Load-Bearing Capacity of Zirconia Crowns Screwed to Multi-Unit Abutments with and without a Titanium Base: An In Vitro Pilot Study
Abstract
:1. Introduction
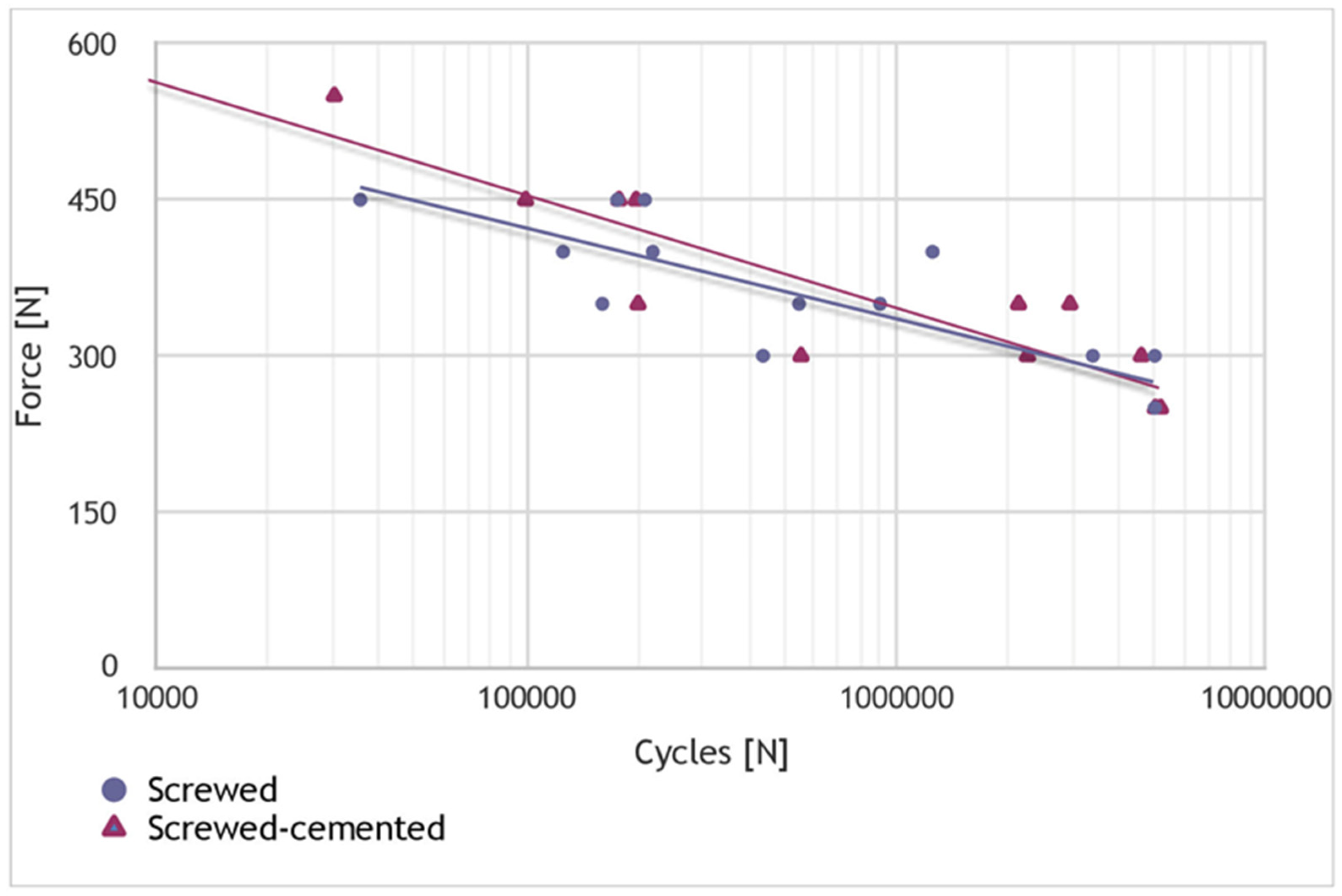
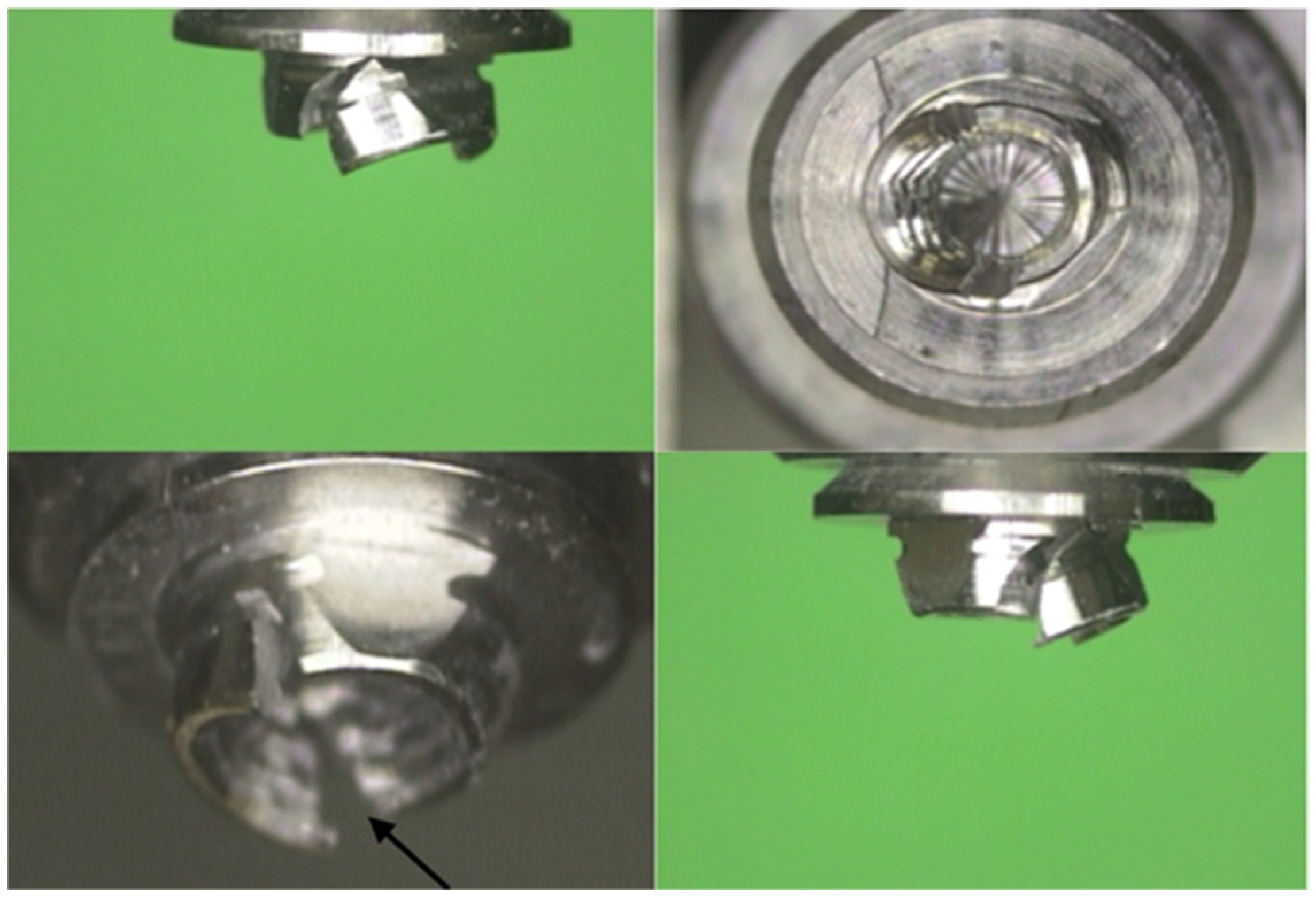
2. Results
3. Discussion
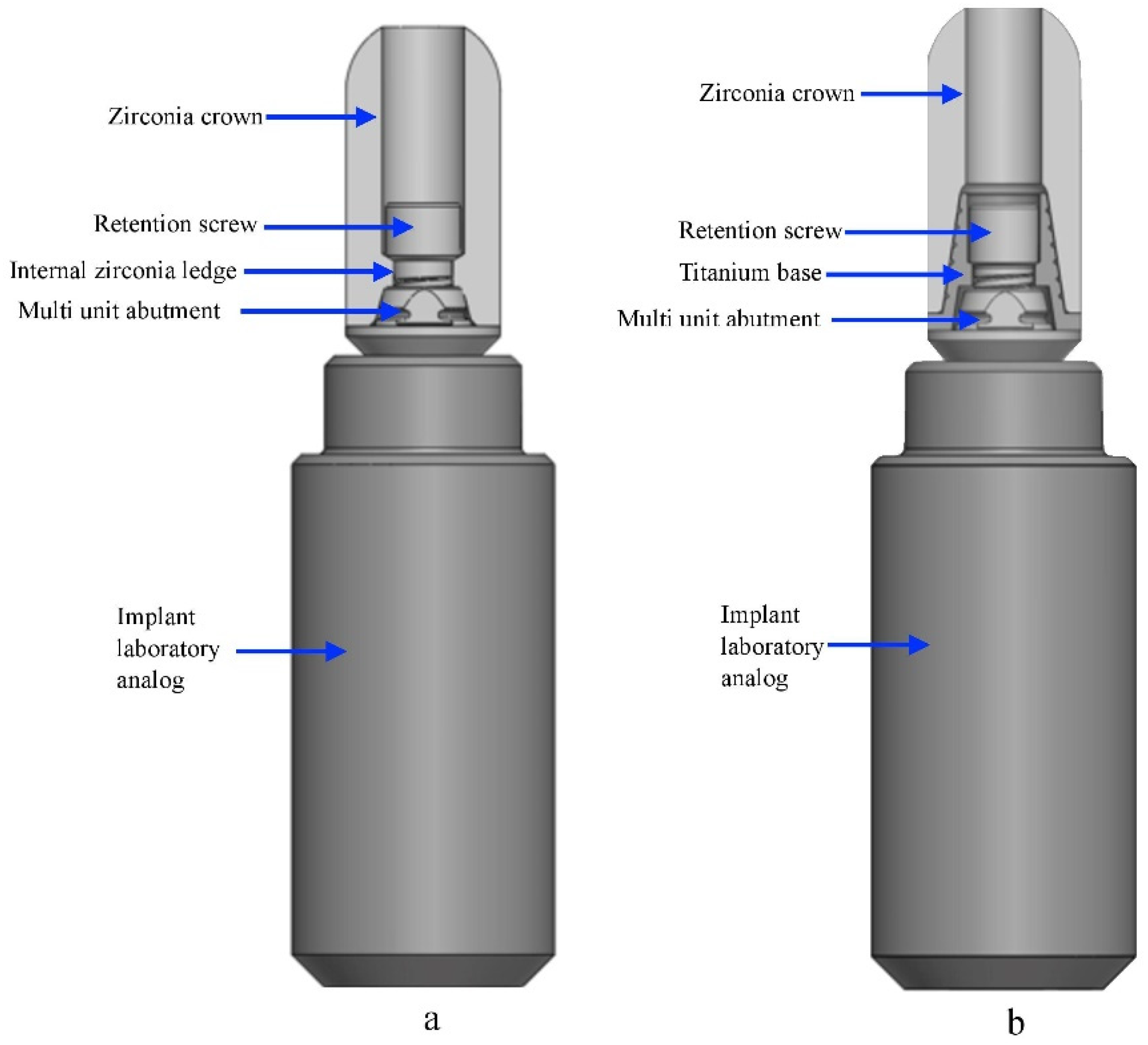
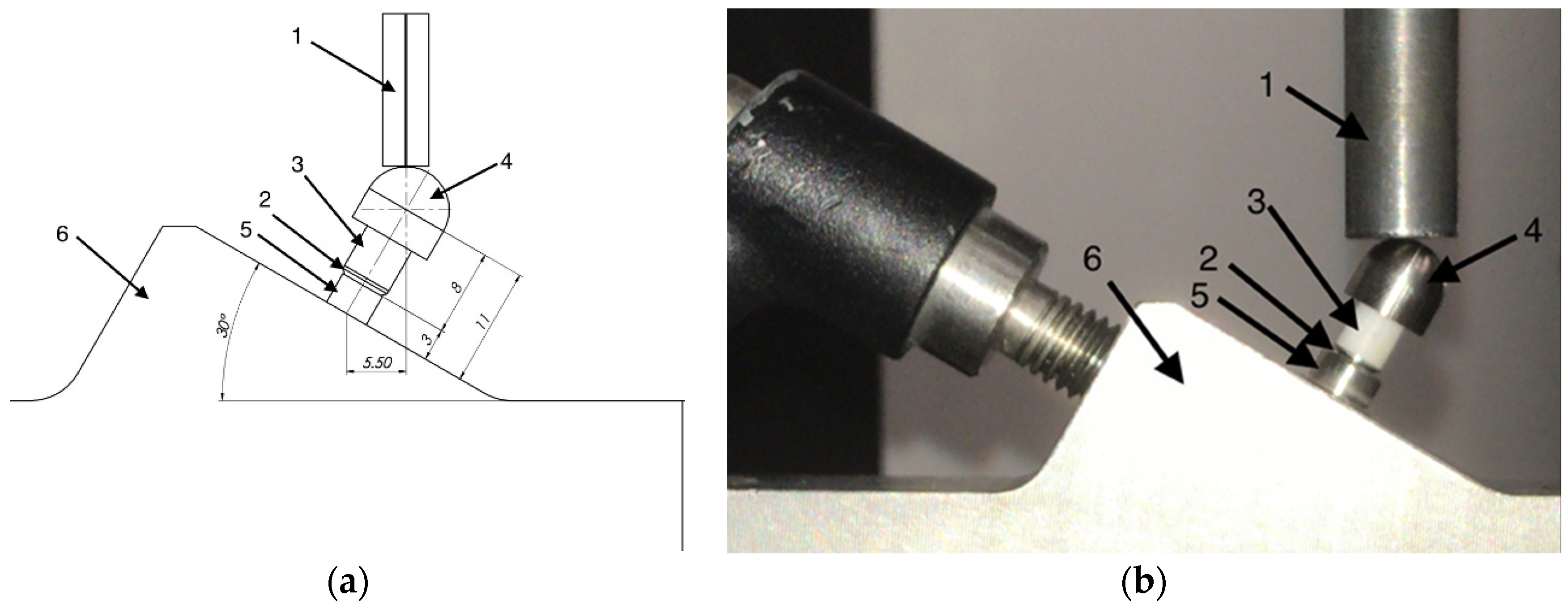
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guncu, M.B.; Cakan, U.; Muhtarogullari, M.; Canay, S. Zirconia-based crowns up to 5 years in function: A retrospective clinical study and evaluation of prosthetic restorations and failures. Int. J. Prosthodont. 2015, 28, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Stimmelmayr, M.; Gueth, J.F.; Edelhoff, D.; Naumann, M. In vitro performance of full-contour zirconia single crowns. Dent. Mater. 2012, 28, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Guess, P.C.; Att, W.; Strub, J.R. Zirconia in fixed implant prosthodontics. Clin. Implant Dent. Relat. Res. 2012, 14, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Michalakis, K.X.; Hirayama, H.; Garefis, P.D. Cement-retained versus screw-retained implant restorations: A critical review. Int. J. Oral Maxillofac. Implant. 2003, 18, 719–728. [Google Scholar]
- Wilson, T.G., Jr. The positive relationship between excess cement and peri-implant disease: A prospective clinical endoscopic study. J. Periodontol. 2009, 80, 1388–1392. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Muhlemann, S.; Zwahlen, M.; Hammerle, C.H.; Schneider, D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin Oral Implants Res 2012, 23, 163–201. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Puisys, A.; Vindasiute, E.; Linkeviciene, L.; Apse, P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin. Oral Implant. Res. 2013, 24, 1179–1184. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Millen, C.; Bragger, U. Clinical performance of screw-versus cement-retained fixed implant-supported reconstructions-A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29 (Suppl. 2014), 84–98. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S. An esthetic titanium abutment: Report of a technique. Int. J. Oral Maxillofac. Implant. 1991, 6, 195–201. [Google Scholar]
- Canullo, L.; Bignozzi, I.; Cocchetto, R.; Cristalli, M.P.; Iannello, G. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-Year follow-up of a randomised multicentre clinical trial. Eur. J. Oral Implant. 2010, 3, 285–296. [Google Scholar]
- Degidi, M.; Nardi, D.; Piattelli, A. One abutment at one time: Non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants. Clin. Oral Implant. Res. 2011, 22, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- Grandi, T.; Guazzi, P.; Samarani, R.; Garuti, G. Immediate positioning of definitive abutments versus repeated abutment replacements in immediately loaded implants: Effects on bone healing at the 1-year follow-up of a multicentre randomised controlled trial. Eur. J. Oral Implant. 2012, 5, 9–16. [Google Scholar]
- McGlumphy, E.A.; Papazoglou, E.; Riley, R.L. The combination implant crown: A cement- and screw-retained restoration. Compendium 1992, 13, 34–41. [Google Scholar] [PubMed]
- Rajan, M.; Gunaseelan, R. Fabrication of a cement- and screw-retained implant prosthesis. J. Prosthet. Dent. 2004, 92, 578–580. [Google Scholar] [CrossRef] [PubMed]
- Uludag, B.; Celik, G. Fabrication of a cement- and screw-retained multiunit implant restoration. J. Oral Implant. 2006, 32, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Hussien, A.N.; Rayyan, M.M.; Sayed, N.M.; Segaan, L.G.; Goodacre, C.J.; Kattadiyil, M.T. Effect of screw-access channels on the fracture resistance of 3 types of ceramic implant-supported crowns. J. Prosthet. Dent. 2016, 116, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.R.; Teixeira, H.S.; Silveira, L.M.; Bonfante, E.A.; Coelho, P.G.; Thompson, V.P. Reliability and failure modes of a hybrid ceramic abutment prototype. J. Prosthodont. 2018, 27, 83–87. [Google Scholar] [CrossRef]
- Linkevicius, T.; Caplikas, A.; Dumbryte, I.; Linkeviciene, L.; Svediene, O. Retention of zirconia copings over smooth and airborne-particle-abraded titanium bases with different resin cements. J. Prosthet. Dent. 2019, 121, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Röhrle, O.; Saini, H.; Ackland, D.C. Occlusal loading during biting from an experimental and simulation point of view. Dent. Mater. 2018, 34, 58–68. [Google Scholar] [CrossRef]
- Umesh, S.; Padma, S.; Asokan, S.; Srinivas, T. Fiber Bragg Grating based bite force measurement. J. Biomech. 2016, 49, 2877–2881. [Google Scholar] [CrossRef]
- Fernandes, C.P.; Glantz, P.O.; Svensson, S.A.; Bergmark, A. A novel sensor for bite force determinations. Dent Mater. 2003, 19, 118–126. [Google Scholar] [CrossRef]
- Kwon, S.J.; Lawson, N.C.; McLaren, E.E.; Nejat, A.H.; Burgess, J.O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent. 2018, 120, 132–137. [Google Scholar] [CrossRef] [PubMed]
- ISO. International Organization for Standardization Endosseous Dental Implants: Dentistry Implants-Dynamic Fatigue Test, ISO 14801; ISO: Geneva, Switzerland, 2016. [Google Scholar]
- Koyama, T.; Sato, T.; Yoshinari, M. Cyclic fatigue resistance of yttria-stabilized tetragonal zirconia polycrystals with hot isostatic press processing. Dent. Mater. J. 2012, 31, 1103–1110. [Google Scholar] [CrossRef] [PubMed]
- Ding, Q.; Zhang, L.; Bao, R.; Zheng, G.; Sun, Y.; Xie, Q. Effects of different surface treatments on the cyclic fatigue strength of one-piece CAD/CAM zirconia implants. J. Mech. Behav. Biomed. Mater. 2018, 84, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Gonzalez, J.A.; Kulkarni, P.A.; Nagy, W.W.; Griggs, J.A. Fatigue lifetime prediction of a reduced-diameter dental implant system: Numerical and experimental study. Dent. Mater. 2018, 34, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Shemtov-Yona, K.; Rittel, D. Random spectrum loading of dental implants: An alternative approach to functional performance assessment. J. Mech. Behav. Biomed. Mater. 2016, 62, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Naumova, E.A.; Roth, F.; Geis, B.; Baulig, C.; Arnold, W.H.; Piwowarczyk, A. Influence of luting materials on the retention of cemented implant-supported crowns: An in vitro study. Materials (Basel) 2018, 11, 1853. [Google Scholar] [CrossRef]
- Gungor, M.B.; Nemli, S.K. The effect of resin cement type and thermomechanical aging on the retentive strength of custom zirconia abutments bonded to titanium inserts. Int. J. Oral Maxillofac. Implant. 2018, 33, 523–529. [Google Scholar] [CrossRef]
- Zenthofer, A.; Rues, S.; Krisam, J.; Rustemeyer, R.; Rammelsberg, P.; Schmitter, M. Debonding forces for two-piece zirconia abutments with implant platforms of different diameter and use of different luting strategies. Int. J. Oral Maxillofac. Implant. 2018, 33, 1041–1046. [Google Scholar] [CrossRef]
- Chun, H.J.; Yeo, I.S.; Lee, J.H.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Han, J.S.; Lee, S.J. Fracture strength study of internally connected zirconia abutments reinforced with titanium inserts. Int. J. Oral Maxillofac. Implant. 2015, 30, 346–350. [Google Scholar] [CrossRef]
- Kelly, J.R.; Rungruanganunt, P. Fatigue behavior of computer-aided design/computer-assisted manufacture ceramic abutments as a function of design and ceramics processing. Int. J. Oral Maxillofac. Implant. 2016, 31, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, B.; Salaita, L.G.; Seidt, J.D.; McGlumphy, E.A.; Clelland, N.L. Load to failure of different zirconia abutments for an internal hexagon implant. J. Prosthet. Dent. 2015, 114, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, P.; Alius, J.; Fischer, C.; Erdelt, K.J.; Beuer, F. Retentive strength of two-piece CAD/CAM zirconia implant abutments. Clin. Implant Dent. Relat. Res. 2014, 16, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Agar-Zoizner, S.; Gelbard, S.; Levartovsky, S. The retentive strength of laser-sintered cobalt- chromium-based crowns after pretreatment with a desensitizing paste containing 8% arginine and calcium carbonate. Int. J. Mol. Sci. 2018, 19, 4082. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Folkman, M.; Arieli, A.; Levartovsky, S. Marginal fit and retention strength of zirconia crowns cemented by self-adhesive resin cements. Oper. Dent. 2018, 43, 151–161. [Google Scholar] [CrossRef]
- Garoushi, S.; Lassila, L.V.; Tezvergil, A.; Vallittu, P.K. Static and fatigue compression test for particulate filler composite resin with fiber-reinforced composite substructure. Dent. Mater. 2007, 23, 17–23. [Google Scholar] [CrossRef]
- Ongthiemsak, C.; Mekayarajjananonth, T.; Winkler, S.; Boberick, K.G. The effect of compressive cyclic loading on retention of a temporary cement used with implants. J. Oral Implant. 2005, 31, 115–120. [Google Scholar] [CrossRef]



| Specimen | Group A(N) | Group B(N) |
|---|---|---|
| 1 | 872 | 718 |
| 2 | 811 | 680 |
| 3 | 675 | 707 |
| Mean | 786 | 702 |
| 80% Level | 629 | 561 |
| Specimen | Load (N) | No. of Cycles | Average No of Cycles | Failure Mode |
|---|---|---|---|---|
| 1 | 450 | 35,670 | - | Zirconia + metal (screw) |
| 2 | 450 | 209,543 | 80,545 | Metal (MUA + screw) Zirconia + metal (screw) |
| 3 | 450 | 176,422 | - | |
| 4 | 400 | 1,254,436 | - | Metal (MUA + screw) |
| 5 | 400 | 125,878 | 533,457 | Metal (MUA + screw) |
| 6 | 400 | 220,056 | - | Metal (MUA + screw) |
| 7 | 350 | 160,749 | - | Metal (MUA + screw) |
| 8 | 350 | 546,871 | 266,048 | Metal (MUA + screw) |
| 9 | 350 | 905,205 | - | Metal (MUA + screw) |
| 10 | 300 | 3,401,784 | - | Metal (MUA + screw) |
| 11 | 300 | 437,068 | 2,946,284 | Metal (MUA + screw) |
| 12 | 300 | 5,000,000 | - | Metal (MUA + screw) |
| 13 | 250 | 5,000,000 | - | No Failure |
| 14 | 250 | 5,000,000 | 5,000,000 | No Failure |
| 15 | 250 | 5,000,000 | - | No Failure |
| Specimen | Load (N) | No. of Cycles | Average No of Cycles | Failure Mode |
|---|---|---|---|---|
| 1 | 550 | 6607 | - | Adhesive + metal (screw) |
| 2 | 550 | 30,341 | 22,450 | Metal (screw) Adhesive + metal (screw) |
| 3 | 550 | 30,341 | - | |
| 4 | 450 | 99,751 | - | Adhesive + metal (MUA) |
| 5 | 450 | 178,367 | 158,818 | Metal (screw) |
| 6 | 450 | 198,337 | - | Adhesive + metal (MUA) |
| 7 | 350 | 2,950,685 | - | Adhesive + metal (screw) |
| 8 | 350 | 200,751 | 1,764,689 | Adhesive + metal (MUA) |
| 9 | 350 | 2,142,632 | - | Adhesive + metal (MUA) |
| 10 | 300 | 553,418 | - | Adhesive + metal (MUA) |
| 11 | 300 | 2,264,147 | 2,472,765 | Metal (screw) |
| 12 | 300 | 4,600,732 | - | Adhesive + metal (MUA |
| 13 | 250 | 5,000,000 | - | No Failure |
| 14 | 250 | 5,000,000 | 5,000,000 | No Failure |
| 15 | 250 | 5,000,000 | - | No Failure |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heller, H.; Arieli, A.; Beitlitum, I.; Pilo, R.; Levartovsky, S. Load-Bearing Capacity of Zirconia Crowns Screwed to Multi-Unit Abutments with and without a Titanium Base: An In Vitro Pilot Study. Materials 2019, 12, 3056. https://doi.org/10.3390/ma12193056
Heller H, Arieli A, Beitlitum I, Pilo R, Levartovsky S. Load-Bearing Capacity of Zirconia Crowns Screwed to Multi-Unit Abutments with and without a Titanium Base: An In Vitro Pilot Study. Materials. 2019; 12(19):3056. https://doi.org/10.3390/ma12193056
Chicago/Turabian StyleHeller, Hadas, Adi Arieli, Ilan Beitlitum, Raphael Pilo, and Shifra Levartovsky. 2019. "Load-Bearing Capacity of Zirconia Crowns Screwed to Multi-Unit Abutments with and without a Titanium Base: An In Vitro Pilot Study" Materials 12, no. 19: 3056. https://doi.org/10.3390/ma12193056





