Effect of 12-Week Vitamin D Supplementation on 25[OH]D Status and Performance in Athletes with a Spinal Cord Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Design
2.3. Vitamin D Supplementation
2.4. The Isokinetic Dynamometer Test
2.5. The Wingate Test
2.6. Blood Parameters
2.7. DASH Questionnaire
2.8. Data Analysis
3. Results
3.1. Vitamin D and Calcium Status
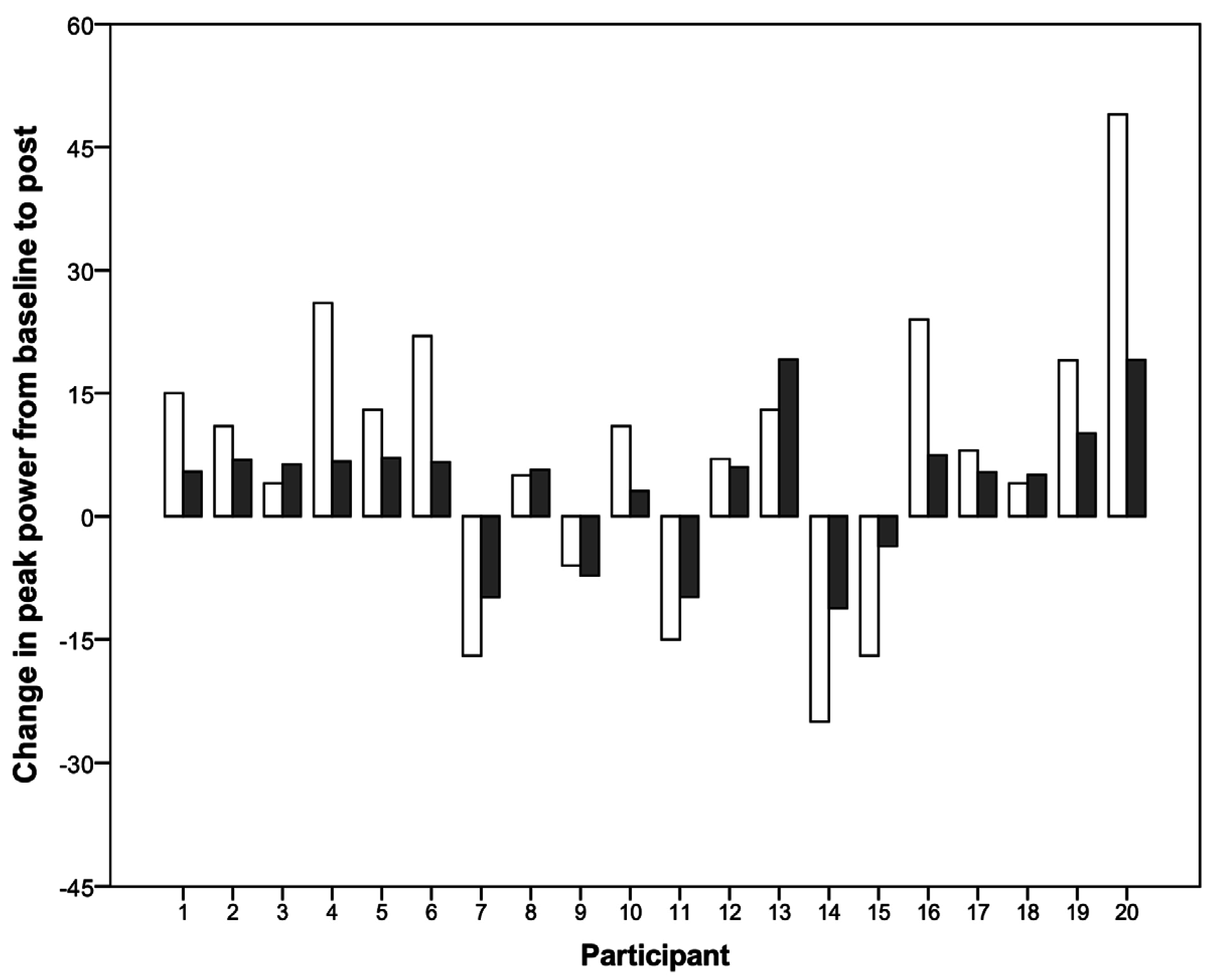
3.2. Performance Tests
3.3. Other Outcome Parameters
4. Discussion
4.1. Vitamin D Status
4.2. Vitamin D and Muscle Performance
4.3. Other Parameters
4.4. Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ward, K.A.; Das, G.; Berry, J.L.; Roberts, S.A.; Rawer, R.; Adams, J.E.; Mughal, Z. Vitamin D status and muscle function in post-menarchal adolescent girls. J. Clin. Endocrinol. Metab. 2009, 94, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Carroll, A.; Onwuneme, C.; McKenna, M.J.; Mayne, P.D.; Molloy, E.J.; Murphy, N.P. Vitamin D status in irish children and adolescents: Value of fortification and supplementation. Clin. Pediatr. (Phila.) 2014, 53, 1345–1351. [Google Scholar] [CrossRef] [PubMed]
- Bruyere, O.; Cavalier, E.; Souberbielle, J.C.; Bischoff-Ferrari, H.A.; Beaudart, C.; Buckinx, F.; Reginster, J.Y.; Rizzoli, R. Effects of vitamin D in the elderly population: Current status and perspectives. Arch. Public Health 2014, 72, 32. [Google Scholar] [CrossRef] [PubMed]
- Constantini, N.W.; Arieli, R.; Chodick, G.; Dubnov-Raz, G. High prevalence of vitamin D insufficiency in athletes and dancers. Clin. J. Sport Med. 2010, 20, 368–371. [Google Scholar] [CrossRef] [PubMed]
- Farrokhyar, F.; Tabasinejad, R.; Dao, D.; Peterson, D.; Ayeni, O.R.; Hadioonzadeh, R.; Bhandari, M. Prevalence of vitamin D inadequacy in athletes: A systematic-review and meta-analysis. Sports Med. 2015, 45, 365–378. [Google Scholar] [CrossRef] [PubMed]
- Garland, C.F.; Gorham, E.D.; Mohr, S.B.; Grant, W.B.; Giovannucci, E.L.; Lipkin, M.; Newmark, H.; Holick, M.F.; Garland, F.C. Vitamin D and prevention of breast cancer: Pooled analysis. J. Steroid Biochem. Mol. Biol. 2007, 103, 708–711. [Google Scholar] [CrossRef] [PubMed]
- Wong, G.; Lim, W.H.; Lewis, J.; Craig, J.C.; Turner, R.; Zhu, K.; Lim, E.M.; Prince, R. Vitamin D and cancer mortality in elderly women. BMC Cancer 2015, 15, 106. [Google Scholar] [CrossRef] [PubMed]
- Berridge, M.J. Vitamin D cell signalling in health and disease. Biochem. Biophys. Res. Commun. 2015, 460, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Mandarino, N.R.; Junior, F.; Salgado, J.V.; Lages, J.S.; Filho, N.S. Is vitamin D deficiency a new risk factor for cardiovascular disease? Open Cardiovasc. Med. J. 2015, 9, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Annweiler, C.; Rolland, Y.; Schott, A.M.; Blain, H.; Vellas, B.; Herrmann, F.R.; Beauchet, O. Higher vitamin D dietary intake is associated with lower risk of alzheimer’s disease: A 7-year follow-up. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Larson-Meyer, D.E.; Willis, K.S. Vitamin D and athletes. Curr. Sports Med. Rep. 2010, 9, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Norman, A.W.; Okamura, W.H.; Bishop, J.E.; Henry, H.L. Update on biological actions of 1alpha,25(OH)2-vitamin D3 (rapid effects) and 24R,25(OH)2-vitamin D3. Mol. Cell. Endocrinol. 2002, 197, 1–13. [Google Scholar] [CrossRef]
- Girgis, C.M.; Clifton-Bligh, R.J.; Hamrick, M.W.; Holick, M.F.; Gunton, J.E. The roles of vitamin D in skeletal muscle: Form, function, and metabolism. Endocr. Rev. 2013, 34, 33–83. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Buckinx, F.; Rabenda, V.; Gillain, S.; Cavalier, E.; Slomian, J.; Petermans, J.; Reginster, J.Y.; Bruyere, O. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: A systematic review and meta-analysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 2014, 99, 4336–4345. [Google Scholar] [CrossRef] [PubMed]
- Ceglia, L.; Harris, S.S. Vitamin D and its role in skeletal muscle. Calcif. Tissue Int. 2013, 92, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Muir, S.W.; Montero-Odasso, M. Effect of vitamin D supplementation on muscle strength, gait and balance in older adults: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2011, 59, 2291–2300. [Google Scholar] [CrossRef] [PubMed]
- Stockton, K.A.; Mengersen, K.; Paratz, J.D.; Kandiah, D.; Bennell, K.L. Effect of vitamin D supplementation on muscle strength: A systematic review and meta-analysis. Osteoporos. Int. 2011, 22, 859–871. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, P.B.; Joseph, C.; Angioi, M. Effects of vitamin D supplementation on upper and lower body muscle strength levels in healthy individuals. A systematic review with meta-analysis. J. Sci. Med. Sport 2015, 18, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Halfon, M.; Phan, O.; Teta, D. Vitamin D: A review on its effects on muscle strength, the risk of fall, and frailty. BioMed Res. Int. 2015, 2015, 953241. [Google Scholar] [CrossRef] [PubMed]
- Dubnov-Raz, G.; Livne, N.; Raz, R.; Cohen, A.H.; Constantini, N.W. Vitamin D supplementation and physical performance in adolescent swimmers. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Jastrzebska, M.; Kaczmarczyk, M.; Jastrzebski, Z. The effect of vitamin D supplementation on training adaptation in well trained soccer players. J. Strength Cond. Res. 2016, 30, 2648–2655. [Google Scholar] [CrossRef] [PubMed]
- Close, G.L.; Leckey, J.; Patterson, M.; Bradley, W.; Owens, D.J.; Fraser, W.D.; Morton, J.P. The effects of vitamin D(3) supplementation on serum total 25[OH]D concentration and physical performance: A randomised dose-response study. Br. J. Sports Med. 2013, 47, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Wyon, M.A.; Koutedakis, Y.; Wolman, R.; Nevill, A.M.; Allen, N. The influence of winter vitamin D supplementation on muscle function and injury occurrence in elite ballet dancers: A controlled study. J. Sci. Med. Sport 2014, 17, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Nemunaitis, G.A.; Mejia, M.; Nagy, J.A.; Johnson, T.; Chae, J.; Roach, M.J. A descriptive study on vitamin D levels in individuals with spinal cord injury in an acute inpatient rehabilitation setting. PM&R 2010, 2, 202–208. [Google Scholar]
- Flueck, J.L.; Hartmann, K.; Strupler, M.; Perret, C. Vitamin D deficiency in swiss elite wheelchair athletes. Spinal Cord 2016. [Google Scholar] [CrossRef] [PubMed]
- Pritchett, K.; Pritchett, R.; Ogan, D.; Bishop, P.; Broad, E.; LaCroix, M. 25(OH)D status of elite athletes with spinal cord injury relative to lifestyle factors. Nutrients 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Magee, P.J.; Pourshahidi, L.K.; Wallace, J.M.; Cleary, J.; Conway, J.; Harney, E.; Madigan, S.M. Vitamin D status and supplementation in elite irish athletes. Int. J. Sport Nutr. Exerc. Metab. 2013, 23, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Germann, G.; Harth, A.; Wind, G.; Demir, E. Standardisation and validation of the german version 2.0 of the disability of arm, shoulder, hand (DASH) questionnaire. Unfallchirurg 2003, 106, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Plichta, S.B.; Kelvin, E.A.; Munro, B.H. Munro’s Statistical Methods for Health Care Research, 6th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2013; p. 567. [Google Scholar]
- Jacobs, P.L.; Mahoney, E.T.; Johnson, B. Reliability of arm wingate anaerobic testing in persons with complete paraplegia. J. Spinal Cord Med. 2003, 26, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, P.L.; Johnson, B.; Somarriba, G.A.; Carter, A.B. Reliability of upper extremity anaerobic power assessment in persons with tetraplegia. J. Spinal Cord Med. 2005, 28, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Brunner, E.; Langer, F. Nichtparametrische Analyse Longitudinaler Daten; R. Oldenbourg Verlag: München, Germany, 1999; p. 237S. [Google Scholar]
- Quadri, A.; Gojanovic, B.; Noack, P.; Fuhrer, C.; Steuer, C.; Huber, A.; Kriemler, S. Seasonal Variation of Vitamin D Levels in Swiss Athletes; Swiss Sports & Exercise Medicine: Bern, Switzerland, 2016; Volume 64, p. 24. [Google Scholar]
- Barger-Lux, M.J.; Heaney, R.P.; Dowell, S.; Chen, T.C.; Holick, M.F. Vitamin D and its major metabolites: Serum levels after graded oral dosing in healthy men. Osteoporos Int. 1998, 8, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P.; Davies, K.M.; Chen, T.C.; Holick, M.F.; Barger-Lux, M.J. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am. J. Clin. Nutr. 2003, 77, 204–210. [Google Scholar] [PubMed]
- Bauman, W.A.; Emmons, R.R.; Cirnigliaro, C.M.; Kirshblum, S.C.; Spungen, A.M. An effective oral vitamin d replacement therapy in persons with spinal cord injury. J. Spinal Cord Med. 2011, 34, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Bauman, W.A.; Morrison, N.G.; Spungen, A.M. Vitamin D replacement therapy in persons with spinal cord injury. J. Spinal Cord Med. 2005, 28, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Oleson, C.V.; Seidel, B.J.; Zhan, T. Association of vitamin D deficiency, secondary hyperparathyroidism, and heterotopic ossification in spinal cord injury. J. Rehabil. Res. Dev. 2013, 50, 1177–1186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, R.; Sharma, U.; Gupta, N.; Kalaivani, M.; Singh, U.; Guleria, R.; Jagannathan, N.R.; Goswami, R. Effect of cholecalciferol and calcium supplementation on muscle strength and energy metabolism in vitamin D-deficient asian indians: A randomized, controlled trial. Clin. Endocrinol. (Oxf.) 2010, 73, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Wyon, M.A.; Wolman, R.; Nevill, A.M.; Cloak, R.; Metsios, G.S.; Gould, D.; Ingham, A.; Koutedakis, Y. Acute effects of vitamin D3 supplementation on muscle strength in judoka athletes: A randomized placebo-controlled, double-blind trial. Clin. J. Sport Med. 2016, 26, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, B.; Whiteley, R.; Farooq, A.; Chalabi, H. Vitamin D concentration in 342 professional football players and association with lower limb isokinetic function. J. Sci. Med. Sport 2014, 17, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Iwamoto, J.; Kanoko, T.; Satoh, K. Low-dose vitamin D prevents muscular atrophy and reduces falls and hip fractures in women after stroke: A randomized controlled trial. Cerebrovasc. Dis. 2005, 20, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Schantz, P.; Sjoberg, B.; Widebeck, A.M.; Ekblom, B. Skeletal muscle of trained and untrained paraplegics and tetraplegics. Acta Physiol. Scand. 1997, 161, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Redzic, M.; Lewis, R.M.; Thomas, D.T. Relationship between 25-hydoxyvitamin D, muscle strength, and incidence of injury in healthy adults: A systematic review. Nutr. Res. 2013, 33, 251–258. [Google Scholar] [CrossRef] [PubMed]



| Participant | Training (h/Week) | Age (Years) | Height (cm) | Weight (kg) | Lesion Level | AIS | Sport | Classification | Follow up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 3.5 | 37 | 185 | 103 | C7 | D | WR | 2.0 | Yes |
| 2 | 11.0 | 20 | 170 | 54 | C6 | A | WR | 1.5 | No |
| 3 | 4.0 | 24 | 179 | 58 | C6 | B | WR | 0.5 | Yes |
| 4 | 3.5 | 35 | 187 | 97 | T4 | A | WB | 1.0 | No |
| 5 | 4.0 | 47 | 185 | 63 | T1 | A | WR | 2.5 | No |
| 6 | 2.5 | 27 | 180 | 70 | T4 | A | WB | 1.0 | Yes |
| 7 | 3.5 | 27 | 181 | 61 | C6 | B | WR | 2.5 | No |
| 8 | 5.0 | 48 | 186 | 67 | C6 | B | WR | 1.0 | Yes |
| 9 | 5.0 | 44 | 176 | 80 | C6 | A | WR | 0.5 | Yes |
| 10 | 12.0 | 35 | 193 | 92 | T1 | C | WB | 2.5 | Yes |
| 11 | 8.0 | 38 | 172 | 70 | C7 | D | WR | 2.0 | Yes |
| 12 | 4.0 | 26 | 188 | 90 | C6 | A | WR | 0.5 | No |
| 13 | 5.0 | 30 | 182 | 65 | C6 | B | WR | 0.5 | No |
| 14 | 8.0 | 34 | 180 | 85 | C5 | C | WR | 1.5 | No |
| 15 | 6.5 | 50 | 185 | 83 | L3 | A | WB | 3.0 | Yes |
| 16 | 13.5 | 21 | 184 | 63 | C7 | D | WR | 2.5 | Yes |
| 17 | 3.5 | 65 | 175 | 65 | C6 | C | WR | 1.5 | No |
| 18 | 15.0 | 33 | 180 | 60 | C6 | A | PT | class 1 | No |
| 19 | 4.0 | 26 | 155 | 52 | CP | - | WR | 1.5 | Yes |
| 20 | 5.0 | 57 | 170 | 72 | T5 | D | PT | class 4 | No |
| Mean ± SD | 6.3 ± 3.7 | 36 ± 12 | 180 ± 8 | 72 ± 15 | - | - | - | - | - |
| Mode | Arm | Baseline | Intermediate | Post | p-Value |
|---|---|---|---|---|---|
| isometric | dominant | 65 [46; 96] | 71 [46; 98] | 72 [50; 100] | 0.071 |
| non-dominant | 64 [49; 104] | 68 [46; 106] * | 71 [49; 106] * | 0.019 | |
| concentric 60°/s | dominant | 46 [30; 77] | 47 [35; 71] | 47 [37; 73] | 0.197 |
| non-dominant | 47 [30; 73] | 50 [33; 71] | 49 [37; 75] | 0.078 | |
| concentric 180°/s | dominant | 34 [24; 61] | 31 [24; 58] | 33 [27; 61] | 0.269 |
| non-dominant | 34 [24; 53] | 37 [24; 54] ** | 35 [26; 53] ** | 0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flueck, J.L.; Schlaepfer, M.W.; Perret, C. Effect of 12-Week Vitamin D Supplementation on 25[OH]D Status and Performance in Athletes with a Spinal Cord Injury. Nutrients 2016, 8, 586. https://doi.org/10.3390/nu8100586
Flueck JL, Schlaepfer MW, Perret C. Effect of 12-Week Vitamin D Supplementation on 25[OH]D Status and Performance in Athletes with a Spinal Cord Injury. Nutrients. 2016; 8(10):586. https://doi.org/10.3390/nu8100586
Chicago/Turabian StyleFlueck, Joelle Leonie, Max Walter Schlaepfer, and Claudio Perret. 2016. "Effect of 12-Week Vitamin D Supplementation on 25[OH]D Status and Performance in Athletes with a Spinal Cord Injury" Nutrients 8, no. 10: 586. https://doi.org/10.3390/nu8100586





