Effects of Olive Oil on Markers of Inflammation and Endothelial Function—A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Experimental Section
2.1. Literature Search
2.2. Study Selection
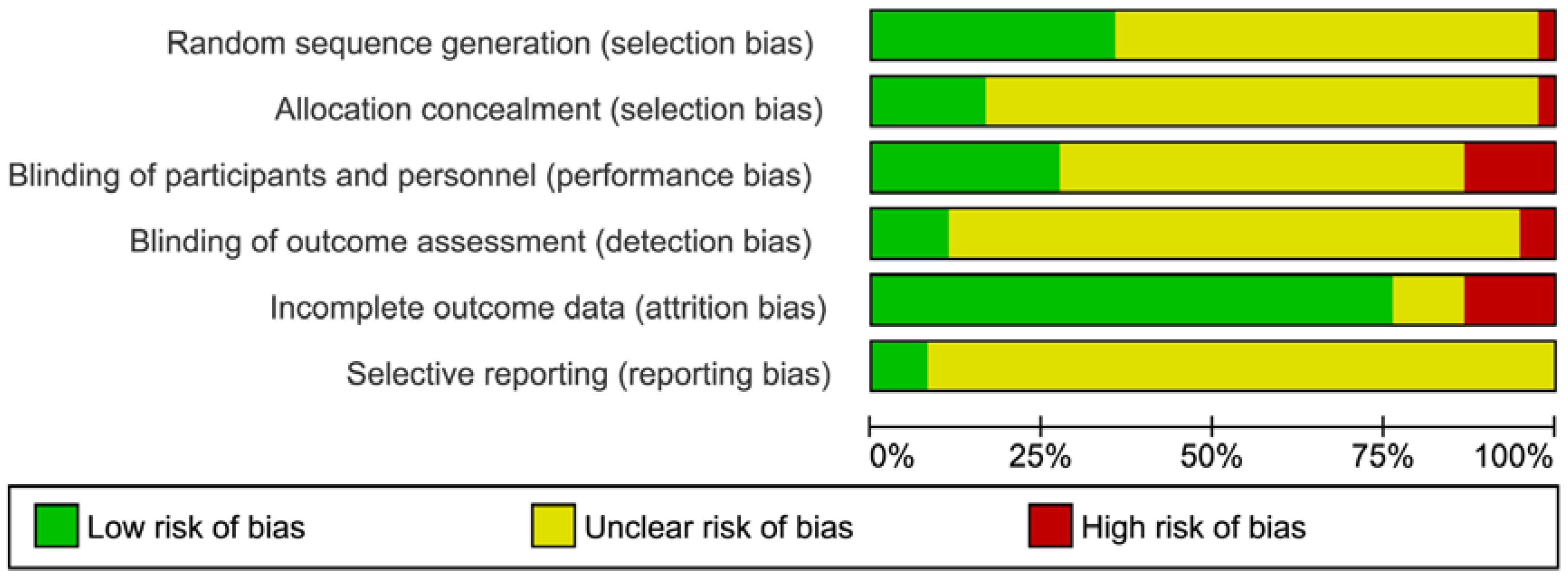
2.3. Risk of Bias Assessment
2.4. Data Extraction and Analyses
2.5. Specific Data Handling/Handling of Missing Data
3. Results
3.1. Literature Search and Study Characteristics


- (1)
- low-fat diet;
- (2)
- healthy diet;
- (3)
- MedD and nuts;
- (4)
- Western diet/diet high in carbohydrates;
- (1)
- flaxseed oil;
- (2)
- coconut oil/palm oil;
- (3)
- olive oil with n-3 fatty acids;
- (1)
- conjugated linoleic acid mix capsules;
- (2)
- n-3 fatty acid capsules;
- (1)
- plant-based olive oil diet vs. National Cancer Institute diet;
- (2)
- monounsaturated fatty acid diet vs. saturated fatty acid diet and low-fat diet.
| Reference | Sample Size; % Female | Age (Years, Mean ± SD) | BMI (kg/m2, Mean ± SD) | Duration (Weeks), Design | Diseases/Health Status/Medication | Olive Oil Intervention | Comparison Group | Outcome Parameters |
|---|---|---|---|---|---|---|---|---|
| Casas et al., 2014 [19] | 164; olive oil: 56.4, control: 59.3 | Olive oil: 68.1 ± 6, control: 67.4 ± 4 | Olive oil: 27.9 ± 3.4, control: 26.5 ± 3.7 | 52, parallel | High risk for CVD (type 2 diabetes mellitus or 3 or more major cardiovascular risk factors) | MedD + extra virgin olive oil (50 mL/day) | Low-fat diet | CRP, sE-selectin, sP-selectin, sVCAM-1 |
| Ceriello et al., 2014 [20] | 24; olive oil: 25, control: 33 | n.d. | Olive oil: 29.8 ± 1.4, control: 29.2 ± 1.1 | 3 months, parallel | Type 2 diabetes mellitus | MedD + extra virgin olive oil (50 mL/day) | Low-fat diet | FMD |
| Damasceno et al., 2010 [17] | 18; 50 | 56 ± 13 | 25.7 ± 2.3 | 4, cross-over | Moderate hypercholesterolemia, no medication, no hormone replacement therapy | MedD + 30–50 g/day virgin olive oil (polyphenols 34.3 mg/100g) | MedD + walnuts (polyphenols 1.3 mg/100g); MedD + almonds (polyphenols 1.1 mg/100g) | CRP, sICAM-1, sVCAM-1 |
| Damsgaard et al., 2008 [21] | 64; 0 | Olive oil high linoleic acid: 24.9 ± 3.8, olive oil low linoleic acid: 25.5 ± 4.4, control high linoleic acid: 26.3 ± 4.8, control low linoleic acid: 24.9 ± 4.9 | Olive oil high linoleic acid: 23.1 ± 1.9, olive oil low linoleic acid: 23.3. ± 1.9, control high linoleic acid: 21.9 ± 1.8, control low linoleic acid: 22.9 ± 1.9 | 8, 2 × 2 factorial | Healthy, no medication | 5 mL/day unrefined extra virgin olive oil capsules | 5 mL/day fish oil capsules | adiponectin, CRP, IL-6, VCAM-1 |
| Damsgaard et al., 2009 [22] | 63; 0 | Olive oil high linoleic acid: 24.9 ± 3.8, olive oil low linoleic acid: 25.5 ± 4.4, control high linoleic acid: 26.3 ± 4.8, control low linoleic acid: 24.9 ± 4.9 | Olive oil high linoleic acid: 23.1 ± 1.9, olive oil low linoleic acid: 23.3. ± 1.9, control high linoleic acid: 21.9 ± 1.8, control low linoleic acid: 22.9 ± 1.9 | 8, 2 × 2 factorial | Healthy, no intensive sports | 5 mL/day unrefined extra virgin olive oil capsules | 5 mL/day fish oil capsules | |
| Eschen et al., 2004 [23] | 60; olive oil: 82, control: 66 | Olive oil: 39 ± 10, control: 38 ± 11 | Olive oil: 24.6 ± 3.7, control:25.1 ± 2.9 | 12, parallel | Healthy, no medication | 10 g/day olive oil capsules | 6.6 g/day n-3 PUFA capsules; 2.0 g/day n-3 PUFA + 7 g/day olive oil capsules | ICAM-1, VCAM-1, P-selectin |
| Eschen et al., 2010 [24] | 138; olive oil: 22, control: 13 | Olive oil: 61 ± 8, control: 58 ± 10 | Olive oil: 27.1 ± 0.4, control: 27.1 ± 0.5 | 24, parallel | Chronic heart failure and left ventricular ejection fraction<40 or stable oral medication | 1 g/day olive oil capsules | 0.9 g/day n-3 PUFA capsules | SICAM-1, sVCAM-1, sP-selectin |
| Esposito et al., 2004 [25] | 180; olive oil: 46, control: 44 | Olive oil: 44.3 ± 6.4, control: 43.5 ± 5.9 | Olive oil: 27.9 ± 3.4, control: 28.1 ± 3.2 | 104, parallel | ≥3 criteria of metabolic syndrome, no medication, no intensive sports | MedD + olive oil | Generally healthy diet | hsCRP, IL-6 |
| Esposito et al., 2009 [26] | 195; olive oil: 50, control: 51.5 | n.d. | n.d. | 208, parallel | Overweight, newly diagnosed type 2 diabetes mellitus, no medication | MedD + 30–50 g olive oil/day | Low-fat diet | adiponectin |
| Flynn et al., 2010 [27] | 28; n.d. | 59.2 ± 6.1 | 27.9 ± 2.8 | 8 weight loss, 24 follow-up, cross-over | Overweight women with invasive breast cancer, stable medication | Plant-based olive oil diet with at least 3 tablespoons extra virgin olive oil/day | National Cancer Institute diet with canola oil | CRP |
| Fuentes et al., 2008 [28] | 20; n.d. | 23.3. ± 1.5 | 24.65 ± 2.91 | 4, cross-over | Healthy, no medication, no intensive sports | MUFA diet based on extra virgin olive oil (38% fat) | SFA diet; low-fat n-3 enriched diet based on α-linoleic acid | sVCAM-1, sICAM-1 |
| Gammelmark et al., 2012 [29] | 50; olive oil: 52, control: 52 | Olive oil: 58.0 ± 17.4, control: 55.4 ± 9.5 | Olive oil: 30.8 ± 4.2, control: 29.5 ± 3.3 | 6, parallel | Abdominally obese, women postmenopausal, no medication except NSAIDs | 2 g/day olive oil capsules | 2 g/day fish oil capsules | Adiponectin, CRP, IL-6 |
| Konstantinidou et al., 2010 [30] | 90; olive oil: 67, control: 63 | Olive oil: 45 ± 10, control: 44 ± 10 | Olive oil: 25 ± 4, control: 26 ± 5 | 12, parallel | Healthy | MedD + virgin olive oil (phenolic content 328 mg/kg) | MedD + washed virgin olive oil (phenolic content 55 mg/kg); habitual diet | sP-selectin |
| Kontogianni et al., 2013 [31] | 37; 78 | 25.6 ± 5.9 | 21.9 ± 2.5 | 6, cross-over | Healthy, no medication, no intensive sports | 15 mL/day extra virgin olive oil | 15 mL/day flaxseed oil | Adiponectin, CRP, TNF-α |
| Maki et al., 2009 [32] | 76; olive oil: 80, control: 88 | Olive oil: 49.6 ± 1.4, control: 49.4 ± 1.7 | Olive oil: 31.1 ± 1.1, control: 32.6 ± 1.5 | 4, parallel | Healthy, abdominally obese | 2 g/day olive oil capsules | 2 g/day krill oil capsules; 2 g/day menhaden oil capsules | CRP |
| Mena et al., 2009 [33] | 106; olive oil: 84, control: 76 | Olive oil: 66 ± 11, control: 66 ± 7 | Olive oil: 28.0 ± 2.9, control: 27.8 ± 3.2 | 12, parallel | Type 2 diabetes mellitus or ≥3 CVD risk factors, ACE inhibitors, diuretics, anti-hypertensive agents, statins, lipid-lowering agents, insulin, oral glucose-lowering agents, aspirin or anti-platelet drugs | MedD + virgin olive oil (1 L/week) | MedD + nuts (30 g/day); low-fat diet | sE-selectin, sP-selectin, sVCAM-1, sICAM-1, IL-6, CRP |
| Mori et al., 2003 [34] | 51; olive oil: 25, control: 28 | Olive oil: 61.5 ± 1.9, control: 60.9 ± 1.9 | Olive oil: 29.9 ± 1.0, control: 28.6 ± 0.7 | 6, parallel | Hypertension, type 2 diabetes mellitus, anti-hypertensive therapy, oral glucose-lowering agents but no insulin | 4 g/day olive oil capsules | 4 g/day EPA capsules; 4 g/day DHA capsules | CRP, IL-6, TNF-α |
| Perez-Martinez et al., 2007 [2] | 16; 0 | n.d. | n.d. | 4, cross-over | Healthy, no medication, no intensive sports | MedD + virgin olive oil | SFA diet; diet high in carbohydrates | VCAM-1 |
| Pfeuffer et al., 2011 [35] | 85; olive oil: 0, control: 0 | n.d. | Conjugated linoleic acid: 28.3 ± 2.3, safflower oil: 28.2 ± 2.0, heated safflower oil: 28.9 ± 2.6 | 4, parallel | Overweight or obese, metabolic syndrome, coronary heart disease | 4.5 g/day olive oil capsules | 4.5 g/day conjugated linoleic acid mixture capsules; 4.5 g/day safflower oil capsules; 4.5 g/day heated safflower oil capsules | CRP, sICAM, sVCAM, sE-selectin |
| Sanders et al., 2011 [18] | 367; olive oil: 61, control: 56 | Olive oil: 55 (range: 54–57), control: 55 (range: 54–57) | Olive oil, males: 27 (range: 26–28), olive oil, females: 26 (range: 25–27), control, males: 26 (range: 25–27), control, females: 25 (range: 24–26) | 52, parallel | No CVD, medication: statins, anti-hypertensive medication, hormone replacement therapy, thyroxine | 3 g/day refined olive oil capsules | 0.45/0.9/1.8 g/day EPA + DHA capsules | CRP, FMD |
| Singhal et al., 2013 [36] | 324; olive oil: 60, control: 66 | Olive oil: 27.6 ± 4.7, control: 28.2 ± 4.8 | Olive oil: 23.6 ± 3.5, control: 23.6 ± 34.3 | 16, parallel | Healthy, no medication | 4 g/day olive oil capsules | 1.6 g/day DHA + 2.4 g/day carrier oil capsules | CRP, FMD |
| Sofi et al., 2010 [37] | 11; olive oil: 0, control: 33 | Olive oil: 54 (range: 42–70), control: 55 (range: 30–41) | Olive oil: 29.3 ± 3.9, control: 29.3 ± 4.1 | 52, parallel | Non-alcoholic fatty liver disease | 6.5 mL/day olive oil | 6.5 mL/day olive oil enriched with n-3 PUFA | adiponectin |
| Stirban et al., 2010 [38] | 34; n.d. | 56.8 ± 8.3 | 31.3 ± 4.1 | 6, cross-over | Type 2 diabetes mellitus, aspirin, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, calcium channel blockers, ß-blockers, diuretics, statins | 2 g/day olive oil capsules | 2 g/day n-3 PUFA capsules | FMD |
| Taylor et al., 2005 [39] | 40; olive oil: 0, control: 0 | Olive oil: 47 ± 8, control: 45 ± 6 | Olive oil: 33 ± 3, control: 33 ± 3 | 12, parallel | Overweight, healthy | 4.5 g/day olive oil capsules | 4.5 g/day conjugated linoleic acid mixture capsules | adiponectin, CRP, FMD, TNF-α |
| Theobald et al., 2007 [40] | 39; 50 | Male: 51.1 ± 7.4, female: 46.2 ± 4.9 | Male: 51.1 ± 7.4, females: 46.2 ± 4.9 | 12, cross-over | Healthy, no medication | 1.5 g/day refined olive oil capsules | 0.7 g/day DHA capsules | IL-6, CRP, sE-Selectin |
| Tholstrup et al., 2008 [41] | 69; olive oil: 100, control: 100 | Olive oil: 59.9 ± 4.9, control: 62.3 ± 5.0 | Olive oil: 25.5 ± 3.3, control: 25.6 ± 3.1 | 16, parallel | Healthy, postmenopausal women, no medication | 5.5 g/day olive oil capsules | 5.5 g/day conjugated linoleic acid mixture capsules; 5.5 g/day conjugated linoleic acid milk capsules | IL-6, ICAM-1, VCAM-1 |
| Thomazella et al., 2011 [42] | 40; olive oil: 0, control: 0 | Olive oil: 55.0 ± 4.6, control: 54.6 ± 5.0 | Olive oil: 26.5 ± 1.9, control: 26.3 ± 2.5 | 12, parallel | ≥1 coronary event, clinical stablility, aspirin, anti-platelet drugs, statins (+ezetimibe), nitrates, ACE inhibitors, ß blockers | MedD + extra virgin olive oil (30 mL/day) | Low-fat therapeutic lifestyle changes diet | CRP, sICAM-1, sVCAM-1, FMD |
| Urpi-Sarda et al., 2012 [43] | 516; n.d. | n.d. | n.d. | 52, parallel | Type 2 diabetes mellitus or ≥3 CVD risk factors | MedD + virgin olive oil (1 L/week) | MedD + nuts; low-fat diet | ICAM-1, IL-6 |
| Voon et al., 2011 [44] | 45; 80 | 30.1 ± 8.3 | 30.1 ± 8.3 | 5, cross-over | healthy | Olive oil (2/3 of total fat) | Coconut oil (2/3 of total fat); palm olein (2/3 of total fat) | CRP, IL-6, TNF-α |
| Wong et al., 2010 [45] | 97; olive oil: 58, control: 53 | Olive oil: 59.0 ± 8.3, control: 61.2 ± 9.0 | Olive oil: 26.4 ± 4.4, control: 25.2 ± 3.7 | 12, parallel | Type 2 diabetes mellitus, no cardiovascular events, oral glucose-lowering agents/insulin | 4 g/day olive oil capsules | 4 g/day fish oil capsules | CRP, FMD |
| Woodman et al., 2003 [46] | 59; olive oil: 25, control: 28 | Olive oil: 61.5 ± 7.6, control: 60.9 ± 8.2 | Olive oil: 29.9 ± 4.0, control: 30.6 ± 3.1 | 6, parallel | Obese, type 2 diabetes mellitus and hypertension, oral glucose-lowering agents and treatment for hypertension | 4 g/day olive oil capsules | 4 g/day EPA capsules; 4 g/day DHA capsules | FMD, P-selectin |
3.2. Markers of Inflammation
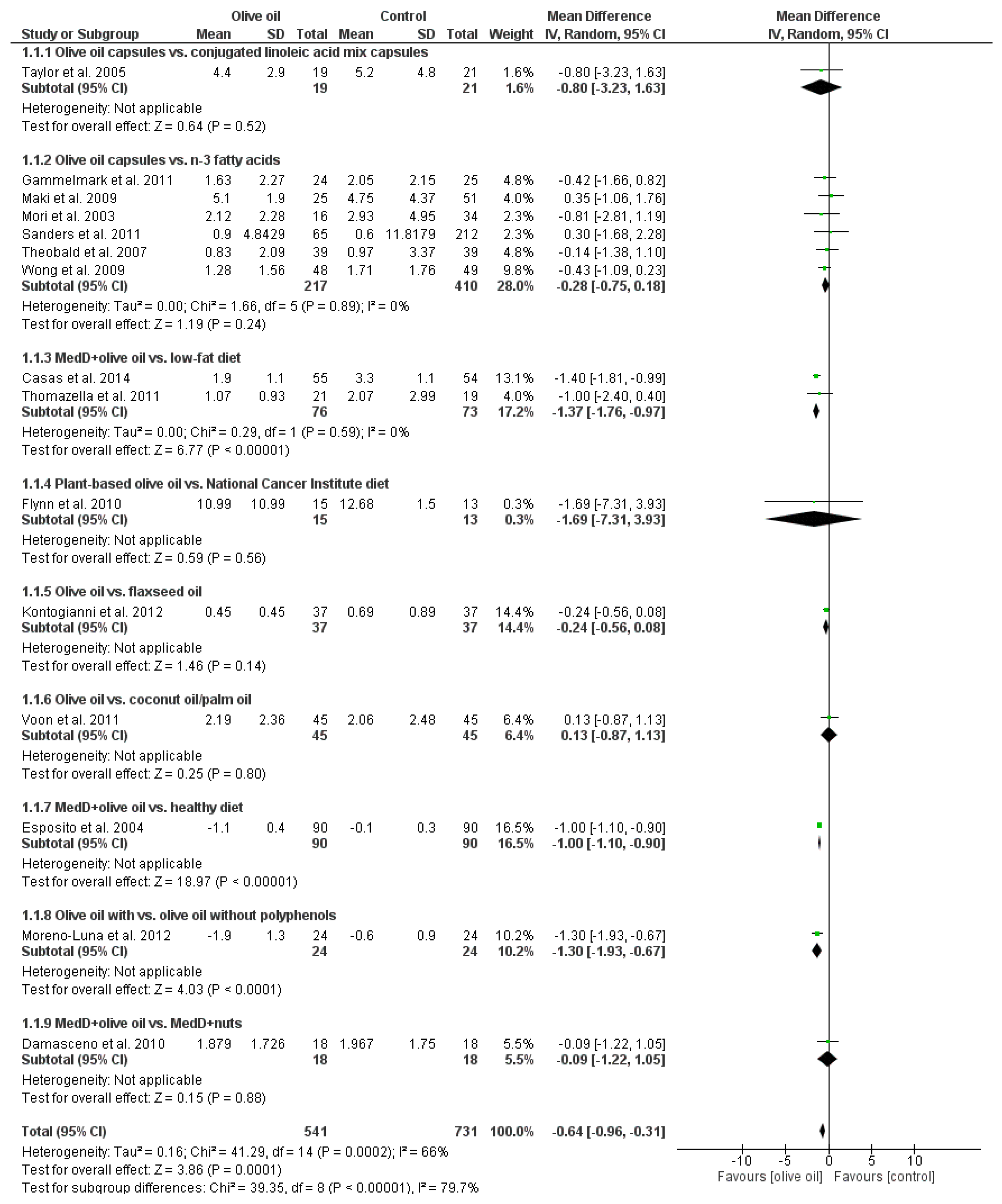
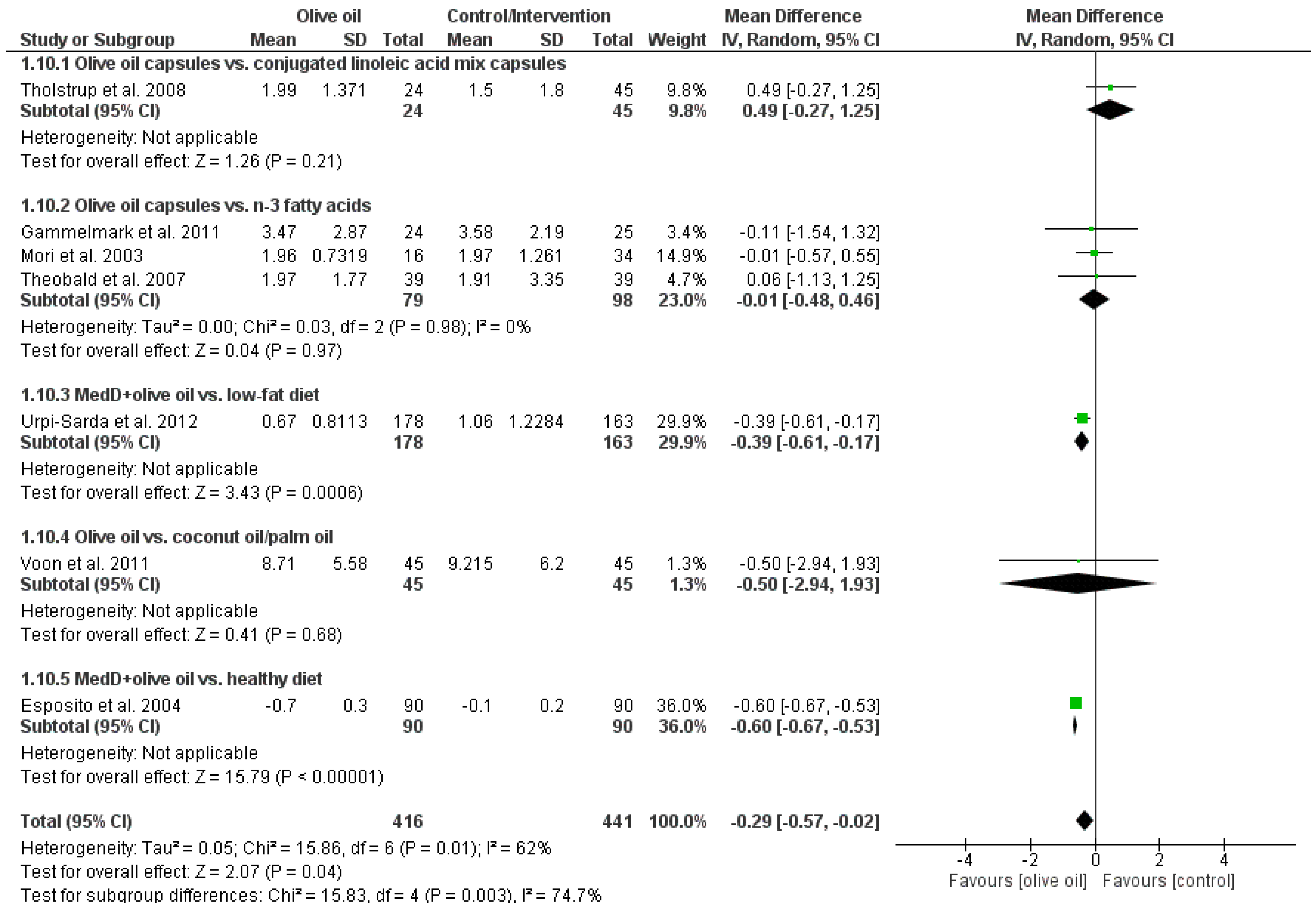
| Outcome Parameter | Mean Difference | 95% Confidence Interval | p-Value | No. of Studies | Sample Size | I2 (%) |
|---|---|---|---|---|---|---|
| C-reactive protein (mg/L) | −0.64 | (−0.96, −0.31) | 0.0001 | 15 | 1272 | 66 |
| Adiponectin (mg/L) | 0.44 | (−0.20, 1.09) | 0.18 | 6 | 313 | 56 |
| Interleukin-6 (pg/mL) | −0.29 | (−0.57, −0.02) | 0.04 | 7 | 857 | 62 |
| Tumor necrosis factor-α (µg/L) | 0.02 | (−0.02, 0.07) | 0.36 | 5 | 303 | 95 |
| sE-Selectin (ng/mL) | −3.16 | (−4.07, −2.25) | 0.00001 | 2 | 187 | 0 |
| sP-Selectin (ng/mL) | 10.78 | (4.01, 17.54) | 0.002 | 4 | 358 | 41 |
| sICAM-1 (ng/L) | −0.02 | (−0.04, 0.00) | 0.02 | 7 | 724 | 84 |
| sVCAM-1 (ng/L) | −0.02 | (−0.05, 0.01) | 0.14 | 8 | 524 | 37 |
| FMD (%) | 0.76 | (0.27, 1.24) | 0.002 | 8 | 851 | 26 |

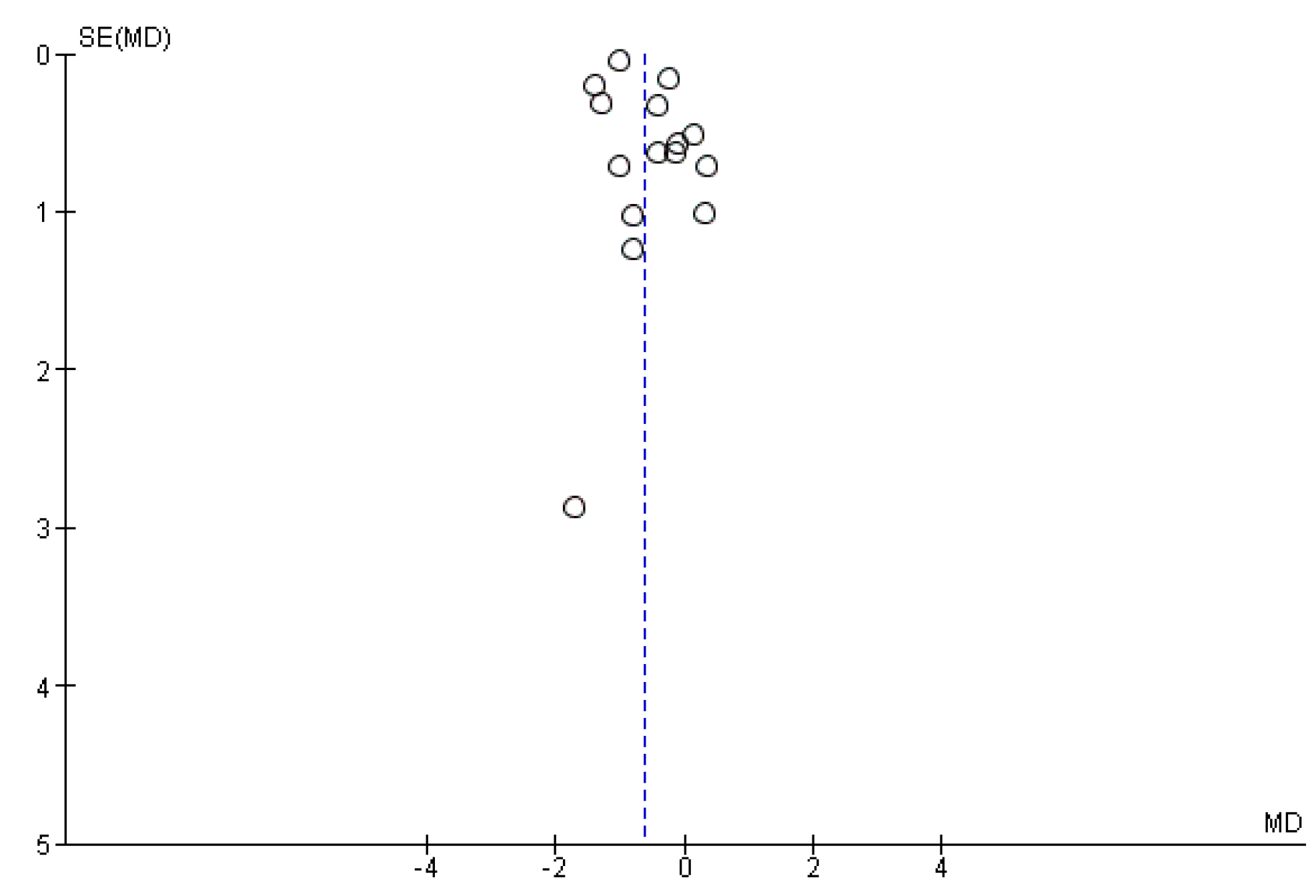
3.3. Publication Bias
4. Discussion
Limitations of the Systematic Review
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef] [PubMed]
- Perez-Martinez, P.; Lopez-Miranda, J.; Blanco-Colio, L.; Bellido, C.; Jimenez, Y.; Moreno, J.A.; Delgado-Lista, J.; Egido, J.; Perez-Jimenez, F. The chronic intake of a mediterranean diet enriched in virgin olive oil, decreases nuclear transcription factor κB activation in peripheral blood mononuclear cells from healthy men. Atherosclerosis 2007, 194, e141–e146. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Fidalgo, S.; Sanchez de Ibarguen, L.; Cardeno, A.; Alarcon de la Lastra, C. Influence of extra virgin olive oil diet enriched with hydroxytyrosol in a chronic dss colitis model. Eur. J. Nutr. 2012, 51, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Luna, R.; Muñoz-Hernandez, R.; Miranda, M.L.; Costa, A.F.; Jimenez-Jimenez, L.; Vallejo-Vaz, A.J.; Muriana, F.J.; Villar, J.; Stiefel, P. Olive oil polyphenols decrease blood pressure and improve endothelial function in young women with mild hypertension. Am. J. Hypertens. 2012, 25, 1299–1304. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Monounsaturated fatty acids and risk of cardiovascular disease: Synopsis of the evidence available from systematic reviews and meta-analyses. Nutrients 2012, 4, 1989–2007. [Google Scholar] [CrossRef] [PubMed]
- Cook-Mills, J.M.; Marchese, M.E.; Abdala-Valencia, H. Vascular cell adhesion molecule-1 expression and signaling during disease: Regulation by reactive oxygen species and antioxidants. Antioxid. Redox Signal. 2011, 15, 1607–1638. [Google Scholar] [CrossRef] [PubMed]
- Roos, M.W.; Sperber, G.O. A diffusion model of cerebral microischemia. Exp. Neurol. 1997, 147, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: A meta-analysis. Int. J. Cardiovasc. Imaging 2010, 26, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Monounsaturated fatty acids, olive oil and health status: A systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Das, U.N.; Stefanadis, C. Adherence to the mediterranean diet attenuates inflammation and coagulation process in healthy adults: The Attica study. J. Am. Coll. Cardiol. 2004, 44, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; McCullough, M.L.; Newby, P.K.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [PubMed]
- Salas-Salvado, J.; Garcia-Arellano, A.; Estruch, R.; Marquez-Sandoval, F.; Corella, D.; Fiol, M.; Gomez-Gracia, E.; Vinoles, E.; Aros, F.; Herrera, C.; et al. Components of the mediterranean-type food pattern and serum inflammatory markers among patients at high risk for cardiovascular disease. Eur. J. Clin. Nutr. 2008, 62, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.A.; Ramos, S.; Granado-Serrano, A.B.; Rodriguez-Ramiro, I.; Trujillo, M.; Bravo, L.; Goya, L. Hydroxytyrosol induces antioxidant/detoxificant enzymes and Nrf2 translocation via extracellular regulated kinases and phosphatidylinositol-3-kinase/protein kinase B pathways in HepG2 cells. Mol. Nutr. Food Res. 2010, 54, 956–966. [Google Scholar] [CrossRef] [PubMed]
- International Prospective Register of Systematic Reviews. Available online: http://www.crd.york.ac.uk/PROSPERO/ (accessed on 7 September 2015).
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- The Cochrane Collaboration. Avalaible online: http://tech.cochrane.org/revman/download (accessed on 7 September 2015).
- Damasceno, N.R.; Perez-Heras, A.; Serra, M.; Cofan, M.; Sala-Vila, A.; Salas-Salvado, J.; Ros, E. Crossover study of diets enriched with virgin olive oil, walnuts or almonds. Effects on lipids and other cardiovascular risk markers. Nutr. Metab. Cardiovasc. Dis. 2011, 21 (Suppl. S1), S14–S20. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.A.; Hall, W.L.; Maniou, Z.; Lewis, F.; Seed, P.T.; Chowienczyk, P.J. Effect of low doses of long-chain n-3 PUFAs on endothelial function and arterial stiffness: A randomized controlled trial. Am. J. Clin. Nutr. 2011, 94, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Casas, R.; Sacanella, E.; Urpi-Sarda, M.; Chiva-Blanch, G.; Ros, E.; Martinez-Gonzalez, M.A.; Covas, M.I.; Rosa Ma, L.R.; Salas-Salvado, J.; Fiol, M.; et al. The effects of the mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease. A randomized trial. PLoS ONE 2014, 9, e100084. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; Esposito, K.; La Sala, L.; Pujadas, G.; De Nigris, V.; Testa, R.; Bucciarelli, L.; Rondinelli, M.; Genovese, S. The protective effect of the mediterranean diet on endothelial resistance to GLP-1 in type 2 diabetes: A preliminary report. Cardiovasc. Diabetol. 2014, 13, 140. [Google Scholar] [CrossRef] [PubMed]
- Damsgaard, C.T.; Frøkiaer, H.; Andersen, A.D.; Lauritzen, L. Fish oil in combination with high or low intakes of linoleic acid lowers plasma triacylglycerols but does not affect other cardiovascular risk markers in healthy men. J. Nutr. 2008, 138, 1061–1066. [Google Scholar] [PubMed]
- Damsgaard, C.T.; Lauritzen, L.; Calder, P.C.; Kjaer, T.R.; Frøkiaer, H. Reduced ex vivo interleukin-6 production by dietary fish oil is not modified by linoleic acid intake in healthy men. J. Nutr. 2009, 139, 1410–1414. [Google Scholar] [CrossRef] [PubMed]
- Eschen, O.; Christensen, J.H.; de Caterina, R.; Schmidt, E.B. Soluble adhesion molecules in healthy subjects: A dose-response study using n-3 fatty acids. Nutr. Metab. Cardiovasc. Dis. 2004, 14, 180–185. [Google Scholar] [CrossRef]
- Eschen, O.; Christensen, J.H.; LA Rovere, M.T.; Romano, P.; Sala, P.; Schmidt, E.B. Effects of marine n-3 fatty acids on circulating levels of soluble adhesion molecules in patients with chronic heart failure. Cell. Mol. Biol. 2010, 56, 45–51. [Google Scholar] [PubMed]
- Esposito, K.; Marfella, R.; Ciotola, M.; di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Maiorino, M.I.; Ciotola, M.; di Palo, C.; Scognamiglio, P.; Gicchino, M.; Petrizzo, M.; Saccomanno, F.; Beneduce, F.; Ceriello, A.; et al. Effects of a mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: A randomized trial. Ann. Intern. Med. 2009, 151, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.M.; Reinert, S.E. Comparing an olive oil-enriched diet to a standard lower-fat diet for weight loss in breast cancer survivors: A pilot study. J. Women’s Health 2010, 19, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, F.; Lopez-Miranda, J.; Perez-Martinez, P.; Jimenez, Y.; Marin, C.; Gomez, P.; Fernandez, J.M.; Caballero, J.; Delgado-Lista, J.; Perez-Jimenez, F. Chronic effects of a high-fat diet enriched with virgin olive oil and a low-fat diet enriched with α-linolenic acid on postprandial endothelial function in healthy men. Br. J. Nutr. 2008, 100, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Gammelmark, A.; Madsen, T.; Varming, K.; Lundbye-Christensen, S.; Schmidt, E.B. Low-dose fish oil supplementation increases serum adiponectin without affecting inflammatory markers in overweight subjects. Nutr. Res. 2012, 32, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidou, V.; Covas, M.I.; Munoz-Aguayo, D.; Khymenets, O.; de la Torre, R.; Saez, G.; Tormos Mdel, C.; Toledo, E.; Marti, A.; Ruiz-Gutierrez, V.; et al. In vivo nutrigenomic effects of virgin olive oil polyphenols within the frame of the mediterranean diet: A randomized controlled trial. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2010, 24, 2546–2557. [Google Scholar]
- Kontogianni, M.D.; Vlassopoulos, A.; Gatzieva, A.; Farmaki, A.E.; Katsiougiannis, S.; Panagiotakos, D.B.; Kalogeropoulos, N.; Skopouli, F.N. Flaxseed oil does not affect inflammatory markers and lipid profile compared to olive oil, in young, healthy, normal weight adults. Metab. Clin. Exp. 2013, 62, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Maki, K.C.; Reeves, M.S.; Farmer, M.; Griinari, M.; Berge, K.; Vik, H.; Hubacher, R.; Rains, T.M. Krill oil supplementation increases plasma concentrations of eicosapentaenoic and docosahexaenoic acids in overweight and obese men and women. Nutr. Res. 2009, 29, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Mena, M.P.; Sacanella, E.; Vazquez-Agell, M.; Morales, M.; Fito, M.; Escoda, R.; Serrano-Martinez, M.; Salas-Salvado, J.; Benages, N.; Casas, R.; et al. Inhibition of circulating immune cell activation: A molecular antiinflammatory effect of the mediterranean diet. Am. J. Clin. Nutr. 2009, 89, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Mori, T.A.; Woodman, R.J.; Burke, V.; Puddey, I.B.; Croft, K.D.; Beilin, L.J. Effect of eicosapentaenoic acid and docosahexaenoic acid on oxidative stress and inflammatory markers in treated-hypertensive type 2 diabetic subjects. Free Radic. Biol. Med. 2003, 35, 772–781. [Google Scholar] [CrossRef]
- Pfeuffer, M.; Fielitz, K.; Laue, C.; Winkler, P.; Rubin, D.; Helwig, U.; Giller, K.; Kammann, J.; Schwedhelm, E.; Böger, R.H.; et al. Cla does not impair endothelial function and decreases body weight as compared with safflower oil in overweight and obese male subjects. J. Am. Coll. Nutr. 2011, 30, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Singhal, A.; Lanigan, J.; Storry, C.; Low, S.; Birbara, T.; Lucas, A.; Deanfield, J. Docosahexaenoic acid supplementation, vascular function and risk factors for cardiovascular disease: A randomized controlled trial in young adults. J. Am.Heart Assoc. 2013, 2, e000283. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Giangrandi, I.; Cesari, F.; Corsani, I.; Abbate, R.; Gensini, G.F.; Casini, A. Effects of a 1-year dietary intervention with n-3 polyunsaturated fatty acid-enriched olive oil on non-alcoholic fatty liver disease patients: A preliminary study. Int. J. Food Sci. Nutr. 2010, 61, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Stirban, A.; Nandrean, S.; Götting, C.; Tamler, R.; Pop, A.; Negrean, M.; Gawlowski, T.; Stratmann, B.; Tschoepe, D. Effects of n-3 fatty acids on macro- and microvascular function in subjects with type 2 diabetes mellitus. Am. J. Clin. Nutr. 2010, 91, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.S.; Williams, S.R.; Rhys, R.; James, P.; Frenneaux, M.P. Conjugated linoleic acid impairs endothelial function. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Theobald, H.E.; Goodall, A.H.; Sattar, N.; Talbot, D.C.; Chowienczyk, P.J.; Sanders, T.A. Low-dose docosahexaenoic acid lowers diastolic blood pressure in middle-aged men and women. J. Nutr. 2007, 137, 973–978. [Google Scholar] [PubMed]
- Tholstrup, T.; Raff, M.; Straarup, E.M.; Lund, P.; Basu, S.; Bruun, J.M. An oil mixture with trans-10, cis-12 conjugated linoleic acid increases markers of inflammation and in vivo lipid peroxidation compared with cis-9, trans-11 conjugated linoleic acid in postmenopausal women. J. Nutr. 2008, 138, 1445–1451. [Google Scholar] [PubMed]
- Thomazella, M.C.; Goes, M.F.; Andrade, C.R.; Debbas, V.; Barbeiro, D.F.; Correia, R.L.; Marie, S.K.; Cardounel, A.J.; daLuz, P.L.; Laurindo, F.R. Effects of high adherence to mediterranean or low-fat diets in medicated secondary prevention patients. Am. J. Cardiol. 2011, 108, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Urpi-Sarda, M.; Casas, R.; Chiva-Blanch, G.; Romero-Mamani, E.S.; Valderas-Martinez, P.; Salas-Salvado, J.; Covas, M.I.; Toledo, E.; Andres-Lacueva, C.; Llorach, R.; et al. The mediterranean diet pattern and its main components are associated with lower plasma concentrations of tumor necrosis factor receptor 60 in patients at high risk for cardiovascular disease. J. Nutr. 2012, 142, 1019–1025. [Google Scholar] [CrossRef] [PubMed]
- Voon, P.T.; Ng, T.K.; Lee, V.K.; Nesaretnam, K. Diets high in palmitic acid (16:0), lauric and myristic acids (12:0 + 14:0), or oleic acid (18:1) do not alter postprandial or fasting plasma homocysteine and inflammatory markers in healthy Malaysian adults. Am. J. Clin. Nutr. 2011, 94, 1451–1457. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.Y.; Yiu, K.H.; Li, S.W.; Lee, S.; Tam, S.; Lau, C.P.; Tse, H.F. Fish-oil supplement has neutral effects on vascular and metabolic function but improves renal function in patients with type 2 diabetes mellitus. Diabet. Med. J. Br. Diabet. Assoc. 2010, 27, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Woodman, R.J.; Mori, T.A.; Burke, V.; Puddey, I.B.; Barden, A.; Watts, G.F.; Beilin, L.J. Effects of purified eicosapentaenoic acid and docosahexaenoic acid on platelet, fibrinolytic and vascular function in hypertensive type 2 diabetic patients. Atherosclerosis 2003, 166, 85–93. [Google Scholar] [CrossRef]
- Danesh, J.; Wheeler, J.G.; Hirschfield, G.M.; Eda, S.; Eiriksdottir, G.; Rumley, A.; Lowe, G.D.; Pepys, M.B.; Gudnason, V. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N. Engl. J. Med. 2004, 350, 1387–1397. [Google Scholar] [CrossRef] [PubMed]
- Shah, T.; Casas, J.P.; Cooper, J.A.; Tzoulaki, I.; Sofat, R.; McCormack, V.; Smeeth, L.; Deanfield, J.E.; Lowe, G.D.; Rumley, A.; et al. Critical appraisal of crp measurement for the prediction of coronary heart disease events: New data and systematic review of 31 prospective cohorts. Int. J. Epidemiol. 2009, 38, 217–231. [Google Scholar] [CrossRef] [PubMed]
- Buckley, D.I.; Fu, R.; Freeman, M.; Rogers, K.; Helfand, M. C-reactive protein as a risk factor for coronary heart disease: A systematic review and meta-analyses for the U.S. Preventive services task force. Ann. Intern. Med. 2009, 151, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Morrow, D.A.; Ridker, P.M. C-reactive protein, inflammation, and coronary risk. Med. Clin. N. Am. 2000, 84, 149–161. [Google Scholar] [CrossRef]
- Bataille, R.; Klein, B. C-reactive protein levels as a direct indicator of interleukin-6 levels in humans in vivo. Arthritis Rheum. 1992, 35, 982–984. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, P.C.; Castell, J.V.; Andus, T. Interleukin-6 and the acute phase response. Biochem. J. 1990, 265, 621–636. [Google Scholar] [CrossRef] [PubMed]
- Danesh, J.; Kaptoge, S.; Mann, A.G.; Sarwar, N.; Wood, A.; Angleman, S.B.; Wensley, F.; Higgins, J.P.; Lennon, L.; Eiriksdottir, G.; et al. Long-term interleukin-6 levels and subsequent risk of coronary heart disease: Two new prospective studies and a systematic review. PLoS Med. 2008, 5, e78. [Google Scholar] [CrossRef] [PubMed]
- Blake, G.J.; Ridker, P.M. Inflammatory bio-markers and cardiovascular risk prediction. J. Intern. Med. 2002, 252, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Kritchevsky, S.B.; Cesari, M.; Pahor, M. Inflammatory markers and cardiovascular health in older adults. Cardiovascul. Res. 2005, 66, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Hao, G.; Li, W.; Guo, R.; Yang, J.G.; Wang, Y.; Tian, Y.; Liu, M.Y.; Peng, Y.G.; Wang, Z.W. Serum total adiponectin level and the risk of cardiovascular disease in general population: A meta-analysis of 17 prospective studies. Atherosclerosis 2013, 228, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Kanhai, D.A.; Kranendonk, M.E.; Uiterwaal, C.S.; van der Graaf, Y.; Kappelle, L.J.; Visseren, F.L. Adiponectin and incident coronary heart disease and stroke. A systematic review and meta-analysis of prospective studies. Obes. Rev. 2013, 14, 555–567. [Google Scholar] [CrossRef] [PubMed]
- Sook Lee, E.; Park, S.S.; Kim, E.; Sook Yoon, Y.; Ahn, H.Y.; Park, C.Y.; Ho Yun, Y.; Woo Oh, S. Association between adiponectin levels and coronary heart disease and mortality: A systematic review and meta-analysis. Int. J. Epidemiol. 2013, 42, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.C.; Xu, A.; Chow, W.S.; Lam, M.C.; Ai, V.H.; Tam, S.C.; Lam, K.S. Hypoadiponectinemia is associated with impaired endothelium-dependent vasodilation. J. Clin. Endocrinol. Metab. 2004, 89, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Celermajer, D.S.; Sorensen, K.E.; Gooch, V.M.; Spiegelhalter, D.J.; Miller, O.I.; Sullivan, I.D.; Lloyd, J.K.; Deanfield, J.E. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992, 340, 1111–1115. [Google Scholar] [CrossRef]
- Schroeder, S.; Enderle, M.D.; Ossen, R.; Meisner, C.; Baumbach, A.; Pfohl, M.; Herdeg, C.; Oberhoff, M.; Haering, H.U.; Karsch, K.R. Noninvasive determination of endothelium-mediated vasodilation as a screening test for coronary artery disease: Pilot study to assess the predictive value in comparison with angina pectoris, exercise electrocardiography, and myocardial perfusion imaging. Am. Heart J. 1999, 138, 731–739. [Google Scholar] [CrossRef]
- Chan, S.Y.; Mancini, G.B.; Kuramoto, L.; Schulzer, M.; Frohlich, J.; Ignaszewski, A. The prognostic importance of endothelial dysfunction and carotid atheroma burden in patients with coronary artery disease. J. Am. Coll. Cardiol. 2003, 42, 1037–1043. [Google Scholar] [CrossRef]
- Gokce, N.; Keaney, J.F.; Hunter, L.M.; Watkins, M.T.; Nedeljkovic, Z.S.; Menzoian, J.O.; Vita, J.A. Predictive value of noninvasively determined endothelial dysfunction for long-term cardiovascular events in patients with peripheral vascular disease. J. Am. Coll. Cardiol. 2003, 41, 1769–1775. [Google Scholar] [CrossRef]
- Yeboah, J.; Folsom, A.R.; Burke, G.L.; Johnson, C.; Polak, J.F.; Post, W.; Lima, J.A.; Crouse, J.R.; Herrington, D.M. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: The multi-ethnic study of atherosclerosis. Circulation 2009, 120, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Siemiatkowski, A.; Rogowski, F.; Wereszczyńska-Siemiatkowska, U.; Malinowska, L.; Borkowski, J. Soluble selectin profiles associated with severe trauma. Arch. Immunol. Ther. Exp. (Warsz.) 2001, 49, 317–324. [Google Scholar] [PubMed]
- Cherian, P.; Hankey, G.J.; Eikelboom, J.W.; Thom, J.; Baker, R.I.; McQuillan, A.; Staton, J.; Yi, Q. Endothelial and platelet activation in acute ischemic stroke and its etiological subtypes. Stroke 2003, 34, 2132–2137. [Google Scholar] [CrossRef] [PubMed]
- Prugger, C.; Luc, G.; Haas, B.; Morange, P.E.; Ferrieres, J.; Amouyel, P.; Kee, F.; Ducimetiere, P.; Empana, J.P.; Group, P.S. Multiple biomarkers for the prediction of ischemic stroke: The prime study. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Karatzi, K.N.; Papamichael, C.M.; Karatzis, E.N.; Papaioannou, T.G.; Aznaouridis, K.A.; Katsichti, P.P.; Stamatelopoulos, K.S.; Zampelas, A.; Lekakis, J.P.; Mavrikakis, M.E. Red wine acutely induces favorable effects on wave reflections and central pressures in coronary artery disease patients. Am. J. Hypertens. 2005, 18, 1161–1167. [Google Scholar] [CrossRef] [PubMed]
- Hertog, M.G.; Kromhout, D.; Aravanis, C.; Blackburn, H.; Buzina, R.; Fidanza, F.; Giampaoli, S.; Jansen, A.; Menotti, A.; Nedeljkovic, S. Flavonoid intake and long-term risk of coronary heart disease and cancer in the seven countries study. Arch. Intern. Med. 1995, 155, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Zern, T.L.; Fernandez, M.L. Cardioprotective effects of dietary polyphenols. J. Nutr. 2005, 135, 2291–2294. [Google Scholar] [PubMed]
- Ruano, J.; Lopez-Miranda, J.; Fuentes, F.; Moreno, J.A.; Bellido, C.; Perez-Martinez, P.; Lozano, A.; Gómez, P.; Jiménez, Y.; Pérez Jiménez, F. Phenolic content of virgin olive oil improves ischemic reactive hyperemia in hypercholesterolemic patients. J. Am. Coll. Cardiol. 2005, 46, 1864–1868. [Google Scholar] [CrossRef] [PubMed]
- Bermudez, B.; Lopez, S.; Ortega, A.; Varela, L.M.; Pacheco, Y.M.; Abia, R.; Muriana, F.J. Oleic acid in olive oil: From a metabolic framework toward a clinical perspective. Curr. Pharm. Des. 2011, 17, 831–843. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Dominguez, L.J.; Delgado-Rodriguez, M. Olive oil consumption and risk of CHD and/or stroke: A meta-analysis of case-control, cohort and intervention studies. Br. J. Nutr. 2014, 112, 248–259. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwingshackl, L.; Christoph, M.; Hoffmann, G. Effects of Olive Oil on Markers of Inflammation and Endothelial Function—A Systematic Review and Meta-Analysis. Nutrients 2015, 7, 7651-7675. https://doi.org/10.3390/nu7095356
Schwingshackl L, Christoph M, Hoffmann G. Effects of Olive Oil on Markers of Inflammation and Endothelial Function—A Systematic Review and Meta-Analysis. Nutrients. 2015; 7(9):7651-7675. https://doi.org/10.3390/nu7095356
Chicago/Turabian StyleSchwingshackl, Lukas, Marina Christoph, and Georg Hoffmann. 2015. "Effects of Olive Oil on Markers of Inflammation and Endothelial Function—A Systematic Review and Meta-Analysis" Nutrients 7, no. 9: 7651-7675. https://doi.org/10.3390/nu7095356
APA StyleSchwingshackl, L., Christoph, M., & Hoffmann, G. (2015). Effects of Olive Oil on Markers of Inflammation and Endothelial Function—A Systematic Review and Meta-Analysis. Nutrients, 7(9), 7651-7675. https://doi.org/10.3390/nu7095356




