Biomarkers and Hematological Indices in the Diagnosis of Iron Deficiency in Children with Inflammatory Bowel Disease
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kulnigg, S.; Gasche, C. Systematic review: Managing anaemia in Crohn’s disease. Aliment. Pharmacol. Ther. 2006, 24, 1507–1523. [Google Scholar] [CrossRef] [PubMed]
- Wiskin, A.E.; Fleming, B.J.; Wootton, S.A.; Beattie, R.M. Anaemia and iron deficiency in children with inflammatory bowel disease. J. Crohns Colitis 2012, 6, 687–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinisch, W.; Staun, M.; Bhandari, S.; Muñoz, M. State of the iron: How to diagnose and efficiently treat iron deficiency anemia in inflammatory bowel disease. J. Crohns Colitis 2013, 7, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Gasche, C.; Lomer, M.C.E.; Cavill, I.; Weiss, G. Iron, anaemia, and inflammatory bowel diseases. Gut 2004, 3, 1190–1197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogler, G.; Vavricka, S. Anemia in inflammatory bowel disease: An under-estimated problem? Front. Med. (Lausanne) 2015, 1, 58. [Google Scholar] [CrossRef] [Green Version]
- Cappellini, M.D.; Comin-Colet, J.; de Francisco, A. Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management. Am. J. Hematol. 2017, 92, 1068–1078. [Google Scholar] [CrossRef] [Green Version]
- Dignass, A.; Farrag, K.; Stein, J. Limitations of Serum Ferritin in Diagnosing Iron Deficiency in Inflammatory Conditions. Int. J. Chronic Dis. 2018, 9394060. [Google Scholar] [CrossRef] [Green Version]
- Dignass, A.U.; Gasche, C.; Bettenworth, D. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J. Crohns Colitis 2015, 9, 211–222. [Google Scholar] [CrossRef]
- Kazal, L.A. Prevention of iron deficiency in infants and toddlers. Am. Fam. Physician 2002, 66, 1217–1224. [Google Scholar]
- Oustamanolakis, P.; Koutroubakis, I.E.; Kouroumalis, E.A. Diagnosing anemia in inflammatory bowel disease: Beyond the established markers. J. Crohns Colitis 2011, 5, 381–391. [Google Scholar] [CrossRef] [Green Version]
- Beguin, Y. Soluble transferrin receptor for the evaluation of erythropoiesis and iron status. Clin. Chim. Acta. 2003, 329, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Skikne, B.S.; Punnonen, K.; Caldron, P.H. Improved differential diagnosis of anemia of chronic disease and iron deficiency anemia: A prospective multicenter evaluation of soluble transferrin receptor and the sTfR/log ferritin index. Am. J. Hematol. 2011, 86, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Krawiec, P.; Mroczkowska-Juchkiewicz, A.; Pac-Kożuchowska, E. Serum Hepcidin in Children with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 2165–2171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krawiec, P.; Pac-Kożuchowska, E. Soluble transferrin receptor and soluble transferrin receptor/log ferritin index in diagnosis of iron deficiency anemia in pediatric inflammatory bowel disease. Dig. Liver Dis. 2019, 51, 352–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Revel-Vilk, S.; Tamary, H.; Broide, E. Serum transferrin receptor in children and adolescents with inflammatory bowel disease. Eur. J. Pediatr. 2000, 159, 585–589. [Google Scholar] [CrossRef]
- Alves, R.A.; Miszputen, S.J.; Figueiredo, M.S. Anemia in inflammatory bowel disease: Prevalence, differential diagnosis and association with clinical and laboratory variables. Sao Paulo Med. J. 2014, 132, 140–146. [Google Scholar] [CrossRef] [Green Version]
- Borgna-Pignatti, C.; Marsella, M. Iron deficiency in infancy and childhood. Pediatr. Ann. 2008, 37, 329–337. [Google Scholar] [CrossRef]
- Venkatesan, M.; Saxena, S.; Kumar, A. Evaluation of iron status in patients of chronic kidney disease—A study to assess the best indicators including serum transferrin receptor assay. Indian J. Nephrol. 2019, 29, 248–253. [Google Scholar] [CrossRef]
- Abitbol, V.; Borderie, D.; Polin, V. Diagnosis of Iron Deficiency in Inflammatory Bowel Disease by Transferrin Receptor-Ferritin Index. Medicine 2015, 94, e1011. [Google Scholar] [CrossRef]
- Oustamanolakis, P.; Koutroubakis, I.E.; Messaritakis, I.; Niniraki, M.; Kouroumalis, E.A. Soluble transferrin receptor-ferritin index in the evaluation of anemia in inflammatory bowel disease: A case-control study. Ann. Gastroenterol 2011, 24, 108–114. [Google Scholar]
- Oustamanolakis, P.; Koutroubakis, I.E. Soluble transferrin receptor-ferritin index is the most efficient marker for the diagnosis of iron deficiency anemia in patients with IBD. Inflamm. Bowel Dis. 2011, 17, E158–E159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vazquez Lopez, M.A.; Carracedo, A.; Lendinez, F.; Javier Muñoz, F.; López, J.; Muñoz, A. The usefulness of serum transferrin receptor for discriminating iron deficiency without anemia in children. Haematologica 2006, 91, 264–265. [Google Scholar] [PubMed]
- Thomas, C.; Thomas, L. Biochemical markers and hematologic indices in the diagnosis of functional iron deficiency. Clin. Chem. 2002, 48, 1066–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Punnonen, K.; Irjala, K.; Rajamaki, A. Serum transferrin receptor, ferritin and TfR-F index in identification of latent iron deficiency. Eur. J. Haematol. 1998, 6, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Jonker, F.A.M.; Van Hensbroek, M.B.; Leenstra, T. Conventional and novel peripheral blood iron markers compared against bone marrow in Malawian children. J. Clin. Pathol. 2014, 67, 717–723. [Google Scholar] [CrossRef]
- Bultink, I.E.M.; Lems, W.F.; van de Stadt, R.J. Ferritin and serum transferrin receptor predict iron deficiency in anemic patients with rheumatoid arthritis. Arthritis Rheum. 2001, 44, 979–981. [Google Scholar] [CrossRef]
- Suominen, P.; Möttönen, T.; Rajamäki, A.; Irjala, K. Single values of serum transferrin receptor and transferrin receptor ferritin index can be used to detect true and functional iron deficiency in rheumatoid arthritis patients with anemia. Arthritis Rheum. 2000, 43, 1016–1020. [Google Scholar] [CrossRef]
- Chen, Y.C.; Hung, S.C.; Tarng, D.C. Association between transferrin receptor-ferritin index and conventional measures of iron responsiveness in hemodialysis patients. Am. J. Kidney Dis. 2006, 47, 1036–1044. [Google Scholar] [CrossRef] [Green Version]
- Łukaszyk, E.; Łukaszyk, M.; Koc-Żórawska, E. Iron status and inflammation in early stages of chronic kidney disease. Kidney Blood Press Res. 2015, 40, 366–373. [Google Scholar] [CrossRef]
- Leonard, A.J.; Patterson, A.J.; Collins, C.E.; Chalmers, K.A. Is soluble transferrin receptor a useful marker in early stage iron deficiency? ESPEN J. 2013, 8, e210–e212. [Google Scholar] [CrossRef]

| Parameter | IBD Patients with Deficiency of Iron | IBD Patients without Iron Deficiency | p |
|---|---|---|---|
| Hb (g/dL) | 11.51 ± 1.66 | 12.79 ± 1.59 | p = 0.0009 |
| Ht (%) | 34.88 ± 4.41 | 38.16 ± 3.79 | p = 0.002 |
| RBC (×106/μL) | 4.632 ± 0.55 | 4.695 ± 0.50 | p = 0.84 |
| MCV (fL) | 76.24 ± 6.52 | 81.23 ± 6.06 | p = 0.006 |
| MCH (pg) | 24.93 ± 2.89 | 27.33 ± 2.76 | p = 0.002 |
| MCHC (g/dL) | 32.63 ± 1.49 | 33.46 ± 1.66 | p = 0.05 |
| RDW-SD (fl) | 40.38 ± 4.85 | 39.41 ± 4.27 | p = 0.53 |
| RDW-CV (%) | 14.95 ± 1.83 | 13.95 ± 2.06 | p = 0.02 |
| Iron (μg/dL) | 34.12 ± 26.04 | 53.03 ± 39.33 | p = 0.04 |
| Transferrin (mg/dL) | 277.24 ± 54.87 | 234.44 ± 60.20 | p = 0.003 |
| SatTf (%) | 8.42 ± 5.98 | 15.36 ± 10.10 | p = 0.0006 |
| Ferritin (ng/mL) | 14.02 ± 13.260 | 73.80 ± 44.37 | p < 0.0001 |
| sTfR (μg/mL) | 1.67 ± 0.99 | 1.06 ± 0.36 | p = 0.0005 |
| sTfR/log ferritin | 2.50 ± 2.93 | 0.61 ± 0.21 | p < 0.0001 |
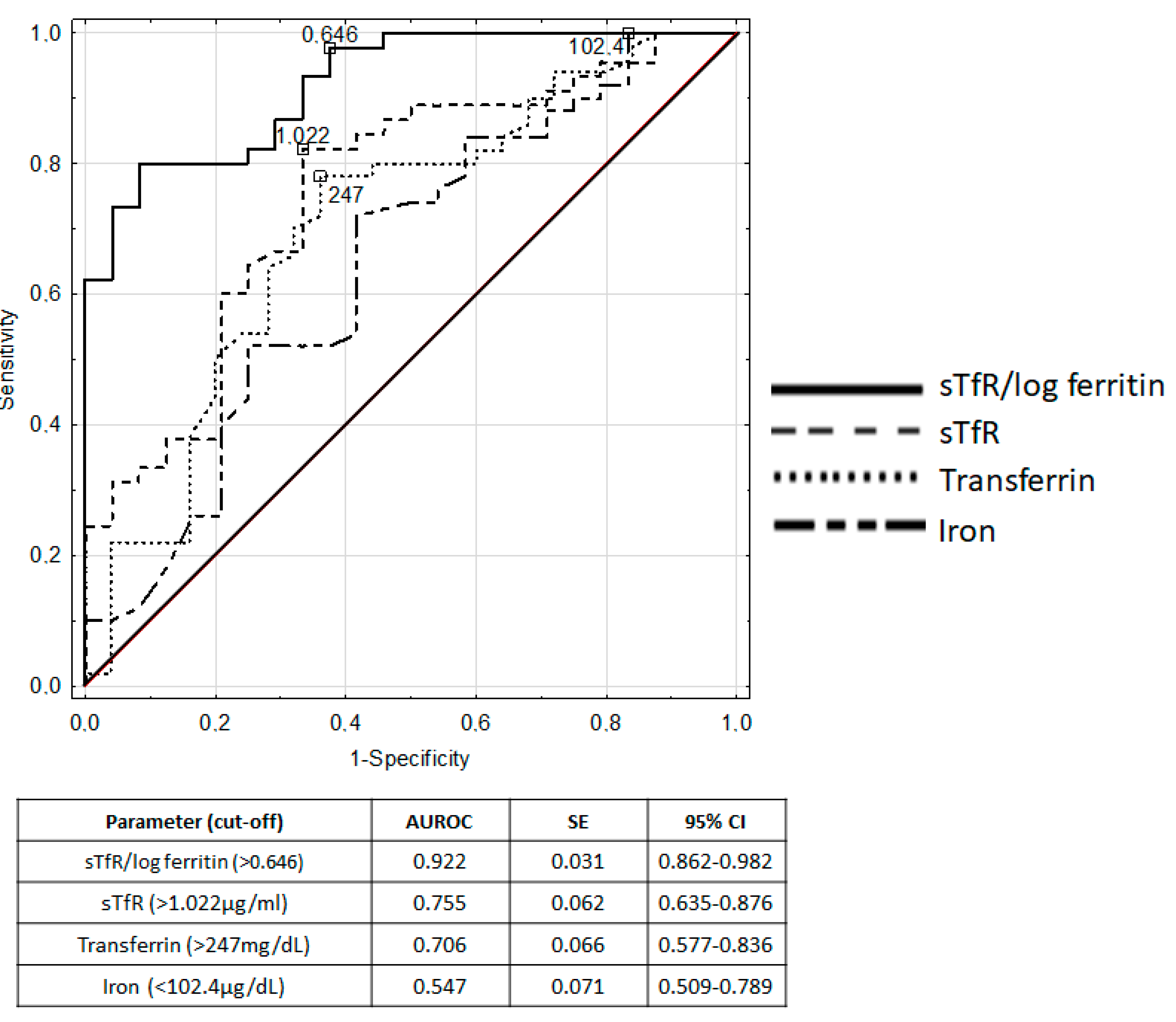
| Parameter [cut-off] | Sensitivity | Specificity | Accuracy | Positive Predictive Value p | Negative Predictive Value |
|---|---|---|---|---|---|
| MCV (<88.1 fL) | 1.00 | 0.08 | 0.69 | 0.69 | 1.00 |
| MCH (<29.1 pg) | 0.96 | 0.32 | 0.75 | 0.74 | 0.80 |
| MCHC (<34.3 g/dL) | 0.90 | 0.44 | 0.75 | 0.76 | 0.69 |
| RDW-SD (>34 fL) | 0.98 | 0.05 | 0.69 | 0.70 | 0.50 |
| RDW-CV (>12.5%) | 0.94 | 0.32 | 0.73 | 0.73 | 0.73 |
| Iron (<102.4 μg/dL) | 1.00 | 0.17 | 0.73 | 0.71 | 1.00 |
| Transferrin (>247 mg/dL) | 0.78 | 0.64 | 0.73 | 0.81 | 0.59 |
| sTfR (>1.022 μg/mL) | 0.82 | 0.67 | 0.77 | 0.82 | 0.67 |
| sTfR/log ferritin (>0.646) | 0.98 | 0.63 | 0.86 | 0.83 | 0.94 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krawiec, P.; Pac-Kożuchowska, E. Biomarkers and Hematological Indices in the Diagnosis of Iron Deficiency in Children with Inflammatory Bowel Disease. Nutrients 2020, 12, 1358. https://doi.org/10.3390/nu12051358
Krawiec P, Pac-Kożuchowska E. Biomarkers and Hematological Indices in the Diagnosis of Iron Deficiency in Children with Inflammatory Bowel Disease. Nutrients. 2020; 12(5):1358. https://doi.org/10.3390/nu12051358
Chicago/Turabian StyleKrawiec, Paulina, and Elżbieta Pac-Kożuchowska. 2020. "Biomarkers and Hematological Indices in the Diagnosis of Iron Deficiency in Children with Inflammatory Bowel Disease" Nutrients 12, no. 5: 1358. https://doi.org/10.3390/nu12051358





