The Role of Health Kiosks in 2009: Literature and Informant Review
Abstract
:1. Introduction
2. Methods and Data Sources
3. Results and Discussion
3.1. Opportunistic Versus Integrated into Clinical Process
3.2. Opportunistic Kiosks
Consumer health information, health education and promotion:
Early kiosk use:
NHS kiosk:
Recent uses in health education:
Patient access to records:
3.3. Kiosks Built into Clinical Process
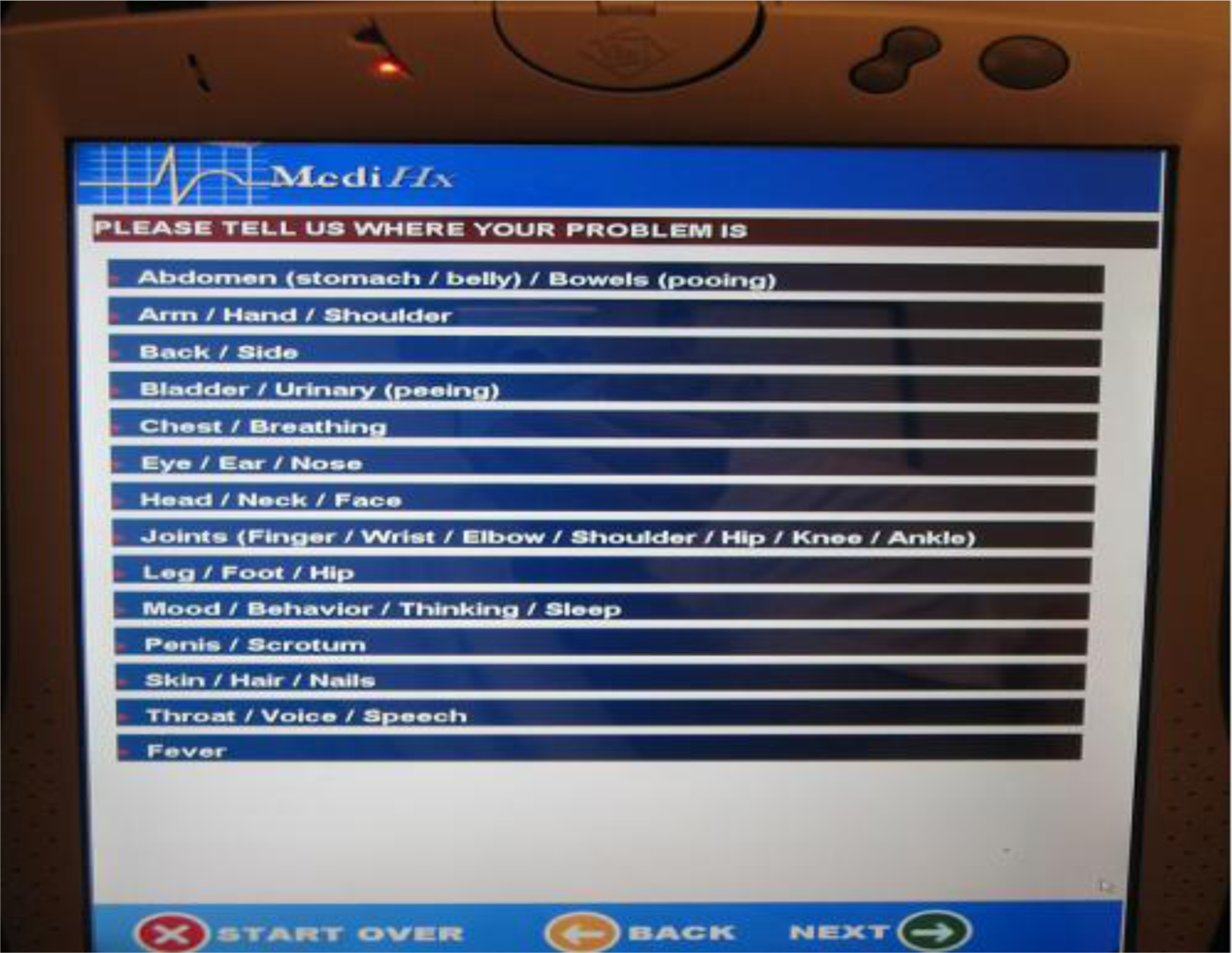
Computer-patient interviews:
Consumer Feedback:
Patient registration and clinic organisation:
Remote consultation and patient monitoring:
3.4. Longevity
3.5. Hardware Issues
Printers:
Handsets:
3.6. Kiosk Locations
Opportunistic community sites:
Willingness of community sites to host a kiosk:
3.7. Kiosk Users
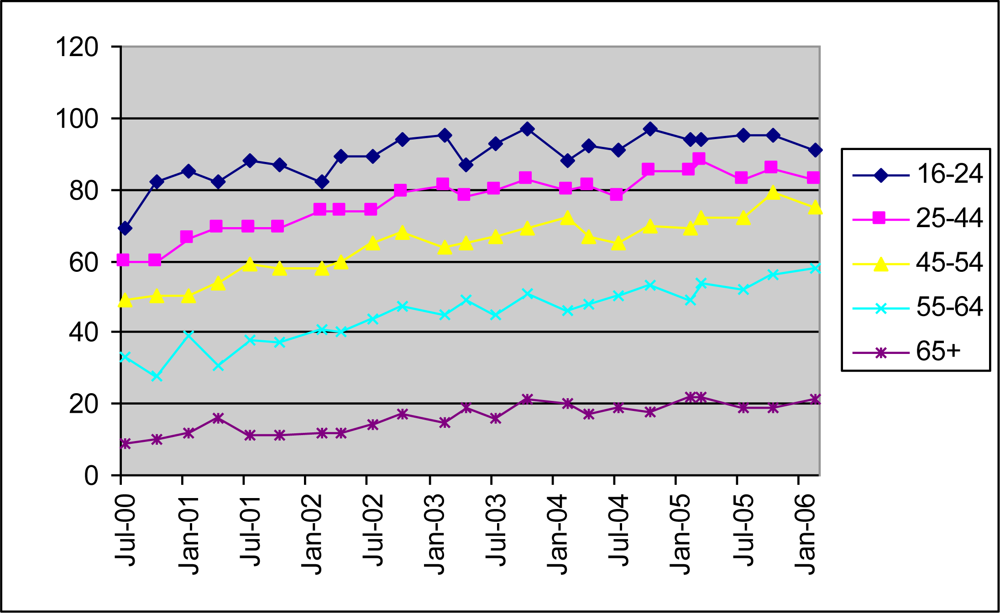
Age:
Social class and deprivation:
Disabilities:
Ethnicity, literacy and language:
3.8. Which Kiosks Are Successful?
3.9. Examples of Success (Opportunistic Kiosks)
Michigan Health Kiosk:
Commercial kiosks in the UK:
Other widely available kiosks in UK:
Opportunistic non health installations:
3.10. Examples of Success (Integrated Kiosks)
Feedback:
Registration:
Computer-patient interviewing:
3.11. Why Do Kiosks Fail?
3.12. Equity and the Digital Divide
3.13. How Current Trends May Influence Kiosks
3.14. Videofeeds from Existing Websites and Organisations
3.15. Kiosk in Community Development
3.16. Taking Kiosk Development Forward
- Show they are aware of successes and failures in kiosk use.
- Have a clear statement of how success for the new kiosk would be measured.
- Involve partnership between information, location, and system providers and a plan for how kiosk use will continue beyond the pilot stage.
- Have novel ideas for presentation and integration into location activities.
- Include some independent method for audit of information quality and assessment of cost effectiveness and equity.
- Schools in a region might work with national or local charities to develop kiosks with quizzes or ‘local magazines’ possibly re-using web-based materials where appropriate but adding a local and fun dimension to the interaction. Kiosks might be sited in locations targeted at older people. Author-schoolchildren would demonstrate the kiosks to older people and engage them with their use.
- As described above DIPEX might be ‘kiosked’, i.e. presented in a simpler format suitable for touchscreen access. A changing and random selection of nine people talking about a particular topic (e.g. cancer) might be presented in a cancer centre. Nursing or other staff would need to be involved and to encourage patients and their companions to use the kiosks. Success would be measured by patient and nursing opinions and level of use.
- Ethnic minority groups may work with PALS locally, Trusts, charities etc to produce audiovisual interviewing kiosks to collect signs and symptoms using spoken language, or to produce tailored information.
- Kiosks might be used to streamline registration and patient flow in a clinic.
- Kiosk enquiry service in hospital, with a human interface – i.e. telehelp where kiosks at entrance link to one enquiry desk and provide other information.
- Some pilot experiments combining patient interviewing such as provided by IMH together with patient assessment systems such as Wellbeing, and patient/consumer education.
3.17. Dos and Don’ts of Health Kiosks
- DO involve the staff or other ‘community’ where the kiosk is to be sited. Unless there is buy in at a local level and people are prepared to look after it and make its use effective it will not work. Locally people need to be clear what constitutes successful kiosk use. Can this be expressed as (e.g.) everyone or a proportion of visitors to that site using the kiosk, or can it be expressed by some change of behaviour, or some improved data collection or patient/public satisfaction, or by some cost saving from using the kiosk to replace some other resource?
- DON’T ‘parachute in’ a kiosk if local staff have not been involved in bidding for one. Nicholas et al. conclude ‘Kiosks appear to have had little impact on the work of health professionals and reception and managerial staff were found to be inconvenienced by their introduction. Little thought was given by staff to the upkeep of the kiosks when they were purchased. Replenishing paper, trying to fix paper jams, and staying at work late to wait for technicians all created much ill-feeling among practice managers and receptionists.... Locations where a health professional helped patients to use the kiosk had a higher number of users per hour.’
- If sited in a health service setting, DO integrate into clinical practice. Use it for booking in, or for a pre-consultation interview, or for a post-consultation information prescription. However, Nicholas noted from their studies ‘The ‘patient information prescription’ pads (an attempt to integrate kiosks in surgery routines) were virtually unused, and there was little evidence of doctors referring patients to the system or searching it with them. .... Nurses were more proactive than GPs, and evidence was found to suggest that they valued information as an important part of a patient’s consultation and recovery programme.’ This indicates that integration into clinical practice will not be easy unless clinical staff can see obvious advantages.
- If possible, for opportunistic kiosks, DO involve local schools or groups in tailoring the information so that they have ownership and they bring friends and relatives to come to see ‘their work [150].
- DON’T include a printer on a kiosk unless someone (as in a bank or an airport) is prepared for a high maintenance job in keeping it working. It will work, as in a bank, if the whole process is cost effective. If production of a booklet or a record or something to be used in the clinical process is the main outcome (see e.g. the U.S. breast screening project [45] then it may be worth it.
- DO make the kiosk interesting and highly visible. Particularly if you want opportunistic use the kiosk needs to be clearly visible and people should be curious as to what it does. Healthpoint when it was launched in the early 1990s was new and novel. NHS kiosk when it was launched in 2001 looked too ‘corporate’. (See new and novel interfaces)
- DON’T overestimate the need for privacy and do not hide the kiosk away. (Some of the NHS kiosks were in pharmacy back rooms only available by appointment).
- On the other hand, DON’T make it look too much like a children’s toy or locate it in a way that this perception is reinforced, otherwise its use may be dominated by toddlers and small children.
- DON’T think you are going to solve the digital divide just by providing kiosks. There are other ways of tackling this, for example, by the provision of Internet connected computers in libraries or opening up school computer labs for parents and grandparents, by aiming to bridge the generation gap through projects such as Liverpool scheme on mobile phones[151]. On the other hand, kiosks may help ensure that at least some information is more widely accessible.
- DON’T try to replicate the Internet on a kiosk. Standing kiosk use is likely to be for a short period and more focused game or ‘page turning’ applications to capture interest for a short period are needed rather than offering ability to search a database or the web. Seated booth use may be longer.
- If the kiosk just provides opportunistic information DO make it clear that information on the kiosk will change frequently otherwise no-one will come to it for repeat use.
- DO talk to private sector suppliers
- DON’T forget that the TV and other mass media may be the most effective way of getting across a specific health promotion message. Doing so within the context of fiction and celebrity may be as effective as through health promotion video/film. For example, cervical cancer screening rates soared after a SOAP character contracted and died from cervical cancer [30]. Celebrity cancers such as Kylie Minogue can raise awareness much more cost effectively than a 1000 kiosks [152,153]. However, kiosks can be used to personalise, tailor, and reinforce a mass media message.
- DO think about using kiosk with sound output and sound assisted input for groups who do not read English.
4. Conclusions
- Integrated kiosks: when information provision can be integrated with services, for example, in walk-in centres, outpatient areas, occupational health settings, etc and can focus on a particular task, such as signing in to a service, collection of data (including perhaps physical monitoring) or structured interview, in information prescription, planned education, or providing patient access to their records.
- Opportunistic kiosks: when they can be used in novel and entertaining ways to grab people’s attention and complement other media in health promotion amongst casual users, in both health service and community settings. The basic nature of an opportunistic ‘stand up’ kiosk should not be forgotten – people will use it for maybe two minutes (so there is little point in having deep nested information) and will probably only use it again if they think there is something new. Opportunistic kiosks should be obvious and in areas where there is a large flow of people. The need for privacy can be overstated and depends on the type of site.
Acknowledgments
References
- Mandl, KD; Katz, SB; Kohane, IS. Social equity and access to the World Wide Web and e-mail: implications for design and implementation of medical applications. In Proceedings AMIA Annual Symposium; Hanley and Belfus: Philadelphia, USA, 1998; pp. 215–219. [Google Scholar]
- Servaes, J; Heinderyckx, F. The ‘new’ ICTs environment in Europe: closing or widening the gap? Telematics. Inform 2002, 19, 91–115. [Google Scholar]
- West, DM; Miller, EA. The digital divide in public e-health: Barriers to accessibility and privacy in state health department websites. J. Health Care Poor Underserve 2006, 17, 652–667. [Google Scholar]
- Warren, M. The digital vicious cycle: Links between social disadvantage and digital exclusion in rural areas. Telecommun. Policy 2007, 31, 374–388. [Google Scholar]
- Brodie, M; Flournoy, RE; Altman, DE; Blendon, RJ; Benson, JM; Rosenbaum, MD. Health information, the Internet, and the digital divide. Health Affair 2000, 19, 255–265. [Google Scholar]
- NOS Households with access to the Internet, GB.
- National Statistics Internet Access, 65% of households had access in 2008.
- NOS Adults who have ever used the Internet by sex/age (Great Britain): Individual Internet Access.
- Jones, R; Pearson, J; McGregor, S; Cawsey, AJ; Barrett, A; Craig, N; Atkinson, JM; Gilmour, WH; McEwen, J. Randomised trial of personalised computer based information for cancer patients. Brit. Med. J 1999, 319, 1241–1247. [Google Scholar]
- Jones, R; McGhee, SM; McGhee, D. Patient on-line access to medical records in general practice. Health Bull 1992, 50, 143–150. [Google Scholar]
- Glazebrook, C; Garrud, P; Avery, A; Coupland, C; Williams, H. Impact of a multimedia intervention “Skinsafe” on patients’ knowledge and protective behaviors. Prev. Med 2006, 42, 449–454. [Google Scholar]
- Benaroia, M; Elinson, R; Zarnke, K. Patient-directed intelligent an interactive computer medical history-gathering systems: A utility and feasibility study in the emergency department. Int. J. Med. Inform 2007, 76, 283–288. [Google Scholar]
- Van Den Kerkhof, EG; Goldstein, DH; Blaine, WC; Rimmer, MJ. A comparison of paper with electronic patient-completed questionnaires in a preoperative clinic. Anesth. Analg 2005, 101, 1075–1080. [Google Scholar]
- Boudioni, M. Report on Use of Touch Screens to Portray Patient Choice (in relation to socially excluded groups, in particular); Commissioned by the Access, Booking and Choice Directorate of the NHS; College of Health: London, UK, 2003; p. 49. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, CA. Digital consumer health information and advisory services in the UK: a user evaluation and sourcebook; City University Centre for information behaviour and the evaluation of research (Ciber): London, U.K, March 2004; p. 69. [Google Scholar]
- Jones, R. Do health kiosks have a role in 2008?
- Gann, R. The people their own physicians: 2000 years of patient information. Health Libraries Rev 1987, 4, 151–155. [Google Scholar]
- Lafaille, R; Hiemstra, H. The regimen of Salerno: a contemporary analysis of a medieval life style programme. Health Promot. Int 1990, 5, 57–74. [Google Scholar]
- Rayner, C. Reality and expectation of the British NHS consumer. J. Adv. Nurs 1979, 4, 69–77. [Google Scholar]
- Clement-Jones, V. Cancer and beyond: the formation of BACUP. Brit. Med. J 1985, 291, 1021–1023. [Google Scholar]
- Lemire, M; Pare, G; Sicotte, C; Harvey, C. Determinants of Internet use as a preferred source of information on personal health. Int. J. Med. Inform 2008, 77, 723–734. [Google Scholar]
- Rice, RE. Influences, usage, and outcomes of Internet health information searching: Multivariate results from the Pew surveys. Int. J. Med. Inform 2006, 75, 8–28. [Google Scholar]
- Bartlett, E. Historical glimpses of patient education in the United States. Pat. Educ. Counsel 1986, 8, 135–139. [Google Scholar]
- Doll, R; Hill, AD. Smoking and carcinoma of the lung. Brit. Med. J 1950, 221, 739–748. [Google Scholar]
- Lalonde, M. A new perspective on the health of Canadians; Health and Welfare Canada: Ottawa, Canada, 1974. [Google Scholar]
- Gann, R. Information services and health promotion: what libraries can do. Health Educ. J 1986, 45, 112–115. [Google Scholar]
- Etzwiler, DD. Current status of patient education. J. Amer. Med. Ass 1973, 220, 583. [Google Scholar]
- Wise, P; Farrant, S; Dowlatshahi, D; Fromson, B; Meadows, K. Computer-based learning and prescriptive feedback improves diabetes knowledge and control (Abstract). Diabetic. Med 1985, 2, 302a. [Google Scholar]
- Homer, GR. Computer aided training in a renal dialysis ward – a unique approach. Current Perspectives in Health Computing Conference Proceedings, Sussex University, March 1985; Bryant, J, Kostrewski, B, Eds.; BJHC Books: Weybridge, Surrey, UK, 1985; pp. 113–127. [Google Scholar]
- Howe, A; Owen-Smith, V; Richardson, J. The impact of a television soap opera on the NHS Cervical Screening Programme in the North West of England. J. Public Health Med 2002, 24, 299–304. [Google Scholar]
- Jones, RB; McLachlan, K. HEALTHPOINT: a public access health information system. In Current Perspectives in Health Computing; Richards, B, Ed.; BJHC Books: Weybridge, Surrey, UK, 1990; pp. 65–69. [Google Scholar]
- Jones, RB; Navin, LM; Murray, KJ. Use of a community-based touch-screen public-access health information system. Health Bull 1993, 51, 34–42. [Google Scholar]
- Jones, RB; Edgerton, E; Baxter, I; Naven, LM; Ritchie, J; Bell, G. Where should a public access health information system be sited? Interact. Comput 1993, 5, 413–421. [Google Scholar]
- Naven, L; Jones, R; Kohli, H; Crawford, J. How should we evaluate a public-access health information system? In Current Perspectives in Health Computing; Richards, B, Ed.; BJHC Books: Weybridge, Surrey, UK, 1996; pp. 557–562. [Google Scholar]
- Campbell, GM; Jones, RB. A computer-based patient education system in the radiology department. In Current Perspectives in Health Computing; Richards, B, Ed.; BJHC Books: Weybridge, Surrey, UK, 1992; pp. 113–120. [Google Scholar]
- Jones, RB; Balfour, F; Gillis, M; Stobo, D; Cawsey, A; Donaldson, K. The accessibility of computer-based health information for patients: kiosks and the Web; Patel, VM, Rogers, R, Haux, R, Eds.; International Medical Informatics Association: London, UK, 2001; pp. 1469–1473. [Google Scholar]
- Sanz, F; Loza, MI; Ahlgrimm, ED; Baetens, P; Cuypers, J; Cranz, H; Coronel, M; FernandezLopez, JL; DeMora, A; SosaIudicissa, M. Telematics in community pharmacies to support responsible self-medication. The TESEMED project; Brender, J, Christensen, JP, Scherrer, JR, McNair, P, Eds.; I O S Press: Copenhagen, Denmark, 1996; pp. 141–145. [Google Scholar]
- Sanz, F; Silveira, C; Diaz, C; Alonso, A; Loza, MI; Cordero, L; Fernandez-Llimos, F; Cadavid, MI; Tiddens, L; Giorgio, F; Cranz, H; Henderson, K; Mircheva, J; Fernandez, JL. Information technology in community pharmacies for supporting responsible self-medication. Amer. J. Health-System Pharm 2000, 57, 1601–1603. [Google Scholar]
- Cross, M. Face to face with the future of remote medical consultations. Guardian; Guardian News and Media Limited: London, UK, 2008.
- Metlay, JP; Camargo, CA; MacKenzie, T; McCulloch, C; Maselli, J; Levin, SK; Kersey, A; Gonzales, R; Invest, I. Cluster-randomized trial to improve antibiotic use for adults with acute respiratory infections treated in emergency departments. Ann. Emerg. Med 2007, 50, 221–230. [Google Scholar]
- Thompson, DA; Lozano, P; Christakis, DA. Parent use of touchscreen computer kiosks for child health promotion in community settings. Pediatrics 2007, 119, 427–434. [Google Scholar]
- Picker Institute Europe; Customer Research Technology. Continuous Patient Feedback - Pilot Survey. Heatherwood and Wexham Park Hospitals NHS Foundation Trust; Picker Institute: London, UK, 2007. [Google Scholar]
- Dixon, S; Bunker, T; Chan, D. Outcome scores collected by touchscreen: medical audit as it should be in the 21st century? Ann. Roy. Coll. Surg. Engl 2007, 89, 689–691. [Google Scholar]
- Gielen, AC; McKenzie, LB; McDonald, EM; Shields, WC; Wang, MC; Cheng, YJ; Weaver, NL; Walker, AR. Using a computer kiosk to promote child safety: Results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics 2007, 120, 330–339. [Google Scholar]
- Kreuter, MW; Black, WJ; Friend, L; Booker, AC; Klump, P; Bobra, S; Holt, CL. Use of computer kiosks for breast cancer education in five community settings. Health Educ. Behav 2006, 33, 625–642. [Google Scholar]
- Aagaard, EM; Nadler, P; Adler, J; Maselli, J; Gonzales, R. An interactive computer kiosk module for the treatment of recurrent uncomplicated cystitis in women. J. Gen. Intern. Med 2006, 21, 1156–1159. [Google Scholar]
- McDonald, EM; Solomon, B; Shields, W; Serwint, JR; Jacobsen, H; Weaver, NL; Kreuter, M; Gielen, AC. Evaluation of kiosk-based tailoring to promote household safety behaviors in an urban pediatric primary care practice. Pat. Educ. Counsel 2005, 58, 168–181. [Google Scholar]
- Peters, J; Jackson, M. Accessibility and use of touchscreens by black and ethnic minority groups in the three cities project. Ethn. Health 2005, 10, 199–211. [Google Scholar]
- Picker Institute Europe; Intouch with Health; Trust; Lothian University NHS Trust. An evaluation of alternative methods of continuous patient questionnaire completion & results presentation; Picker Institute: London, UK, 2005; p. 13. [Google Scholar]
- Porter, SC; Cai, ZH; Gzibbons, W; Goldmann, DA; Kohane, IS. The asthma kiosk: A patient-centered technology for collaborative decision support in the emergency department. J. Amer. Med. Inform. Assoc 2004, 11, 458–467. [Google Scholar]
- Porter, SC; Forbes, P; Feldman, HA; Goldmann, DA. Impact of patient-centered decision support on quality of asthma care in the emergency department. Pediatrics 2006, 117, E33–E42. [Google Scholar]
- Porter, SC; Kohane, IS; Goldmann, DA. Improving data quality: A parent-completed computer interview to capture medication history. Pediatr. Res 2004, 55, 120A. [Google Scholar]
- Porter, SC; Kohane, IS; Goldmann, DA. Parents as partners in obtaining the medication history. J. Amer. Med. Inform. Assoc 2005, 12, 299–305. [Google Scholar]
- Sanghavi, DM. Taking well-child care into the 21st century - A novel, effective method for improving parent knowledge using computerized tutorials. Arch. Ped. Adolesc. Med 2005, 159, 482–485. [Google Scholar]
- Goldschmidt, L; Goodrich, GL. Development and evaluation of a point-of-care interactive patient education kiosk. J. Telemed. Telecare 2004, 10, S30–S32. [Google Scholar]
- Goldschmidt, L. Information Technology in Ophthalmology and Medicine: Patient Education Kiosks. In Tele-ophthalmology; Springer-Verlag: New York, USA, 2006; p. 10. [Google Scholar]
- Radvan, D; Wiggers, J; Hazell, T. HEALTH CHIPs: opportunistic community use of computerized health information programs. Health Educ. Res 2004, 19, 581–590. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. The characteristics of users and non-users of a kiosk information system. Aslib. Proc 2004, 56, 48–61. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. Three years of digital consumer health information: a longitudinal study of the touch screen health kiosk. Inform. Process. Manag 2003, 39, 479–502. [Google Scholar]
- Connell, CM; Shaw, BA; Holmes, SB; Hudson, ML; Derry, HA; Strecher, VJ. The development of an Alzheimer’s disease channel for the Michigan Interactive Health Kiosk Project. J. Health Commun 2003, 8, 11–22. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. Delivering consumer health information digitally: A comparison between the web and touchscreen kiosk. J. Med. Systems 2003, 27, 13–34. [Google Scholar]
- Gould, SM; Anderson, J. Economic analysis of bilingual interactive multimedia nutrition education. J. Nutr. Educ. Behavior 2002, 34, 273–278. [Google Scholar]
- Berber, B; Lawless, K; Smolin, L; Brodsky, I; Girotti, M; Pelaez, L; Eiser, A. Diabetes and your eyes: A pilot study on multimedia education for underserved populations. Amia 2002 Symposium, Proc 2002, 1026. [Google Scholar]
- Lawless, K; Gerber, B; Smolin, L. Diabetes and your eyes: A pilot study on multimedia education for underserved populations. Int J Instr Media 2004, 1074–1079. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. An evaluation of the use of NHS touch-screen health kiosks: a national study. Aslib. Proc 2002, 54, 372–384. [Google Scholar]
- Boyes, A; Newell, S; Girgis, A. Rapid assessment of psychosocial well-being: are computers the way forward in a clinical setting? Qual. Life Res 2002, 11, 27–35. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. Establishing metrics for the evaluation of touch screen kiosks. J. Inform. Sci 2001, 27, 61–71. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. Health kiosk use: a national comparative study. Aslib. Proc 2001, 53, 130–140. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. Comparing web and touch screen transaction log files. J. Med. Int. Res 2001, 3, e18. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P. The impact of location on the use of information systems - Case study - health information kiosks. J. Doc 2002, 58, 284–301. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P; Chahal, P. Determinants of health kiosk use and usefulness: Case study of a kiosk which serves a multi-cultural population. Libri 2001, 51, 102–113. [Google Scholar]
- Nicholas, D; Huntington, P; Williams, P; Vickery, P. Health information: an evaluation of the use of touch screen kiosks in two hospitals. Health Inf. Libr. J 2001, 18, 213–219. [Google Scholar]
- Nicholas, D; Williams, P; Huntington, P. Digital health information: case study the information kiosk. Aslib. Proc 2000, 52, 315–330. [Google Scholar]
- Nicholas, D; Williams, P; Huntington, P. Health information kiosk use in health organisations: the views of the health professionals. Aslib. Proc 2001, 53, 368–386. [Google Scholar]
- Jones, R. Evaluation of NHS Direct kiosks; University of Glasgow: Glasgow, UK, 2001; p. 28. [Google Scholar]
- Ershler, LE; East, TD. Information kiosks: Portals to our patients and their families. J Amer Med Inform Assoc 2000, 1003–1003. [Google Scholar]
- Lewis, D; Nath, C. Feasibility of a kiosk-based patient education system in a busy outpatient clinic setting. Diabetes Educator 1997, 23, 577–586. [Google Scholar]
- Strecher, VJ; Greenwood, T; Wang, C; Dumont, D. Interactive multimedia and risk communication. J. Nat. Cancer Inst. Monogr 1999, 25, 134–139. [Google Scholar]
- Westman, J; Hampel, H; Bradley, T. Efficacy of a touchscreen computer based family cancer history questionnaire and subsequent cancer risk assessment. J. Med. Genetics 2000, 37, 354–360. [Google Scholar]
- Schneider, WJ; Furth, PA; Blalock, TH; Sherrill, TA. A pilot study of a headache program in the workplace. The effect of education. J. Occupat. Env. Med 1999, 41, 202–209. [Google Scholar]
- Thomas, R; Cahill, J; Santilli, L. Using an interactive computer game to increase skill and self-efficacy regarding safer sex negotiation: field test results. Health Educat. Behav 1997, 24, 71–86. [Google Scholar]
- Lindholm, LH; Isacsson, A; Slaug, B; Maller, TR. Acceptance by Swedish users of a multimedia program for primary and secondary prevention of malignant melanoma. J. Cancer Educ 1998, 13, 207–212. [Google Scholar]
- Endres, J; Welch, T; Perseli, T. Use of a computerized kiosk in an assessment of food safety knowledge of high school students and science teachers. J. Nutr. Educ 2001, 33, 37–42. [Google Scholar]
- Hripcsak, G; Knirsch, CA; Jain, NL; Stazesky, RC; Pablos-Mendez, A; Fulmer, T. A health information network for managing innercity tuberculosis: Bridging clinical care, public health, and home care. Comput. Biomed. Res 1999, 32, 67–76. [Google Scholar]
- Wylie-Rosett, J; Swencionis, C; Ginsberg, M; Cimino, C; Wassertheil-Smoller, S; Caban, A; Segal-Isaacson, CJ; Martin, T; Lewis, J. Computerized weight loss intervention optimizes staff time; the clinical and cost results of a controlled clinical trial conducted in a managed care setting. J. Amer. Diet. Assn 2001, 101, 1155–1162. [Google Scholar]
- Anderson, ES; Winett, RA; Wojcik, JR; Winett, SG; Bowden, T. A computerized social cognitive intervention for nutrition behavior: direct and mediated effects on fat, fiber, fruits, and vegetables, self-efficacy, and outcome expectations among food shoppers. Ann. Behav. Med 2001, 23, 88–100. [Google Scholar]
- Carroll, JM; Stein, C; Byron, M; Dutram, K. Using interactive multimedia to deliver nutrition education to Maine’s WIC clients. J. Nutr. Educ 1996, 28, 19–25. [Google Scholar]
- Maynard, L. Lifestyle Health Screening Pilot Study Report; EDF Occupational Health Department: London, UK, 2008. [Google Scholar]
- Baldry, M; Cheal, C; Fisher, B; Gillet, M; Huet, V. Giving patients their own records in general practice: experience of patients and staff. Brit. Med. J 1986, 292, 596–598. [Google Scholar]
- Fisher, B; Fitton, R; Poirier, C; Stables, D. Patient record access - the time has come! Br. J. Gen. Pract 2007, 57, 507–511. [Google Scholar]
- Department of Health. Copying Letters to Patients.
- Jones, RB; Atkinson, JM; Coia, DA; Paterson, L; Morton, AR; McKenna, K; Craig, N; Morrison, J; Gilmour, WH. Randomised trial of personalised computer based information for patients with schizophrenia. Brit. Med. J 2001, 322, 835–840. [Google Scholar]
- Pyper, C; Amery, J; Watson, M; Crook, C. Patients’ experiences when accessing their on-line electronic patient records in primary care. Br. J. Gen. Pract 2004, 54, 38–43. [Google Scholar]
- Pyper, C; Amery, J; Watson, M; Crook, C. Access to electronic health records in primary care - a survey of patients’ views. Med Sci Monit 2004, 10, SR17–SR22. [Google Scholar]
- Pyper, C; Amery, J; Watson, M; Crook, C; Thomas, B. Patients’ access to their online electronic health records. J. Telemed. Telecare 2002, 8, 103–105. [Google Scholar]
- Boorer, L. Pilot study of the impact of Renal Patient View; MSc DissertationUniversity of Plymouth: Plymouth, UK, 2008. [Google Scholar]
- Slack, WV; Hicks, GP; Reed, CE; van Cura, LJ. A computer-based medical history system. N. Engl. J. Med 1966, 274, 194–198. [Google Scholar]
- Jones, R; Knill-Jones, RP. Electronic Patient Record Project: Direct Patient Input to the Record; University of Glasgow, Department of Public Health: Glasgow, UK, 1994; p. 13. [Google Scholar]
- Knill-Jones, RP; Crean, GP; Holden, R; Marjoribanks, F. Practical aspects of expert systems and computer-taken clinical histories in dyspepsia. MIC90 Proceedings of the first Hong Kong (Asia-Pacific) Medical Informatics Conference; Hedley, AJ, Chun Por, W, Eds.; Hong Kong Society of Medical Informatics Ltd and Hong Kong Computer Society: Hong Kong, China, 1991; pp. 192–199. [Google Scholar]
- Jones, RB; Cawsey, A; Al-Barwani, F; Reynolds, J; Knill-Jones, RP. Researching a patient workstation. In HC96, Current Perspectives in Health Computing; Richards, B, Ed.; BJHC Books: Weybridge Surrey, UK, 1996; pp. 678–684. [Google Scholar]
- Vitkun, SA; Halpern-Lewis, JG; Williams, SA; Gage, JS; Poppers, PJ. Patient’s perceptions of an anesthesia preoperative computerized patient interview. J. Clin. Monit. Comput 1999, 15, 503–507. [Google Scholar]
- Dugaw, JE; Civello, K; Chuinard, C; Jones, GN. Will patients use a computer to give a medical history? J. Fam. Pract 2000, 49, 921–923. [Google Scholar]
- Glasgow, RE; Toobert, DJ; Hampson, SE; Noell, JW. A brief office-based intervention to facilitate diabetes dietary self-management. Health Educ. Res 1995, 10, 467–478. [Google Scholar]
- Glasgow, RE; Toobert, DJ; Hampson, SE; Strycker, LA. Implementation, generalization and long-term results of the “choosing well” diabetes self-management intervention. Pat. Educ. Counsel 2002, 48, 115–122. [Google Scholar]
- Cull, A; Gould, A; House, A; Smith, A; Strong, V; Velikova, G; Wright, P; Selby, P. Validating automated screening for psychological distress by means of computer touchscreens for use in routine oncology practice. Brit. J. Cancer 2001, 85, 1842–1849. [Google Scholar]
- Bachman, JW. The patient-computer interview: A neglected tool that can aid the clinician. Mayo. Clin. Proc 2003, 78, 67–78. [Google Scholar]
- West Fife Locality Conference Evaluation Report 07/11/07; Dunfermline and West Fife Community Health Partnership: Dunfermline, UK, 2007.
- EMIS. EMIS case study: Greyfriars Surgery. December 2005: Patients help to reduce check-in queues using automated arrivals.
- Ellis, S; Waring, N. Piloting eReception in an acute setting.
- Kings College Hospital. NHS Foundation Trust Camberwell Sexual Health Centre.
- Chisolm, DJ; Young, RR; McAlearney, AS. Implementation of a touch-screen new patient registration system: a case study. J. Med. Pract. Manag 2005, 21, 159–162. [Google Scholar]
- Kaae, L. Check out the check-in.
- Fintor, L. The Michigan health kiosk: Cancer info on the go. J. Nat. Cancer Inst 1998, 90, 809–810. [Google Scholar]
- Hunter, E; Travers, H; Gibson, J. Health Interactive Technology Report to Health Promotion Queensland on “Implementing and evaluating an innovative, sustainable, IT-based approach to enhancing health literacy and local capacity in disadvantaged remote populations”; Health Promotion Queensland: Brisbane, Australia, 2007; p. 79. [Google Scholar]
- Hunter, E; Travers, H; Gibson, J; Campion, J. Bridging the triple divide: performance and innovative multimedia in the service of behavioural health change in remote Indigenous settings. Australas. Psych 2007, 15, S44–48. [Google Scholar]
- Jones, RB; Pearson, J; Cawsey, AJ; Bental, D; Barrett, A; White, J; White, CA; Gilmour, WH. Effect of different forms of information produced for cancer patients on their use of the information, social support, and anxiety: randomised trial. Brit. Med. J 2006, 332, 942–946A. [Google Scholar]
- Naven, L; Jones, R; Kohli, H; Crawford, J. How should we evaluate a public-access health information system? In Current Perspectives in Health Computing 1990; Richards, B, Ed.; BJHC Books: Weybridge, UK, 1996; pp. 557–62. [Google Scholar]
- Ehealthinsider Healthcare booths go on trial in Scotland.
- Jones, RB; Edgerton, E; Baxter, I; Naven, LM; Ritchie, J; Bell, G; Murray, K. Where Should a Public-Access Health Information-System Be Sited. Interact. Comput 1993, 5, 413–421. [Google Scholar]
- Metlay, JP; Camargo, CA; Bos, K; Gonzales, R. Assessing the suitability of intervention sites for quality improvement studies in emergency departments. Acad. Emerg. Med 2005, 12, 667–670. [Google Scholar]
- Kaltenthaler, E; Shackley, P; Stevens, K; Beverley, C; Parry, G; Chilcott, M. Computerised Cognitive Behavioural Therapy for Depression and Anxiety Report commissioned by NHS R&D HTA Programme on behalf of NICE; National Institute for Clinical Excellence: London, UK, 2002. [Google Scholar]
- Selwyn, N; Gorard, S; Furlong, J; Madden, L. Older adults’ use of information and communications technology in everyday life. Ageing Soc 2003, 23, 561–582. [Google Scholar]
- Sagawa, H; Takeuchi, M. Development of an information kiosk with a sign language recognition system. Cuu 2000 Conf Proc 2000, 149–150. [Google Scholar]
- Young, RTP. 3rd age interfaces: A usability evaluation of the ‘your guide’ Kiosk prototype from an older user’s perspective. In Universal Access and Assistive Technology; Keates, S, Langdon, P, Clarkson, PJ, Robinson, P, Eds.; Springer: New York, NY, USA, 2002; pp. 141–150. [Google Scholar]
- Jackson, M; Peters, J. Introducing touchscreens to black and ethnic minority groups—a report of processes and issues in the Three Cities project. Health Inform. Libr. J 2003, 20, 143–149. [Google Scholar]
- Hahn, EA; Cellal, D; Dobrez, DG; Shiomoto, G; Taylor, SG; Galvez, AG; Diaz, P; Valenzuela, V; Chiang, H-L; Khan, S; Hudgens, SA; Du, H. Quality of life assessment for low literacy Latinos: a new multimedia program for self-administration. J. Oncol. Man 2003, 12, 9–12. [Google Scholar]
- Hahn, EA; Cella, D; Dobrez, D; Shiomoto, G; Marcus, E; Taylor, SG; Vohra, M; Chang, C-H; Wright, BD; Linacre, JM; Weiss, BD; Valenzuela, V; Chiang, H-L; Webster, K. The talking touchscreen: a new approach to outcomes assessment in low literacy. Psycho-Oncol 2004, 13, 86–95. [Google Scholar]
- Hahn, EA; Cella, D; Dobrez, DG; Weiss, BD; Du, H; Lai, J-S; Victorson, D; Garcia, SF. The impact of literacy on health-related quality of life measurement and outcomes in cancer outpatients. Qual. Life Res 2007, 16, 495–507. [Google Scholar]
- Ida, M; Mori, H; Nakamura, S; Shikano, K. A noise-robust speech input interface for information kiosk terminals. Electron. Commun. Jap. II 2004, 87, 51–61. [Google Scholar]
- McCauley, L; D’Mello, S. MIKI: A speech enabled Intelligent Kiosk. Intelligent. Virtual Agents, Proc 2006, 4133, 132–144. [Google Scholar]
- Thumboo, J; Wee, H-L; Cheung, Y-B; Machin, D; Luo, N; Fong, K-Y. Development of a Smiling Touchscreen multimedia program for HRQoL assessment in subjects with varying levels of literacy. Value Health 2006, 9, 312–319. [Google Scholar]
- Blignaut, P. An empirical methodology for usability analysis of a touchscreen-based information kiosk system for African users with low levels of computer literacy. User-Centered Interact. Paradigms Uni. Access Inf. Soc 2004, 3196, 203–218. [Google Scholar]
- Maguire, MC. A review of user-interface design guidelines for public information kiosk systems. Int. J. Human-Comput. Stud 1999, 50, 263–286. [Google Scholar]
- Jones, R; White, J; Craig, N; Morrison, J. A randomised controlled trial of computer-based treatment for psychological problems in primary care Final Report to Health Services Research Committee; University of Glasgow: Glasgow, UK, November 2000; p. 32. [Google Scholar]
- Dempski, KL; Harvey, BL. Touchable interactive walls: Opportunities and challenges. In Entertain Comput - Icec 2005; Springer Berlin: Heidelberg, Germany, 2005; pp. 192–202. [Google Scholar]
- HMC Manual of Services; HMC-Interactive: Plymouth, UK, 2008.
- Whitfield, L. Self-service kiosks for Birmingham hospital.
- Gray, M. Direct Electronic Patient Data Entry Workshops; Sept/Oct 2004 British Computer Society, Disability Group: London, UK, 2004. [Google Scholar]
- Jones, R; Knill-Jones, RP. Electronic Patient Record Project: Direct Patient Input to the Record: Update; University of Glasgow, Department of Public Health: Glasgow, UK, 1997; p. 13. [Google Scholar]
- Keefner Health Info Kiosks Generate Solid ROI: Study.
- Donoghue, D. Evaluation of the Public Internet Access Point Initiative; Hall Aitken: Glasgow, UK, August 04 2004; p. 51. [Google Scholar]
- Farrand, P. Development of a supported self-help book prescription scheme in primary care. Prim. Care Ment. Health 2005, 3, 61–66. [Google Scholar]
- Gilhooly, M; Gilhooly, K; Jones, R. Quality of life: conceptual challenges in exploring the role of ICT in active ageing. In Information and Communication Technologies for Active Ageing Opportunities and Challenges for the European Union; Cabrera, M, Malanowski, N, Eds.; IOS Press: Amsterdam, The Netherlands, 2009; pp. 49–76. [Google Scholar]
- Gilmour, J. A. Reducing disparities in the access and use of Internet health information. A discussion paper. Int. J. Nurs. Stud 2007, 44, 1270–1278. [Google Scholar]
- Chang, BL; Bakken, S; Brown, SS; Houston, TK; Kreps, GL; Kukafka, R; Safran, C; Stavri, PZ. Bridging the digital divide: Reaching vulnerable populations. J. Amer. Med. Inform. Assoc 2004, 11, 448–457. [Google Scholar]
- Gustafson, DH; Hawkins, R; McTavish, F; Pingree, S; Chen, WC; Volrathongchai, K; Stengle, W; Stewart, JA; Serlin, RC. Internet-based interactive support for cancer patients: Are integrated systems better? J. Communicat 2008, 58, 238–257. [Google Scholar]
- Gustafson, DH; McTavish, FM; Stengle, W; Ballard, D; Jones, E; Julesberg, K; McDowell, H; Landucci, G; Hawkins, R. Reducing the digital divide for low-income women with breast cancer: A feasibility study of a population-based intervention. J. Health Communicat 2005, 10, 173–193. [Google Scholar]
- Gustafson, DH; McTavish, FM; Stengle, W; Ballard, D; Hawkins, R; Shaw, BR; Jones, E; Julesberg, K; McDowell, H. Use and impact of eHealth system by low-income women with breast cancer. J. Health Communicat 2005, 10, 195–218. [Google Scholar]
- Gustafson, DH; Hawkins, RP; Boberg, EW; McTavish, F; Owens, B; Wise, M; Berhe, H; Pingree, S. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. Int. J. Med. Inform 2002, 65, 169–177. [Google Scholar]
- Jones, RB; Douglas, F; Naven, LM. Schoolchildren’s use of and ideas for a computer-based health information system. MIC94: Third Hong Kong (Asia-Pacific) Medical Informatics Conference Conference Proceedings; Hedley, AJ, Ed.; Hong Kong Computer Society: Hong Kong, China, 1994. [Google Scholar]
- Rowland, D. Mobile Phone Training for Older People Presentation. UK Public Health Association conference, Edinburgh, UK, April 2007.
- Kelaher, M; Cawson, J; Miller, J; Kavanagh, A; Dunt, D; Studdert, DM. Use of breast cancer screening and treatment services by Australian women aged 25–44 years following Kylie Minogue’s breast cancer diagnosis. Int. J. Epidemiol 2008, 37, 1326–1332. [Google Scholar]
- Twine, C; Barthelmes, L; Gateley, CA. Kylie Minogue’s breast cancer: Effects on referrals to a rapid access breast clinic in the UK. The Breast 2006, 15, 667–669. [Google Scholar]







| Setting, (Number of kiosks, reference | Year publication, country, (type of access) | Comments |
|---|---|---|
| Scottish telepresence project (N = ?1) [39] | 2008, Scotland, (R) | Newspaper article about teleconsultation where patient booth. Booth includes stethoscope, blood-pressure cuff and thermometer, works on a standard network & needs about 3.5 megabits per second. |
| Part of cluster RCT in 16 hospitals (so N = 8 intervention). [40] | 2007 USA, (O). | Package of interventions to improve antibiotic use in acute respiratory infection: clinical lead, posters, brochures, interactive tailored video kiosk. Modest decrease in antibiotics: but no reporting of kiosk as component. |
| Kiosks in library, government office, and a McDonald’s in low-income urban locations in Seattle Mar to Oct 2005. (N = 3) [41] | 2007 USA, (O) | Users entered child age, were shown selected info. McDonald’s most popular. 28% responded exit survey. 48% had less than high school education, 26% had never used the Internet. |
| Picker Institute study of patient feedback on two wards in hospitals in Slough. (N = 2) [42] | 2007 UK, (R/O) | Two inpatient wards (surgery/urology and respiratory) |
| Kiosks in aboriginal areas. (N = 11) | 2007 Australia, (O) | To improve health literacy in diabetes, alcohol use and child health for remote indigenous populations in Queensland. |
| Orthopaedic outpatients. (N = 1) [43] | 2007 England, (R) | To collect ‘outcome scores’ Oswestry Disability Score from patients |
| Chicago emergency department [44] | 2007 USA, (R) | To promote child safety. Received tailored report |
| Different sites in metropolitan St. Louis, Missouri, between June 2, 2003, and October 21, 2004. (four kiosks hosted at N = 40) [45] | 2006 USA, (O) | Reflections of You kiosk. Tailored magazines about breast cancer and mammography. Questions on touch-screen used to generate and print each tailored magazine. 44/110 potential hosts 44 agreed. 7/day valid usages. |
| Outpatient clinic California (one kiosk, small patient numbers). [46] | 2006, USA, (R) | Small scale patient education kiosk for management of uncomplicated urinary tract infections. When published162 women have accessed computer directed therapy. |
| Primary care waiting room USA. Tailored info. for parents (mean age 26). (N = 1) [47] | 2005, USA, (R) | Household safety. Information tailored to child and parent. |
| Health centres and libraries in deprived areas of Leicester, Sheffield, Nottingham (England) (N = 3) [48] | 2005 England, (O) | Written and spoken information on 10 topics in Chinese, Bengali, Gujarati, Urdu, and Mirpuri Punjabi. 2,456 users of 3 kiosks over 10 months. |
| Outpatient waiting areas. (N = 2) [49] | 2005 UK, (R/O) | Patient feedback in outpatient setting (diabetes and orthopaedics clinics) in Edinburgh |
| Five diabetes clinics in Chicago | 2005 USA, (R) | Aimed at low health literacy patients. Relatively less use of the computer among these participants |
| Emergency departments in USA (N = 1) [50–53] | 2004–6 USA, (R) | Used to collect medication information about asthma and make recommendations. Could be used sitting or standing. |
| Hospital paediatric waiting room in New Mexico USA for Navajo parents (N = 1).[54] | 2005 USA, (R) | Aim to improve knowledge of fever management, dental care, sleep position, nutrition, and car seat use |
| Patient waiting area of multi-specialty clinics, USA (N = 2) [55,56] | 2004–6 USA, (O) | Information about eye disease in Spanish and English. Two kiosks for 2.5 years, 1 for 1.5 years. 38,868 user sessions. |
| (1) kiosk in shopping centre; (2) kiosks in 18 community settings in New South Wales, Australia [57] | 2004 Australia, (O) | (1)Three-quarters noticed kiosk and 21% used it.
(2)57064 user sessions, i.e. 19 user sessions on average/day |
| Primary care waiting room near Edinburgh [58] | 2004 Scotland (O) | Studied characteristics of users Vs non users in a postal survey of just under 200 patients |
| 20 In Touch with Health kiosks sited in UK primary care [59] | 2003 UK, (O) | Studied 20 kiosks over three years and half years. Novelty value for 4–5 months followed by decline |
| Kiosks sited in churches, senior centres, schools, shopping malls, grocery stores, hospitals (N = 100) [60] | 2003 USA, (O) | Addition of Alzheimer ‘channel’ for Michigan Kiosk project. 100 kiosks sited in seniors centres, shopping malls etc. |
| In Touch and NHS kiosk compared with Surgery Door web site. England [61] | 2003 UK, (O) | Comparison of log files (time spent etc) between web information and kiosk information |
| Nutrition education in food assistance programs among Hispanics in USA [62] | 2002 USA, (R) | Bilingual Spanish-English. Comparative cost-effectiveness study Vs peer educators |
| Outpatient waiting room, diabetes eye examinations. [63,64] | 2002, USA, (R) | Aimed at underserved populations |
| NHS Direct kiosks England [65] | 2002 UK, (O) | Comparison of one month’s log data between 120 kiosks |
| Patient interviewing for anxiety and depression. [66] | 2002 USA, (R) | Validation study of computerised HADS versus paper HADS (N = 1,304) |
| Country | Kiosk name | Max number approx | Dates | Sources |
|---|---|---|---|---|
| UK | Healthpoint | 60 | 1989–1998 | [31] (Jones, personal knowledge) |
| UK | NHS Kiosk | 136 | Sep 2000-c.2005 | [75] (Bob Gann email) |
| UK | In Touch with Health | 200 | Approx 1997-Continuing | [67] emails from Kevin Snowball (In Touch with Health) |
| USA | Michigan | 100 | 1998–2004 | [60,78,113] |
| Aust | Health CHIPS | 20 | Main tranch of kiosks no longer supported, used in certain niche ‘markets’ | [57] (email Trevor Hazell) [114,115] |
| UK | Wellpoint | 268 | 2003-Continuing | Emails and phone calls Chris Dawson (Wellpoint) |
| UK | StartHere
BT Street Kiosks Colorama –iStop Community projects | 130
50 55 | 2004–2007
2007–2008 2000-continuing | Emails from Mark Worger, Business Development Officer StartHere |
| UK | Elephant kiosks | 164 | Current installations in Staffordshire and Suffolk Primary Care and, Cambridgeshire Hospital | Email Mark Worger on behalf of Annette Walker (Elephant Kiosks) |
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Jones, R. The Role of Health Kiosks in 2009: Literature and Informant Review. Int. J. Environ. Res. Public Health 2009, 6, 1818-1855. https://doi.org/10.3390/ijerph6061818
Jones R. The Role of Health Kiosks in 2009: Literature and Informant Review. International Journal of Environmental Research and Public Health. 2009; 6(6):1818-1855. https://doi.org/10.3390/ijerph6061818
Chicago/Turabian StyleJones, Ray. 2009. "The Role of Health Kiosks in 2009: Literature and Informant Review" International Journal of Environmental Research and Public Health 6, no. 6: 1818-1855. https://doi.org/10.3390/ijerph6061818
APA StyleJones, R. (2009). The Role of Health Kiosks in 2009: Literature and Informant Review. International Journal of Environmental Research and Public Health, 6(6), 1818-1855. https://doi.org/10.3390/ijerph6061818