Evaluation of Dimensional Changes According to Aging Period and Postcuring Time of 3D-Printed Denture Base Prostheses: An In Vitro Study
Abstract
:1. Introduction
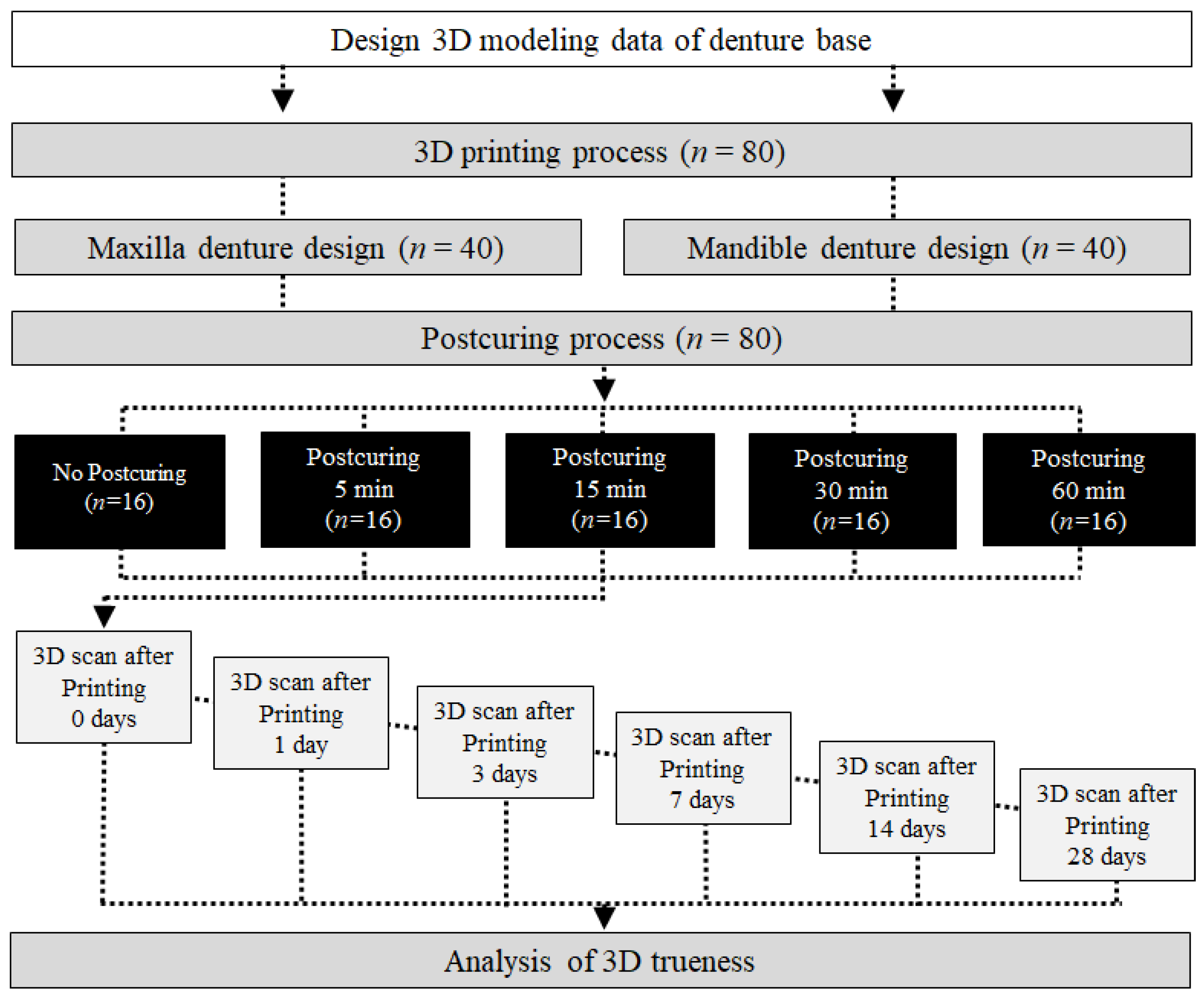
2. Materials and Methods
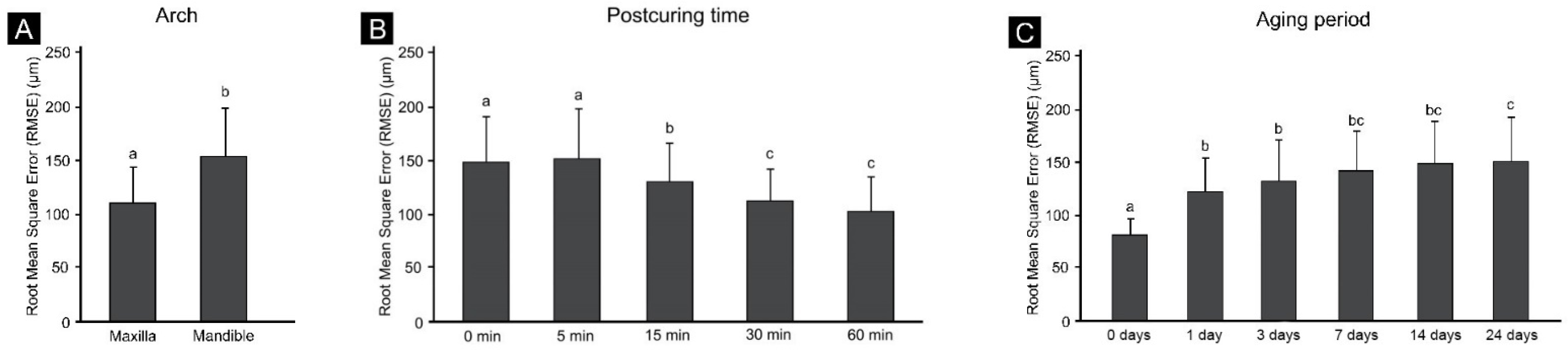
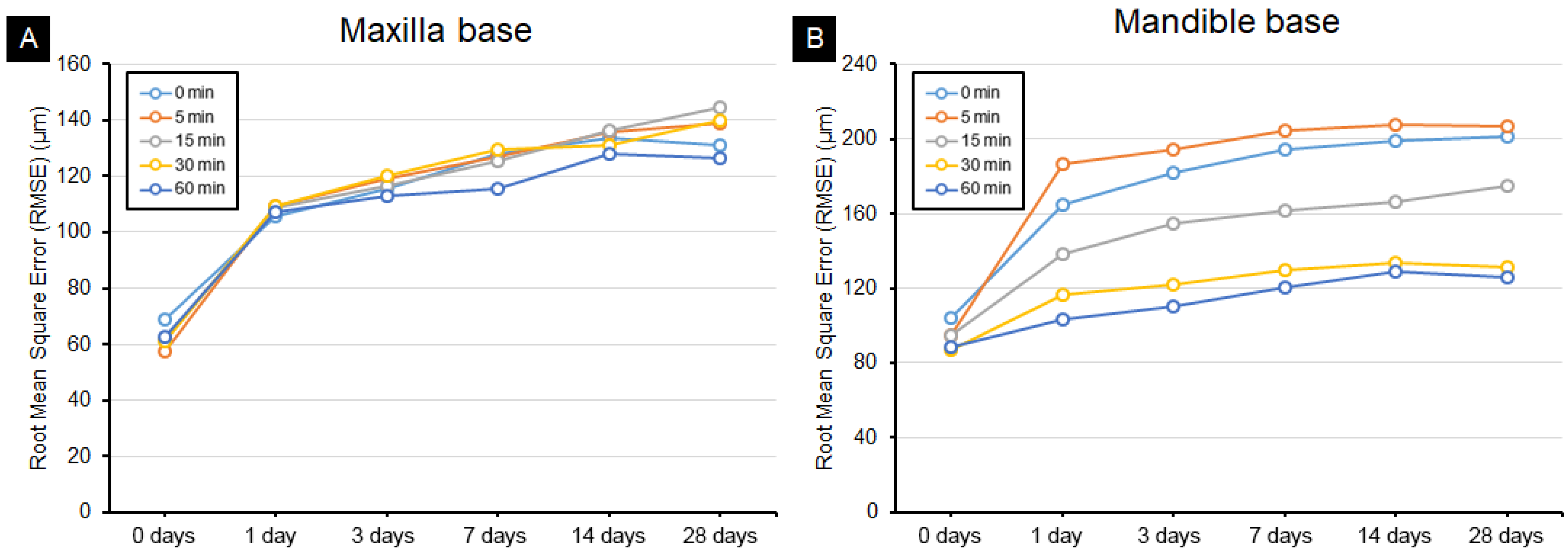
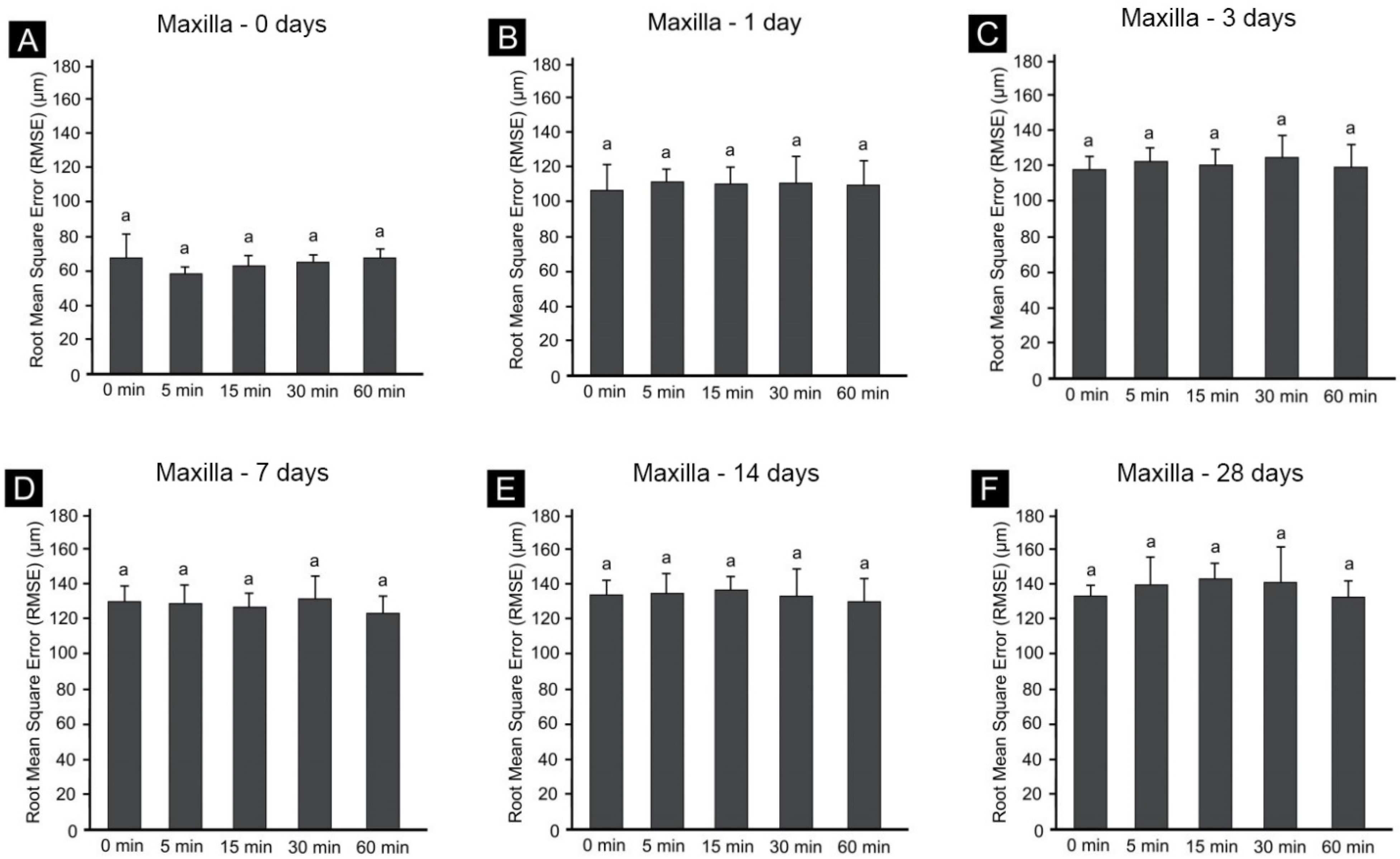
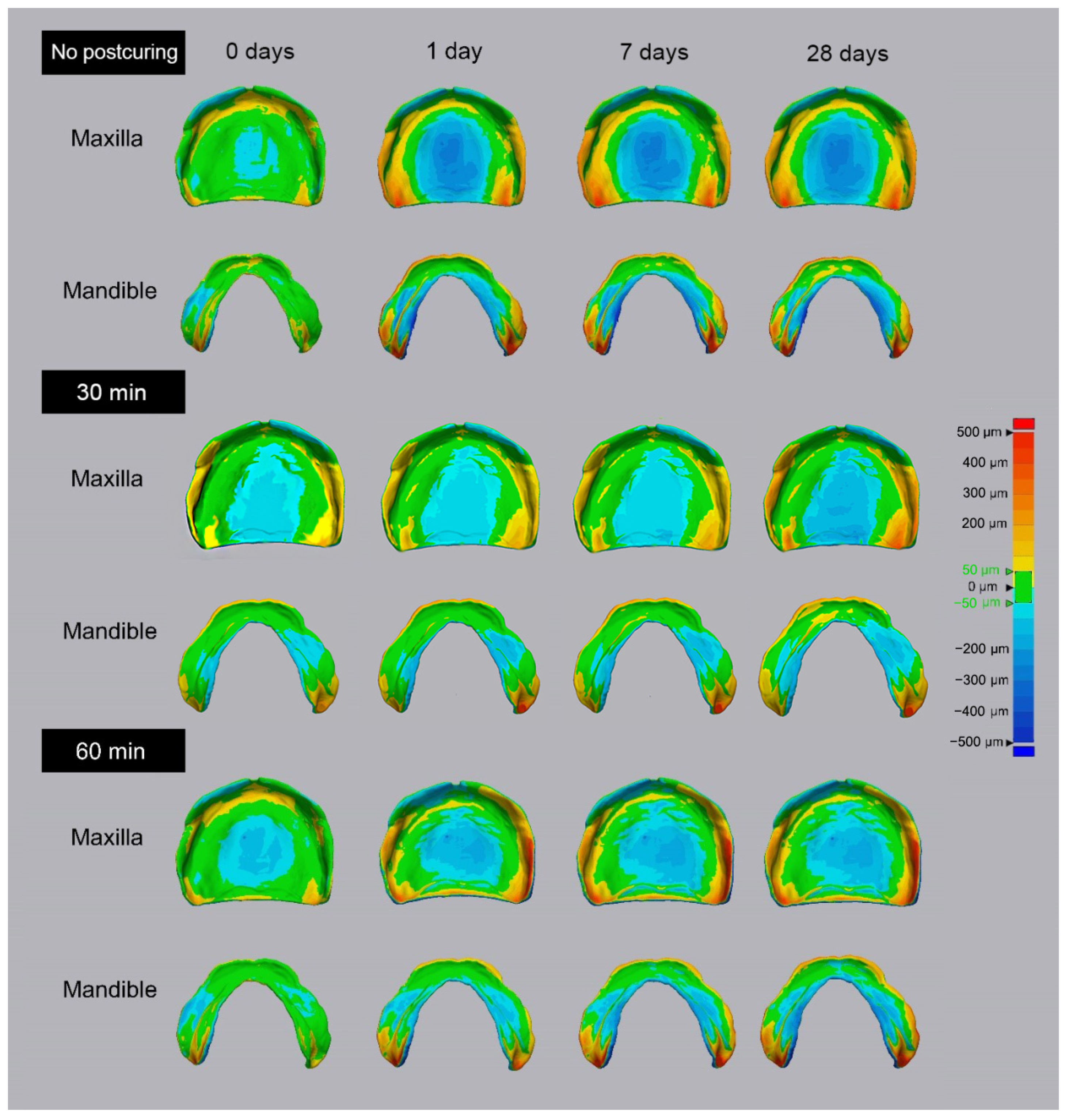
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Rekow, D.; Thompson, V.P. Near-surface damage—A persistent problem in crowns obtained by computer-aided design and manufacturing. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2005, 219, 233–243. [Google Scholar] [CrossRef]
- Attaran, M. The rise of 3-D printing: The advantages of additive manufacturing over traditional manufacturing. Bus. Horiz. 2017, 60, 677–688. [Google Scholar] [CrossRef]
- Jeong, I.-D.; Lee, J.-J.; Jeon, J.-H.; Kim, J.-H.; Kim, H.-Y.; Kim, W.-C. Accuracy of complete-arch model using an intraoral video scanner: An in vitro study. J. Prosthet. Dent. 2016, 115, 755–759. [Google Scholar] [CrossRef]
- Martorelli, M.; Gloria, A.; Bignardi, C.; Calì, M.; Maietta, S. Design of Additively Manufactured Lattice Structures for Biomedical Applications. J. Healthc. Eng. 2020, 2020, 2707560-3. [Google Scholar] [CrossRef]
- Quinn, G. On edge chipping testing and some personal perspectives on the state of the art of mechanical testing. Dent. Mater. 2014, 31, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Khaledi, A.-A.; Farzin, M.; Akhlaghian, M.; Pardis, S.; Mir, N. Evaluation of the marginal fit of metal copings fabricated by using 3 different CAD-CAM techniques: Milling, stereolithography, and 3D wax printer. J. Prosthet. Dent. 2019, 124, 81–86. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A. Current status and applications of additive manufacturing in dentistry: A literature-based review. J. Oral Biol. Craniofacial Res. 2019, 9, 179–185. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2015, 32, 54–64. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry—State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- McGuinness, N.J.; Stephens, C.D. Storage of Orthodontic Study Models in Hospital Units in the UK. Br. J. Orthod. 1992, 19, 227–232. [Google Scholar] [CrossRef]
- Zhang, Z.-C.; Li, P.-L.; Chu, F.-T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop. Fortschr. Der Kieferorthopädie 2019, 80, 194–204. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Park, M.-E.; Shin, S.-Y. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, 861.e1–861.e7. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Minakuchi, S. Effect of printing direction on stress distortion of three-dimensional printed dentures using stereolithography technology. J. Mech. Behav. Biomed. Mater. 2020, 110, 103949. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors Influencing the Dimensional Accuracy of 3D-Printed Full-Coverage Dental Restorations Using Stereolithography Technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [Green Version]
- Dikova, T.; Dzhendov, D.; Ivanov, D.; Bliznakova, K. Dimensional accuracy and surface roughness of polymeric dental bridges produced by different 3D printing processes. Arch. Mater. Sci. Eng. 2018, 2, 65–75. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.-B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef]
- Jin, M.-C.; Yoon, H.-I.; Yeo, I.-S.; Kim, S.-H.; Han, J.-S. The effect of build angle on the tissue surface adaptation of maxillary and mandibular complete denture bases manufactured by digital light processing. J. Prosthet. Dent. 2019, 123, 473–482. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build Angle: Does It Influence the Accuracy of 3D-Printed Dental Restorations Using Digital Light-Processing Technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Loflin, W.A.; English, J.D.; Borders, C.; Harris, L.M.; Moon, A.; Holland, J.N.; Kasper, F.K. Effect of print layer height on the assessment of 3D-printed models. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 283–289. [Google Scholar] [CrossRef] [Green Version]
- Jongsma, L.A.; Kleverlaan, C.J. Influence of temperature on volumetric shrinkage and contraction stress of dental composites. Dent. Mater. 2015, 31, 721–725. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Schmidt, F.; Beuer, F.; Li, P.; Spintzyk, S.; Fernandez, P.K. Stereolithography vs. Direct Light Processing for Rapid Manufacturing of Complete Denture Bases: An In Vitro Accuracy Analysis. J. Clin. Med. 2021, 10, 1070. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Shim, J.-S.; Lee, D.; Shin, S.-H.; Nam, N.-E.; Park, K.-H.; Shim, J.-S.; Kim, J.-E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Reymus, M.; Lumkemann, N.; Stawarczyk, B. 3D-printed material for temporary restorations: Impact of print layer thickness and post-curing method on degree of conversion. Int. J. Comput. Dent. 2019, 22, 231–237. [Google Scholar] [PubMed]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—an in vitro study. Clin. Oral Investig. 2019, 24, 701–710. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Bajaj, D.; Siena, F.L.; Breedon, P. Effects of post-curing conditions on mechanical properties of 3D printed clear dental aligners. Rapid Prototyp. J. 2020, 26, 1337–1344. [Google Scholar] [CrossRef]
- Joda, T.; Matthisson, L.; Zitzmann, N.U. Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation. J. Clin. Med. 2020, 9, 1436. [Google Scholar] [CrossRef]
- Ozsoy, U. Comparison of Different Calculation Methods Used to Analyze Facial Soft Tissue Asymmetry: Global and Partial 3-Dimensional Quantitative Evaluation of Healthy Subjects. J. Oral Maxillofac. Surg. 2016, 74, 1847.e1–1847.e9. [Google Scholar] [CrossRef]
- Etemad-Shahidi, Y.; Qallandar, O.B.; Evenden, J.; Alifui-Segbaya, F.; Ahmed, K.E. Accuracy of 3-Dimensionally Printed Full-Arch Dental Models: A Systematic Review. J. Clin. Med. 2020, 9, 3357. [Google Scholar] [CrossRef]
- Ko, J.; Bloomstein, R.D.; Briss, D.; Holland, J.N.; Morsy, H.M.; Kasper, F.K.; Huang, W. Effect of build angle and layer height on the accuracy of 3-dimensional printed dental models. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 451–458.e2. [Google Scholar] [CrossRef]
- Hwang, H.-J.; Lee, S.J.; Park, E.-J.; Yoon, H.-I. Assessment of the trueness and tissue surface adaptation of CAD-CAM maxillary denture bases manufactured using digital light processing. J. Prosthet. Dent. 2018, 121, 110–117. [Google Scholar] [CrossRef]
- Yoon, H.-I.; Hwang, H.-J.; Ohkubo, C.; Han, J.-S.; Park, E.-J. Evaluation of the trueness and tissue surface adaptation of CAD-CAM mandibular denture bases manufactured using digital light processing. J. Prosthet. Dent. 2018, 120, 919–926. [Google Scholar] [CrossRef]
- Akaltan, F.; Batak, B.; Oguz, E.I.; Orhan, K. Comparative analysis of denture base adaptation performance between pour and other conventional fabrication techniques. J. Prosthet. Dent. 2019, 123, 183.e1–183.e5. [Google Scholar] [CrossRef] [Green Version]
- Kenning, K.B.; Risinger, D.C.; English, J.D.; Cozad, B.E.; Harris, L.M.; Ontiveros, J.C.; Kasper, F.K. Evaluation of the dimensional accuracy of thermoformed appliances taken from 3D printed models with varied shell thicknesses: An in vitro study. Int. Orthod. 2021, 19, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Cui, K.; Shang, X.; Luo, C.; Shen, Z.; Gao, H.; Xiong, G. A Kind of Accuracy Improving Method Based on Error Analysis and Feedback for DLP 3D Printing. In Proceedings of the 2019 IEEE International Conference on Service Operations and Logistics, and Informatics (SOLI), Zhengzhou, China, 6–8 November 2019; pp. 5–9. [Google Scholar] [CrossRef]
- Barker, T.M.; Earwaker, W.J.S.; Lisle, D.A. Accuracy of stereolithographic models of human anatomy. Australas. Radiol. 1994, 38, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.-H.; Lim, J.-H.; Kang, Y.-J.; Kim, J.-H.; Shim, J.-S.; Kim, J.-E. Evaluation of the 3D Printing Accuracy of a Dental Model According to its Internal Structure and Cross-Arch Plate Design: An In Vitro Study. Materials 2020, 13, 5433. [Google Scholar] [CrossRef] [PubMed]
- Fuh, J.Y.H.; Lu, L.; Tan, C.C.; Shen, Z.X.; Chew, S. Processing and characterising photo-sensitive polymer in the rapid prototyping process. J. Mater. Process. Tech. 1999, 90, 211–217. [Google Scholar] [CrossRef]
- Choi, J.-Y.; Choi, J.-H.; Kim, N.-K.; Kim, Y.; Lee, J.-K.; Kim, M.-K.; Lee, J.-H.; Kim, M.-J. Analysis of errors in medical rapid prototyping models. Int. J. Oral Maxillofac. Surg. 2002, 31, 23–32. [Google Scholar] [CrossRef]
- Camardella, L.T.; Vilella, O.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef] [Green Version]
- Hazeveld, A.; Slater, J.J.H.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef]
- Karalekas, D.; Aggelopoulos, A. Study of shrinkage strains in a stereolithography cured acrylic photopolymer resin. J. Mater. Process. Technol. 2003, 136, 146–150. [Google Scholar] [CrossRef]
- Mccarty, M.C.; Chen, S.J.; English, J.D.; Kasper, F. Effect of print orientation and duration of ultraviolet curing on the dimensional accuracy of a 3-dimensionally printed orthodontic clear aligner design. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.M.; Cheng, L.Y.; Chow, T.; Clark, R.K. Effect of processing method on the dimensional accuracy and water sorption of acrylic resin dentures. J. Prosthet. Dent. 1999, 81, 300–304. [Google Scholar] [CrossRef]
- Li, P.; Krämer-Fernandez, P.; Klink, A.; Xu, Y.; Spintzyk, S. Repairability of a 3D printed denture base polymer: Effects of surface treatment and artificial aging on the shear bond strength. J. Mech. Behav. Biomed. Mater. 2020, 114, 104227. [Google Scholar] [CrossRef] [PubMed]

| Components | Amount |
|---|---|
| ethoxylated bisphenol A dimethacrylate | 88–98% |
| 2,4,6-Trimethylbenzoyl-diphenyl-diphenyl Phosphine oxide | 2–5% |
| Printing Technology | LCD Type |
|---|---|
| Build volume | 120 mm × 68 mm × 200 mm |
| Z-layer resolution | 10 microns |
| XY resolution | 47 microns |
| Light source | 405-nm parallel aligned LED |
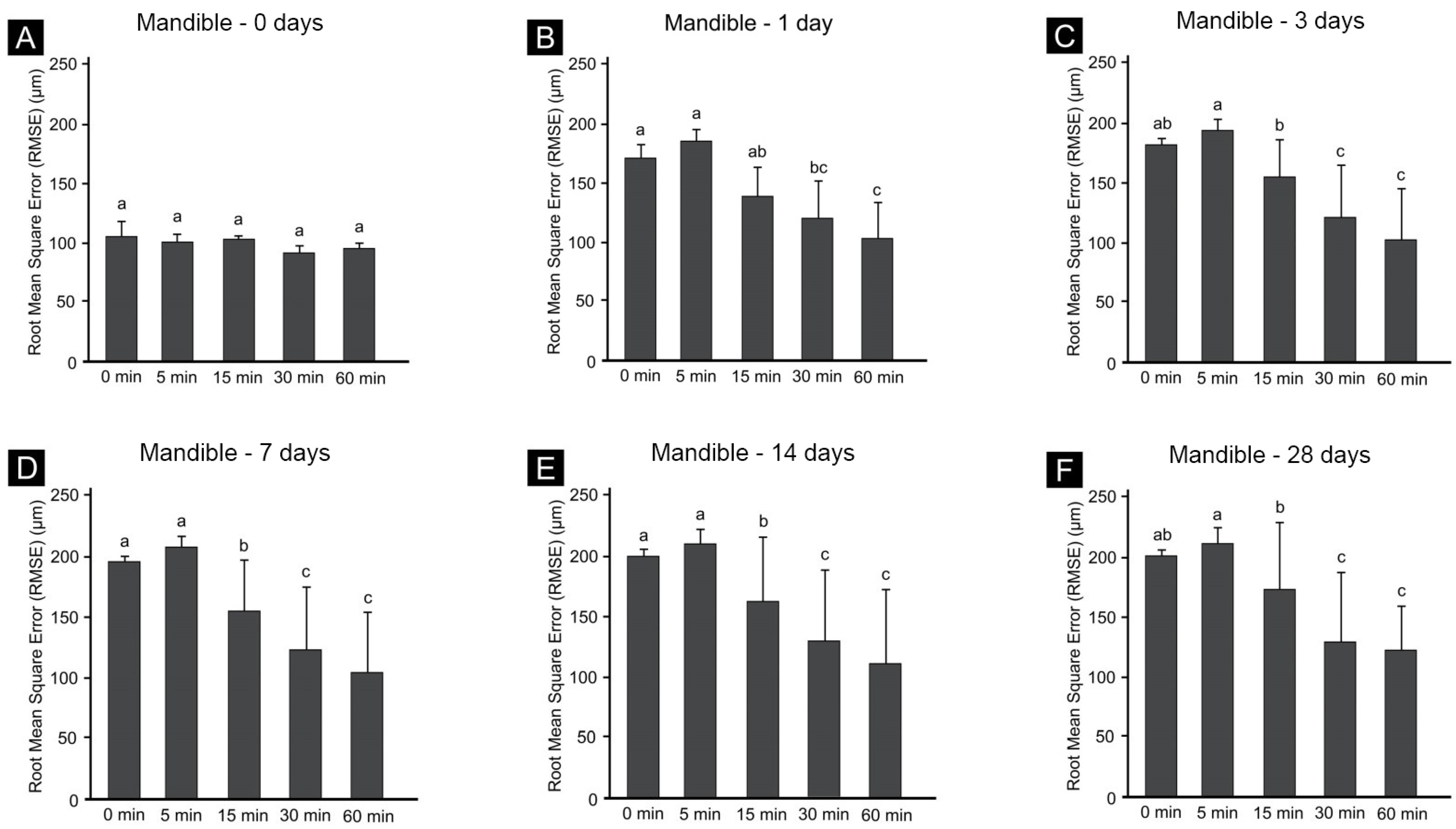
| Minute | 0 Days | 1 Day | 3 Days | 7 Days | 14 Days | 28 Days | |
|---|---|---|---|---|---|---|---|
| Maxilla | 0 | 69.1 ± 13.3 | 105.5 ± 9.4 | 115.7 ± 3.4 | 127.8 ± 5.2 | 133.6 ± 4.9 | 131.2 ± 5.3 |
| 5 | 57.7 ± 8.8 | 109.5 ± 8.9 | 119 ± 9.0 | 126.9 ± 9.9 | 135.6 ± 12.1 | 138.8 ± 12.6 | |
| 15 | 61.4 ± 3.7 | 108.8 ± 21.8 | 116.8 ± 31.2 | 125.2 ± 35.8 | 136.5 ± 44.6 | 144.7 ± 46.9 | |
| 30 | 61 ± 4.3 | 109.5 ± 35.1 | 120.2 ± 40.4 | 129.5 ± 46.7 | 130.9 ± 52.31 | 140.1 ± 54.1 | |
| 60 | 62.7 ± 8.0 | 107.5 ± 28.3 | 112.9 ± 34.4 | 115.7 ± 35.8 | 127.8 ± 40.3 | 126.6 ± 39.2 | |
| Mandible | 0 | 104.2 ± 11.5 | 164.8 ± 14.9 | 182 ± 8.9 | 194.1 ± 10.7 | 199.3 ± 7.8 | 201.1 ± 5.5 |
| 5 | 95.1 ± 3.0 | 186.2 ± 7.7 | 194 ± 9.3 | 204.3 ± 13.0 | 207.5 ± 12.8 | 206.6 ± 15.0 | |
| 15 | 95 ± 5.7 | 138.2 ± 10.2 | 155 ± 10.45 | 161.9 ± 8.8 | 166.7 ± 6.9 | 174.7 ± 7.0 | |
| 30 | 87.2 ± 6.12 | 116.6 ± 15.0 | 122.2 ± 17.6 | 129.4 ± 19.5 | 134 ± 18.9 | 131.5 ± 21.0 | |
| 60 | 88.5 ± 10.1 | 103.4 ± 13.6 | 110 ± 14.5 | 120.8 ± 15.4 | 129.3 ± 14.4 | 125.7 ± 13.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.-H.; Doh, R.-M.; Lim, J.-H.; Kwon, J.-S.; Shim, J.-S.; Kim, J.-E. Evaluation of Dimensional Changes According to Aging Period and Postcuring Time of 3D-Printed Denture Base Prostheses: An In Vitro Study. Materials 2021, 14, 6185. https://doi.org/10.3390/ma14206185
Shin S-H, Doh R-M, Lim J-H, Kwon J-S, Shim J-S, Kim J-E. Evaluation of Dimensional Changes According to Aging Period and Postcuring Time of 3D-Printed Denture Base Prostheses: An In Vitro Study. Materials. 2021; 14(20):6185. https://doi.org/10.3390/ma14206185
Chicago/Turabian StyleShin, Seung-Ho, Re-Mee Doh, Jung-Hwa Lim, Jae-Sung Kwon, June-Sung Shim, and Jong-Eun Kim. 2021. "Evaluation of Dimensional Changes According to Aging Period and Postcuring Time of 3D-Printed Denture Base Prostheses: An In Vitro Study" Materials 14, no. 20: 6185. https://doi.org/10.3390/ma14206185







