Impact of Packing and Processing Technique on Mechanical Properties of Acrylic Denture Base Materials
Abstract
:1. Introduction
2. Results and Discussion
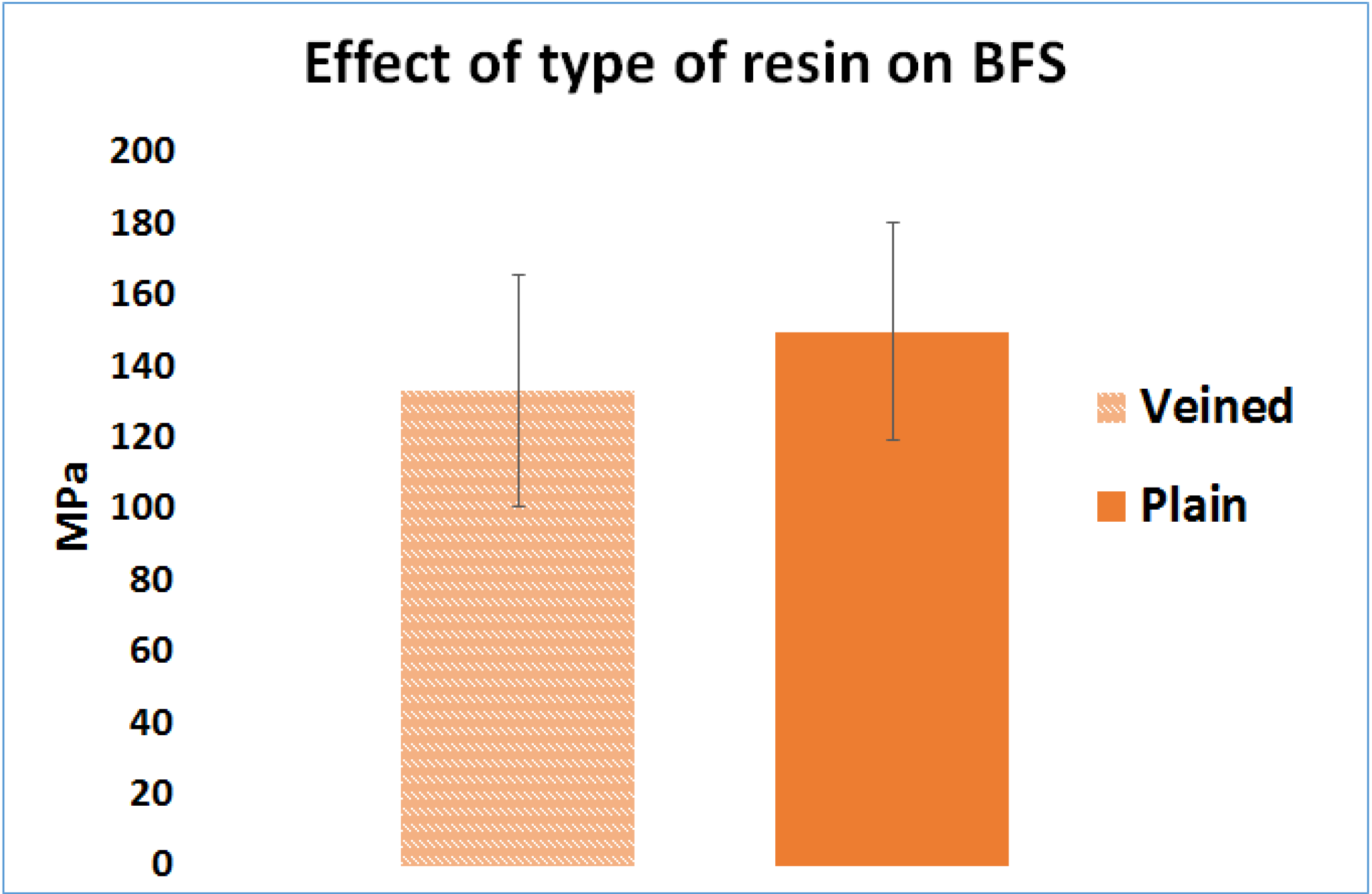
2.1. Effect of the Resin Type (Factor A)
2.2. Effect of Packing Method on Biaxial Flexural Strength (Factor B)

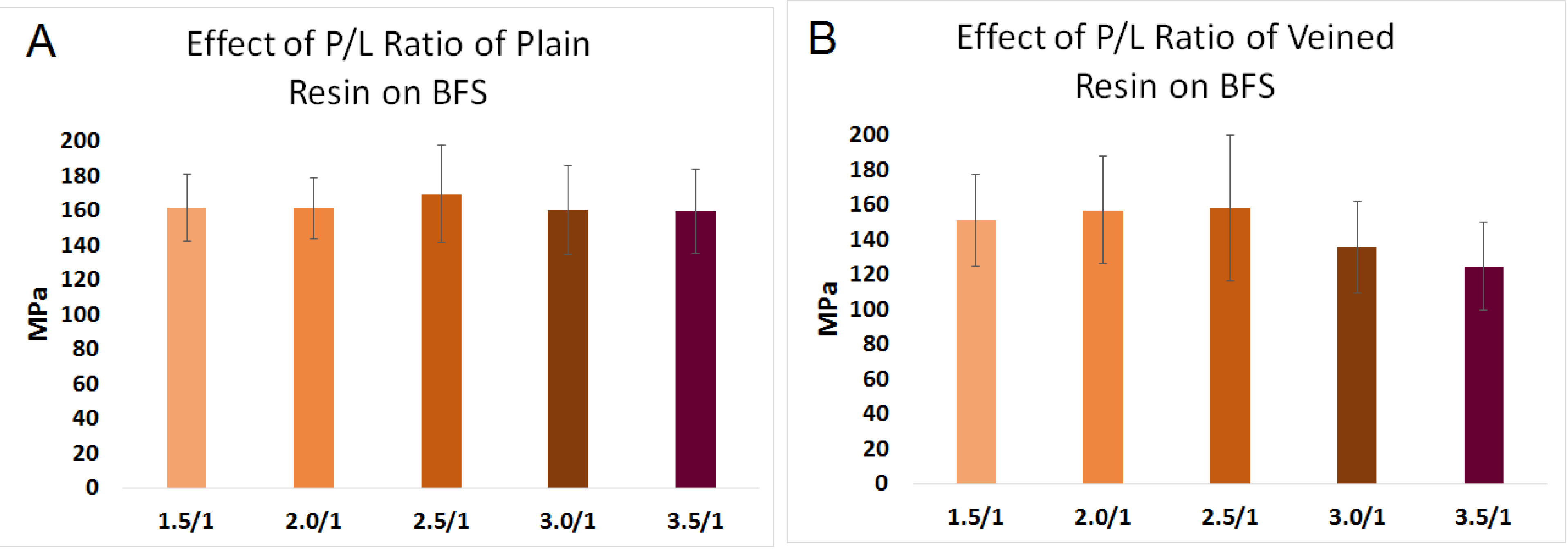
2.3. Effect of Powder-to-Liquid Ratio on BFS (Factor C)
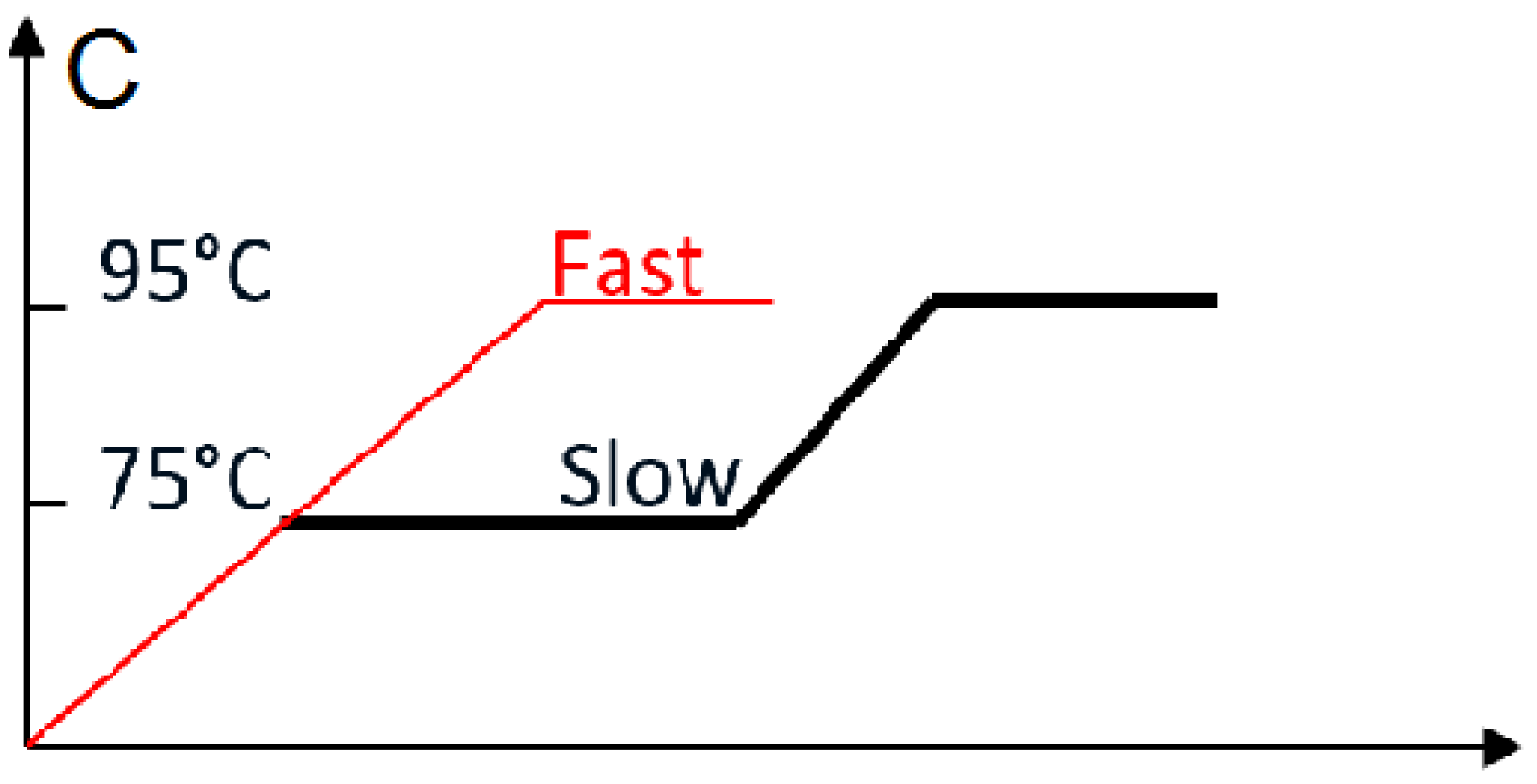
2.4. Effect of Curing Time in Water Bath (Factor E)

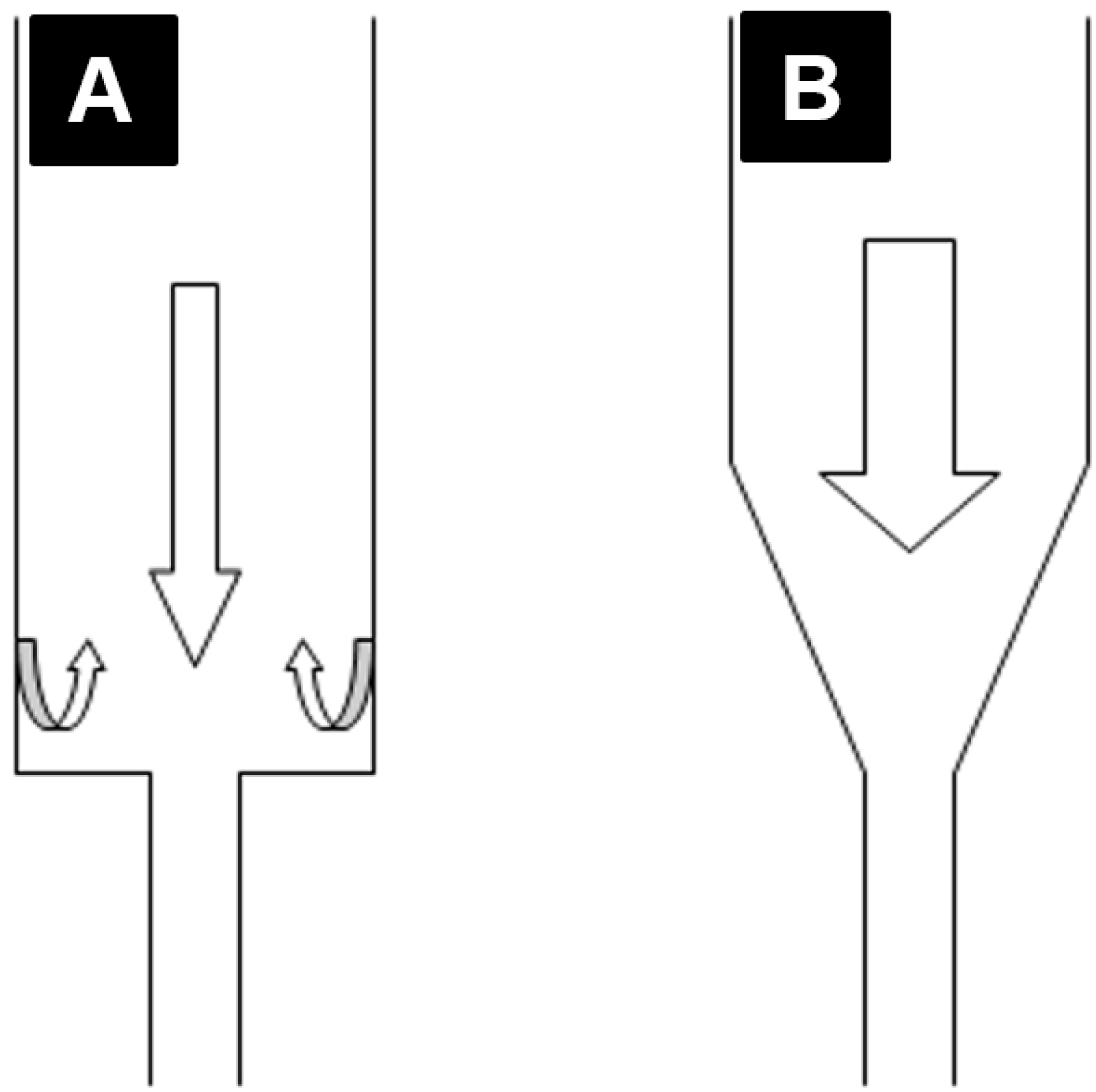
2.5. Effect of Extruder Angle on Mechanical Properties of PMMA
2.5.1. Effect of Extruder Angle on BFS of PMMA
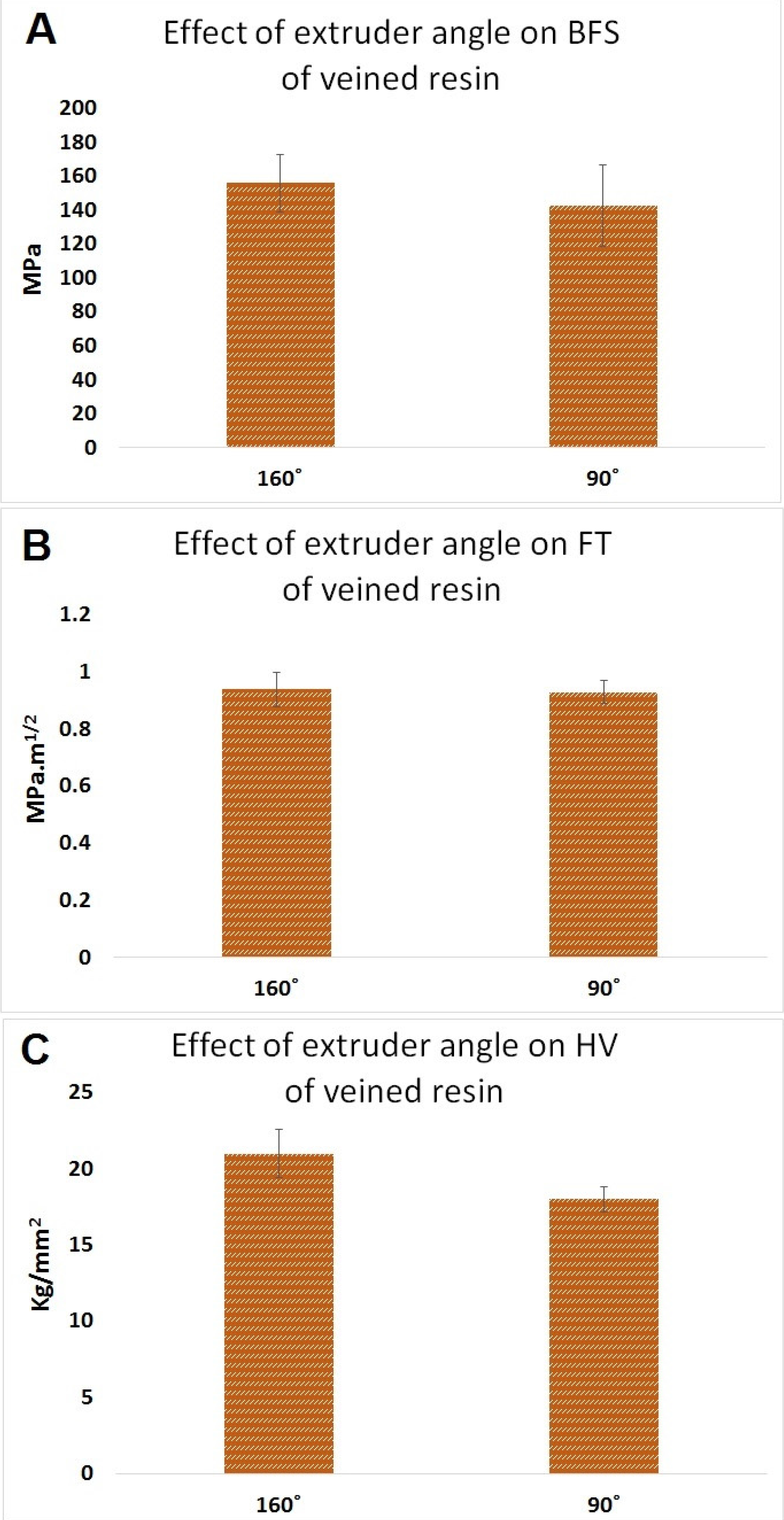
2.5.2. Effect of Extruder Angle on Fracture Toughness of PMMA
2.5.3. Effect of Extruder Angle on Hardness of PMMA
2.6. Analysis of Temperature within Curing Baths; Inside and Outside Curing Resin

2.7. Discussion

3. Experimental Section
3.1. Materials
3.2. Sample Preparation
3.3. Factor Codes
3.4. Wax Discs’ Preparation
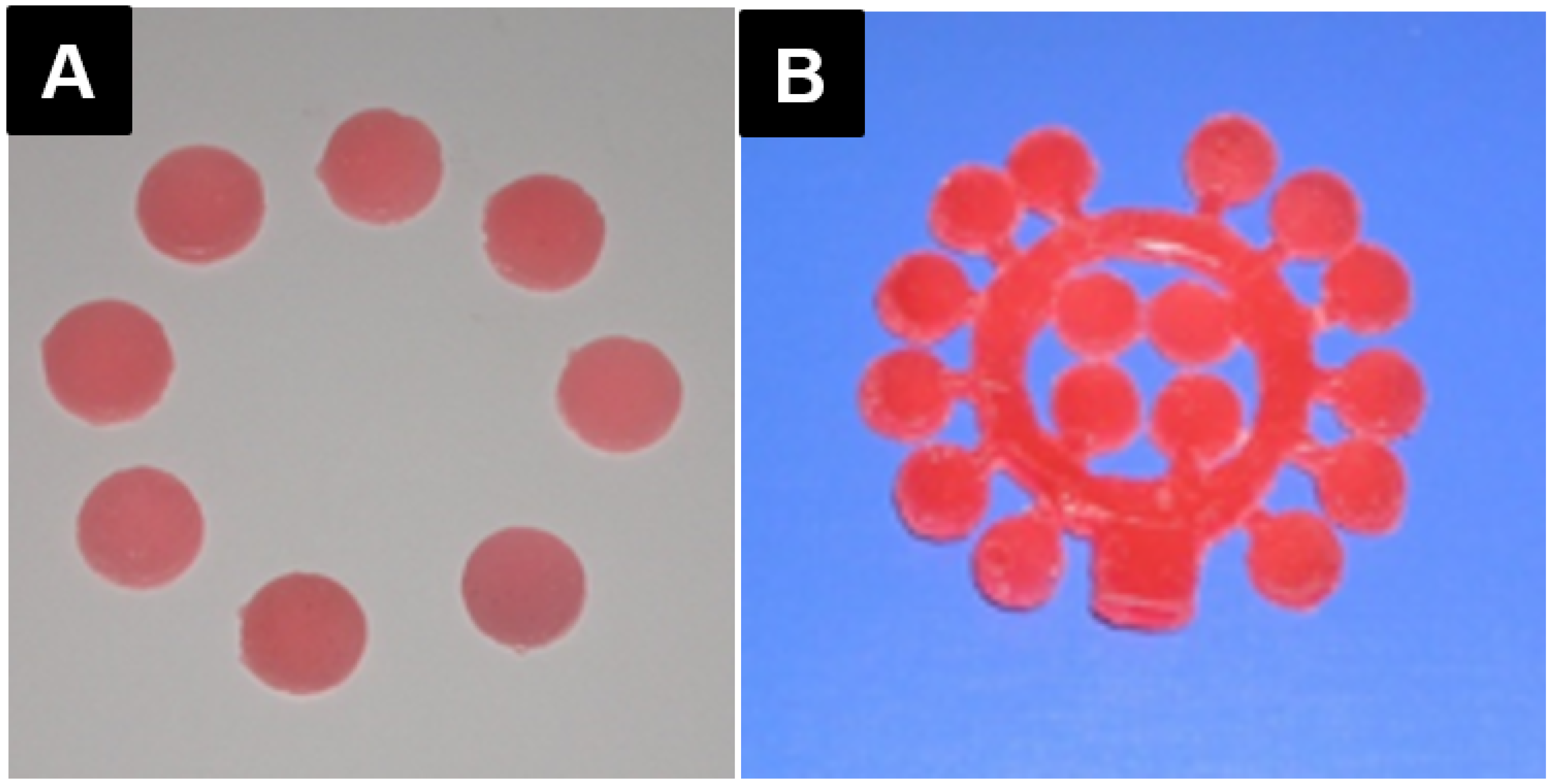
3.5. Flasking and Packing the Wax Discs
3.5.1. Conventional Technique (Factor B1)
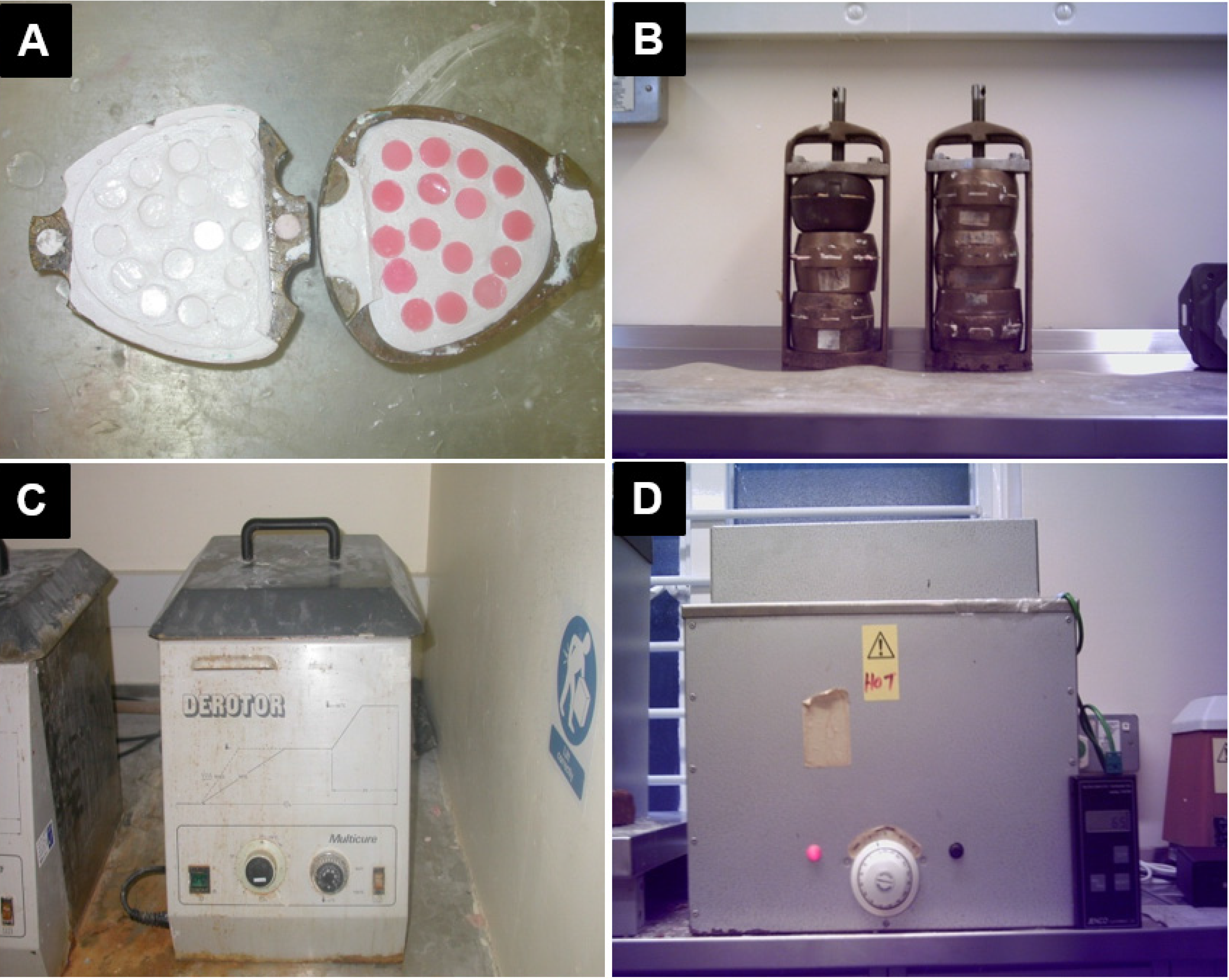
3.5.2. Injection Technique (Factor B2)
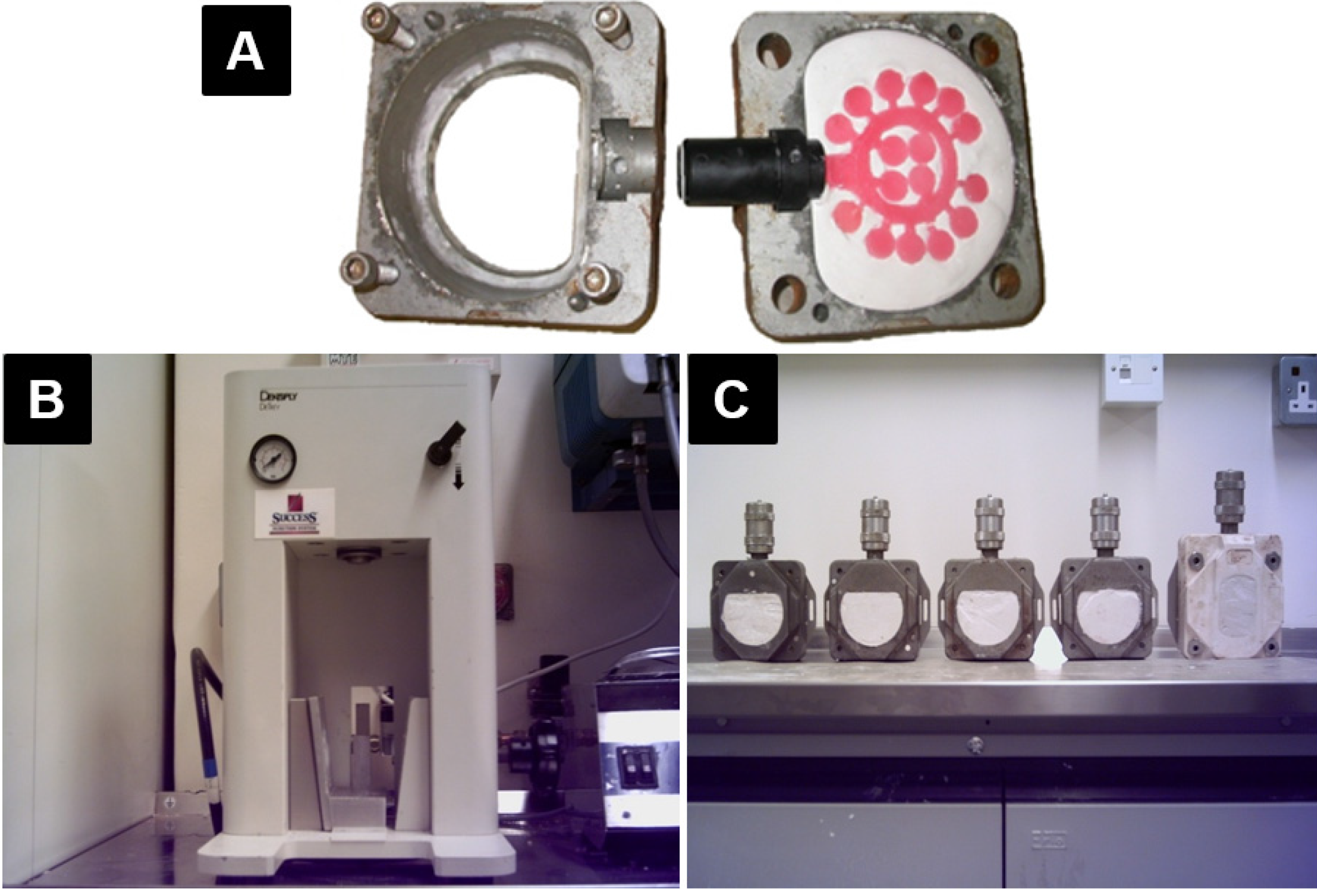
3.6. De-Flasking and Preparing the Discs
3.7. Modification of the Injection-Packing Technique

3.8. Evaluation of the Performance of the Processors

3.9. Biaxial Flexural Strength Testing
3.10. Data Analysis
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Jagger, D.C.; Harrison, A.; Jandt, K.D. The reinforcement of dentures. J. Oral Rehabil. 1999, 26, 185–194. [Google Scholar] [CrossRef] [PubMed]
- John, J.; Gangadhar, S.A.; Shah, I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J. Prosthet. Dent. 2001, 86, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Johnston, E.P.; Smith, D.E. Flexural fatigue of 10 commonly used denture base resins. J. Prosthet. Dent. 1981, 46, 478–480. [Google Scholar] [CrossRef] [PubMed]
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture—A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Alakuijala, P.; Lassila, V.P.; Lappalainen, V. In vitro fatigue fracture of an acrylic resin-based partial denture: An exploratory study. J. Prosthet. Dent. 1994, 72, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Lassila, V.P.; Lappalainen Niom, R. The effect of notch shape and self-cured acrylic resin repair on the fatigue resistance of an acrylic resin denture base. J. Oral Rehabil. 1996, 23, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Ganzarolli, S.M.; de Mello, J.A.; Shinkai, R.S.; del Bel Cury, A.A. Internal adaptation and some physical properties of methacrylate-based denture base resins polymerized by different techniques. J. Biomed. Mater. Res. Part B Appl. Biomater. 2007, 82, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Lamb, D.J.; Ellis, B.; van Noort, R. The fracture topography of acrylic dentures broken in service. Biomaterials 1985, 6, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Watts, D.C. The effect of reinforcement with woven E-glass fibers on the impact strength of complete dentures fabricated with high-impact acrylic resin. J. Prosthet. Dent. 2004, 91, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Nejatian, T.; Johnson, A.; van Noort, R. Reinforcement of denture base resin. Adv. Sci. Technol. 2006, 49, 124–129. [Google Scholar] [CrossRef]
- Hedzelek, W.; Gajdus, P. Comparison of mechanical strength of palatal denture bases made from various plastic materials. Int. J. Prosthodont. 2006, 19, 193–194. [Google Scholar] [PubMed]
- Stafford, G.D.; Huggett, R.; MacGregor, A.R.; Graham, J. The use of nylon as a denture-base material. J. Dent. 1986, 14, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Yunus, N.; Rashid, A.A.; Azmi, L.L.; Abu-Hassan, M.I. Some flexural properties of a nylon denture base polymer. J. Oral Rehabil. 2005, 32, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Radford, D.R.; Juszczyk, A.S.; Clark, R.K.F. The bond between acrylic resin denture teeth and the denture base: Recommendations for best practice. Br. Dent. J. 2014, 216, 165–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Praveen, B.; Babaji, H.V.; Prasanna, B.G.; Rajalbandi, S.K.; Shreeharsha, T.V.; Prashant, G.M. Comparison of Impact Strength and Fracture Morphology of Different Heat Cure Denture Acrylic Resins: An In vitro Study. J. Int. Oral Health 2014, 6, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Kanchanavasita, W.; Anstice, H.M.; Pearson, G.J. Long-term flexural strengths of resin-modified glass-ionomer cements. Biomaterials 1998, 19, 1703–1713. [Google Scholar] [CrossRef] [PubMed]
- Higgs, W.A.J.; Lucksanasombool, P.; Higgs, R.J.E.D.; Swain, M.V. Evaluating acrylic and glass-ionomer cement strength using the biaxial flexure test. Biomaterials 2001, 22, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Wagner, W.C.; Chu, T.M. Biaxial flexural strength and indentation fracture toughness of three new dental core ceramics. J. Prosthet. Dent. 1996, 76, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.Y.; Mueller, H.J.; Chai, J.; Wozniak, W.T. Comparative mechanical property characterization of 3 all-ceramic core materials. Int. J. Prosthodont. 1999, 12, 534–541. [Google Scholar] [PubMed]
- Yilmaz, H.; Aydin, C.; Gul, B.E. Flexural strength and fracture toughness of dental core ceramics. J. Prosthet. Dent. 2007, 98, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Pick, B.; Meira, J.B.C.; Driemeier, L.; Braga, R.R. A critical view on biaxial and short-beam uniaxial flexural strength tests applied to resin composites using Weibull, fractographic and finite element analyses. Dent. Mater. 2010, 26, 83–90. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, W.J. Dental Materials and Their Selection; Quintessence Pub. Co.: Chicago, IL, USA, 2002. [Google Scholar]
- Uzun, G.; Hersek, N. Comparison of the fracture resistance of six denture base acrylic resins. J. Biomater. Appl. 2002, 17, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Gharechahi, J.; Asadzadeh, N.; Shahabian, F.; Gharechahi, M. Flexural strength of acrylic resin denture bases processed by two different methods. J. Dent. Res. Dent. Clin. Dent. Prospect. 2014, 8, 148–152. [Google Scholar]
- Doǧan, A.; Bek, B.; Çevik, N.N.; Usanmaz, A. The effect of preparation conditions of acrylic denture base materials on the level of residual monomer, mechanical properties and water absorption. J. Dent. 1995, 23, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Honorez, P.; Catalan, A.; Angnes, U.; Grimonster, J. The effect of three processing cycles on some physical and chemical properties of a heat-cured acrylic resin. J. Prosthet. Dent. 1989, 61, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Wright, D.D.; Lautenschlager, E.P. The effect of processing temperature and time on the structure and fracture characteristics of self-reinforced composite poly(methyl methacrylate). J. Mater. Sci. Mater. Med. 1999, 10, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Hayhurst, L.; Johnson, A. The effect of resin type, packing and processing methods on the Biaxial Flexural strength of polymethyl methacrylate denture base materials. Quintessence J. Dent. Technol. 2004, 2, 414–420. [Google Scholar]
- Piddock, V.; Marquis, P.M.; Wilson, H.J. Comparison of the strengths of aluminous porcelain fired on to platinum and palladium foils. J. Oral Rehabil. 1986, 13, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Tan, F.; Qiao, X.L.; Chen, J.G.; Wang, H.S. Effects of coupling agents on the properties of epoxy-based electrically conductive adhesives. Int. J. Adhes. Adhes. 2005, 26, 406–413. [Google Scholar] [CrossRef]
- Li, A.G.; Kobayashi, A.S.; Bradt, R.C. Indentation fracture toughness of sintered silicon carbide in the palmqvist crack regime. J. Am. Ceram. Soc. 1989, 72, 904–911. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nejatian, T.; Sefat, F.; Johnson, T. Impact of Packing and Processing Technique on Mechanical Properties of Acrylic Denture Base Materials. Materials 2015, 8, 2093-2109. https://doi.org/10.3390/ma8052093
Nejatian T, Sefat F, Johnson T. Impact of Packing and Processing Technique on Mechanical Properties of Acrylic Denture Base Materials. Materials. 2015; 8(5):2093-2109. https://doi.org/10.3390/ma8052093
Chicago/Turabian StyleNejatian, Touraj, Farshid Sefat, and Tony Johnson. 2015. "Impact of Packing and Processing Technique on Mechanical Properties of Acrylic Denture Base Materials" Materials 8, no. 5: 2093-2109. https://doi.org/10.3390/ma8052093





