Intestinal Phosphorus Absorption in Chronic Kidney Disease
Abstract
:1. Introduction: The Importance of Managing Phosphorus Homeostasis in CKD
1.1. CKD is a Major Health Problem that Disrupts Phosphorus Metabolism
1.2. Reducing Dietary Phosphorus Intake or Absorption is a Strategy to Combat the Effects of CKD on Phosphorus Homeostasis
2. Overview of the Physiologic Mechanisms Controlling Phosphorus Homeostasis
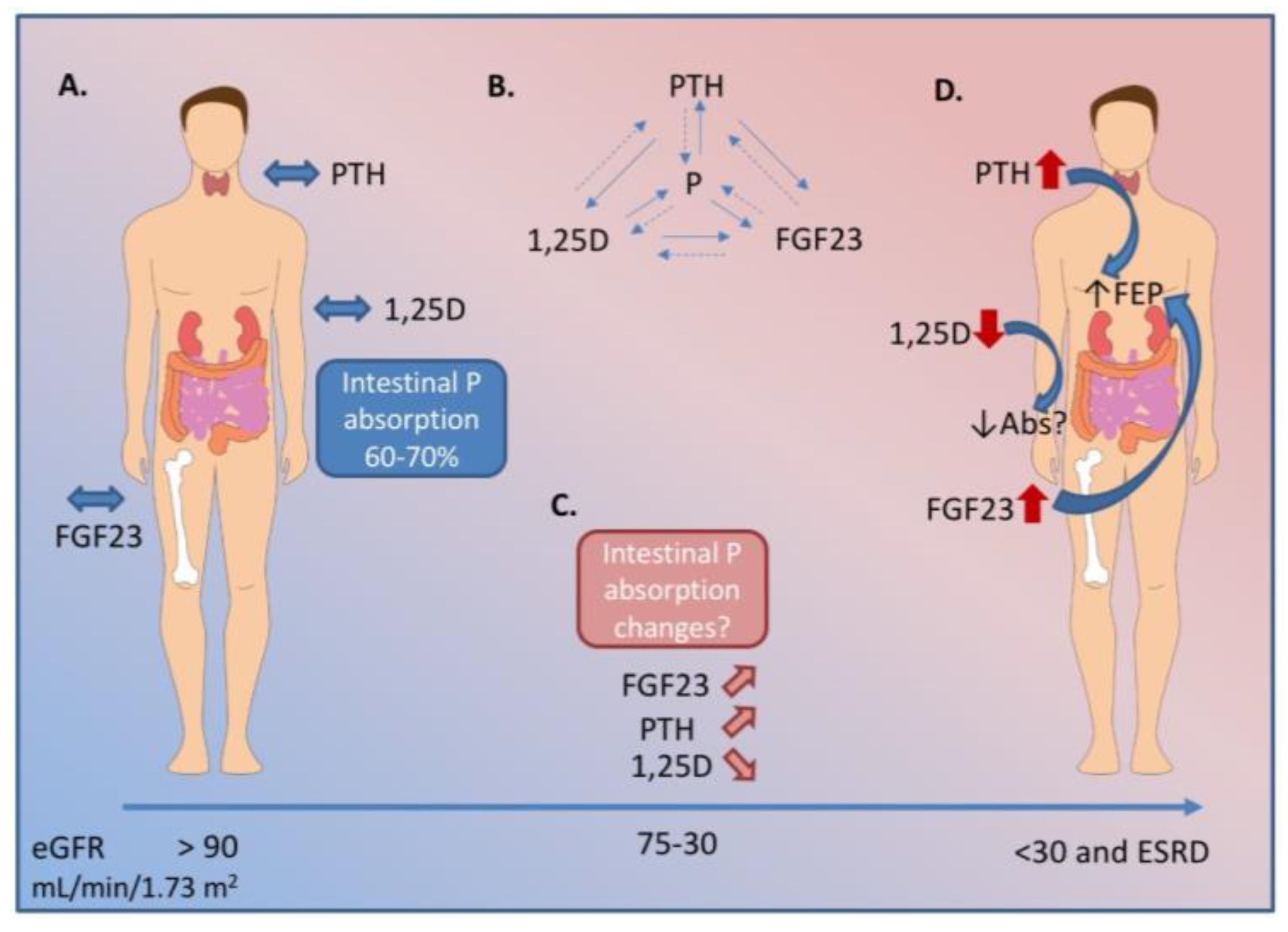
3. Mechanisms of Intestinal Phosphorus Absorption
4. 1,25-Dihydroxvitamin D Regulation of Intestinal Phosphorus Absorption
5. Role of Dietary Phosphorus Load in Intestinal Phosphorus Absorption
6. The Pathophysiological Changes in Phosphorus Homeostasis in Chronic Kidney Disease
6.1. CKD is a Progressive Disease Affecting Phosphorus Homeostasis
6.2. Phosphorus Management in CKD is Challenged by Insufficient Clinical Management Strategies
7. Intestinal Phosphorus Absorption in the Context of CKD
8. Summary and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Andrew, S.L.; Josef, C.; Kline, B. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39, S12–S66. [Google Scholar]
- Isakova, T.; Wahl, P.; Vargas, G.S.; Gutierrez, O.M.; Scialla, J.; Xie, H.; Appleby, D.; Nessel, L.; Bellovich, K.; Chen, J.; et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 2011, 79, 1370–1378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moe, S.; Drueke, T.; Cunningham, J.; Goodman, W.; Martin, K.; Olgaard, K.; Ott, S.; Sprague, S.; Lameire, N.; Eknoyan, G.; et al. Definition, evaluation, and classification of renal osteodystrophy: A position statement from kidney disease: Improving global outcomes (KDIGO). Kidney Int. 2006, 69, 1945–1953. [Google Scholar] [CrossRef] [PubMed]
- Bernasconi, R.; Aeschbacher, S.; Blum, S.; Mongiat, M.; Girod, M.; Todd, J.; Estis, J.; Nolan, N.; Renz, H.; Risch, L.; et al. Fibroblast growth factor 23 and renal function among young and healthy individuals. Clin. Chem. Lab. Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, O.M.; Mannstadt, M.; Isakova, T.; Tauh-Hain, J.A.; Tamez, H.; Shah, A.; Smith, K.; Lee, H.; Thadhani, R.; Juppner, H.; et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. New Engl. J. Med. 2008, 359, 584–592. [Google Scholar] [CrossRef] [PubMed]
- National Kidney Foundation. K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Chronic Kidney Disease. Available online: http://www2.kidney.org/professionals/KDOQI/guidelines_bone/ (accessed on 1 August 2018).
- Lopez-Hilker, S.D.A.R.N.S.; Martin, K.J.; Slatopolsky, E. Phosphorus restriction reverses hyperparathyroidism in uremia independent of changes in calcium and calcitriol. Ren. Fluid. Electrol. Physiol. 1990, 28, F432–F437. [Google Scholar] [CrossRef] [PubMed]
- Medicine, I.O. Dietary Reference Intakes For Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride; National Academy Press: Washington, DC, USA, 1997; p. 432. [Google Scholar]
- Calvo, M.S.; Park, Y.K. Changing phosphorus content of the us diet: Potential adverse effects on bone. J. Nutr. 1996, 126, S1168–S1180. [Google Scholar] [CrossRef] [PubMed]
- Calvo, M.S.; Uribarri, J. Contributions to total phosphorus intake: All sources considered. Seminars Dial. 2013, 26, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.C.; Shi, M.; Cho, H.J.; Adams-Huet, B.; Paek, J.; Hill, K.; Shelton, J.; Amaral, A.P.; Faul, C.; Taniguchi, M.; et al. Klotho and phosphate are modulators of pathologic uremic cardiac remodeling. JASN 2015, 26, 1290–1302. [Google Scholar] [CrossRef] [PubMed]
- Moorthi, R.N.; Moe, S.M. CKD-mineral and bone disorder: Core curriculum 2011. Am. J. Kidney Dis. 2011, 58, 1022–1036. [Google Scholar] [CrossRef] [PubMed]
- Uribarri, J. Phosphorus homeostasis in normal health and in chronic kidney disease patients with special emphasis on dietary phosphorus intake. Seminars Dial. 2007, 20, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Deng, M.; Zhao, J.; Huang, L. Decreased expression of klotho gene in uremic atherosclerosis in apolipoprotein E-deficient mice. Biochem. Biophys. Res. Commun. 2010, 391, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Block, G.A.; Ix, J.H.; Ketteler, M.; Martin, K.J.; Thadhani, R.I.; Tonelli, M.; Wolf, M.; Juppner, H.; Hruska, K.; Wheeler, D.C. Phosphate homeostasis in CKD report of a scientific symposium sponsored by the national kidney foundation. Am. J. Kidney Dis. 2013, 62, 457–473. [Google Scholar] [CrossRef] [PubMed]
- Berndt, T.; Kumar, R. Novel mechanisms in the regulation of phosphorus homeostasis. Physiology 2009, 24, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Bergwitz, C.; Juppner, H. Regulation of phosphate homeostasis by PHD, vitamin D, and FGF23. Annu. Rev. Med. 2010, 61, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Perwad, F.; Zhang, M.Y.; Tenenhouse, H.S.; Portale, A.A. Fibroblast growth factor 23 impairs phosphorus and vitamin D metabolism in vivo and suppresses 25-hydroxyvitamin d-1alpha-hydroxylase expression in vitro. Am. J. Physiol. Ren. Physiol. 2007, 293, F1577–F1583. [Google Scholar] [CrossRef] [PubMed]
- Silver, J.; Naveh-Many, T. Phosphate and the parathyroid. Kidney Int. 2009, 75, 898–905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walling, M. Intestinal Ca and phosphate transport differential responses to vitamin D3 metabolites. Am. J. Physiol. 1977, 2, E488–E494. [Google Scholar] [CrossRef] [PubMed]
- Rizzoli, R.F.H.; Bonjour, J.P. Role of 1,25-dihydroxyvitamin D3 on intestinal phosphate absorption in rats with a normal vitamin D supply. J. Clin. Investig. 1977, 60, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.B.; DeLuca, H.F. Characterization of intestinal phosphate absorption using a novel in vivo method. AJP: Endocrinol. Metab. 2007, 292, E1917–E1921. [Google Scholar] [CrossRef] [PubMed]
- Burnett-Bowie, S.M.; Henao, M.P.; Dere, M.E.; Lee, H.; Leder, B.Z. Effects of hPTH(1–34) infusion on circulating serum phosphate, 1,25-dihydroxyvitamin D, and FGF23 levels in healthy men. J. Bone Miner. Res. 2009, 24, 1681–1685. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, T.O.; Imel, E.A.; Holm, I.A.; Jan de Beur, S.M.; Insogna, K.L. A clinician’s guide to X-linked hypophosphatemia. J. Bone Miner. Res. 2011, 26, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Ritter, C.S.; Slatopolsky, E. Phosphate toxicity in CKD: The killer among us. CJASN 2016, 11, 1088–1100. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.Y.; Kuro-o, M.; Razzaque, M.S. Molecular regulation of phosphate metabolism by fibroblast growth factor-23-klotho system. Adv. Chronic Kidney Dis. 2011, 18, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Inoue, Y.; Segawa, H.; Kaneko, I.; Yamanaka, S.; Kusano, K.; Kawakami, E.; Furutani, J.; Ito, M.; Kuwahata, M.; Saito, H.; et al. Role of the vitamin D receptor in FGF23 action on phosphate metabolism. Biochem. J. 2005, 390, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, K.J.; Murer, H. Sulphate and phosphate transport in the renal proximal tubule. Philos. Trans. R. Soc. B Biol. Sci. 1982, 299, 549–558. [Google Scholar] [CrossRef]
- Forster, I.C.; Hernando, N.; Biber, J.; Murer, H. Phosphate transporters of the SLC20 and SLC 34 families. Mol. Asp. Medicine 2013, 34, 386–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernando, N.; Wagner, C.A. Mechanisms and regulation of intestinal phosphate absorption. Compr. Physiol. 2018, 8, 1065–1090. [Google Scholar] [PubMed]
- Sabbagh, Y.; O’Brien, S.P.; Song, W.; Boulanger, J.H.; Stockmann, A.; Arbeeny, C.; Schiavi, S.C. Intestinal npt2b plays a major role in phosphate absorption and homeostasis. JASN 2009, 20, 2348–2358. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, C.; Meinild, A.K.; Murer, H.; Forster, I.C. Voltage- and substrate-dependent interactions between sites in putative re-entrant domains of a Na(+)-coupled phosphate cotransporter. Eur. J. Physiol. 2011, 461, 645–663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, G.R.; Zerwekh, J.E.; Parker, T.F.; Krejs, G.J.; Pak, C.Y.; Fordtran, J.S. Absorption of phosphate in the jejunum of patients with chronic renal failure before and after correction of vitamin D deficiency. Gastroenterology 1983, 85, 908–916. [Google Scholar] [PubMed]
- Katai, K.M.K.; Kishida, S.; Segawa, H.; Nii, H.; Tanaka, H.; Tani, Y.; Arai, H.; Tatsumi, S.; Morita, K.; Taketani, Y.; et al. Regulation of intestinal Na+-dependent phosphate co-transporters by a low-phosphate diet and 1,25-dyhydroxyvitamin D3. Biochem. J. 1999, 343, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Bai, L.; Collins, J.F.; Ghishan, F.K. Age-dependent regulation of rat intestinal type iib sodium-phosphate cotransporter by 1,25-(OH)(2) vitamin D(3). Am. J. Physiol. Cell. Physiol. 2002, 282, C487–C493. [Google Scholar] [CrossRef] [PubMed]
- Nemere, I.; Garcia-Garbi, N.; Hammerling, G.J.; Winger, Q. Intestinal cell phosphate uptake and the targeted knockout of the 1,25D3-MARRS receptor/PDIA3/ERp57. Endocrinology 2012, 153, 1609–1615. [Google Scholar] [CrossRef] [PubMed]
- Capuano, P.R.T.; Wagner, C.A.; Bacic, D.; Kato, S.; Uchiyama, Y.; St-Arnoud, R.; Murer, H.; Biber, J. Intestinal and renal adaptation to a low-Pi diet of type II NaPi cotransporters in vitamin D receptor- and 1alphaOHase-deficient mice. J. Physiol. Cell. Physiol. 2004, 288, C429–C434. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.B.; Walling, W.M.; Brautbar, N. Intestinal phosphate absorption: Influence of vitamin D and non vitamin D factors. Am. J. Physiol. Gastrointest. Liver Physiol. 1986, 205, G369–G373. [Google Scholar] [CrossRef] [PubMed]
- Giral, H.; Caldas, Y.; Sutherland, E.; Wilson, P.; Breusegem, S.; Barry, N.; Blaine, J.; Jiang, T.; Wang, X.; Levi, M. Regulation of rat intestinal na-dependent phosphate transporters by dietary phosphate. Am. J. Physiol. Ren. Physiol. 2009, 297, F1466–F1475. [Google Scholar] [CrossRef] [PubMed]
- Saddoris, K.L.; Fleet, J.C.; Radcliffe, J.S. Sodium-dependent phosphate uptake in the jejunum is post-transcriptionally regulated in pigs fed a low-phosphorus diet and is independent of dietary calcium concentration. J. Nutr. 2010, 140, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.; Churchill, L.J.; Srai, S.K.; Biber, J.; Murer, H.; Jaeger, P.; Debnam, E.S.; Unwin, R.J.; Epithelial, T.; Cell Biology, G. Intestinal phosphate absorption in a model of chronic renal failure. Kidney Int. 2007, 72, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Isakova, T.; Gutierrez, O.M.; Smith, K.; Epstein, M.; Keating, L.K.; Juppner, H.; Wolf, M. Pilot study of dietary phosphorus restriction and phosphorus binders to target fibroblast growth factor 23 in patients with chronic kidney disease. Nephrol. Dial. Transplant. 2011, 26, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Segawa, H.; Kaneko, I.; Yamanaka, S.; Ito, M.; Kuwahata, M.; Inoue, Y.; Kato, S.; Miyamoto, K. Intestinal Na-P(i) cotransporter adaptation to dietary P(i) content in vitamin D receptor null mice. Am. J. Physiol. Ren. Physiol. 2003, 287, F39–F47. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, H.; Nagano, N.; Urakawa, I.; Yamazaki, Y.; Iijima, K.; Fujita, T.; Yamashita, T.; Fukumoto, S.; Shimada, T. Direct evidence for a causative role of FGF23 in the abnormal renal phosphate handling and vitamin D metabolism in rats with early-stage chronic kidney disease. Kidney Int. 2010, 78, 975–980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolf, M. Mineral (mal)adaptation to kidney disease—Young investigator award address: American society of nephrology kidney week 2014. CJASN 2015, 10, 1875–1885. [Google Scholar] [CrossRef] [PubMed]
- Koh, N.; Fujimori, T.; Nishiguchi, S.; Tamori, A.; Shiomi, S.; Nakatani, T.; Sugimura, K.; Kishimoto, T.; Kinoshita, S.; Kuroki, T.; et al. Severely reduced production of klotho in human chronic renal failure kidney. Biochem. Biophys. Res. Commun. 2001, 280, 1015–1020. [Google Scholar] [CrossRef] [PubMed]
- Faul, C.; Amaral, A.P.; Oskouei, B.; Hu, M.C.; Sloan, A.; Isakova, T.; Gutierrez, O.M.; Aguillon-Prada, R.; Lincoln, J.; Hare, J.M.; et al. FGF23 induces left ventricular hypertrophy. J. Clin. Investig. 2011, 121, 4393–4408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dhingra, R.; Sullivan, L.M.; Fox, C.S.; Wang, T.J.; D’Agostino, R.B., Sr.; Gaziano, J.M.; Vasan, R.S. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch. Int. Med. 2007, 167, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Karp, H.; Ekholm, P.; Kemi, V.; Itkonen, S.; Hirvonen, T.; Narkki, S.; Lamberg-Allardt, C. Differences among total and in vitro digestible phosphorus content of plant foods and beverages. J. Ren. Nutr. 2012, 22, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Waheed, A.A.; Pedraza, F.; Lenz, O.; Isakova, T. Phosphate control in end-stage renal disease: Barriers and opportunities. Nephrol. Dial. Transplant. 2013, 28, 2961–2968. [Google Scholar] [CrossRef] [PubMed]
- Murtaugh, M.A.; Filipowicz, R.; Baird, B.C.; Wei, G.; Greene, T.; Beddhu, S. Dietary phosphorus intake and mortality in moderate chronic kidney disease: Nhanes iii. Nephrol. Dial. Transplant. 2012, 27, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Hill Gallant, K.M.; Weaver, C.M.; Towler, D.A.; Thuppal, S.V.; Bailey, R.L. Nutrition in cardioskeletal health. Adv. Nutr. 2016, 7, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Calvo, M.S.; Moshfegh, A.J.; Tucker, K.L. Assessing the health impact of phosphorus in the food supply: Issues and considerations. Adv. Nutr. 2014, 5, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, C.; Sayre, S.S.; Leon, J.B.; Machekano, R.; Love, T.E.; Porter, D.; Marbury, M.; Sehgal, A.R. Effect of food additives on hyperphosphatemia among patients with end-stage renal disease: A randomized controlled trial. JAMA 2009, 301, 629–635. [Google Scholar] [CrossRef] [PubMed]
- De Fornasari, M.L.; Dos Santos Sens, Y.A. Replacing phosphorus-containing food additives with foods without additives reduces phosphatemia in end-stage renal disease patients: A randomized clinical trial. J. Ren. Nutr. 2017, 27, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, J.; Scanni, R.; Bestmann, L.; Hulter, H.N.; Krapf, R. A controlled increase in dietary phosphate elevates BP in healthy human subjects. JASN 2018, 29, 2089–2098. [Google Scholar] [CrossRef] [PubMed]
- Moorthi, R.N.; Armstrong, C.L.; Janda, K.; Ponsler-Sipes, K.; Asplin, J.R.; Moe, S.M. The effect of a diet containing 70% protein from plants on mineral metabolism and musculoskeletal health in chronic kidney disease. Am. J. Nephrol. 2014, 40, 582–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- St-Jules, D.E.; Woolf, K.; Pompeii, M.L.; Kalantar-Zadeh, K.; Sevick, M.A. Reexamining the phosphorus-protein dilemma: Does phosphorus restriction compromise protein status? J. Ren. Nutr. 2016, 26, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Moe, S.M.; Chertow, G.M. The case against calcium-based phosphate binders. CJASN 2006, 1, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Friedman, E.A. Calcium-based phosphate binders are appropriate in chronic renal failure. CJASN 2006, 1, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Hill, K.M.; Martin, B.R.; Wastney, M.E.; McCabe, G.P.; Moe, S.M.; Weaver, C.M.; Peacock, M. Oral calcium carbonate affects calcium but not phosphorus balance in stage 3–4 chronic kidney disease. Kidney Int. 2013, 83, 959–966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spiegel, D.M.; Brady, K. Calcium balance in normal individuals and in patients with chronic kidney disease on low- and high-calcium diets. Kidney Int. 2012, 81, 1116–1122. [Google Scholar] [CrossRef] [PubMed]
- Block, G.A.; Wheeler, D.C.; Persky, M.S.; Kestenbaum, B.; Ketteler, M.; Spiegel, D.M.; Allison, M.A.; Asplin, J.; Smits, G.; Hoofnagle, A.N.; et al. Effects of phosphate binders in moderate CKD. JASN 2012, 23, 1407–1415. [Google Scholar] [CrossRef] [PubMed]
- SM, M. Current diagnosis & treatment. Nephrology & hypertension. In Current Diagnosis & Treatment. Nephrology & Hypertension; Lerma, E.V. McGraw-Hill Medical: New York, NY, USA, 2018; pp. 237–254. [Google Scholar]
- Gutekunst, L. An update on phosphate binders: A dietitian’s perspective. J. Ren. Nutr. 2016, 26, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Farrington, K.; Newman, S.P.; Varghese, Z.; Moorhead, J.F. Comparison of radioisotope methods for the measurement of phosphate absorption in normal subjects and in patients with chronic renal failure. Clin. Sci. 1979, 60, 55–63. [Google Scholar] [CrossRef]
- Loghman-Adham, M. Renal and intestinal pi transport adaptation to low phosphorus diet in uremic rats. JASN 1993, 3, 1930–1937. [Google Scholar] [PubMed]
- Stremke, E.R.; McCabe, L.D.; McCabe, G.P.; Martin, B.R.; Moe, S.M.; Weaver, C.M.; Peacock, M.; Hill Gallant, K.M. Twenty-four-hour urine phosphorus as a biomarker of dietary phosphorus intake and absorption in ckd: A secondary analysis from a controlled diet balance study. CJASN 2018, 13, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stremke, E.R.; Hill Gallant, K.M. Intestinal Phosphorus Absorption in Chronic Kidney Disease. Nutrients 2018, 10, 1364. https://doi.org/10.3390/nu10101364
Stremke ER, Hill Gallant KM. Intestinal Phosphorus Absorption in Chronic Kidney Disease. Nutrients. 2018; 10(10):1364. https://doi.org/10.3390/nu10101364
Chicago/Turabian StyleStremke, Elizabeth R., and Kathleen M. Hill Gallant. 2018. "Intestinal Phosphorus Absorption in Chronic Kidney Disease" Nutrients 10, no. 10: 1364. https://doi.org/10.3390/nu10101364



