The Importance of Gender-Sensitive Health Care in the Context of Pain, Emergency and Vaccination: A Narrative Review
Abstract
:1. Introduction
1.1. Gender and Public Health: Background
1.2. Aims
2. Methods
3. Gender Medicine and Gender-Sensitive Care
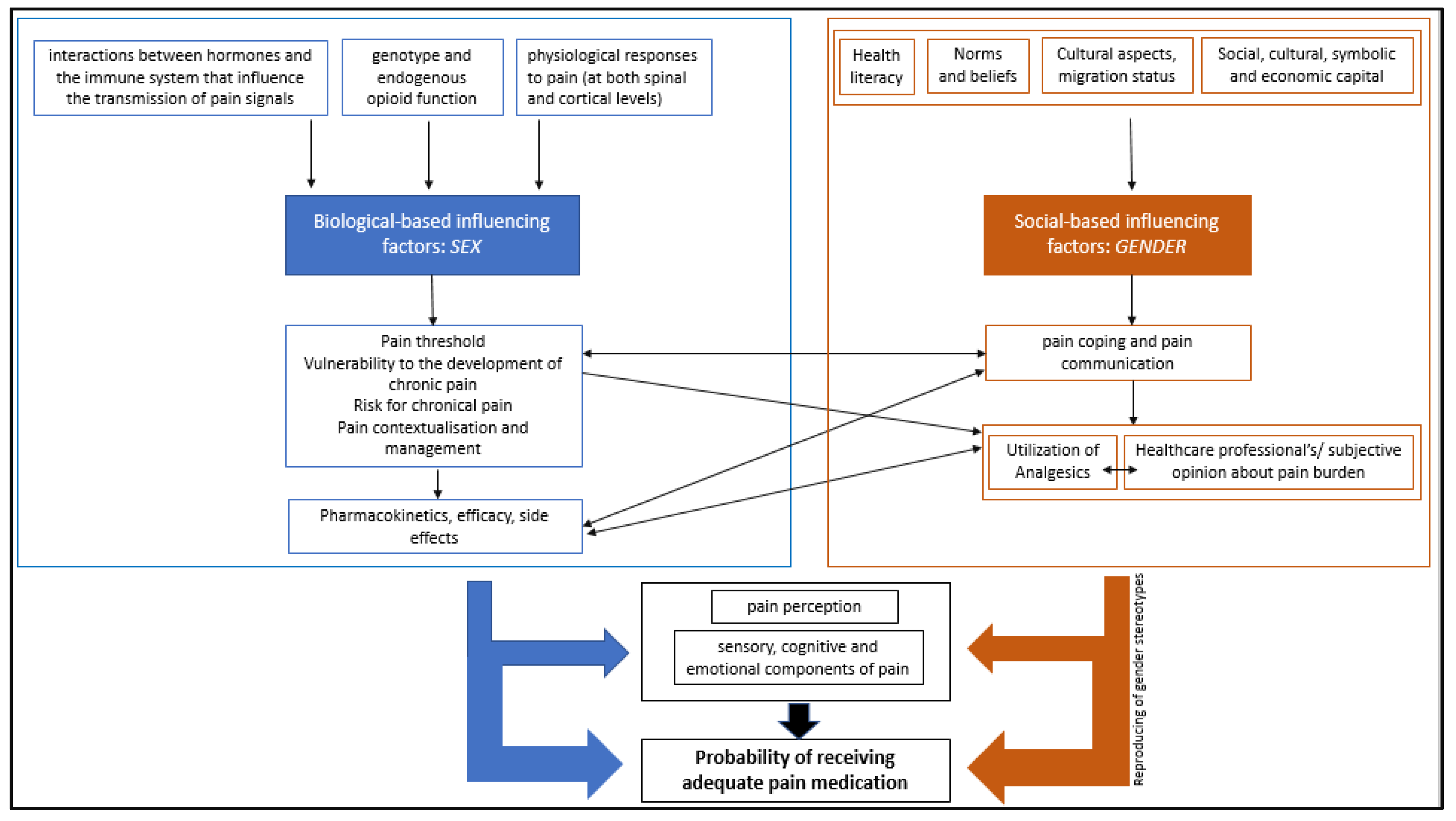
4. Case Study: Pain
4.1. Gender-Specific Pain Perception and Communication
4.2. Pain Management Depending on Gender
5. Case Study: Emergency Care
5.1. Gender Inequality in Emergency Care
5.2. Emergency Care and Gender Stereotypes
5.3. Consequences of Non-Gender-Sensitive Emergency Care
6. Case Study: Vaccination
6.1. Gender-Related Differences in Utilization
6.2. Sex Differences in Efficacy
6.3. Adverse Events and Gender
6.4. Lack of Sex- and Gender-Sensitive Vaccine Research
7. Discussion
7.1. Discussion of Overall Results
7.2. Answering Research Questions
7.3. Conclusions
7.4. Future Developments
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Celik, H.; Lagro-Janssen, T.A.; Widdershoven, G.G.; Abma, T.A. Bringing gender sensitivity into healthcare practice: A systematic review. Patient Educ. Couns. 2011, 84, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Simoes, E.; Brucker, S.Y.; Krämer, B.; Wallwiener, D. University Gynaecology and Obstetrics, quo vadis? A Department of Women’s Health-University Women’s Hospital of the future? Arch. Gynecol. Obstet. 2015, 291, 327–340. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Delivered by Women, Led by Men: A Gender and Equity Analysis of the Global Health and Social Workforce; Human Resources for Health Observer Series 2019, No. 24; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- European Institute for Gender Equality. Gender Equality Index. 2021: Health; EIGE: Vilnius, Lithuania, 2021. [Google Scholar]
- Manandhar, M.; Hawkes, S.; Buse, K.; Nosrati, E.; Magar, V. Gender, health and the 2030 agenda for sustainable development. Bull. World Health Organ. 2018, 96, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.M.; Yoon, S.-Y. Gender, Women, and the Tobacco Epidemic; WHO: Manila, Philippines, 2010. [Google Scholar]
- Gahagan, J.; Bryson, M.K. Introduction: Sex- and Gender-Based Analysis (SGBA) and Public Health. In Sex- and Gender-Based Analysis in Public Health; Gahagan, J., Bryson, M.K., Eds.; Springer: Cham, Switzerland, 2021; pp. 1–8. [Google Scholar]
- Miller, V.M.; Rocca, W.A.; Faubion, S.S. Sex Differences Research, Precision Medicine, and the Future of Women’s Health. J. Womens Health 2015, 24, 969–971. [Google Scholar] [CrossRef] [PubMed]
- van Hagen, L.J.; Muntinga, M.; Appelman, Y.; Verdonk, P. Sex- and gender-sensitive public health research: An analysis of research proposals in a research institute in the Netherlands. Women Health 2021, 61, 109–119. [Google Scholar] [CrossRef]
- Simba, H.; Ngcobo, S. Are Pandemics Gender Neutral? Women’s Health and COVID-19. Front. Glob. Womens Health 2020, 1, 570666. [Google Scholar] [CrossRef]
- Kuhlmann, E.; Lotta, G.; Fernandez, M.; Herten-Crabb, A.; Mac Fehr, L.; Maple, J.L.; Paina, L.; Wenham, C.; Willis, K. SDG5 “Gender Equality” and the COVID-19 pandemic: A rapid assessment of health system responses in selected upper-middle and high-income countries. Front. Public Health 2023, 11, 1078008. [Google Scholar] [CrossRef]
- Scott, K. Canada’s Gender Pandemic Response. Did It Measure Up? Canadian Centre for Policy Alternatives: Ottawa, ON, Canada, 2023. [Google Scholar]
- Bimpong, K.; Thomson, K.; Mcnamara, C.L.; Balaj, M.; Akhter, N.; Bambra, C.; Todd, A. The Gender Pain Gap: Gender inequalities in pain across 19 European countries. Scand. J. Public Health 2022, 50, 287–294. [Google Scholar] [CrossRef]
- Seijmonsbergen-Schermers, A.E.; van den Akker, T.; Rydahl, E.; Beeckman, K.; Bogaerts, A.; Binfa, L.; Frith, L.; Gross, M.M.; Misselwitz, B.; Hálfdánsdóttir, B.; et al. Variations in use of childbirth interventions in 13 high-income countries: A multinational cross-sectional study. PLoS Med. 2020, 17, e1003103. [Google Scholar] [CrossRef]
- Jones, L.; Othman, M.; Dowswell, T.; Alfirevic, Z.; Gates, S.; Newburn, M.; Jordan, S.; Lavender, T.; Neilson, J.P. Pain management for women in labour: An overview of systematic reviews. Cochrane Database Syst. Rev. 2012, 3, CD009234. [Google Scholar] [CrossRef]
- Safdar, B.; Greenberg, M.R. Applying the gender lens to emergency care: From bench to bedside. Acad. Emerg. Med. 2014, 21, 1325–1328. [Google Scholar] [CrossRef] [PubMed]
- Srajer, A.; Wylie, M.; Zaver, F.; Lonergan, K.; Brain, P.; Lang, E. Emergency physician gender is associated with early pregnancy loss management: A multisite retrospective cohort study. Emerg. Med. J. 2023, 40, 242–247. [Google Scholar] [CrossRef]
- Vidal Fuertes, C.; Johns, N.E.; Goodman, T.S.; Heidari, S.; Munro, J.; Hosseinpoor, A.R. The Association between Childhood Immunization and Gender Inequality: A Multi-Country Ecological Analysis of Zero-Dose DTP Prevalence and DTP3 Immunization Coverage. Vaccines 2022, 10, 1032. [Google Scholar] [CrossRef] [PubMed]
- Brucker, S.Y.; Simoes, E. Frauengesundheit. In Frauengesundheit—Frauenmedizin. Fachübergreifend und Kompakt; Brucker, S.Y., Doubek, K., Scharl, A., Simoes, E., Wallwiener, D., Eds.; Elsevier Verlag: München, Germany, 2023; pp. 1–18. [Google Scholar]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice); World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Miani, C.; Wandschneider, L.; Niemann, J.; Batram-Zantvoort, S.; Razum, O. Measurement of gender as a social determinant of health in epidemiology-A scoping review. PLoS ONE 2021, 16, e0259223. [Google Scholar] [CrossRef] [PubMed]
- Glezerman, M. Gender Medicine: The Groundbreaking New Science of Gender- and Sex-Based Diagnosis and Treatment; The Overlook Press: New York, NY, USA, 2016; p. 30. [Google Scholar]
- Oertelt-Prigione, S. Putting gender into sex- and gender-sensitive medicine. EClinicalMedicine 2020, 20, 100305. [Google Scholar] [CrossRef] [PubMed]
- Hankivsky, O. Women’s health, men’s health, and gender and health: Implications of intersectionality. Soc. Sci. Med. 2012, 74, 1712–1720. [Google Scholar] [CrossRef]
- Ohlmeier, C.; Mikolajczyk, R.; Frick, J.; Prütz, F.; Haverkamp, W.; Garbe, E. Incidence, prevalence and 1-year all-cause mortality of heart failure in Germany: A study based on electronic healthcare data of more than six million persons. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2015, 104, 688–696. [Google Scholar] [CrossRef]
- Keteepe-Arachi, T.; Sharma, S. Cardiovascular Disease in Women: Understanding Symptoms and Risk Factors. Eur. Cardiol. 2017, 12, 10–13. [Google Scholar] [CrossRef]
- Isorni, M.A.; Blanchard, D.; Teixeira, N.; le Breton, H.; Renault, N.; Gilard, M.; Lefèvre, T.; Mulak, G.; Danchin, N.; Spaulding, C.; et al. Impact of gender on use of revascularization in acute coronary syndromes: The national observational study of diagnostic and interventional cardiac catheterization (ONACI). Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2015, 86, E58–E65. [Google Scholar] [CrossRef]
- Baggio, G.; Corsini, A.; Floreani, A.; Giannini, S.; Zagonel, V. Gender medicine: A task for the third millennium. Clin. Chem. Lab. Med. 2013, 51, 713–727. [Google Scholar] [CrossRef] [PubMed]
- Schulte, K.J.; Mayrovitz, H.N. Myocardial Infarction Signs and Symptoms: Females vs. Males. Cureus 2023, 15, e37522. [Google Scholar] [CrossRef] [PubMed]
- Oertelt-Prigione, S.; Dalibert, L.; Verdonk, P.; Stutz, E.Z.; Klinge, I. Implementation Strategies for Gender-Sensitive Public Health Practice: A European Workshop. J. Womens Health 2017, 26, 1255–1261. [Google Scholar] [CrossRef] [PubMed]
- Lin, V.; L’Orange, H. Gender-sensitive Indicators for Healthcare. In The Palgrave Handbook of Gender and Healthcare; Kuhlmann, E., Annandale, E., Eds.; Palgrave Macmillan: London, UK, 2012; pp. 92–110. [Google Scholar]
- Graf, J. Prävention: Definitionen und Ansätze. In Frauengesundheit—Frauenmedizin. Fachübergreifend und Kompakt; Brucker, S.Y., Doubek, K., Scharl, A., Simoes, E., Wallwiener, D., Eds.; Elsevier Verlag: München, Germany, 2023; pp. 175–178. [Google Scholar]
- Buzer.de. § 20—Sozialgesetzbuch (SGB) Fünftes Buch (V)—Gesetzliche Krankenversicherung—(SGB V); Buzer: Falkensee, Germany, 2023; Available online: https://www.buzer.de/20_SGB_V.htm (accessed on 15 March 2023).
- Chen, E.H.; Shofer, F.S.; Dean, A.J.; Hollander, J.E.; Baxt, W.G.; Robey, J.L.; Sease, K.L.; Mills, A.M. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2008, 15, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Osborne, N.R.; Davis, K.D. Sex and gender differences in pain. Int. Rev. Neurobiol. 2022, 164, 277–307. [Google Scholar] [CrossRef] [PubMed]
- Fillingim, R.B.; King, C.D.; Ribeiro-Dasilva, M.C.; Rahim-Williams, B.; Riley, J.L., 3rd. Sex, gender, and pain: A review of recent clinical and experimental findings. J. Pain 2009, 10, 447–485. [Google Scholar] [CrossRef] [PubMed]
- Pieretti, S.; Di Giannuario, A.; Di Giovannandrea, R.; Marzoli, F.; Piccaro, G.; Minosi, P.; Aloisi, A.M. Gender differences in pain and its relief. Ann. Ist. Super. Sanita 2016, 52, 184–189. [Google Scholar] [CrossRef]
- Bartley, E.J.; Fillingim, R.B. Sex differences in pain: A brief review of clinical and experimental findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Goffaux, P.; Michaud, K.; Gaudreau, J.; Chalaye, P.; Rainville, P.; Marchand, S. Sex differences in perceived pain are affected by an anxious brain. Pain 2011, 152, 2065–2073. [Google Scholar] [CrossRef]
- Alabas, O.A.; Tashani, O.A.; Tabasam, G.; Johnson, M.I. Gender role affects experimental pain responses: A systematic review with meta-analysis. Eur. J. Pain 2012, 16, 1211–1223. [Google Scholar] [CrossRef]
- Lord, B.; Cui, J.; Kelly, A.M. The impact of patient sex on paramedic pain management in the prehospital setting. Am. J. Emerg. Med. 2009, 27, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, A.T.; Hollingshead, N.A.; Matthias, M.S.; Bair, M.J.; Kroenke, K. The influence of patient sex, provider sex, and sexist attitudes on pain treatment decisions. J. Pain 2014, 15, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, E.P.; Paganini, G.A.; ten Brinke, L. Gender Stereotypes Explain Disparities in Pain Care and Inform Equitable Policies. Policy Insights Behav. Brain Sci. 2020, 7, 198–204. [Google Scholar] [CrossRef]
- Yang, Y.; Carlin, A.S.; Faustino, P.J.; Motta, M.I.; Hamad, M.L.; He, R.; Watanuki, Y.; Pinnow, E.E.; Khan, M.A. Participation of women in clinical trials for new drugs approved by the food and drug administration in 2000-2002. J. Women’s Health 2009, 18, 303–310. [Google Scholar] [CrossRef]
- Fillingim, R.B.; Gear, R.W. Sex differences in opioid analgesia: Clinical and experimental findings. Eur. J. Pain 2004, 8, 413–425. [Google Scholar] [CrossRef]
- Guðmundsdóttir, E.Ý.; Nieuwenhuijze, M.; Einarsdóttir, K.; Hálfdánsdóttir, B.; Gottfreðsdóttir, H. Use of pain management in childbirth among migrant women in Iceland: A population-based cohort study. Birth 2022, 49, 486–496. [Google Scholar] [CrossRef]
- Fair, F.; Raben, L.; Watson, H.; Vivilaki, V.; van den Muijsenbergh, M.; Soltani, H.; ORAMMA Team. Migrant women’s experiences of pregnancy, childbirth and maternity care in European countries: A systematic review. PLoS ONE 2020, 15, e0228378. [Google Scholar] [CrossRef]
- Rubenson Wahlin, R.; Ponzer, S.; Lövbrand, H.; Skrivfars, M.; Lossius, H.M.; Castrén, M. Do male and female trauma patients receive the same prehospital care?: An observational follow-up study. BMC Emerg. Med. 2016, 16, 6. [Google Scholar] [CrossRef]
- Gomez, D.; Haas, B.; de Mestral, C.; Sharma, S.; Hsiao, M.; Zagorski, B.; Rubenfeld, G.; Ray, J.; Nathens, A.B. Gender-associated differences in access to trauma center care: A population-based analysis. Surgery 2012, 152, 179–185. [Google Scholar] [CrossRef]
- Borkhoff, C.M.; Hawker, G.A.; Kreder, H.J.; Glazier, R.H.; Mahomed, N.N.; Wright, J.G. The effect of patients’ sex on physicians’ recommendations for total knee arthroplasty. CMAJ Can. Med. Assoc. J. 2008, 178, 681–687. [Google Scholar] [CrossRef]
- Hentschel, T.; Heilman, M.E.; Peus, C.V. The Multiple Dimensions of Gender Stereotypes: A Current Look at Men’s and Women’s Characterizations of Others and Themselves. Front. Psychol. 2019, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Feykes, C.E. Geschlechterstereotype im Rettungsdienst: Resultate einer empirischen Erhebung. Rettungsdienst 2021, 44, 30–36. [Google Scholar]
- Michael, M.; Al Agha, S.; Böhm, L.; Bosse, H.M.; Pohle, A.N.; Schürmann, J.; Hannappel, O.; Tengg, E.; Weiß, C.; Bernhard, M. Alters- und geschlechtsbezogene Verteilung von Zuführung, Ersteinschätzung, Entlassart und Verweildauer in der zentralen Notaufnahme. Notf. Rett. 2023, 26, 39–48. [Google Scholar] [CrossRef]
- Sieverding, M.; Kendel, F. Gender (role) aspects in doctor–patient communication. Bundesgesundheitsbl 2012, 55, 1118–1124. [Google Scholar] [CrossRef] [PubMed]
- Melberg, T.; Kindervaag, B.; Rosland, J. Gender-specific ambulance priority and delays to primary percutaneous coronary intervention: A consequence of the patients’ presentation or the management at the emergency medical communications center? Am. Heart J. 2013, 166, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Macrae, C.N.; Milne, A.B.; Bodenhausen, G.V. Stereotypes as energy-saving devices: A peek inside the cognitive toolbox. J. Personal. Soc. Psychol. 1994, 66, 37–47. [Google Scholar] [CrossRef]
- Schoeneberg, C.; Kauther, M.D.; Hussmann, B.; Keitel, J.; Schmitz, D.; Lendemans, S. Gender-specific differences in severely injured patients between 2002 and 2011: Data analysis with matched-pair analysis. Crit. Care 2013, 17, R277. [Google Scholar] [CrossRef]
- Nutbeam, T.; Weekes, L.; Heidari, S.; Fenwick, R.; Bouamra, O.; Smith, J.; Stassen, W. Sex-disaggregated analysis of the injury patterns, outcome data and trapped status of major trauma patients injured in motor vehicle collisions: A prespecified analysis of the UK trauma registry (TARN). BMJ Open 2022, 12, e061076. [Google Scholar] [CrossRef]
- Sederholm Lawesson, S.; Isaksson, R.M.; Ericsson, M.; Ängerud, K.; Thylén, I.; SymTime Study Group. Gender disparities in first medical contact and delay in ST-elevation myocardial infarction: A prospective multicentre Swedish survey study. BMJ Open 2018, 8, e020211. [Google Scholar] [CrossRef]
- Graf, J. Impfungen. In Frauengesundheit—Frauenmedizin. Fachübergreifend und Kompakt; Brucker, S.Y., Doubek, K., Scharl, A., Simoes, E., Wallwiener, D., Eds.; Elsevier Verlag: München, Germany, 2023; pp. 207–208. [Google Scholar]
- Falcaro, M.; Castañon, A.; Ndlela, B.; Checchi, M.; Soldan, K.; Lopez-Bernal, J.; Elliss-Brookes, L.; Sasieni, P. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: A register-based observational study. Lancet 2021, 398, 2084–2092. [Google Scholar] [CrossRef]
- Hiller, J.; Schatz, K.; Drexler, H. Gender influence on health and risk behavior in primary prevention: A systematic review. Z. Gesundh. Wiss. 2017, 25, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, V.; Partha, G.; Karmakar, M. Gender differences in utilization of preventive care services in the United States. J. Womens Health 2012, 21, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Gamper, M.; Seidel, J.; Kupfer, A.; Keim-Klärner, S.; Klärner, A. Gender and Health Inequalities: Social Networks in the Context of Health and Health Behavior. In Social Networks and Health Inequalities; Klärner, A., Gamper, M., Keim-Klärner, S., Moor, I., von der Lippe, H., Vonneilich, N., Eds.; Springer VS: Wiesbaden, Germany, 2020; pp. 245–372. [Google Scholar]
- Poethko-Müller, C.; Schmitz, R. Vaccination coverage in German adults. Results of the German health interview and examination survey for adults (DEGS1). Bundesgesundheitsbl 2013, 56, 845–857. [Google Scholar] [CrossRef]
- Syan, S.K.; Gohari, M.R.; Levitt, E.E.; Belisario, K.; Gillard, J.; DeJesus, J.; MacKillop, J. COVID-19 Vaccine Perceptions and Differences by Sex, Age, and Education in 1,367 Community Adults in Ontario. Front. Public Health 2021, 9, 719665. [Google Scholar] [CrossRef] [PubMed]
- Herman, R.; McNutt, L.A.; Mehta, M.; Salmon, D.A.; Bednarczyk, R.A.; Shaw, J. Vaccination perspectives among adolescents and their desired role in the decision-making process. Hum. Vaccines Immunother. 2019, 15, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Corsi, D.J.; Bassani, D.G.; Kumar, R.; Awasthi, S.; Jotkar, R.; Kaur, N.; Jha, P. Gender inequity and age-appropriate immunization coverage in India from 1992 to 2006. BMC Int. Health Hum. Rights 2009, 9, S3. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Ceballo, R.; International COVID-19 Parental Attitude Study (COVIPAS) Group. Parental gender differences in attitudes and willingness to vaccinate against COVID-19. J. Paediatr. Child Health 2022, 58, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Grandahl, M.; Oscarsson, M.; Stenhammar, C.; Nevéus, T.; Westerling, R.; Tydén, T. Not the right time: Why parents refuse to let their daughters have the human papillomavirus vaccination. Acta Paediatr. 2014, 103, 436–441. [Google Scholar] [CrossRef]
- Flanagan, K.L.; Fink, A.L.; Plebanski, M.; Klein, S.L. Sex and Gender Differences in the Outcomes of Vaccination over the Life Course. Annu. Rev. Cell Dev. Biol. 2017, 33, 577–599. [Google Scholar] [CrossRef]
- Allison, M.A.; Dunne, E.F.; Markowitz, L.E.; O’Leary, S.T.; Crane, L.A.; Hurley, L.P.; Stokley, S.; Babbel, C.I.; Brtnikova, M.; Beaty, B.L.; et al. HPV vaccination of boys in primary care practices. Acad. Pediatr. 2013, 13, 466–474. [Google Scholar] [CrossRef]
- Schwartz, B.I.; Maccani, M.; Bansal, S.; Gannon, M. Parental perceptions of the HPV vaccine for prevention of anogenital and oropharyngeal cancers. Vaccine X 2023, 14, 100298. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Xu, L.; Simoens, C.; Martin-Hirsch, P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018, 5, CD009069. [Google Scholar] [CrossRef] [PubMed]
- Jensen, A.; Stromme, M.; Moyassari, S.; Chadha, A.S.; Tartaglia, M.C.; Szoeke, C.; Ferretti, M.T. COVID-19 vaccines: Considering sex differences in efficacy and safety. Contemp. Clin. Trials 2022, 115, 106700. [Google Scholar] [CrossRef] [PubMed]
- Trigunaite, A.; Dimo, J.; Jørgensen, T.N. Suppressive effects of androgens on the immune system. Cell. Immunol. 2015, 294, 87–94. [Google Scholar] [CrossRef]
- Fish, E.N. The X-files in immunity: Sex-based differences predispose immune responses. Nat. Rev. Immunol. 2008, 8, 737–744. [Google Scholar] [CrossRef]
- Fink, A.L.; Klein, S.L. Sex and Gender Impact Immune Responses to Vaccines Among the Elderly. Physiology 2015, 30, 408–416. [Google Scholar] [CrossRef]
- Klein, S.L.; Jedlicka, A.; Pekosz, A. The Xs and Y of immune responses to viral vaccines. Lancet Infect. Dis. 2010, 10, 338–349. [Google Scholar] [CrossRef]
- Simell, B.; Lahdenkari, M.; Reunanen, A.; Käyhty, H.; Väkeväinen, M. Effects of ageing and gender on naturally acquired antibodies to pneumococcal capsular polysaccharides and virulence-associated proteins. Clin. Vaccine Immunol. CVI 2008, 15, 1391–1397. [Google Scholar] [CrossRef]
- Su, J.R.; Moro, P.L.; Ng, C.S.; Lewis, P.W.; Said, M.A.; Cano, M.V. Anaphylaxis after vaccination reported to the Vaccine Adverse Event Reporting System, 1990-2016. J. Allergy Clin. Immunol. 2019, 143, 1465–1473. [Google Scholar] [CrossRef]
- Halsey, N.A.; Griffioen, M.; Dreskin, S.C.; Dekker, C.L.; Wood, R.; Sharma, D.; Jones, J.F.; LaRussa, P.S.; Garner, J.; Berger, M.; et al. Immediate hypersensitivity reactions following monovalent 2009 pandemic influenza A (H1N1) vaccines: Reports to VAERS. Vaccine 2013, 31, 6107–6112. [Google Scholar] [CrossRef]
- Gee, J.; Marquez, P.; Sum, J.; Calvert, G.M.; Liu, R.; Myers, T.; Nair, N.; Martin, S.; Clark, T.; Markowitz, L.; et al. First Month of COVID-19 Vaccine Safety Monitoring—United States, December 14, 2020-January 13, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Shimabukuro, T.T.; Cole, M.; Su, J.R. Reports of Anaphylaxis After Receipt of mRNA COVID-19 Vaccines in the US-December 14, 2020–January 18, 2021. JAMA 2021, 325, 1101–1102. [Google Scholar] [CrossRef] [PubMed]
- Mentzer, D.; Keller-Stanislawski, B. Verdachtsfälle von Nebenwirkungen oder Impfkomplikationen nach Impfung mit den Omikron-adaptierten bivalenten COVID-19-Impfstoffen Comirnaty Original/Omicron BA.1, Comirnaty Original/Omicron BA.4-5, Spikevax bivalent/Omicron BA.1 (bis 31.10.2022 in Deutschland gemeldet). Bull. Arzneim. 2022, 4, 29–34. [Google Scholar]
- Ciarambino, T.; Barbagelata, E.; Corbi, G.; Ambrosino, I.; Politi, C.; Lavalle, F.; Ruggieri, A.; Moretti, A. Gender differences in vaccine therapy: Where are we in COVID-19 pandemic? Monaldi Arch. Chest Dis. 2021, 91, 4. [Google Scholar] [CrossRef] [PubMed]
- Vassallo, A.; Shajahan, S.; Harris, K.; Hallam, L.; Hockham, C.; Womersley, K.; Woodward, M.; Sheel, M. Sex and Gender in COVID-19 Vaccine Research: Substantial Evidence Gaps Remain. Front. Glob. Women’s Health 2021, 2, 761511. [Google Scholar] [CrossRef] [PubMed]
- Ella, R.; Reddy, S.; Blackwelder, W.; Potdar, V.; Yadav, P.; Sarangi, V.; Aileni, V.K.; Kanungo, S.; Rai, S.; Reddy, P.; et al. Efficacy, safety, and lot-to-lot immunogenicity of an inactivated SARS-CoV-2 vaccine (BBV152): Interim results of a randomised, double-blind, controlled, phase 3 trial. Lancet 2021, 398, 2173–2184. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Future Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef]
- Wainwright, S.; Caskey, R.; Rodriguez, A.; Holicky, A.; Wagner-Schuman, M.; Glassgow, A.E. Screening fathers for postpartum depression in a maternal-child health clinic: A program evaluation in a midwest urban academic medical center. BMC Pregnancy Childbirth 2023, 23, 675. [Google Scholar] [CrossRef]
- Rovner, G.S.; Sunnerhagen, K.S.; Björkdahl, A.; Gerdle, B.; Börsbo, B.; Johansson, F.; Gillanders, D. Chronic pain and sex-differences; women accept and move, while men feel blue. PLoS ONE 2017, 12, e0175737. [Google Scholar] [CrossRef]
- Klimmer, M.M. Der Mann als Goldstandard? Gendereffekte in Medizin und Unfallforschung. Rettungsdienst 2021, 44, 12–18. [Google Scholar]
- Chang, C.H.; Yang, F. How Gender Stereotypes Impact Health Information Seeking Intention: Insights from an Implicit Association Test. Cogent Soc. Sci. 2021, 7, 1. [Google Scholar] [CrossRef]
- Stommel, W.; Plug, I.; Olde Hartman, T.C.; Lucassen, P.L.B.J.; van Dulmen, S.; Das, E. Gender stereotyping in medical interaction: A Membership Categorization Analysis. Patient Educ. Couns. 2022, 105, 3242–3248. [Google Scholar] [CrossRef] [PubMed]
- Bensing, J.M.; Kerssens, J.J.; van der Pasch, M. Patient-directed gaze as a tool for discover-ing and handling psychosocial problems in general practice. J. Nonverbal Behav. 2005, 19, 223–242. [Google Scholar] [CrossRef]
- Roter, D.L.; Hall, J.A.; Aoki, Y. Physician gender effects in medical communication. A meta-analytic review. JAMA 2002, 288, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Graf, J.; Smolka, R.; Simoes, E.; Zipfel, S.; Junne, F.; Holderried, F.; Wosnik, A.; Doherty, A.M.; Menzel, K.; Herrmann-Werner, A. Communication skills of medical students during the OSCE: Gender-specific differences in a longitudinal trend study. BMC Med. Educ. 2017, 17, 75. [Google Scholar] [CrossRef]
- United Nations Population Fund; International Confederation of Midwives; World Health Organization. State of the World’s Midwifery 2021; United Nations Population Fund: New York, NY, USA, 2021; Available online: https://www.un-ilibrary.org/content/books/9789214030935/read (accessed on 13 June 2023).
- Wortmann, L.; Haarmann, L.; Yeboah, A.; Kalbe, E. Gender medicine teaching increases medical students’ gender awareness: Results of a quantitative survey. GMS J. Med. Educ. 2023, 40, Doc45. [Google Scholar]
- Cirillo, D.; Catuara-Solarz, S.; Morey, C.; Guney, E.; Subirats, L.; Mellino, S.; Gigante, A.; Valencia, A.; Rementeria, M.J.; Chadha, A.S.; et al. Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. NPJ Digit. Med. 2020, 3, 81. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graf, J.; Simoes, E.; Kranz, A.; Weinert, K.; Abele, H. The Importance of Gender-Sensitive Health Care in the Context of Pain, Emergency and Vaccination: A Narrative Review. Int. J. Environ. Res. Public Health 2024, 21, 13. https://doi.org/10.3390/ijerph21010013
Graf J, Simoes E, Kranz A, Weinert K, Abele H. The Importance of Gender-Sensitive Health Care in the Context of Pain, Emergency and Vaccination: A Narrative Review. International Journal of Environmental Research and Public Health. 2024; 21(1):13. https://doi.org/10.3390/ijerph21010013
Chicago/Turabian StyleGraf, Joachim, Elisabeth Simoes, Angela Kranz, Konstanze Weinert, and Harald Abele. 2024. "The Importance of Gender-Sensitive Health Care in the Context of Pain, Emergency and Vaccination: A Narrative Review" International Journal of Environmental Research and Public Health 21, no. 1: 13. https://doi.org/10.3390/ijerph21010013




