Are Raw BIA Variables Useful for Predicting Resting Energy Expenditure in Adults with Obesity?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Anthropometry and Bioelectrical Impedance Analysis
2.3. Indirect Calorimetry
2.4. Statistical Analysis
3. Results
(unstandardized regression coefficients, R2 = 0.621; SEE = 259 kcal)
(unstandardized regression coefficients, R2 = 0.688; SEE = 208 kcal)
(unstandardized regression coefficients, R2 = 0.647; SEE = 250 kcal)
(unstandardized regression coefficients, R2 = 0.707; SEE = 201 kcal)
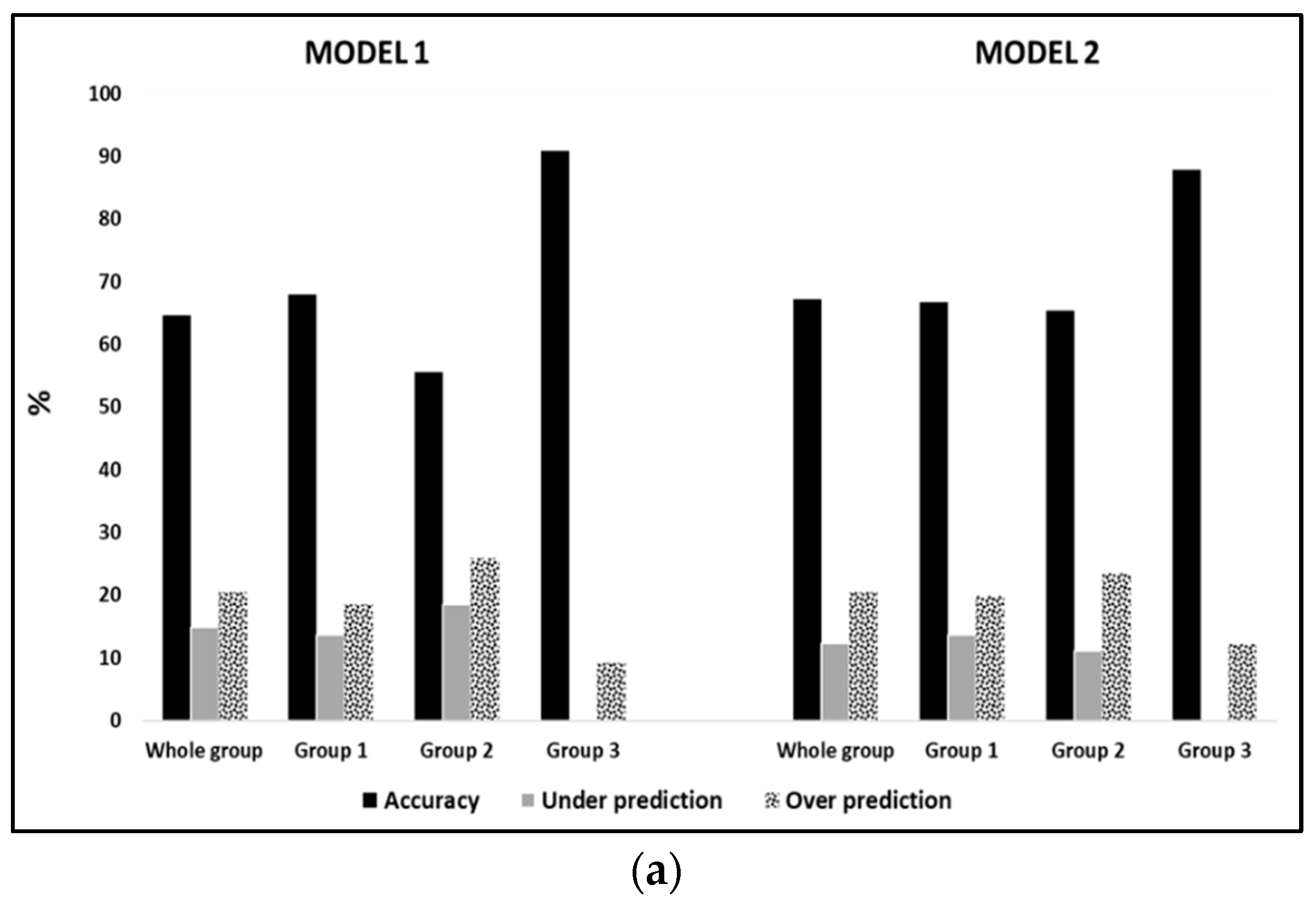
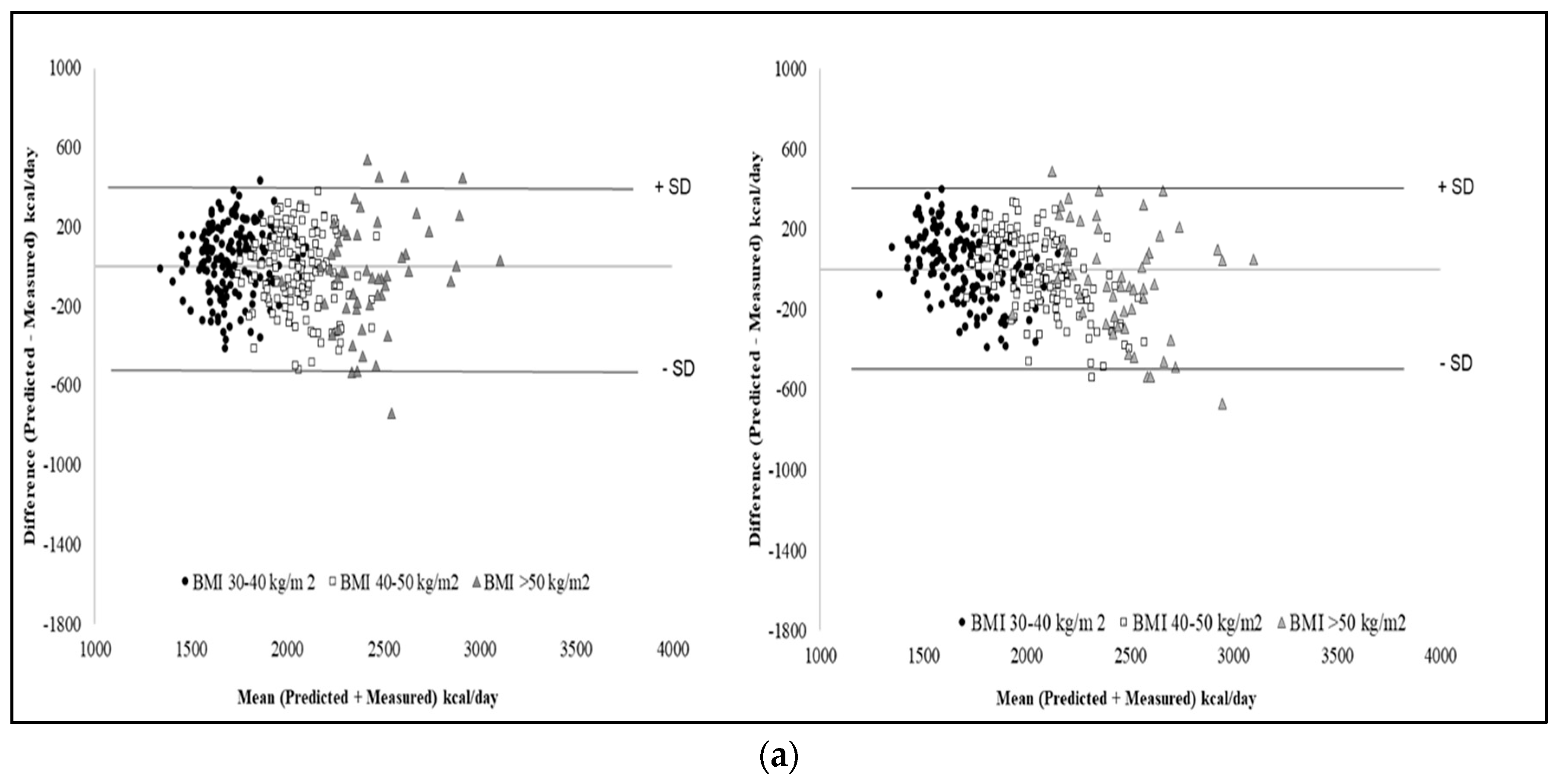
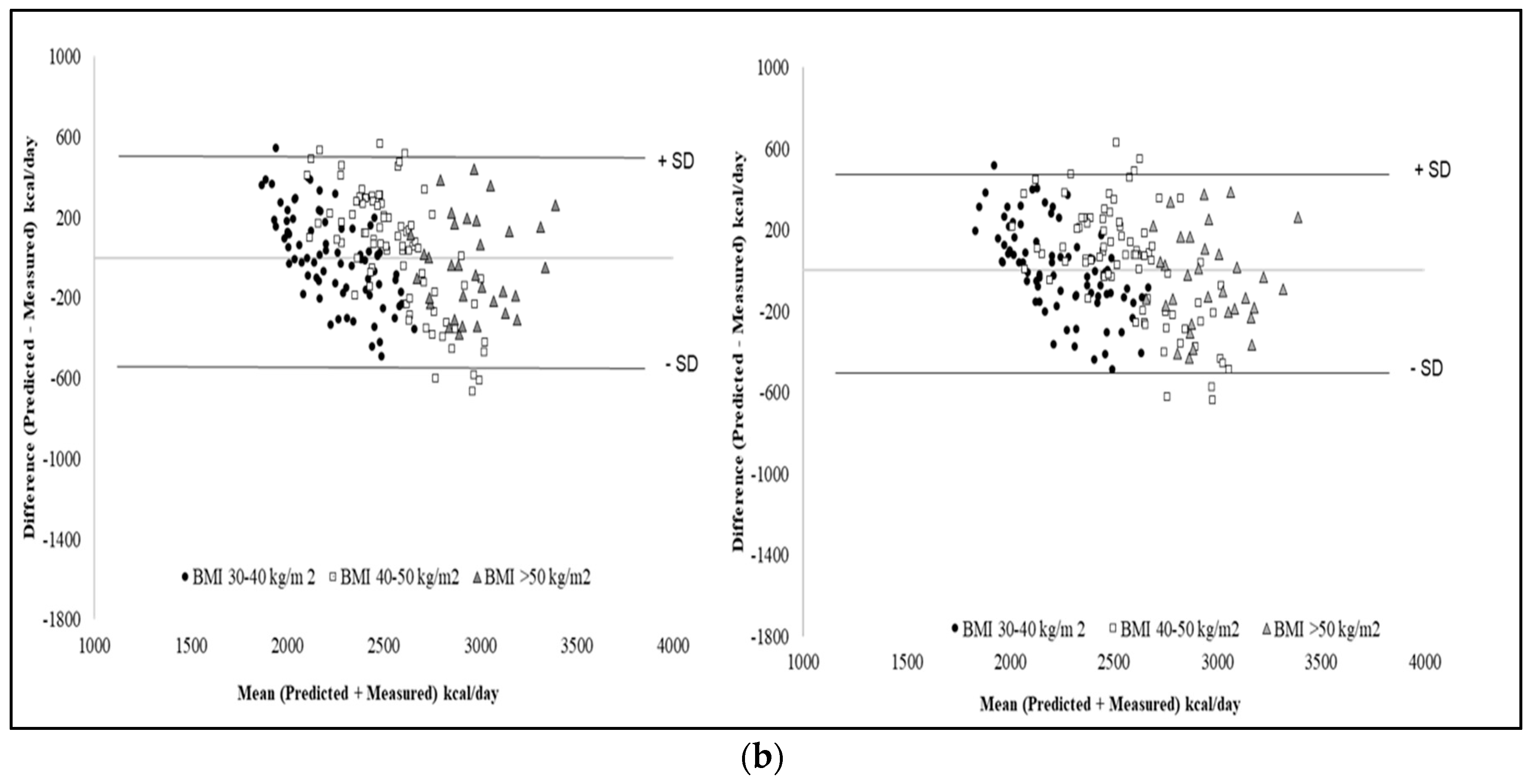
Validation of the New Predictive Equations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Heymsfield, S.B.; Harp, J.B.; Reitman, M.L.; Beetsch, J.W.; Schoeller, D.A.; Erondu, N.; Pietrobelli, A. Why do obese patients not lose more weight when treated with low-calorie diets? A mechanistic perspective. Am. J. Clin. Nutr. 2007, 85, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro Volp, A.C.; Esteves de Oliveira, F.C.; Duarte Moreira Alves, R.; Esteves, E.A.; Bressan, J. Energy expenditure: Components and evaluation methods. Nutr. Hosp. 2011, 26, 430–440. [Google Scholar]
- Bedogni, G.; Bertoli, S.; Leone, A.; De Amicis, R.; Lucchetti, E.; Agosti, F.; Marazzi, N.; Battezzati, A.; Sartorio, A. External validation of equations to estimate resting energy expenditure in 14952 adults with overweight and obesity and 1948 adults with normal weight from Italy. Clin. Nutr. 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Marra, M.; Cioffi, I.; Sammarco, R.; Montagnese, C.; Naccarato, M.; AmaPasanisi, F.V.; Contaldo, F. Prediction and evaluation of resting energy expenditure in a large group of obese outpatients. Int. J. Obes. (Lond.) 2017, 41, 697–705. [Google Scholar] [CrossRef]
- Marra, M.; Montagnese, C.; Sammarco, R.; Amato, V.; Della Valle, E.; Franzese, A.; Contaldo, F.; Pasanisi, F. Accuracy of predictive equations for estimating resting energy expenditure in obese adolescents. J. Pediatr. 2015, 166, 1390–1396. [Google Scholar] [CrossRef]
- Madden, A.M.; Mulrooney, H.M.; Shah, S. Estimation of energy expenditure using prediction equations in overweight and obese adults: A systematic review. J. Hum. Nutr. Diet. 2016, 29, 458–476. [Google Scholar] [CrossRef]
- Müller, M.J.; Bosy-Westphal, A.; Klaus, S.; Kreymann, G.; Lührmann, P.M.; Neuhäuser-Berthold, M.; Noack, R.; Pirke, K.M.; Platte, P.; Selberg, O.; et al. World Health Organization equations have shortcomings for predicting resting energy expenditure in person from a modern; affluent population: Generation of a new reference standard from a retrospective analysis of German database of resting energy expenditure. Am. J. Clin. Nutr. 2004, 80, 1379–1390. [Google Scholar]
- Jésus, P.; Achamrah, N.; Grigioni, S.; Charles, J.; Rimbert, A.; Folope, V.; Petit, A.; Déchelotte, P.; Coëffier, M. Validity of predictive equations for resting energy expenditure according to the body mass index in a population of 1726 patients followed in a Nutrition Unit. Clin. Nutr. 2015, 34, 529–535. [Google Scholar] [CrossRef]
- Huang, K.C.; Kormas, N.; Steinbeck, K.; Loughnan, G.; Caterson, I.D. Resting metabolic rate in severely obese diabetic and nondiabetic subjects. Obes. Res. 2004, 12, 840–845. [Google Scholar] [CrossRef]
- Horgan, G.W.; Stubbs, J. Predicting basal metabolic rate in the obese is difficult. Eur. J. Clin. Nutr. 2003, 57, 335–340. [Google Scholar] [CrossRef]
- Forbes, G.B.; Brown, M.R.; Welle, S.L.; Lipinski, B.A. Deliberate overfeeding in women and men: Energy cost and composition of the weight gain. Br. J. Nutr. 1986, 56, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bosy-Westphal, A.; Eichhorn, C.; Kutzner, D.; Illner, K.; Heller, M.; Müller, M.J. The age-related decline in resting energy expenditure in humans is due to the loss of fat-free mass and to alterations in its metabolically active components. J. Nutr. 2003, 133, 2356–2362. [Google Scholar] [CrossRef] [PubMed]
- Ravussin, E.; Burnand, B.; Schutz, Y.; Jéquier, E. Twentyfour-hour energy expenditure and resting metabolic rate in obese, moderately obese, and control subjects. Am. J. Clin. Nutr. 1982, 35, 566–573. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Di Renzo, L.; Morini, P.; de Miranda, R.C.; Romano, L.; Colica, C. New equations to estimate resting energy expenditure in obese adults from body composition. Acta Diabetol. 2018, 55, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Wilms, B.; Schmid, S.M.; Ernst, B.; Thurnheer, M.; Mueller, M.J.; Schultes, B. Poor prediction of resting energy expenditure in obese women by established equation. Metabolism 2010, 59, 1181–1189. [Google Scholar] [CrossRef]
- Weijs, P.J. Validity of predictive equations for resting energy expenditure in US and Dutch overweight and obese class I and II adults aged 18–65 y. Am. J. Clin. Nutr. 2008, 88, 959–970. [Google Scholar] [CrossRef]
- Achamrah, N.; Colange, G.; Delay, J.; Rimbert, A.; Folope, V.; Petit, A.; Grigioni, S.; Déchelotte, P.; Coëffier, M. Comparison of body composition assessment by DXA and BIA according to the body mass index: A retrospective study on 3655 measures. PLoS ONE 2018, 13, e0200465. [Google Scholar] [CrossRef]
- Day, K.; Kwok, A.; Evans, A.; Mata, F.; Verdejo-Garcia, A.; Hart, K.; Ward, L.C.; Truby, H. Comparison of a Bioelectrical Impedance Device against the Reference Method Dual Energy X-Ray Absorptiometry and Anthropometry for the Evaluation of Body Composition in Adults. Nutrients 2018, 10, 1469. [Google Scholar] [CrossRef]
- Das, S.K. Body composition measurement in severe obesity. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 602–606. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Manuel Gómez, J.; Lilienthal Heitmann, B.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis—Part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef]
- Norman, K.; Stobäus, N.; Pirlich, M.; Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin. Nutr. 2012, 31, 854–861. [Google Scholar] [CrossRef]
- Blauw, L.L.; Boon, M.R.; Rosendaal, F.R.; de Mutsert, R.; Gast, K.B.; van Dijk, K.W.; Rensen, P.C.; Dekkers, O.M.; NEO Study Group. Smoking is associated with increased resting energy expenditure in the general population: The NEO study. Metabolism 2015, 64, 1548–1555. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis—Part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Elia, M.; Livesey, G. Theory and validity of indirect calorimetry during net lipid synthesis. Am. J. Clin. Nutr. 1988, 47, 591–607. [Google Scholar] [CrossRef]
- Compher, C.; Frankenfield, D.; Keim, N.; Roth-Yousey, L. Evidence Analysis Working Group. Best practice methods to apply to measurement of resting metabolic rate in adults: A systematic review. J. Am. Diet. Assoc. 2006, 106, 881–903. [Google Scholar] [CrossRef] [PubMed]
- Fullmer, S.; Benson-Davies, S.; Earthman, C.P.; Frankenfield, D.C.; Gradwell, E.; Lee, P.S.; Piemonte, T.; Trabulsi, J. Evidence analysis library review of best practices for performing indirect calorimetry in healthy and non-critically ill individuals. J. Acad. Nutr. Diet. 2015, 115, 1417–1446. [Google Scholar] [CrossRef]
- Weir, J.B. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef]
- Frankenfield, D.; Roth-Yousey, L.; Compher, C.; The Evidence Analysis Working Group. Comparison of predictive equations for resting metabolic rate in healthy non-obese and obese adults: A systematic review. J. Am. Diet. Assoc. 2005, 105, 775–789. [Google Scholar] [CrossRef]
- Frankenfield, D.C.; Rowe, W.A.; Smith, J.S.; Cooney, R.N. Validation of several established equations for resting metabolic rate in obese and non-obese people. J. Am. Diet. Assoc. 2003, 103, 1152–1159. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Harris, J.; Benedict, F.G. A biometric study of human basal metabolism. Proc. Natl. Acad. Sci. USA 1918, 4, 370–373. [Google Scholar] [CrossRef]
- Henry, C.J. Basal metabolic rate studies in humans: Measurement and development of new equations. Public Health Nutr. 2005, 8, 1133–1152. [Google Scholar] [CrossRef]
- Mifflin, M.D.; St Jeor, S.T.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef]
- Lazzer, S.; Agosti, F.; Silvestri, P.; Derumeaux-Burel, H.; Sartorio, A. Prediction of resting energy expenditure in severely obese Italian women. J. Endocrinol. Investig. 2007, 30, 20–27. [Google Scholar] [CrossRef]
- Horie, L.M.; Gonzales, M.C.; Torrinhas, R.S.; Cecconello, I.; Waitzberg, D.L. New specific equation to estimate Resting Energy Expenditure in severely obese Patients. Obesity 2011, 19, 1090–1094. [Google Scholar] [CrossRef]
- Lazzer, S.; Bedogni, G.; Lafortuna, C.L.; Marazzi, N.; Busti, C.; Galli, R.; De Col, A.; Agosti, F.; Sartorio, A. Relationship between basal metabolic rate, gender, age, and body composition in 8780 white obese subjects. Obesity 2010, 18, 71–78. [Google Scholar] [CrossRef]
- Maddocks, M.; Kon, S.S.; Jones, S.E.; Canavan, J.L.; Nolan, C.M.; Higginson, I.J.; Gao, W.; Polkey, M.I.; Man, W.D. Bioelectrical impedance phase angle relates to function, disease severity and prognosis in stable chronic obstructive pulmonary disease. Clin. Nutr. 2015, 34, 1245–1250. [Google Scholar] [CrossRef]
- Orozco-Ruiz, X.; Pichardo-Ontiveros, E.; Tovar, A.R.; Torres, N.; Medina-Vera, I.; Prinelli, F.; Lafortuna, C.L.; Guevara-Cruz, M. Development and validation of new predictive equation for resting energy expenditure in adults with overweight and obesity. Clin. Nutr. 2018, 37, 2198–2205. [Google Scholar] [CrossRef]
- Bernstein, R.S.; Thornton, J.C.; Yang, M.U.; Wang, J.; Redmond, A.M.; Pierson, R.N., Jr.; Pi-Sunyer, F.X.; Van Itallie, T.B. Prediction of the resting metabolic rate in obese patients. Am. J. Clin. Nutr. 1983, 37, 595–602. [Google Scholar] [CrossRef]

| BMI Subgroup 1 | BMI Subgroup 2 | BMI Subgroup 3 | All Subjects | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M (n = 251) | F (n = 483) | M (n = 248) | F (n = 424) | M (n = 103) | F (n = 171) | M (n = 602) | F (n = 1078) | ||
| Age | years | 35.4 ± 12.1 | 35.4 ± 13.5 | 33.4 ± 11.8 | 34.4 ± 12.3 | 33.2 ± 10.8 * | 36.9 ± 11.1 | 34.2 ± 11.8 | 35.2 ± 12.7 |
| Weight | kg | 109 ± 11 * | 91 ± 10 | 135 ± 13 * | 116 ± 12 | 166 ± 17 * | 144 ± 14 | 129 ± 24 * | 109 ± 22 |
| Height | cm | 175 ± 6 * | 161 ± 6 | 174 ± 6 * | 162 ± 6 | 173 ± 8 * | 161 ± 6 | 174 ± 7 * | 161 ± 6 |
| BMI | kg/m2 | 35.5 ± 2.9 * | 35.0 ± 2.9 | 44.4 ± 2.8 | 44.4 ± 2.8 | 55.3 ± 4.2 | 55.8 ± 4.8 | 42.6 ± 7.7 | 42.0 ± 8.1 |
| BI-Index | cm2/Ω | 73.1 ± 9.5 * | 51.6 ± 6.7 | 79.1 ± 10.7 * | 58.2 ± 7.5 | 88.2 ± 12.3 * | 65.8 ± 9.1 | 78.1 ± 11.8 * | 56.5 ± 9.0 |
| PhA | degrees | 7.33 ± 0.89 * | 6.58 ± 0.82 | 7.36 ± 0.97 * | 6.73 ± 0.83 | 7.35 ± 1.03 * | 6.62 ± 0.98 | 7.34 ± 0.95 * | 6.64 ± 0.85 |
| MREE | kcal/d | 2225 ± 307 * | 1698 ± 221 | 2577 ± 344 * | 2112 ± 263 | 3009 ± 241 * | 2433 ± 299 | 2504 ± 420 * | 1978 ± 372 |
| RQ | 0.845 ± 0.053 | 0.843 ± 0.051 | 0.840 ± 0.060 | 0.837 ± 0.061 | 0.842 ± 0.062 | 0.829 ± 0.062 | 0.842 ± 0.061 | 0.839 ± 0.064 | |
| BMI Subgroup 1 | BMI Subgroup 2 | BMI Subgroup 3 | All Subjects | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M (n = 81) | F (n = 156) | M (n = 81) | F (n = 138) | M (n = 33) | F (n = 56) | M (n = 195) | F (n = 350) | ||
| Age | years | 34.2 ± 11.3 | 34.9 ± 13.4 | 34.1 ± 12.1 | 34.5 ± 12.2 | 34.1 ± 12.0 * | 36.7 ± 11.4 | 34.1 ± 11.7 | 35.1 ± 12.7 |
| Weight | kg | 109 ± 11.4 * | 90 ± 10 | 135 ± 12 * | 115 ± 10 | 162 ± 16 * | 143 ± 15 | 129 ± 23 * | 108 ± 22 |
| Height | cm | 176 ± 6 * | 161 ± 5 | 175 ± 6 * | 162 ± 6 | 173 ± 7 * | 161 ± 6 | 175 ± 7 * | 161 ± 6 |
| BMI | kg/m2 | 35.3 ± 3.0 * | 34.6 ± 2.8 | 44.2 ± 3.1 | 43.9 ± 2.6 | 55.3 ± 4.5 | 55.3 ± 4.5 | 42.2 ± 7.4 | 41.6 ± 8.0 |
| BI-Index | cm2/Ω | 73.3 ± 9.6 * | 51.2 ± 6.7 | 79.7 ± 10.4 * | 57.8 ± 6.5 | 87.8 ± 11.2 * | 65.4 ± 10.6 | 78.4 ± 11.4 * | 56.1 ± 9.0 |
| PhA | degrees | 7.36 ± 0.86 * | 6.56 ± 0.83 | 7.39 ± 0.89 * | 6.71 ± 0.92 | 7.28 ± 1.00 * | 6.57 ± 1.03 | 7.36 ± 0.89 * | 6.62 ± 0.9 |
| MREE | kcal/d | 2240 ± 290 * | 1683 ± 213 | 2545 ± 346 * | 2086 ± 260 | 2979 ± 217 * | 2480 ± 299 | 2492 ± 400 * | 1970 ± 381 |
| RQ | 0.838 ± 0.051 | 0.846 ± 0.052 | 0.826 ± 0.053 | 0.836 ± 0.062 | 0.829 ± 0.047 | 0.823 ± 0.061 | 0.831 ± 0.053 | 0.838 ± 0.054 | |
| BMI Subgroup 1 | BMI Subgroup 2 | BMI Subgroup 3 | All Subjects | |||||
|---|---|---|---|---|---|---|---|---|
| M (n = 251) | F (n = 483) | M (n = 248) | F (n = 424) | M (n = 103) | F (n = 171) | M (n = 602) | F (n = 1078) | |
| Age | −0.211 *** | −0.254 *** | −0.134 * | −0.238 *** | 0.07 | −0.023 | −0.160 *** | −0.126 *** |
| Weight | 0.638 *** | 0.569 *** | 0.569 *** | 0.629 *** | 0.458 *** | 0.462 *** | 0.785 *** | 0.826 *** |
| Height | 0.476 *** | 0.375 *** | 0.400 *** | 0.498 *** | 0.356 *** | 0.235 *** | 0.252 *** | 0.267 *** |
| BMI | 0.402 *** | 0.426 *** | 0.350 *** | 0.371 *** | 0.221 *** | 0.334 *** | 0.710 *** | 0.770 *** |
| BI-index | 0.384 *** | 0.424 *** | 0.418 *** | 0.416 *** | 0.471 *** | 0.486 *** | 0.572 *** | 0.652 *** |
| Phase angle | 0.115 * | 0.150 ** | 0.175 *** | 0.086 * | −0.072 | 0.204 ** | 0.093 ** | 0.123 *** |
| Model | Sex | Predictive Equations | R2 | SEE (kcal/d) |
|---|---|---|---|---|
| BMI Subgroup 1 (n = 251 M; n = 483 F) | ||||
| 1 | M | REE = 16.6 × Weight − 3.23 × Age + 536 | 0.423 | 233 |
| 2 | M | REE = 14.6 × Weight − 3.32 × Age + 34.9 × PhA + 4.7 × BI-I + 157 | 0.444 | 230 |
| 1 | F | REE = 11.9 × Weight − 2.48 × Age + 704 | 0.347 | 178 |
| 2 | F | REE = 10 × Weight − 2.34 × Age + 32 × PhA + 4.7 × BI-I + 416 | 0.374 | 175 |
| BMI Subgroup 2 (n = 248 M; n = 424 F) | ||||
| 1 | M | REE=15.4 × Weight – 2.71 × Age + 585 | 0.333 | 282 |
| 2 | M | REE=12.1 × Weight − 3.48 × Age + 52.1 × PhA + 6.12 × BI-I + 191 | 0.373 | 274 |
| 1 | F | REE=13.8 × Weight − 2.67 × Age + 597 | 0.408 | 202 |
| 2 | F | REE= 12.6 × Weight − 2.64 × Age + 31.2 × PhA + 3.4 × BI-I + 324 | 0.422 | 200 |
| BMI Subgroup 3 (n = 103 M; n = 171 F) | ||||
| 1 | M | REE = 6.32 × Weight + 1960 | 0.210 | 215 |
| 2 | M | REE = 4.09 × Weight + 6.81 × BI-I + 1730 | 0.315 | 200 |
| 1 | F | REE = 9.59 × Weight +1051 | 0.213 | 261 |
| 2 | F | REE = 6.90 × Weight + 88.6 × PhA + 11.4 × BI-I + 84 | 0.324 | 245 |
| Bias (Mean Percentage Difference between Predicted and Measured REE) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Subjects | BMI Subgroup 1 | BMI Subgroup 2 | BMI Subgroup 3 | |||||||||||||
| M (n = 195) | F (n = 350) | M (n = 81) | F (n = 156) | M (n = 81) | F (n = 138) | M (n = 33) | F (n = 56) | |||||||||
| Model | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 |
| Eq developed in: | ||||||||||||||||
| Whole sample | 1.5 | 1.4 | 1.1 | 0.8 | 0.9 | 1.4 | 3.0 | 2.7 | 2.5 | 2.6 | −0.7 | −0.5 | −1.8 | −1.2 | −1.2 | −1.2 |
| Subgroup 1 | 1.1 | 1.0 | 1.5 | 1.2 | ||||||||||||
| Subgroup 2 | 2.2 | 2.0 | 1.2 | 0.9 | ||||||||||||
| Subgroup 3 | 0.5 | 0.4 | −1.2 | −0.6 | ||||||||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marra, M.; Cioffi, I.; Sammarco, R.; Santarpia, L.; Contaldo, F.; Scalfi, L.; Pasanisi, F. Are Raw BIA Variables Useful for Predicting Resting Energy Expenditure in Adults with Obesity? Nutrients 2019, 11, 216. https://doi.org/10.3390/nu11020216
Marra M, Cioffi I, Sammarco R, Santarpia L, Contaldo F, Scalfi L, Pasanisi F. Are Raw BIA Variables Useful for Predicting Resting Energy Expenditure in Adults with Obesity? Nutrients. 2019; 11(2):216. https://doi.org/10.3390/nu11020216
Chicago/Turabian StyleMarra, Maurizio, Iolanda Cioffi, Rosa Sammarco, Lidia Santarpia, Franco Contaldo, Luca Scalfi, and Fabrizio Pasanisi. 2019. "Are Raw BIA Variables Useful for Predicting Resting Energy Expenditure in Adults with Obesity?" Nutrients 11, no. 2: 216. https://doi.org/10.3390/nu11020216
APA StyleMarra, M., Cioffi, I., Sammarco, R., Santarpia, L., Contaldo, F., Scalfi, L., & Pasanisi, F. (2019). Are Raw BIA Variables Useful for Predicting Resting Energy Expenditure in Adults with Obesity? Nutrients, 11(2), 216. https://doi.org/10.3390/nu11020216







