Socioeconomic Determinants of Universal Health Coverage in the Asian Region
Abstract
:1. Introduction
2. Methods
2.1. Survey Design
2.2. Target Countries and Data
2.3. Analysis Method and Conditions
3. Results
3.1. Basic Statistical Analysis and Panel Data Analysis
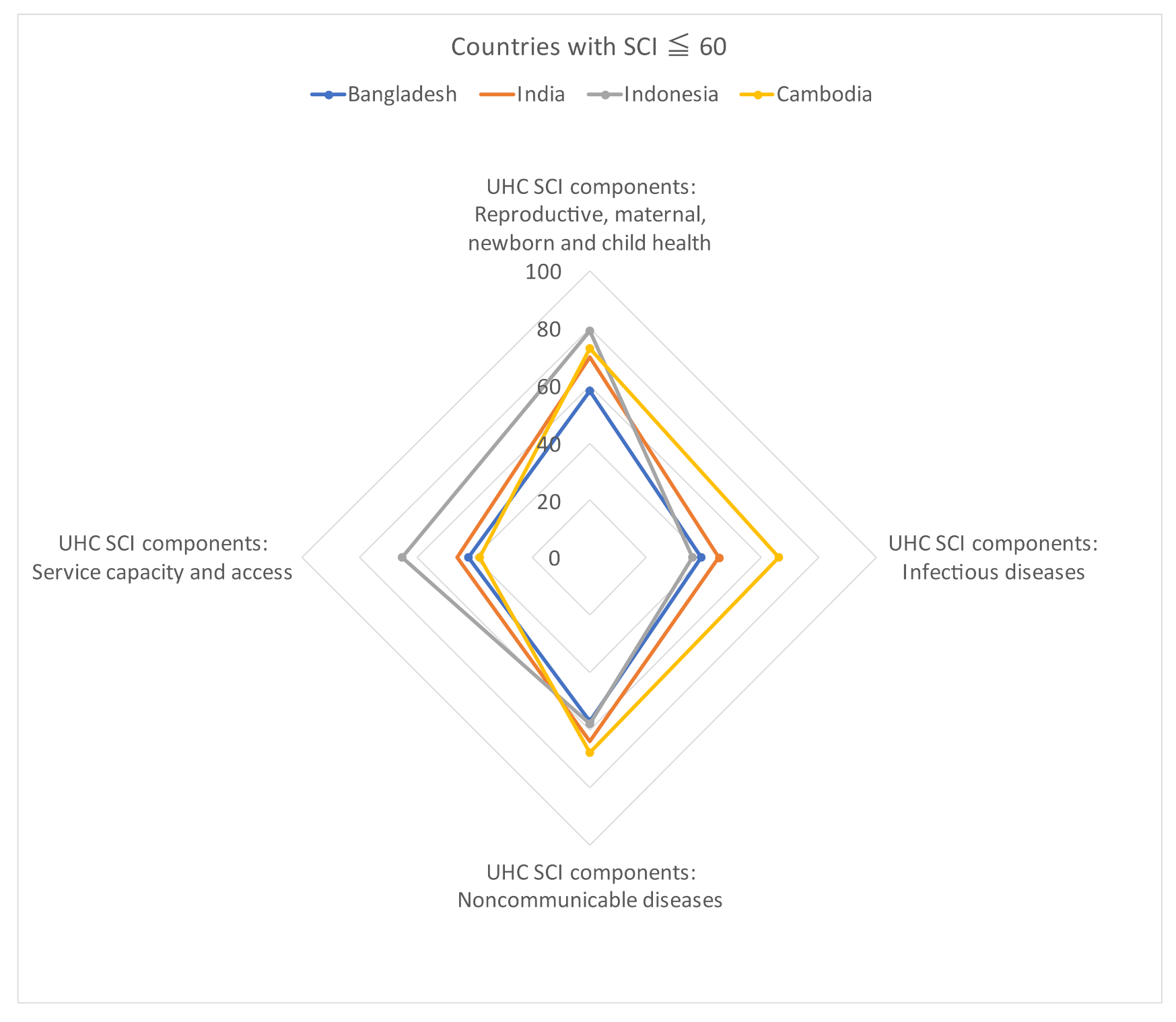
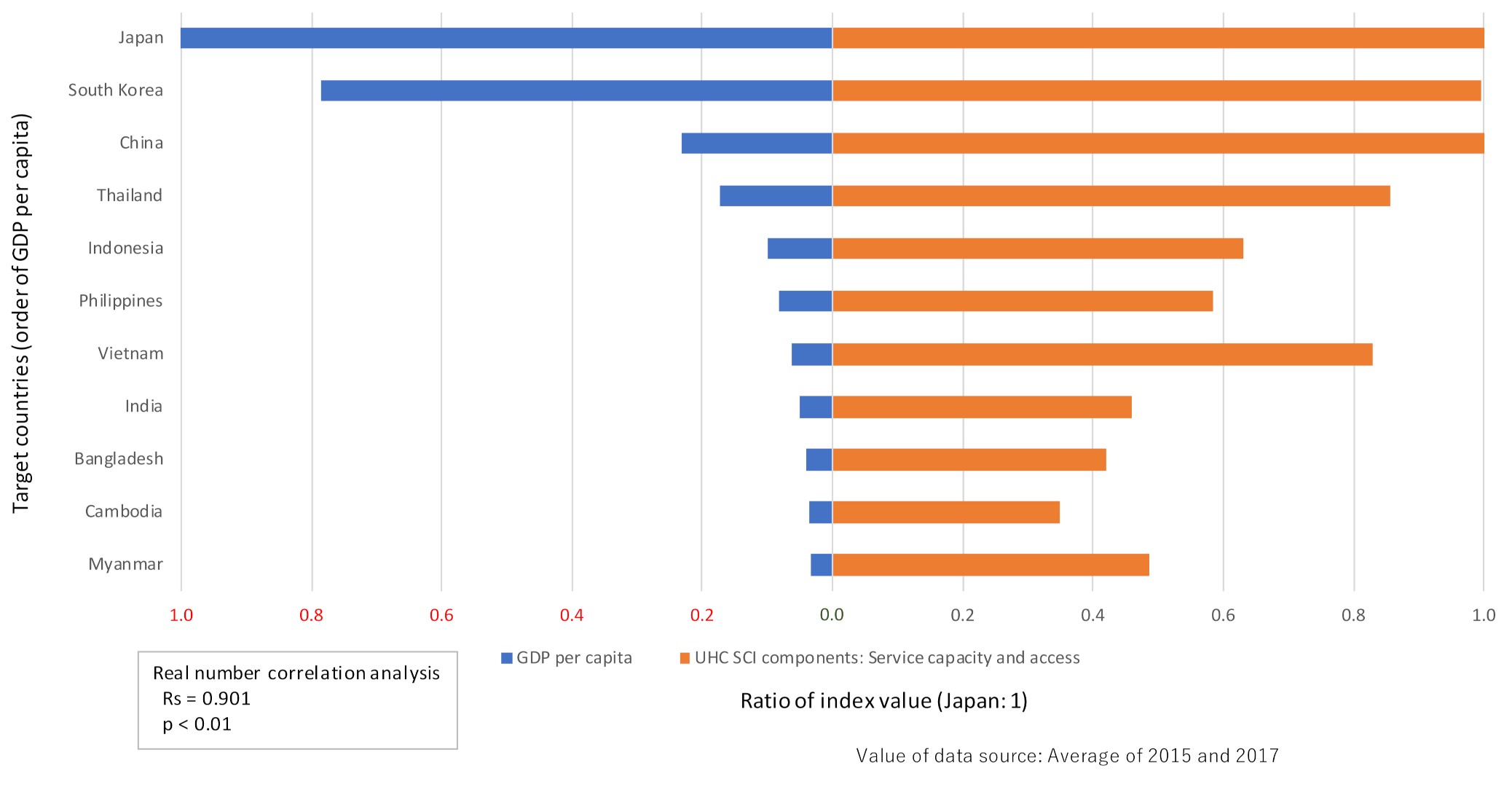
3.2. Multiple Regression Analysis of SCI Components
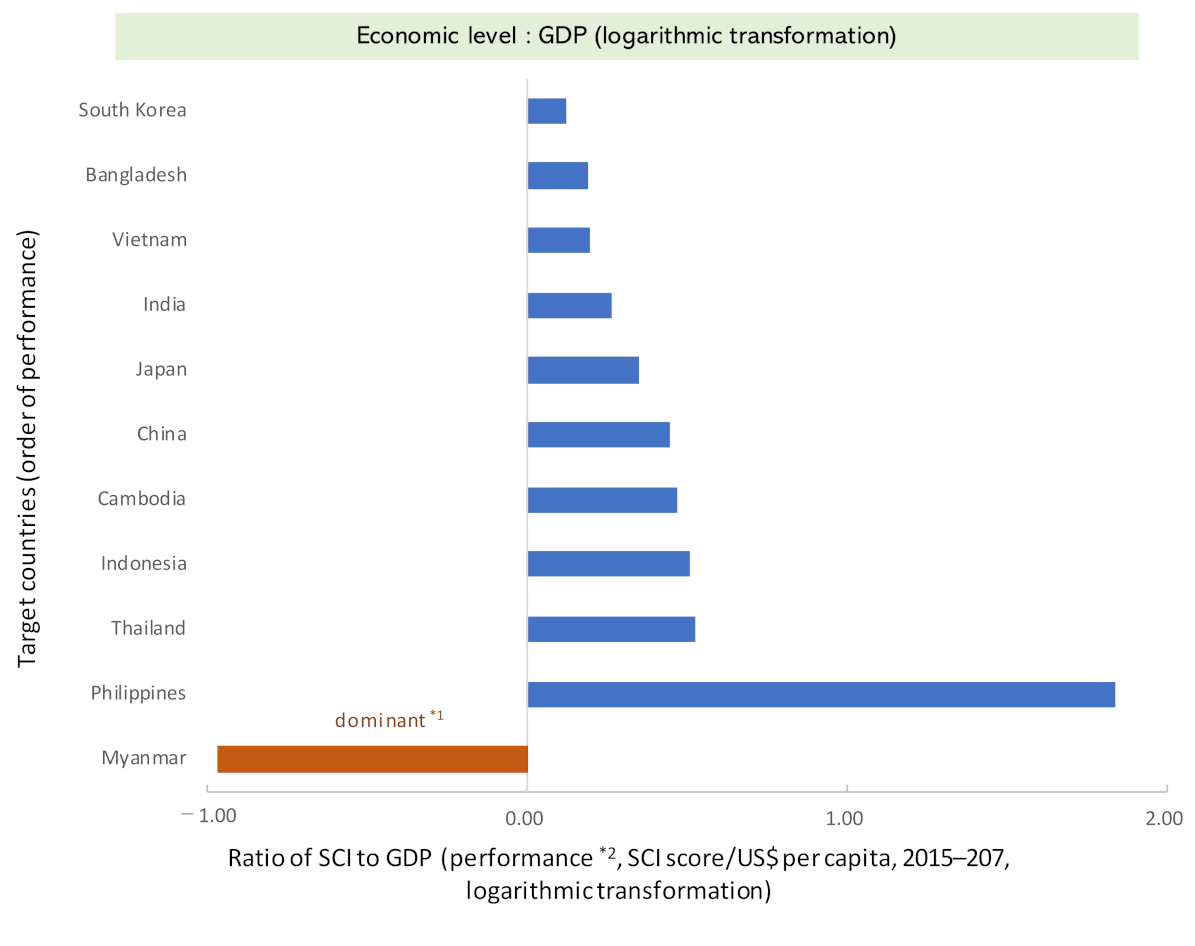
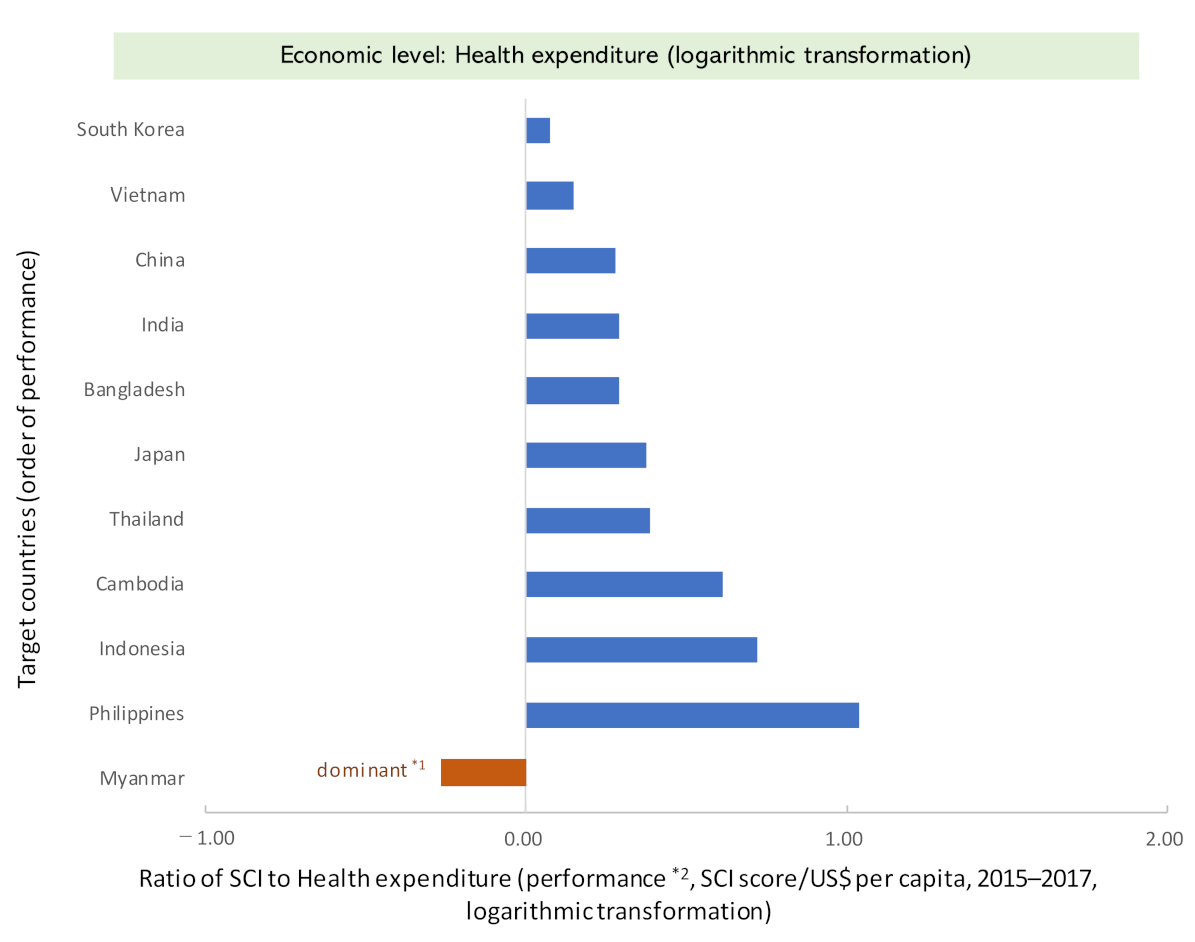
3.3. Performance Analysis—Outcome and Economy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Development Programme. What Are the Sustainable Development Goals? 2021. Available online: https://www.undp.org/sustainable-development-goals (accessed on 22 October 2021).
- World Health Organization. Sustainable Development Goals. 2020. Available online: https://www.afro.who.int/health-topics/sustainable-development-goals (accessed on 22 October 2021).
- United Nations. Resolution Adopted by the General Assembly on 6 July 2017, Work of the Statistical Commission Pertaining to the 2030 Agenda for Sustainable Development (A/RES/71/313 Archived 28 November 2020 at the Wayback Machine). 2017. Available online: https://undocs.org/A/RES/71/313 (accessed on 2 February 2022).
- United Nations. Resolution Adopted by the General Assembly on 25 September 2015, Transforming Our World: The 2030 Agenda for Sustainable Development (A/RES/70/1 Archived 28 November 2020 at the Wayback Machine). 2015. Available online: https://sdgs.un.org/2030agenda (accessed on 2 February 2022).
- World Health Organization. Tracking Universal Health Coverage. Global Monitoring Report. 2017. Available online: http://www.who.int/healthinfo/universal_health_coverage/report/2017/en/ (accessed on 22 October 2021).
- World Health Organization. Universal Health Coverage. 2021. Available online: https://www.who.int/westernpacific/health-topics/universal-health-coverag (accessed on 22 October 2021).
- World Health Organization. Monitoring Report. 2019. Available online: http://www.who.int/healthinfo/universal_health_coverage/report/2019/en/ (accessed on 22 October 2021).
- Rao, K.D.; Makimoto, S.; Peters, M.; Leung, G.M.; Bloom, G.; Katsuma, Y. Vulnerable populations and universal health coverage. In Leave No One Behind: Time for Specifics on the Sustainable Development Goals; Kharas, H., McArthur, J.W., Ohno, I., Eds.; Brookings Institution Press: Washington, DC, USA, 2019; pp. 129–148. [Google Scholar]
- UHC2030. Chapter 2: Core Content for Understanding UHC and Public Budgets for Health. 2021. Available online: https://www.uhc2030.org/what-we-do/voices/accountability/budget-toolkit/chapter-2-core-content-for-understanding-uhc-and-public-budgets-for-health/ (accessed on 22 October 2021).
- Eregata, G.T.; Hailu, A.; Memirie, S.T.; Norheim, O.F. Measuring progress towards universal health coverage: National and subnational Analysis in Ethiopia. BMJ Glob. Health 2019, 4, e001843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDonnell, A.; Urrutia, A.F.; Samman, E. Reaching Universal Health Coverage: A Political Economy Review of Trends Across 49 Countries [ODI Working Paper]; Overseas Development Institute: London, UK, 2019; pp. 1–34. Available online: https://cdn.odi.org/media/documents/200623_uhc_paper_final.pdf;570 (accessed on 2 February 2022).
- Mundy, L.; Trowman, R.; Kearney, B. Overcoming the barriers to achieving universal health care in the Asian region. Int. J. Technol. Assess. Health Care 2018, 34, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Reich, M.R.; Harris, J.; Ikegami, N.; Maeda, A.; Cashin, C.; Araujo, E.C.; Takemi, K.; Evans, T.G. Moving towards universal health coverage: Lessons from 11 country studies. Lancet 2016, 387, 811–816. [Google Scholar] [CrossRef]
- Aftab, W.; Siddiqui, F.J.; Tasic, H.; Perveen, S.; Siddiqi, S.; Bhutta, Z.A. Implementation of health and health-related sustainable development goals: Progress, challenges and opportunities—A systematic literature review. BMJ Glob. Health 2020, 5, e002273. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, A.B.; Amor, S.H.; Ayadi, I.; Khelil, M.; Zoghlami, C.; Abdelfattah, S.B. Financing health care in Tunisia. Current state of health care expenditure and socialization prospects, on the road to Universal Health Coverage. Tunis. Med. 2018, 96, 789–807. [Google Scholar]
- Ergo, A.; Htoo, T.S.; Badiani-Magnusson, R.; Royono, R. A new hope: From neglect of the health sector to aspirations for Universal Health Coverage in Myanmar. Health Policy Plan. 2019, 34 (Suppl. S1), i38–i46. [Google Scholar] [CrossRef]
- Khan, J.A.M.; Ahmed, S.; Evans, T.G. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh—An estimation of financial risk protection of universal health coverage. Health Policy Plan. 2017, 32, 1102–1110. [Google Scholar] [CrossRef] [Green Version]
- Verguet, S.; Jamison, D.T.; Gelband, H.; Horton, S.; Jha, P.; Laxminarayan, R.; Mock, C.N.; Nugent, R. Health Policy Analysis: Applications of Extended Cost-Effectiveness Analysis Methodology in Disease Control Priorities, 3rd ed.; World Bank Group eLibrary: Washington, DC, USA, 2017; Chapter 8. [Google Scholar] [CrossRef]
- Global Burden of Disease Health Financing Collaborator Network. Trends in future health financing and coverage: Future health spending and universal health coverage in 188 countries. Lancet 2018, 391, 1783–1798. [Google Scholar] [CrossRef] [Green Version]
- The World Bank Group. World Bank Open Data. 2021. Available online: https://data.worldbank.org (accessed on 22 October 2021).
- World Health Organization. UHC Index of Service Coverage (SCI). 2021. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/uhc-index-of-service-coverage (accessed on 22 October 2021).
- World Health Organization. The Global Health Observatory. 2022. Available online: https://www.who.int/data/gho (accessed on 22 June 2021).
- Folayan, M.O.; Tantawi, M.E.; Virtanen, J.I.; Feldens, C.A.; Rashwan, M.; Kemoli, A.M.; Villena, R.; Al-Batayneh, O.B.; Amalia, R.; Gaffar, B.; et al. An ecological study on the association between universal health service coverage index, health expenditures, and early childhood caries. BMC Oral Health 2021, 21, 126. [Google Scholar] [CrossRef]
- Vaisey, S.; Miles, A. What You Can—And Can’t—Do with Three-Wave Panel Data. Sociol. Methods Res. 2017, 46, 44–67. [Google Scholar] [CrossRef] [Green Version]
- Chen, G.; Peirce, V.; Marsh, W. Evaluation of the national institute for health and care excellence diagnostics assessment program decisions: Incremental cost-effectiveness ratio thresholds and decision-modifying factors. Value Health 2020, 23, 1300–1306. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Torrance, G.W.; Claxton, K.; Stoddart, G.L. Methods for the Economic Evaluation of Health Care Programmes, 3rd ed.; Oxford University Press: London, UK, 2005. [Google Scholar]
- Asian Development Bank. Country Poverty Analysis: Cambodia; Publication Stock No. RPS114209; Asian Development Bank: Mandaluyong, Philippines, 2012; ISBN 978-92-9092-539-2. Available online: www.adb.org (accessed on 2 February 2022).
- Kassai, R.; van Weel, C.; Flegg, K.; Tong, S.F.; Han, T.M.; Noknoy, S.; Dashtseren, M.; Le An, P.; Ng, C.J.; Khoo, E.M.; et al. Priorities for primary health care policy implementation: Recommendations from the combined experience of six countries in the Asia-Pacific. Aust. J. Prim. Health 2020, 26, 351–357. [Google Scholar] [CrossRef]
- Malhotra, R.; Bautista, M.A.C.; Müller, A.M.; Aw, S.; Koh, G.C.H.; Theng, Y.L.; Hoskins, S.J.; Wong, C.H.; Miao, C.; Lim, W.S.; et al. The aging of a young nation: Population aging in Singapore. Gerontologist 2019, 59, 401–410. [Google Scholar] [CrossRef]
- Laranjeira, E.; Szrek, H. Going beyond life expectancy in assessments of health systems’ performance: Life expectancy adjusted by perceived health status. Int. J. Health Econ. Manag. 2016, 16, 133–161. [Google Scholar] [CrossRef]
- Moon, S.; Shin, J. Performance of universal health insurance: Lessons from South Korea. World Health Popul. 2007, 9, 95–113. [Google Scholar] [CrossRef]
- Romaniuk, P.; Poznańska, A.; Brukało, K.; Holecki, T. Health system outcomes in BRICS countries and their association with the economic context. Front. Public Health 2020, 8, 80. [Google Scholar] [CrossRef]
- Takura, T. An evaluation of clinical economics and cases of cost-effectiveness. Intern. Med. 2018, 57, 1191–1200. [Google Scholar] [CrossRef] [Green Version]
- Tambor, M.; Klich, J.; Domagała, A. Financing healthcare in central and eastern European countries: How far are we from universal health coverage? Int. J. Environ. Res. Public Health 2021, 18, 1382. [Google Scholar] [CrossRef]
- Van Minh, H.; Pocock, N.S.; Chaiyakunapruk, N.; Chhorvann, C.; Duc, H.A.; Hanvoravongchai, P.; Lim, J.; Lucero-Prisno, D.E.; Ng, N.; Phaholyothin, N.; et al. Progress toward universal health coverage in ASEAN. Glob. Health Action 2014, 7, 25856. [Google Scholar] [CrossRef] [Green Version]
- Feng, C.; Wang, H.; Lu, N.; Chen, T.; He, H.; Lu, Y.; Tu, X.M. Log-transformation and its implications for data analysis. Shanghai Arch. Psychiatry 2014, 26, 105–109. [Google Scholar] [CrossRef]
- Otto, R.; Ferguson, M.R.; Marro, K.; Grinstead, J.W.; Friedman, S.D. Limitations of using logarithmic transformation and linear fitting to estimate relaxation rates in iron-loaded liver. Pediatr. Rad. 2011, 41, 1259–1265. [Google Scholar] [CrossRef]
- Templin, T.; Dieleman, J.L.; Wigley, S.; Mumford, J.E.; Miller-Petrie, M.; Kiernan, S.; Bollyky, T.J. Democracies linked to greater universal health coverage compared with autocracies, even in an economic recession. Health Aff. 2021, 40, 1234–1242. [Google Scholar] [CrossRef]
- Henke, K.D. The Economic and the Health Dividend of the Health Care System, Vital Transformation; Health Forum: Vilnius, Lithuania, 2013; Available online: https://vitaltransformation.com/sustainablehealth/pdfs/presentations/Klaus-Dirk%20Henke.pdf (accessed on 22 October 2021).
- Yamada, G.; Imanaka, Y. Input–output analysis on the economic impact of medical care in Japan. Environ. Health Prev. Med. 2015, 20, 379–387. [Google Scholar] [CrossRef] [Green Version]
- Prinja, S.; Gupta, R.; Bahuguna, P.; Sharma, A.; Kumar Aggarwal, A.; Phogat, A.; Kumar, R. A composite indicator to measure universal health care coverage in India: Way forward for post-2015 health system performance monitoring framework. Health Policy Plan. 2017, 32, 43–56. [Google Scholar] [CrossRef] [Green Version]





| Country | World Bank Country Income Group | Population (Total) | Population Aged 65 and Above | GDP Per Capita | Health Expenditure † | |
|---|---|---|---|---|---|---|
| Population > 50 Million People | (Million People) | (% of Total Population) | (Current USD) | (% of GDP) | ||
| Bangladesh | LMIC | 160 | 5.1 | 1406 | 2.4 | |
| Cambodia | LMIC | 15 | 4.4 | 1326 | 6.1 | |
| China | UMIC | 1399 | 10.3 | 8397 | 5.0 | |
| India | LMIC | 1344 | 6.0 | 1793 | 3.6 | |
| Indonesia | UMIC | 263 | 5.7 | 3627 | 2.9 | |
| Japan | HIC | 126 | 27.1 | 36,954 | 10.8 | |
| South Korea | HIC | 51 | 13.5 | 30,169 | 6.9 | |
| Myanmar | LMIC | 52 | 5.6 | 1200 | 5.3 | |
| Philippines | LMIC | 105 | 4.9 | 3096 | 4.4 | |
| Thailand | UMIC | 69 | 11.4 | 6217 | 3.8 | |
| Vietnam | LMIC | 95 | 7.0 | 2770 | 5.8 | |
| Country | Government health expenditures | Unemployment rate | Poverty rate †† | UHC index of service coverage (SCI) | ||
| Population > 50 million people | (% of general government expenditures) | (%: ratio of unemployed persons to the labor force) | (%: poverty gap, the default poverty line is $1.90 PPP/day) | Consists of four indicators | ||
| Bangladesh | 3.2 | 4.4 | 2.3 | 47.0 | ||
| Cambodia | 6.7 | 0.4 | 6.0 | 57.5 | ||
| China | 9.2 | 4.0 | 0.1 | 77.5 | ||
| India | 3.4 | 5.5 | 2.2 | 53.5 | ||
| Indonesia | 7.4 | 5.7 | 0.8 | 55.0 | ||
| Japan | 23.8 | 3.2 | 0.2 | 81.5 | ||
| South Korea | 4.3 | 1.2 | 0.7 | 85.5 | ||
| Myanmar | 8.0 | 6.3 | 1.2 | 60.0 | ||
| Philippines | 13.1 | 3.6 | 0.1 | 59.0 | ||
| Thailand | 14.6 | 1.0 | 0.0 | 77.5 | ||
| Vietnam | 9.0 | 2.2 | 0.4 | 74.0 | ||
| UHC Index of Service Coverage (SCI) | Partial Regression Coefficient | Standardized Partial Regression Coefficient | S.E. | p-Value | 95% CI |
|---|---|---|---|---|---|
| Population (total: million people) | 0.0049 | 0.1921 | 0.0012 | 0.0001 | 0.0025–0.0074 |
| GDP per capita (current USD) | 0.0017 | 1.6129 | 0.0002 | <0.001 | 0.0013–0.0021 |
| Health expenditure (% of GDP) | 2.3481 | 0.4116 | 1.5748 | 0.136 | −0.7386–5.4347 |
| Government health expenditures (% of general government expenditures) | 1.4511 | 0.6575 | 0.2804 | <0.001 | 0.9015–2.0006 |
| Unemployment rate (%: ratio of unemployed persons) | −1.4764 | −0.2253 | 0.7105 | 0.0377 | −2.8689–−0.0838 |
| Poverty rate (%: poverty gap) | −1.6736 | −0.2303 | 0.4674 | 0.0003 | −2.5897–−0.7575 |
| Model: R2 = 0.991, F test: p < 0.001 | |||||
| UHC Index of Service Coverage (SCI) | Partial Regression Coefficient | Standardized Partial Regression Coefficient | VIF | p-Value | 95% CI |
|---|---|---|---|---|---|
| UHC SCI components: Reproductive, maternal, newborn and child health | 0.5336 | 0.4370 | 1.4083 | 0.0001 | 0.3826–0.6846 |
| UHC SCI components: Infectious diseases | 0.1908 | 0.6303 | 3.2725 | 0.0002 | 0.1337–0.2478 |
| UHC SCI components: Noncommunicable diseases | 0.3701 | 0.1677 | 3.4415 | 0.0780 | −0.0566–0.7968 |
| UHC SCI components: Service capacity and access | 0.3581 | 0.9209 | 1.1719 | 0.0000 | 0.3142–0.4019 |
| Constant term | 0.0028 | 0.5974 | −0.0095–0.0151 | ||
| Model: p < 0.01 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takura, T.; Miura, H. Socioeconomic Determinants of Universal Health Coverage in the Asian Region. Int. J. Environ. Res. Public Health 2022, 19, 2376. https://doi.org/10.3390/ijerph19042376
Takura T, Miura H. Socioeconomic Determinants of Universal Health Coverage in the Asian Region. International Journal of Environmental Research and Public Health. 2022; 19(4):2376. https://doi.org/10.3390/ijerph19042376
Chicago/Turabian StyleTakura, Tomoyuki, and Hiroko Miura. 2022. "Socioeconomic Determinants of Universal Health Coverage in the Asian Region" International Journal of Environmental Research and Public Health 19, no. 4: 2376. https://doi.org/10.3390/ijerph19042376






