sdAb) into the Enzymatic Groove Directly Inhibits BoNT Zinc Metalloprotease Activity: A Novel and Specific Immunotherapeutic Approach to Botulism
5. Cell Penetrating Antibody (Transbody)
6. Conclusions
Acknowledgments
References
- Sugiyama, H. Clostridium botulinum neurotoxin. Microbiol. Rev. 1980, 44, 419–448. [Google Scholar] [PubMed]
- Gill, D.M. Bacterial toxins: A table of lethal amounts. Microbiol. Rev. 1982, 46, 86–94. [Google Scholar]
- Hatheway, C.L. Toxigenic clostridia. Clin. Microbiol. Rev. 1990, 3, 66–98. [Google Scholar]
- Rotz, L.D.; Khan, A.S.; Lillibridge, S.R.; Ostroff, S.M.; Huhge, J.M. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 2002, 8, 225–230. [Google Scholar]
- Arnon, S.S.; Schechter, R.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Hauer, J.; Layton, M.; Lillibridge, S.; Osterholm, M.T.; O’Toole, T.; Parker, G.; Perl, T.M.; Russell, P.K.; Swerdlow, D.L.; Tonat, K. Botulinum toxin as a biological weapon: Medical and public health management. JAMA 2001, 285, 1059–1070. [Google Scholar]
- Fuginaga, Y.; Matsumura, T.; Jin, Y.; Takegahara, Y.; Sugawara, Y. A novel function of botulinum toxin-associated proteins: HA proteins disrupt intestinal epithelial barrier to increase toxin absorption. Toxicon 2009, 54, 583–586. [Google Scholar]
- Poulain, B.; Popoff, M.R.; Molgo, J. How to botulinum neurotoxins block neurotransmitter release: From botulism to the molecular mechanism of action. The Botulinum J. 2008, 1, 14–56. [Google Scholar]
- Whelan, S.M.; Elmore, M.J.; Bodsworth, N.J.; Brehm, J.K.; Atkinson, T.; Minton, N.P. Molecular cloning of the Clostridium botulinum structural gene encoding the type B neurotoxin and determination of its entire nucleotide sequence. Appl. Environ. Microbiol. 1992, 58, 2345–2354. [Google Scholar] [PubMed]
- Sebaihia, M.; Peck, M.W.; Minton, N.P.; Thomson, N.R.; Holden, M.T.G.; Mitchell, W.J.; Carter, A.T.; Bentley, S.D.; Mason, D.R.; Crossman, L.; et al. Genome sequence of a proteolytic (Group I) Clostridium botulinum strain Hall A and comparative analysis of the clostridial genomes. Genome Res. 2007, 17, 1082–1092. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Iida, H. Conversion of toxigenicity in Clostridium botulinum type C. Jpn. J. Microbiol. 1970, 14, 87–89. [Google Scholar] [PubMed]
- Eklund, M.W.; Poysky, F.T.; Reed, S.M. Bacteriophage and the toxigenicity of Clostridium botulinum type D. Nat. New Biol. 1972, 235, 16–17. [Google Scholar] [PubMed]
- Eklund, M.W.; Poysky, F.T.; Mseitif, L.M.; Strom, M.S. Evidence for plasmid-mediated toxin and bacteriocin production in Clostridium botulinum type G. Appl. Environ. Microbiol. 1988, 54, 1405–1408. [Google Scholar] [PubMed]
- Franciosa, G.; Maugliani, A.; Scalfaro, C.; Aureli, P. Evidence that plasmid-borne botulinum neurotoxin type B genes are widespread among Clostridium botulinum serotype B strains. PLoS ONE 2009, 4, e4829. [Google Scholar] [PubMed]
- Lacy, D.B.; Tepp, W.; Cohen, A.C.; DasGupta, B.R.; Stevens, R.C. Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat. Struct. Biol. 1998, 5, 898–902. [Google Scholar]
- Swaminathan, S.; Eswaramoorthy, S. Structural analysis of the catalytic and binding sites of Clostridium botulinum neurotoxin B. Nat. Struct. Biol. 2000, 7, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Schiavo, G.; Rossetto, O.; Santucci, A.; DasGupta, B.R.; Montecucco, C. Botulinum neurotoxins are zinc protein. J. Biol. Chem. 1992, 267, 23479–23483. [Google Scholar]
- Brunger, A.T.; Rummel, A. Receptor and substrate interactions of clostridial neurotoxins. Toxicon 2009, 54, 550–560. [Google Scholar]
- Thanongsaksrikul, J. Therapeutic Antibodies for Disease Caused by Biological Weapon(s). 2010. [Google Scholar]
- Maksymowych, A.B.; Simpson, L.L. Binding and transcytosis of botulinum neurotoxin by polarized human colon carcinoma cells. J. Biol. Chem. 1998, 273, 21950–21957. [Google Scholar]
- Rummel, A.; Eichner, T.; Weil, T.; Karnath, T.; Gutcaits, A.; Mahrhold, S.; Sandhoff, K.; Proia, R.L.; Acharya, K.R.; Bigalke, H.; Binz, T. Identification of the protein receptor binding site of botulinum neurotoxins B and G proves the double-receptor concept. Proc. Natl. Acad. Sci.USA 2007, 104, 359–364. [Google Scholar]
- Dong, M.; Tepp, W.H.; Liu, H.; Johnson, E.A.; Chapman, E.R. Mechanism of botulinum neurotoxin B and G entry into hippocampal neurons. J. Cell. Biol. 2007, 179, 1511–1522. [Google Scholar]
- Dong, M.; Yeh, F.; Tepp, W.H.; Dean, C.; Johnson, E.A.; Janz, R.; Chapman, E.R. SV2 is the protein receptor for botulinum neurotoxin A. Science 2006, 312, 592–596. [Google Scholar]
- Schmidt, M.F.; Robinson, J.P.; DasGupta, B.R. Direct visualization of botulinum neurotoxin-induced channels in phospholipid vesicles. Nature 1993, 364, 827–830. [Google Scholar]
- Koriazova, L.K.; Montal, M. Translocation of botulinum neurotoxin light chain protease through the heavy chain channel. Nat. Struct. Biol. 2003, 10, 13–18. [Google Scholar]
- Brunger, A.T.; Jin, R.; Breidenbach, M.A. Highly specific interaction between botulinum neurotoxins and synaptic vesicle proteins. Cell. Mol. Life Sci. 2008, 65, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- Schiavo, G.; Matteoli, M.; Montecucco, C. Neurotoxins affecting neuroexocytosis. Physiol. Rev. 2000, 80, 717–766. [Google Scholar]
- Blasi, J.; Chapman, E.R.; Link, E.; Binz, T.; Yamasaki, S.; de Camilli, P.; Südhof, T.C.; Niemann, H.; Jahn, R. Botulinum neurotoxin A selectively cleaves the synapticprotein SNAP-25. Nature 1993, 365, 160–163. [Google Scholar]
- Schiavo, G.; Rossetto, O.; Catsicas, S.; Polverino de Laureto, P.; DasGupta, B.R.; Benfenati, F.; Montecucco, C. Identification of the nerve terminal targets of botulinum neurotoxin serotypes A, D, and E. J. Biol. Chem. 1993, 268, 23784–23787. [Google Scholar] [PubMed]
- Binz, T.; Blasi, J.; Yamasaki, S.; Baumeister, A.; Link, E.; Südhof, T.C.; Jahn, R.; Niemann, H. Proteolysis of SNAP-25 by types E and A botulinal neurotoxins. J. Biol. Chem. 1994, 269, 1617–1620. [Google Scholar]
- Schiavo, G.; Shone, C.C.; Bennett, M.K.; Scheller, R.H.; Montecucco, C. Botulinum neurotoxin type C cleaves a single Lys-Ala bond within the carboxyl-terminal region of syntaxins. J. Biol. Chem. 1995, 270, 10566–10570. [Google Scholar]
- Blasi, J.; Chapman, E.R.; Yamasaki, S.; Binz, T.; Niemann, H.; Jahn, R. Botulinum neurotoxin C1 blocks neurotransmitter release by means of cleaving HPC-1/syntaxin. EMBO J. 1993, 12, 4821–4828. [Google Scholar]
- Schiavo, G.; Benfenati, F.; Poulain, B.; Rossetto, O.; de Laureto, P.P.; DasGupta, B.R.; Montecucco, C. Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin. Nature 1992, 359, 832–835. [Google Scholar]
- Schiavo, G.; Shone, C.C.; Rossetto, O.; Alexander, F.C.; Montecucco, C. Botulinum neurotoxin serotype F is a zinc endopeptidase specific for VAMP/synaptobrevin. J. Biol. Chem. 1993, 268, 11516–11519. [Google Scholar]
- Yamasaki, S.; Baumeister, A.; Binz, T.; Blasi, J.; Link, E.; Cornille, F.; Roques, B.; Fykse, E.M.; Südhof, T.; Jahn, R.; Niemann, H. Cleavage of members of the synaptobrevin/VAMP family by types D and F botulinal neurotoxins and tetanus toxin. J. Biol. Chem. 1994, 269, 12764–12772. [Google Scholar]
- Yamasaki, S.; Binz, T.; Hayashi, T.; Szabo, E.; Yamasaki, N.; Eklund, M.; Jahn, R.; Niemann, H. Botulinum neurotoxin type G proteolyzes the Ala81-Ala82 bond of Rat synaptobrevin 2. Biochem. Biophys. Res. 1994, 200, 829–835. [Google Scholar]
- Emmeluth, D. Botulism (Deadly Disease and Epidemics), 1st ed; Chelsea House Publishers: Broomall, PA, USA, 2005. [Google Scholar]
- Cenci di Bello, I.; Poulain, B.; Shone, C.C.; Tauc, L.; Dolly, J.O. Antagonism of the intracellular action of botulinum neurotoxin type A with monoclonal antibodies that map to light-chain epitopes. Eur. J. Biochem. 1994, 219, 161–169. [Google Scholar]
- Anne, C.; Turcaud, S.; Quancard, J.; Teffo, F.; Meudal, H.; Fournié-Zaluski, M.C.; Roques, B.P. Development of potent inhibitors of botulinum neurotoxin type B. J. Med. Chem. 2003, 46, 4648–4656. [Google Scholar]
- Blommaert, A.; Turcaud, S.; Anne, C.; Roques, B.P. Small tripeptide surrogates with low nanomolar affinity as potent inhibitors of botulinum neurotoxin B metallo-proteolytic activity. Bioorg. Med. Chem. 2004, 12, 3055–3062. [Google Scholar]
- Koenig, M.G. Trivalent botulinus antotoxin. Ann. Intern. Med. 1969, 70, 643–645. [Google Scholar]
- Investigational heptavalent botulinum antitoxin (HBAT) to replace licensed botulinum antitoxin AB and investigational botulinum antitoxin E. MMWR 2010, 59, 299.
- U.S. Food and Drug. Alphabetical List of Licensed Products: Information Updated through February 28, 2011. Available online: http://www.fda.gov/downloads/BiologicsBloodVaccines/UCM149970.pdf (accessed on 27 March 2011).
- Arnon, S.S.; Schechter, R.; Maslanka, S.E.; Jewell, N.P.; Hatheway, C.L. Human botulism immune globulin for the treatment of infant botulism. N. Engl. J. Med. 2006, 354, 462–471. [Google Scholar]
- Arnon, S.S. Creation and development of the public service orphan drug human botulism immune globulin. Pediatrics 2007, 119, 785–789. [Google Scholar]
- Nowakowski, A.; Wang, C.; Powers, D.B.; Amersdorfer, P.; Smith, T.J.; Montgomery, V.A.; Sheridan, R.; Blake, R.; Smith, L.A.; Marks, J.D. Potent neutralization of botulinum neurotoxin by recombinant oligoclonal antibody. Proc. Natl. Acad. Sci. USA 2002, 99, 11346–11350. [Google Scholar]
- Levy, R.; Forsyth, C.M.; LaPorte, S.L.; Geren, I.N.; Smith, L.A.; Marks, J.D. Fine and Domain-level epitope mapping of botulinum neurotoxin type A neutralizing antibodies by yeast surface display. J. Mol. Biol. 2007, 365, 196–210. [Google Scholar]
- Lou, J.; Geren, I.; Garcia-Rodriguez, C.; Forsyth, C.M.; Wen, W.; Knopp, K.; Brown, J.; Smith, T.; Smith, L.A.; Marks, J.D. Affinity maturation of human botulinum neurotoxin antibodies by light chain shuffling via yeast mating. Protein Eng. Des. Sel. 2010, 23, 311–319. [Google Scholar]
- Atassi, M.Z. Immune recognition of BoNTs A and B: how anti-toxin antibodies that bind to the heavy chain obstruct toxin action. Toxicon 2009, 54, 600–613. [Google Scholar]
- Cheng, L.W.; Stanker, L.H.; Henderson, T.D., II; Lou, J.; Marks, J.D. Antibody protection against botulinum neurotoxin intoxication in mice. Infect. Immun. 2009, 77, 4305–4313. [Google Scholar] [CrossRef] [PubMed]
- Keller, M.A.; Stiehm, E.R. Passive immunity in prevention of infectious diseases. Clin. Microbiol. Rev. 2000, 13, 602–614. [Google Scholar]
- Ellis, M.; Chir, B. Human antitetanus serum in the treatment of tetanus. Br. Med. J. 1963, 1, 1123–1126. [Google Scholar]
- Gallagher, J.R. Use of convalescent measles serum to control measles in a preparatory school. Am. J. Public Health Nations Health 1935, 25, 595–598. [Google Scholar]
- Casadevall, A.; Pirofski, L.A. New concepts in antibody-mediated immunity. Infect. Immun. 2004, 72, 6191–6196. [Google Scholar]
- Orange, J.S.; Hossny, E.M.; Weiler, C.R.; Ballow, M.; Berger, M.; Bonilla, F.A.; Buckley, R.; Chinen, J.; El-Gamal, Y.; Mazer, B.D.; Nelson, R.P., Jr.; Patel, D.D.; Secord, E.; Sorensen, R.U.; Wasserman, R.L.; Cunningham-Rundles, C. Use of intravenous immunoglobulin in human disease: A review of evidence by members of the primary immunodeficiency committee of the American academy of allergy, asthma and immunology. J. Allerg. Clin. Immunol. 2006, 117, 525–553. [Google Scholar]
- Deng, Y-Q.; Dai, J-X.; Ji, G-H.; Jiang, T.; Wang, H-J.; Yang, H.; Tan, W-L.; Liu, R.; Yu, M.; Ge, B-X.; Zhu, Q-Y.; Qin, E-D.; Guo, Y-J.; Qin, C-F. A broadly Flavivirus cross-neutralizing monoclonal antibody that recognizes a novel epitope within fushion loop of E protein. PLoS ONE 2011, 6, e16059. [Google Scholar] [PubMed]
- Blanchard, T.G.; Czinn, S.J.; Maurer, R.; Thomas, W.; Soman, G.; Nedrud, J.G. Urease-specific monoclonal antibodies prevent Helicobacter felis infection in mice. Infect. Immun. 1995, 63, 1394–1399. [Google Scholar] [PubMed]
- Colomar, M.; Puga, I.; López, M.; Massot, M.; Jorquera, J.I.; Reina, M.; Vilaró, S.; Espel, E. Neutralization of measles virus infectivity and antibody-dependent cell-mediated cytotoxicity activity against an Epstein-Barr virus-infected cell line by intravenous administration of immunoglobulin G. Clin. Diagn. Lab. Immunol. 2003, 10, 751–756. [Google Scholar]
- Han, Y.; Kozel, T.R.; Zhang, M.X.; MacGill, R.S.; Carroll, M.C.; Cutler, J.E. Complement is essential for protection by an IgM and an IgG3 monoclonal antibody against experimental hematogenously disseminated candidiasis. J. Immunol. 2001, 167, 1550–1557. [Google Scholar]
- Köhler, G.; Milstein, C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 1975, 256, 495–497. [Google Scholar]
- Haurum, J.S. Recombinant polyclonal antibodies: The next generation of antibody therapeutics? Drug Discov. Today 2006, 11, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Casadevall, A.; Scharff, M.D. Return to the past: The case for antibody-based therapies in infectious diseases. Clin. Infect. Dis. 1995, 21, 150–161. [Google Scholar]
- Nelson, A.L.; Reichert, J.M. Development trends for therapeutic antibody fragments. Nat. Biotechnol. 2009, 27, 331–337. [Google Scholar]
- Li, J.; Zhu, Z. Research and development of next generation of antibody-based therapeutics. Acta. Pharmacol. Sin. 2010, 31, 1198–1207. [Google Scholar]
- Mazuet, C.; Dano, J.; Popoff, M.R.; Créminon, C.; Volland, H. Characterization of botulinum neurotoxin type A neutralizing monoclonal antibodies and influence of their half-lives on therapeutic activity. PLoS ONE 2010, 5, e12416. [Google Scholar]
- Köhler, G. Immunoglobulin chain loss in hybridoma lines. Proc. Natl. Acad. Sci. USA 1980, 77, 2197–2199. [Google Scholar]
- Courtenay-Luck, N.S.; Epenetos, A.A.; Winearls, C.G.; Ritter, M.A. Preexisting human anti-murine immunoglobulin reactivity due to polyclonal rheumatoid factors. Cancer Res. 1987, 47, 4520–4525. [Google Scholar]
- Tjandra, J.J.; Ramadi, L.; McKenzie, I.F.C. Development of human anti-murine antibody (HAMA) response in patients. Immunol. Cell Biol. 1990, 68, 367–376. [Google Scholar]
- Losman, M.J.; DeJager, R.L.; Monostier, M.; Sharkey, R.M.; Goldenberg, D.M. Human immune response to anti-carcinoembryonic antigen murine monoclonal antibodies. Cancer Res. 1990, 1, 1055–1058. [Google Scholar]
- Morrison, S.L.; Johnson, M.J.; Herzenberg, L.A.; Oi, V.T. Chimeric human antibody molecules: Mouse antigen-binding domains with human constant region domains. Proc. Natl. Acad. Sci. USA 1984, 81, 6851–6855. [Google Scholar]
- Stern, M.; Herrmann, R. Overview of monoclonal antibodies in cancer therapy: Present and promise. Crit. Rev. Oncol. Hematol. 2005, 54, 11–29. [Google Scholar]
- Normann, S.J. Why antibody inhibits vascular clearance of staphylococcal enterotoxin B. J. Immunol. 1970, 104, 673–678. [Google Scholar]
- Devaux, C.; Moreau, E.; Goyffon, M.; Rochat, H.; Billiald, P. Construction and functional evaluation of a single-chain antibody fragment that neutralizes toxin AahI from the venom of the scorpion Androctonus australis hector. Eur. J. Biochem. 2001, 268, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Christensen, E.I.; Verrous, P.J.; Nielsen, R. Receptor-mediated endocytosis in renal proximal tubule. Pflug. Arch. Eur. J. Phys. 2009, 458, 1039–1048. [Google Scholar]
- Riechmann, L.; Clark, M.; Waldmann, H.; Winter, G. Reshaping human antibodies for therapy. Nature 1988, 332, 323–327. [Google Scholar]
- Maneewatch, S.; Sakolvaree, Y.; Tapchaisri, P.; Saengjaruk, P.; Songserm, T.; Wongratanachewin, S.; Tongtawe, P.; Srimanote, P.; Chaisri, U.; Chaicumpa, W. Humanized-monoclonal antibody against heterologous Leptospira infection. Protein Eng. Des. Sel. 2009, 22, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Reichert, J.; Pavlou, A. Monoclonal antibodies market. Nat. Rev. Drug Discov. 2004, 3, 383–384. [Google Scholar]
- Brüggemannand, M.; Taussig, M.J. Production of human antibody repertoires in transgenic mice. Curr. Opin. Biotechnol. 1997, 8, 455–458. [Google Scholar]
- Chiorazzi, N.; Wasserman, R.L.; Kunkel, H.G. Use of Epstein-Barr virus-transformed B cell lines for the generation of immunoglobulin-producing human B cell hybridomas. J. Exp. Med. 1982, 156, 930–935. [Google Scholar]
- Rosen, A.; Persson, K.; Klein, G. Human monoclonal antibodies to a genus-specific chlamydial antigen produced by EBV-transformed B cells. J. Immunol. 1983, 130, 2899–2902. [Google Scholar]
- Garzelli, C.; Puglisi, C.; Falcone, G. Human monoclonal antibody to purified protein derivative of tuberculin produced by hybrids constructed with Epstein-Barr virus-transformed B lymphocytes and mouse myeloma cells. Eur. J. Immunol. 1986, 16, 584–587. [Google Scholar]
- Foung, S.K.H.; Perkins, S.; Raubitschek, A.; Larrick, J.; Lizak, G.; Fishwild, D.; Engleman, E.G.; Grumet, F.C. Rescue of human monoclonal antibody production from an EBV-transformed B cell line by fusion to a human-mouse hybridoma. J. Immunol. Methods 1984, 70, 83–90. [Google Scholar]
- Goldsby, R.A.; Kindt, T.J.; Osborne, B.A. Kuby Immunology, 5th ed; W.H. Freeman and Company: New York, NY, USA, 2003; Chapter 5. [Google Scholar]
- Maizels, N. Immunoglobulin gene diversification. Annu. Rev. Genet. 2005, 39, 23–46. [Google Scholar]
- Boder, E.T.; Wittrup, K.D. Yeast surface display for screening combinatorial polypeptide libraries. Nat. Biotechnol. 1997, 15, 553–557. [Google Scholar]
- Daugherty, P.S.; Olsen, M.J.; Iverson, B.L.; Georgiou, G. Development of an optimized expression system for the screening of antibody libraries displayed on the Escherichia coli surface. Protein Eng. 1999, 12, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Beerli, R.R.; Bauer, M.; Buser, R.B.; Gwerder, M.; Muntwiler, S.; Maurer, P.; Saudan, P.; Bachmann, M.F. Isolation of human monoclonal antibodies by mammalian cell display. Proc. Natl. Acad. Sci. USA 2008, 105, 14336–14341. [Google Scholar]
- Hanes, J.; Plückthun, A. In vitro selection and evolution of functional proteins by using ribosome display. Proc. Natl. Acad. Sci. USA 1997, 94, 4937–4942. [Google Scholar]
- Smith, G.P. Filamentous fusion phage: Novel expression vectors that display cloned antigens on the virion surface. Science 1985, 228, 1315–1317. [Google Scholar]
- Hoogenboom, H.R. Selecting and screening recombinant antibody libraries. Nat. Biotechnol. 2005, 23, 1105–1116. [Google Scholar]
- Kulkeaw, K.; Sakolvaree, Y.; Srimanote, P.; Tongtawe, P.; Maneewatch, S.; Sookrung, N.; Tungtrongchitr, A.; Tapchaisri, P.; Kurazono, H.; Chaicumpa, W. Human monoclonal ScFv neutralize lethal Thai cobra, Naja kaouthia, neurotoxin. J. Proteomics 2009, 72, 270–282. [Google Scholar] [CrossRef] [PubMed]
- Hoogenboom, H.R. Overview of antibody phage-display technology and its applications. In Antibody Phage Display: Methods and Protocols; O’Brien, P.M., Aitken, R., Eds.; Humana Press Inc.: Totowa, NJ, USA, 2002; pp. 1–37. [Google Scholar]
- Sidhu, S.S.; Fellouse, F.A. Synthetic therapeutic antibodies. Nat. Chem. Biol. 2006, 2, 682–688. [Google Scholar]
- Winter, G.; Griffiths, A.D.; Hawkins, R.E.; Hoogenboom, H.R. Making antibodies by phage display technology. Annu. Rev. Immunol. 1994, 12, 433–455. [Google Scholar]
- de Haard, H.J.; Kazemier, B.; van der Bent, A.; Oudshoorn, P.; Boender, P.; van Gemen, B.; Arends, J.W.; Hoogenboom, H.R. Absolute conservation of residue 6 of immunoglobulin heavy chain regions of class IIA is required for correct folding. Protein Eng. 1998, 11, 1267–1276. [Google Scholar] [PubMed]
- Maneewatch, S.; Thanongsaksrikul, J.; Songserm, T.; Theung-In, K.; Kulkeaw, K.; Thathisong, U.; Srimanote, P.; Tongtawe, P.; Tapchaisri, P.; Chaicumpa, W. Human single-chain antibodies that neutralize homologous and heterologous strains and clades of influenza A virus subtype H5N1. Antivir. Ther. 2009, 14, 221–230. [Google Scholar] [PubMed]
- Poungpair, O.; Chaicumpa, W.; Kulkeaw, K.; Maneewatch, S.; Theung-In, K.; Srimanote, P.; Tongtawe, P.; Songserm, T.; Lekcharoensuk, P.; Tapchaisri, P. Human single chain monoclonal antibody that recognizes matrix protein of heterologous influenza A virus subtype. J. Virol. Methods 2009, 159, 105–111. [Google Scholar]
- Thanongsaksrikul, J.; Srimanote, P.; Maneewatch, S.; Choowongkomon, K.; Tapchaisri, P.; Makino, S.; Kurazono, H.; Chaicumpa, W. A VHH that neutralizes the zinc metalloproteinase activity of botulinum neurotoxin type A. J. Biol. Chem. 2010, 285, 9657–9666. [Google Scholar] [PubMed]
- Joosten, V.; Lokman, C.; van den Hondel, C.A.; Punt, P.J. The production of antibody fragments and antibody fusion proteins by yeasts and filamentous fungi. Microb. Cell. Fact. 2003, 2, 1–15. [Google Scholar]
- Hamers-Casterman, C.; Atarhouch, T.; Muyldermans, S.; Robinson, G.; Hamers, C.; Songa, E.B.; Bendahman, N.; Hamers, R. Naturally occurring antibodies devoid of light chains. Nature 1993, 363, 446–448. [Google Scholar]
- Davies, J.; Riechmann, L. Camelising human antibody fragments: NMR studies on VH domains. FEBS Lett. 1994, 339, 285–290. [Google Scholar]
- Muyldermans, S.; Atarhouch, T.; Saldanha, J.; Barbosa, J.A.; Hamers, R. Sequence and structure of VH domain from naturally occurring camel heavy chain immunoglobulins lacking light chains. Protein Eng. 1994, 7, 1129–1135. [Google Scholar]
- Nguyen, V.K.; Hamers, R.; Muyldermans, S. Camel heavy-chain antibodies: Diverse germline V(H)H and specific mechanisms enlarge the antigen-binding repertoire. EMBO J. 2000, 19, 921–930. [Google Scholar]
- Conrath, K.E.; Wernery, U.; Muyldermans, S.; Nguyen, V.K. Emergence and evolution of functional heavy-chain antibodies in Camelidae. Dev. Comp. Immunol. 2003, 27, 87–103. [Google Scholar]
- Wu, T.T.; Johnson, G.; Kabat, E.A. Length distribution of CDRH3 in antibodies. Proteins 1993, 16, 1–7. [Google Scholar]
- Muyldermans, S. Single domain camel antibodies: Current status. J. Biotechnol. 2001, 74, 277–302. [Google Scholar]
- Desmyter, A.; Decanniere, K.; Muyldermans, S.; Wyns, L. Antigen specificity and high affinity binding provided by one single loop of a camel single-domain antibody. J. Biol. Chem. 2001, 276, 26285–26290. [Google Scholar]
- de Genst, E.; Silence, K.; Decannierer, K.; Conrath, K.; Loris, R.; Kinne, J.; Muyldermans, S.; Wyns, L. Molecular basis for the preferential cleft recognition by dromedary heavy-chain antibodies. Proc. Natl. Acad. Sci. USA 2006, 103, 4586–4591. [Google Scholar]
- Lauwereys, M.; Ghahroudi, M.A.; Desmyter, A.; Kinne, J.; Holzer, W.; de Genst, E.; Wyn, L.; Muyldermans, S. Potent enzyme inhibitors derived from dromedary heavy-chain antibodies. EMBO J. 1998, 17, 3512–3520. [Google Scholar]
- Conrath, K.E.; Lauwereys, M.; Galleni, M.; Matagne, A.; Frere, J.M.; Kinne, J.; Wyn, L.; Muyldermans, S. β-lactamase inhibitors derived from single-domain antibody fragments elicited in the Camelidae. Antimicrob. Agents Chemother. 2001, 45, 2807–2812. [Google Scholar] [CrossRef] [PubMed]
- Ghahroudi, M.A.; Desmyter, A.; Wyns, L.; Hamers, R.; Muyldermans, S. Selection and identification of single domain antibody fragments from camel heavy-chain antibodies. FEBS Lett. 1997, 414, 521–526. [Google Scholar]
- Harmsen, M.M.; de Haard, H.J. Properties, production, and applications of camelid single-domain antibody fragments. Appl. Microbiol. Biotechnol. 2007, 77, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Chulanetra, M.; Chaicumpa, W. Human antibody that neutralizes tetrodotoxin. Mahidol University, Thailand. Unpublished work, 2011.
- Muyldermans, S.; Cambillau, C.; Wyns, L. Recognition of antigens by single domain antibody fragments: The superfluous luxury of paired domains. TIBS 2001, 26, 230–235. [Google Scholar]
- Dong, J.; Thompson, A.A.; Fan, Y.; Lou, J.; Conrad, F.; Ho, M.; Pires-Alves, M.; Wilson, B.A.; Stevens, R.C.; Marks, J.D. A single-domain llama antibody potently inhibits the enzymatic activity of botulinum neurotoxin by binding to the non-catalytic α-exosite binding region. J. Mol. Biol. 2010, 397, 1106–1118. [Google Scholar]
- Conway, J.O.; Sherwood, L.J.; Collazo, M.T.; Garza, J.A.; Hayhurst, A. Llama single domain antibodies specific for the 7 botulinum neurotoxin serotypes as heptaplex immunoreagents. PLoS ONE 2010, 5, e8818. [Google Scholar]
- Derossi, D.; Joliot, A.H.; Chassaing, G.; Prochiantz, A. The third helix of the Antennapedia homeodomain translocates through biological membranes. J. Biol. Chem. 1994, 269, 10444–10450. [Google Scholar]
- Pooga, M.; Hallbrink, M.; Zorko, M.; Langel, U. Cell penetration by transpotan. FASEB J. 1998, 12, 67–77. [Google Scholar]
- Poungpair, O.; Pootong, A.; Maneewatch, S.; Srimanote, P.; Tongtawe, P.; Songserm, T.; Tapchaisri, P.; Chaicumpa, W. A human single chain transbody specific to matrix protein (M1) interferes with the replication of Influenza A virus. Bioconjugate Chem. 2010, 21, 1134–1141. [Google Scholar] [CrossRef]
- Noguchi, H.; Matsumoto, S. Protein transduction technology: A novel therapeutic perspective. Acta Med. Okayama 2006, 60, 1–11. [Google Scholar]
- Lundberg, M.; Johansson, M. Is VP22 nuclear homing an artifact? Nat. Biotechnol. 2001, 19, 713–714. [Google Scholar] [CrossRef] [PubMed]
- Letoha, T.; Gaal, S.; Somlai, C.; Czajlik, A.; Perczel, A.; Penke, B. Membrane translocation of penetratin and its derivatives in different cell lines. J. Mol. Recognit. 2003, 16, 272–279. [Google Scholar]
- Saalik, P.; Elmquist, A.; Hansen, M.; Padari, K.; Saar, K.; Viht, K.; Langel, U.; Pooga, M. Protein cargo delivery properties of cell-penetrating peptides: A comparative study. Bioconjugate Chem. 2004, 15, 1246–1253. [Google Scholar] [CrossRef]
- Kaplan, I.M.; Wadia, J.S.; Dowdy, S.F. Cationic TAT peptide transduction domain enters cells by macropinocytosis. J. Control. Release 2005, 102, 247–253. [Google Scholar]
- Richard, J.P.; Melikov, K.; Brooks, H.; Prevot, P.; Lebleu, B.; Chernomordik, L.V. Cellular uptake of unconjugated TAT peptide involves clathrin-dependent endocytosis and heparin sulfate receptors. J. Biol. Chem. 2005, 280, 15300–15306. [Google Scholar]
- Morris, M.C.; Deshayes, S.; Heitz, F.; Divita, G. Cell-penetrating peptides: From molecular mechanisms to therapeutics. Biol. Cell 2008, 100, 201–217. [Google Scholar]
- Raha, S.; Paunesku, T.; Woloschak, G. Peptide-mediated cancer targeting of nanoconjugates. WIREs Nanomed. Nanobiotechnol. 2010, 3, 269–281. [Google Scholar]
- Deshayes, S.; Morris, M.C.; Divita, G.; Heitz, F. Cell-penetrating peptides: Tools for intracellular delivery of therapeutics. Cell Mol. Life Sci. 2005, 62, 1839–1849. [Google Scholar]
© 2011 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Thanongsaksrikul, J.; Chaicumpa, W. Botulinum Neurotoxins and Botulism: A Novel Therapeutic Approach. Toxins 2011, 3, 469-488. https://doi.org/10.3390/toxins3050469
Thanongsaksrikul J, Chaicumpa W. Botulinum Neurotoxins and Botulism: A Novel Therapeutic Approach. Toxins. 2011; 3(5):469-488. https://doi.org/10.3390/toxins3050469
Chicago/Turabian StyleThanongsaksrikul, Jeeraphong, and Wanpen Chaicumpa. 2011. "Botulinum Neurotoxins and Botulism: A Novel Therapeutic Approach" Toxins 3, no. 5: 469-488. https://doi.org/10.3390/toxins3050469




