Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Survey Items
2.3. Analysis
2.4. Health Literacy Score
3. Results
3.1. Sample Characteristics
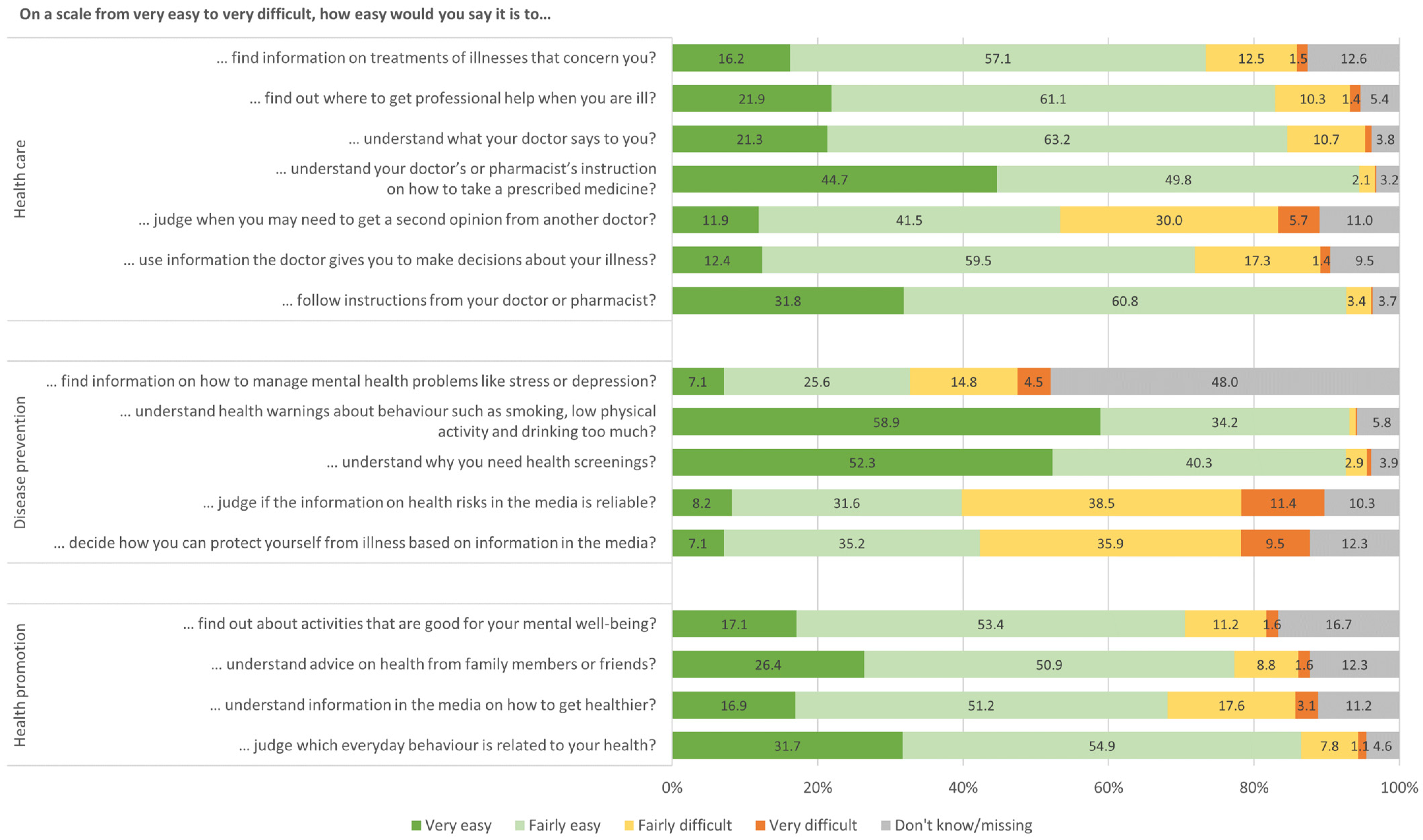
3.2. Results of the HLS-EU-Q16 Items
3.3. Health Literacy Levels and Subgroup Differences by Socioeconomic and Health Characteristics
3.4. Health System Performance Assessment according to Health Literacy Levels
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rademakers, J.; Heijmans, M. Beyond Reading and Understanding: Health Literacy as the Capacity to Act. Int. J. Environ. Res. Public Health 2018, 15, 1676. [Google Scholar] [CrossRef] [Green Version]
- Sørensen, K.; van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.; Wang, D.; Liu, C.; Jiang, J.; Wang, X.; Chen, H.; Ju, X.; Zhang, X. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam. Med. Community Health 2020, 8, 2. [Google Scholar] [CrossRef]
- Adriaenssens, J.; Rondia, K.; van den Broucke, S.; Kohn, L. Health literacy: What lessons can be learned from the experiences and policies of different countries? Int. J. Health Plann. Manag. 2021, 37, 886–901. [Google Scholar] [CrossRef] [PubMed]
- Schyve, P.M. Language differences as a barrier to quality and safety in health care: The Joint Commission perspective. J. Gen. Intern. Med. 2007, 22 (Suppl. S2), 360–361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dukić, N.; Blecich, A.A.; Cerović, L. Economic Implications of Insufficient Health Literacy. Econ. Res. Ekon. Istraživanja 2013, 26, 117–132. [Google Scholar] [CrossRef]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [Green Version]
- Schaeffer, D.; Berens, E.-M.; Vogt, D. Health Literacy in the German Population. Dtsch. Ärzteblatt Int. 2017, 114, 53–60. [Google Scholar] [CrossRef] [Green Version]
- Baumeister, A.; Chakraverty, D.; Aldin, A.; Seven, Ü.S.; Skoetz, N.; Kalbe, E.; Woopen, C. “The system has to be health literate, too”—Perspectives among healthcare professionals on health literacy in transcultural treatment settings. BMC Health Serv. Res. 2021, 21, 716. [Google Scholar] [CrossRef]
- Sentell, T.; Pitt, R.; Buchthal, O.V. Health Literacy in a Social Context: Review of Quantitative Evidence. Health Lit. Res. Pract. 2017, 1, e41–e70. [Google Scholar] [CrossRef]
- Blümel, M.; Spranger, A.; Achstetter, K.; Maresso, A.; Busse, R. Germany: Health system review. Health Syst. Transit. 2020, 22, i-273. [Google Scholar]
- Stauder, J.; Kossow, T. Selektion oder bessere Leistungen—Warum sind Privatversicherte gesünder als gesetzlich Versicherte? Gesundheitswesen 2017, 79, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, F.; Koller, D. Verschiedene Regionen, verschiedene Versichertenpopulationen? Soziodemografische und gesundheitsbezogene Unterschiede zwischen Krankenkassen. Gesundheitswesen 2017, 79, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Huber, J.; Mielck, A. Morbidität und Gesundheitsversorgung bei GKV- und PKV-Versicherten: Forschungsstand empirischer Studien. Bundesgesundheitsblatt Gesundh. Gesundh. 2010, 53, 925–938. [Google Scholar] [CrossRef]
- Hoffmann, F.; Icks, A. Unterschiede in der Versichertenstruktur von Krankenkassen und deren Auswirkungen für die Versorgungsforschung: Ergebnisse des Bertelsmann-Gesundheitsmonitors. Gesundheitswesen 2012, 74, 291–297. [Google Scholar] [CrossRef]
- Baccolini, V.; Rosso, A.; Di Paolo, C.; Isonne, C.; Salerno, C.; Migliara, G.; Prencipe, G.P.; Massimi, A.; Marzuillo, C.; de Vito, C.; et al. What is the Prevalence of Low Health Literacy in European Union Member States? A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 36, 753–761. [Google Scholar] [CrossRef]
- MacLeod, S.; Musich, S.; Gulyas, S.; Cheng, Y.; Tkatch, R.; Cempellin, D.; Bhattarai, G.R.; Hawkins, K.; Yeh, C.S. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr. Nurs. 2017, 38, 334–341. [Google Scholar] [CrossRef]
- Hayran, O.; Özer, O. Organizational health literacy as a determinant of patient satisfaction. Public Health 2018, 163, 20–26. [Google Scholar] [CrossRef]
- Altin, S.V.; Stock, S. The impact of health literacy, patient-centered communication and shared decision-making on patients’ satisfaction with care received in German primary care practices. BMC Health Serv. Res. 2016, 16, 450. [Google Scholar] [CrossRef] [Green Version]
- Papanicolas, I.; Smith, P. Health System Performance Comparison: An Agenda for Policy, Information and Research; Open University Press: Maidenhead, UK, 2013; ISBN 9780335247264. [Google Scholar]
- World Health Organization. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action, 2007. Available online: https://apps.who.int/iris/handle/10665/43918 (accessed on 31 October 2022).
- World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies; World Health Organization: Geneva, Switzerland, 2010; ISBN 9789241564052. [Google Scholar]
- Smith, P.C. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects; Cambridge University Press: Cambridge, UK, 2010; ISBN 9780521116763. [Google Scholar]
- World Health Organization. Regional Office for Europe. The Tallinn Charter: Health Systems for Health and Wealth WHO/EURO:2008-4229-43988-62011. 2021. Available online: https://apps.who.int/iris/handle/10665/349648 (accessed on 31 October 2022).
- Jürges, H. Health Insurance Status and Physician Behavior in Germany. Schmollers Jahrb. 2009, 129, 297–307. [Google Scholar] [CrossRef]
- Blümel, M.; Röttger, J.; Köppen, J.; Achstetter, K.; Busse, R. Integrating the Population Perspective into Health System Performance Assessment (IPHA): Study Protocol for a Cross-Sectional Study in Germany Linking Survey and Claims Data of Statutorily and Privately Insured. Int. J. Health Policy Manag. 2020, 9, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Achstetter, K.; Blümel, M.; Köppen, J.; Hengel, P.; Busse, R. Assessment of health system performance in Germany: Survey-based insights into the perspective of people with private health insurance. Int. J. Health Plann. Manag. 2022, 37, 3103–3125. [Google Scholar] [CrossRef] [PubMed]
- Statistisches Bundesamt. Angaben zur Krankenversicherung (Ergebnisse des Mikrozensus)—Fachserie 13 Reihe 1.1 2015. Statistisches Bundesamt: Wiesbaden, Germany, 2016; Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Gesundheitszustand-Relevantes-Verhalten/Publikationen/Downloads-Gesundheitszustand/krankenversicherung-mikrozensus-2130110159004.pdf?__blob=publicationFile (accessed on 31 October 2022).
- Verband der Privaten Krankenversicherungen e.V. Zahlenbericht der privaten Krankenversicherung, 2015; Verband der Privaten Krankenversicherung e.V.: Köln, Germany, 2016. [Google Scholar]
- Röttger, J.; Blümel, M.; Engel, S.; Grenz-Farenholtz, B.; Fuchs, S.; Linder, R.; Verheyen, F.; Busse, R. Exploring Health System Responsiveness in Ambulatory Care and Disease Management and its Relation to Other Dimensions of Health System Performance (RAC)—Study Design and Methodology. Int. J. Health Policy Manag. 2015, 4, 431–437. [Google Scholar] [CrossRef] [Green Version]
- Jordan, S.; Hoebel, J. Gesundheitskompetenz von Erwachsenen in Deutschland: Ergebnisse der Studie „Gesundheit in Deutschland aktuell“ (GEDA). Bundesgesundheitsblatt Gesundh. Gesundh. 2015, 58, 942–950. [Google Scholar] [CrossRef] [PubMed]
- Röthlin, F.; Pelikan, J.M.; Ganahl, K. Die Gesundheitskompetenz der 15-jährigen Jugendlichen in Österreich. Abschlussbericht der österreichischen Gesundheitskompetenz Jugendstudie im Auftrag des Hauptverbands der Österreichischen Sozialversicherungsträger (HVSV), Wien, 2013. Available online: https://www.sozialversicherung.at/cdscontent/load?contentid=10008.715507 (accessed on 31 October 2022).
- Dahlman, D.; Ekefäll, M.; Garpenhag, L. Health Literacy among Swedish Patients in Opioid Substitution Treatment: A Mixed-Methods Study. Drug Alcohol Depend. 2020, 214, 108186. [Google Scholar] [CrossRef] [PubMed]
- Statistisches Bundesamt. Lebensbedingungen in Deutschland und der Europäischen Union—Fachserie 15 Reihe 3—2018; Statistisches Bundesamt, Wiesbaden, Germany, 2020. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Einkommen-Konsum-Lebensbedingungen/Lebensbedingungen-Armutsgefaehr-dung/Publikationen/Downloads-Lebensbedingungen/einkommen-lebensbedingungen-2150300187004.pdf?__blob=publicationFile (accessed on 31 October 2022).
- Ehmann, A.T.; Groene, O.; Rieger, M.A.; Siegel, A. The Relationship between Health Literacy, Quality of Life, and Subjective Health: Results of a Cross-Sectional Study in a Rural Region in Germany. Int. J. Environ. Res. Public Health 2020, 17, 1683. [Google Scholar] [CrossRef] [Green Version]
- Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health literacy: Report of the Council on Scientific Affairs. JAMA 1999, 281, 552–557. [Google Scholar] [CrossRef]
- Levin-Zamir, D.; Baron-Epel, O.B.; Cohen, V.; Elhayany, A. The Association of Health Literacy with Health Behavior, Socioeconomic Indicators, and Self-Assessed Health From a National Adult Survey in Israel. J. Health Commun. 2016, 21, 61–68. [Google Scholar] [CrossRef]
- Eichler, K.; Wieser, S.; Brügger, U. The costs of limited health literacy: A systematic review. Int. J. Public Health 2009, 54, 313–324. [Google Scholar] [CrossRef] [Green Version]
- Levy, H.; Janke, A. Health Literacy and Access to Care. J. Health Commun. 2016, 21 (Suppl. S1), 43–50. [Google Scholar] [CrossRef] [Green Version]
- Gemeinsamer Bundesausschuss. Qualitätsberichte der Krankenhäuser. Available online: https://www.g-ba.de/themen/qualitaetssicherung/datenerhebung-zur-qualitaetssicherung/datenerhebung-qualitaetsbericht/ (accessed on 28 October 2022).
- Lyles, C.R.; Karter, A.J.; Young, B.A.; Spigner, C.; Grembowski, D.; Schillinger, D.; Adler, N.E. Correlates of patient-reported racial/ethnic health care discrimination in the Diabetes Study of Northern California (DISTANCE). J. Health Care Poor Underserved 2011, 22, 211–225. [Google Scholar] [CrossRef] [PubMed]
- Vamos, S.; Okan, O.; Sentell, T.; Rootman, I. Making a Case for "Education for Health Literacy": An International Perspective. Int. J. Environ. Res. Public Health 2020, 17, 1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griese, L.; Berens, E.-M.; Nowak, P.; Pelikan, J.M.; Schaeffer, D. Challenges in Navigating the Health Care System: Development of an Instrument Measuring Navigation Health Literacy. Int. J. Environ. Res. Public Health 2020, 17, 5731. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Levin-Zamir, D.; Duong, T.V.; Okan, O.; Brasil, V.V.; Nutbeam, D. Building health literacy system capacity: A framework for health literate systems. Health Promot. Int. 2021, 36, i13–i23. [Google Scholar] [CrossRef]
- Güner, M.D.; Ekmekci, P.E. A Survey Study Evaluating and Comparing the Health Literacy Knowledge and Communication Skills Used by Nurses and Physicians. Inq. A J. Med. Care Organ. Provis. Financ. 2019, 56, 46958019865831. [Google Scholar] [CrossRef]
| Health Literacy Score Available a | ||||||
|---|---|---|---|---|---|---|
| Total | Yes | No | ||||
| n | % | n | % | n | % | |
| Total | 3601 | 100 | 2801 | 77.8 | 800 | 22.2 |
| Gender (n = 3589) | ||||||
| Male | 2323 | 64.7 | 1806 | 64.7 | 517 | 64.9 |
| Female | 1266 | 35.3 | 986 | 35.3 | 280 | 35.1 |
| Age (years) (n = 3588) | ||||||
| Mean (SD) b | 58.5 (14.6) | 57.8 (14.3) | 60.0 (15.6) | |||
| 18–34 | 307 | 8.6 | 243 | 8.7 | 64 | 8.0 |
| 35–49 | 637 | 17.8 | 509 | 18.2 | 128 | 16.1 |
| 50–64 | 1220 | 34.0 | 999 | 35.8 | 221 | 27.8 |
| 65–74 | 928 | 25.9 | 717 | 25.7 | 211 | 26.5 |
| 75+ | 496 | 13.8 | 324 | 11.6 | 172 | 21.6 |
| Educational level (n = 3572) | ||||||
| Low (ISCED 0–1) | 57 | 1.6 | 39 | 1.4 | 18 | 2.3 |
| Medium (ISCED 2–4) | 641 | 17.9 | 481 | 17.3 | 160 | 20.3 |
| High (ISCED 5–8) | 2874 | 80.5 | 2264 | 81.3 | 610 | 77.4 |
| Work status (n = 3560) | ||||||
| Full-time | 1578 | 44.3 | 1274 | 45.8 | 304 | 39.1 |
| Part-time | 315 | 8.8 | 257 | 9.2 | 58 | 7.5 |
| Retired | 1431 | 40.2 | 1068 | 38.4 | 363 | 46.7 |
| Other (student, parental leave, unemployed, etc.) | 236 | 6.6 | 183 | 6.6 | 53 | 6.8 |
| Monthly net equivalent income c (n = 3399) | ||||||
| Up to €1136 | 81 | 2.4 | 62 | 2.3 | 19 | 2.6 |
| €1137–€1893 | 374 | 11.0 | 277 | 10.4 | 97 | 13.3 |
| €1894–€2839 | 1418 | 41.7 | 1084 | 40.6 | 334 | 45.7 |
| €2840+ | 1526 | 44.9 | 1245 | 46.7 | 281 | 38.4 |
| Subjective social status (n = 3514) | ||||||
| Lower middle class | 150 | 4.3 | 113 | 4.1 | 37 | 4.9 |
| Middle class | 1616 | 46.0 | 1247 | 45.3 | 369 | 48.6 |
| Upper middle class | 1512 | 43.0 | 1222 | 44.4 | 290 | 38.2 |
| Upper class | 137 | 3.9 | 103 | 3.7 | 34 | 4.5 |
| None of those | 99 | 2.8 | 69 | 2.5 | 30 | 3.9 |
| Self-rated health (n = 3582) | ||||||
| (Very) bad | 119 | 3.3 | 93 | 3.3 | 26 | 3.3 |
| Moderate | 890 | 24.8 | 710 | 25.5 | 180 | 22.7 |
| Good | 2098 | 58.6 | 1646 | 59.0 | 452 | 56.9 |
| Very good | 475 | 13.3 | 339 | 12.2 | 136 | 17.1 |
| Chronic diseases (n = 3584) | ||||||
| None | 1475 | 41.2 | 1079 | 38.6 | 396 | 50.0 |
| Yes, one | 1247 | 34.8 | 998 | 35.7 | 249 | 31.4 |
| Yes, several | 862 | 24.1 | 715 | 25.6 | 147 | 18.6 |
| Taking care of own health (n = 3589) | ||||||
| Less/not at all | 93 | 2.6 | 56 | 2.0 | 37 | 4.7 |
| Moderate | 1213 | 33.8 | 912 | 32.6 | 301 | 38.0 |
| (Very) much | 2283 | 63.6 | 1829 | 65.4 | 454 | 57.3 |
| Health Literacy Levels | n | % | 95%-CI |
|---|---|---|---|
| Inadequate (score 0–8) | 263 | 9.4 | 8.4–10.5 |
| Problematic (score 9–12) | 1032 | 36.8 | 35.1–38.6 |
| Sufficient (score 13–16) | 1506 | 53.8 | 51.9–55.6 |
| Health Literacy Level | |||||
|---|---|---|---|---|---|
| Low (Inadequate/Problematic) | High (Sufficient) | ||||
| n | % | n | % | p-Value | |
| Total | 1295 | 46.2 | 1506 | 53.8 | |
| Gender (n = 2792) | 0.023 | ||||
| Male | 863 | 47.8 | 943 | 52.2 | |
| Female | 427 | 43.3 | 559 | 56.7 | |
| Age (years) (n = 2792) | <0.001 | ||||
| 18–34 | 131 | 53.9 | 112 | 46.1 | |
| 35–49 | 269 | 52.8 | 240 | 47.2 | |
| 50–64 | 482 | 48.2 | 517 | 51.8 | |
| 65–74 | 275 | 38.4 | 442 | 61.6 | |
| 75+ | 132 | 40.7 | 192 | 59.3 | |
| Educational level (n = 2784) | 0.735 | ||||
| Low (ISCED 0–1) | 16 | 41.0 | 23 | 59.0 | |
| Medium (ISCED 2–4) | 227 | 47.2 | 254 | 52.8 | |
| High (ISCED 5–8) | 1044 | 46.1 | 1220 | 53.9 | |
| Work status (n = 2782) | <0.001 | ||||
| Full-time | 644 | 50.5 | 630 | 49.5 | |
| Part-time | 117 | 45.5 | 140 | 54.5 | |
| Retired | 434 | 40.6 | 634 | 59.4 | |
| Other (student, parental leave, unemployed, etc.) | 88 | 48.1 | 95 | 51.9 | |
| Monthly net equivalent income a (n = 2668) | <0.001 | ||||
| Up to €1136 | 37 | 59.7 | 25 | 40.3 | |
| €1137–€1893 | 154 | 55.6 | 123 | 44.4 | |
| €1894–€2839 | 505 | 46.6 | 579 | 53.4 | |
| €2840+ | 532 | 42.7 | 713 | 57.3 | |
| Subjective social status (n = 2754) | <0.001 | ||||
| Lower middle class | 68 | 60.2 | 45 | 39.8 | |
| Middle class | 622 | 49.9 | 625 | 50.1 | |
| Upper middle class | 514 | 42.1 | 708 | 57.9 | |
| Upper class | 40 | 38.8 | 63 | 61.2 | |
| None of those | 30 | 43.5 | 39 | 56.5 | |
| Self-rated health (n = 2788) | <0.001 | ||||
| (Very) bad | 57 | 61.3 | 36 | 38.7 | |
| Moderate | 366 | 51.5 | 344 | 48.5 | |
| Good | 747 | 45.4 | 899 | 54.6 | |
| Very good | 121 | 35.7 | 218 | 64.3 | |
| Chronic diseases (n = 2792) | 0.040 | ||||
| None | 473 | 43.8 | 606 | 56.2 | |
| Yes, one | 460 | 46.1 | 538 | 53.9 | |
| Yes, several | 357 | 49.9 | 358 | 50.1 | |
| Taking care of own health (n = 2797) | 0.001 | ||||
| Less/not at all | 33 | 58.9 | 23 | 41.1 | |
| Moderate | 458 | 50.2 | 454 | 49.8 | |
| (Very) much | 802 | 43.8 | 1027 | 56.2 | |
| Health Literacy Level | |||||||
|---|---|---|---|---|---|---|---|
| Total n = 2801 | Low (Inadequate/Problematic) n = 1295 | High (Sufficient) n = 1506 | |||||
| n | % | n | % [95%-CI] | n | % [95%-CI] | p-Value | |
| Satisfaction | |||||||
| Overall satisfaction with the health system (n = 2718) | <0.001 | ||||||
| (Very) dissatisfied | 127 | 4.7 | 81 | 6.4 [5.2–7.9] | 46 | 3.2 [2.4–4.2] | |
| Neither satisfied nor dissatisfied | 768 | 28.3 | 423 | 33.5 [31.0–36.2] | 345 | 23.7 [21.5–25.9] | |
| (Very) satisfied | 1823 | 67.1 | 757 | 60.0 [57.3–62.7] | 1066 | 73.2 [70.8–75.4] | |
| Access | |||||||
| Accessing after-hours medical care (n = 2796) | <0.001 | ||||||
| Very/somewhat difficult | 1588 | 56.8 | 839 | 64.9 [62.3–67.5] | 749 | 49.8 [47.3–52.3] | |
| Very/somewhat easy | 593 | 21.2 | 208 | 16.1 [14.2–18.2] | 385 | 25.6 [23.4–27.8] | |
| Never needed after-hours medical care | 615 | 22.0 | 245 | 19.0 [16.9–21.2] | 370 | 24.6 [22.5–26.8] | |
| Unmet needs due to a | |||||||
| Waiting time (n = 2580) | 207 | 8.0 | 136 | 11.5 [9.8–13.4] | 71 | 5.1 [4.0–6.3] | <0.001 |
| Distance (n = 2551) | 90 | 3.5 | 61 | 5.2 [4.1–6.6] | 29 | 2.1 [1.4–3.0] | <0.001 |
| Financial reasons (n = 2622) | 199 | 7.6 | 135 | 11.0 [9.4–12.9] | 64 | 4.6 [3.6–5.8] | <0.001 |
| Coverage | |||||||
| Out-of-pocket health spending in the past year b (n = 2671) | |||||||
| Medical products (pharmaceuti-cals and medical aids) | 2043 | 76.5 | 976 | 78.7 [76.4–80.9] | 1067 | 74.6 [72.3–76.8] | 0.012 |
| Deductible | 1202 | 45.0 | 603 | 48.6 [45.9–51.4] | 599 | 41.9 [39.3–44.4] | <0.001 |
| Services (inpatient/ambulatory care by physicians/allied health professionals) | 659 | 24.7 | 351 | 28.3 [25.9–30.9] | 308 | 21.5 [19.5–23.7] | <0.001 |
| Dental care | 661 | 24.7 | 354 | 28.5 [26.1–31.1] | 307 | 21.5 [19.4–23.6] | <0.001 |
| Other services | 529 | 19.8 | 275 | 22.2 [19.9–24.6] | 254 | 17.7 [15.8–19.8] | 0.004 |
| No out-of-pocket spending | 351 | 13.1 | 131 | 10.4 [8.8–12.2] | 220 | 15.2 [13.4–17.1] | <0.001 |
| Quality | |||||||
| Reasons for hospital choice b (n = 2562) | |||||||
| Reputation | 2028 | 79,2 | 922 | 78.0 [75.6–80.3] | 1106 | 80.1 [78.0–82.2] | 0.183 |
| Medical quality | 1596 | 62.3 | 739 | 62.5 [59.7–65.2] | 857 | 62.1 [59.5–64.6] | 0.827 |
| Amenities | 583 | 22.8 | 291 | 24.6 [22.2–27.1] | 292 | 21.2 [19.1–23.4] | 0.037 |
| Quality differences between hospitals (n = 2746) | <0.001 | ||||||
| No/some differences | 645 | 23.5 | 240 | 18.9 [16.8–21.2] | 405 | 27.4 [25.2–29.7] | |
| Notable differences | 2101 | 76.5 | 1028 | 81.1 [78.8–83.2] | 1073 | 72.6 [70.3–74.8] | |
| Knowledge about information sources regarding hospital quality a | |||||||
| Hospital websites (n = 2758) | 2350 | 85.2 | 1088 | 85.1 [83.0–86.9] | 1262 | 85.3 [83.5–87.1] | 0.847 |
| Hospital quality reports (n = 2702) | 1216 | 45.0 | 497 | 39.4 [36.7–42.1] | 719 | 49.9 [47.3–52.5] | <0.001 |
| Other sources (n = 2730) | 1541 | 56.4 | 709 | 55.8 [53.0–58.5] | 832 | 57.0 [54.5–59.5] | 0.514 |
| Safety | |||||||
| Experiences in the past two years a | |||||||
| Received wrong medication/dose (n = 2533) | 188 | 7.4 | 118 | 10.1 [8.5–11.9] | 70 | 5.1 [4.0–6.4] | <0.001 |
| Suspected medical error in treat-ment/care (n = 2525) | 396 | 15.7 | 234 | 20.2 [18.0–22.6] | 162 | 11.8 [10.2–13.6] | <0.001 |
| Was told that a medical error had been made (n = 2623) | 123 | 4.7 | 57 | 4.6 [3.6–5.9] | 66 | 4.7 [3.7–5.9] | 0.914 |
| Received wrong results of medical/laboratory tests (n = 2400) | 107 | 4.5 | 69 | 6.3 [5.0–7.9] | 38 | 2.9 [2.1–3.9] | <0.001 |
| Improved health | |||||||
| Perceived health (VAS from 0 [worst] to 100 [best health]), mean (95%-CI) c (n = 2788) | 75.7 | 1291 | 73.9 [73.0–74.7] | 1497 | 77.3 [76.6–78.1] | <0.001 | |
| Responsiveness | |||||||
| Very good/good rating of the last physician’s visit (GP or SP) (vs. moderate/bad/very bad) | |||||||
| Waiting time until the appointment (n = 2611) | 2177 | 83.4 | 936 | 77.5 [75.1–79.8] | 1241 | 88.5 [86.7–90.0] | <0.001 |
| Waiting time in medical practice (n = 2643) | 1969 | 74.5 | 844 | 68.7 [66.0–71.2] | 1125 | 79.6 [77.4–81.6] | <0.001 |
| Free choice of physician/practice (n = 2607) | 2405 | 92.3 | 1066 | 88.3 [86.4–90.0] | 1339 | 95.6 [94.5–96.6] | <0.001 |
| Respectful treatment (n = 2643) | 2478 | 93.8 | 1121 | 91.2 [89.5–92.7] | 1357 | 96.0 [94.8–96.9] | <0.001 |
| Comprehensible explanations (n = 2642) | 2376 | 89.9 | 1029 | 83.7 [81.6–85.7] | 1347 | 95.3 [94.1–96.3] | <0.001 |
| Participation in shared decision-making (n = 2615) | 2262 | 86.5 | 949 | 78.4 [76.0–80.7] | 1313 | 93.5 [92.1–94.7] | <0.001 |
| Talk confidentially (n = 2616) | 2452 | 93.7 | 1102 | 90.3 [88.6–91.9] | 1350 | 96.7 [95.7–97.5] | <0.001 |
| Coordination of care among different physicians (n = 1953) | 1162 | 59.5 | 418 | 46.1 [42.9–49.3] | 744 | 71.1 [68.3–73.8] | <0.001 |
| Trust that treatment solely serves for well-being (and not other interests) (n = 2602) | 2103 | 80.8 | 880 | 73.4 [70.8–75.8] | 1223 | 87.2 [85.3–88.8] | <0.001 |
| Discrimination experiences in health care in the past year a (n = 2675) | 220 | 8.2 | 156 | 12.6 [10.8–14.5] | 64 | 4.5 [3.5–5.6] | <0.001 |
| High need for reforms in Germany (vs. low/no need) | |||||||
| Coordination between physicians and hospitals (n = 2405) | 1153 | 47.9 | 613 | 55.0 [52.0–57.9] | 540 | 41.9 [39.2–44.6] | <0.001 |
| Coordination between physicians (n = 2557) | 1217 | 47.6 | 665 | 55.1 [52.3–57.9] | 552 | 40.9 [38.3–43.5] | <0.001 |
| Amount of money spent out-of-pocket (n = 2536) | 975 | 38.4 | 511 | 43.5 [40.7–46.4] | 464 | 34.1 [31.6–36.6] | <0.001 |
| Availability of SPs (n = 2762) | 641 | 23.2 | 375 | 29.3 [26.9–31.9] | 266 | 17.9 [16.0–19.9] | <0.001 |
| Quality of care (n = 2669) | 584 | 21.9 | 323 | 26.1 [23.7–28.6] | 261 | 18.2 [16.3–20.3] | <0.001 |
| Availability of home care services (n = 1877) | 413 | 22.0 | 238 | 27.9 [24.9–30.9] | 175 | 17.1 [14.9–19.5] | <0.001 |
| Availability of GPs (n = 2728) | 571 | 20.9 | 311 | 24.6 [22.3–27.0] | 260 | 17.8 [15.9–19.8] | <0.001 |
| Availability of hospitals (n = 2745) | 168 | 6.1 | 99 | 7.8 [6.4–9.4] | 69 | 4.7 [3.7–5.8] | 0.001 |
| Social and financial risk protection | |||||||
| Households with out-of-pocket spending ≥500€ in the past year (vs. <500€) (n = 2312) | 789 | 34.1 | 398 | 36.1 [33.3–39.0] | 391 | 32.3 [29.7–35.0] | 0.058 |
| Very strong/strong financial burden by out-of-pocket spending (vs. fair/less strong/not at all) (n = 2348) | 273 | 11.6 | 168 | 15.1 [13.0–17.2] | 105 | 8.5 [7.1–10.2] | <0.001 |
| Difficulties paying health insurance premium a (n = 2660) | 73 | 2.7 | 44 | 3.6 [2.7–4.7] | 29 | 2.0 [1.4–2.8] | 0.013 |
| Improved efficiency | |||||||
| Experiences in the past two years a | |||||||
| Duplicate tests due to lack of co-ordination (n = 2462) | 572 | 23.2 | 323 | 28.7 [26.1–31.4] | 249 | 18.6 [16.6–20.8] | <0.001 |
| Subjectively unnecessary services (e.g., pharmaceuticals) (n = 2432) | 624 | 25.7 | 358 | 32.4 [29.7–35.2] | 266 | 20.1 [18.0–22.3] | <0.001 |
| Relation of health insurance premium to coverage (n = 2751) | 0.004 | ||||||
| Low/too low | 119 | 4.3 | 65 | 5.1 [4.0–6.4] | 54 | 3.6 [2.8–4.7] | |
| Fair | 1716 | 62.4 | 753 | 59.2 [56.5–61.9] | 963 | 65.1 [62.6–67.5] | |
| Too high/high | 916 | 33.3 | 453 | 35.6 [33.0–38.3] | 463 | 31.3 [29.0–33.7] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Achstetter, K.; Köppen, J.; Haltaufderheide, M.; Hengel, P.; Blümel, M.; Busse, R. Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey. Int. J. Environ. Res. Public Health 2022, 19, 16711. https://doi.org/10.3390/ijerph192416711
Achstetter K, Köppen J, Haltaufderheide M, Hengel P, Blümel M, Busse R. Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey. International Journal of Environmental Research and Public Health. 2022; 19(24):16711. https://doi.org/10.3390/ijerph192416711
Chicago/Turabian StyleAchstetter, Katharina, Julia Köppen, Matthias Haltaufderheide, Philipp Hengel, Miriam Blümel, and Reinhard Busse. 2022. "Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey" International Journal of Environmental Research and Public Health 19, no. 24: 16711. https://doi.org/10.3390/ijerph192416711
APA StyleAchstetter, K., Köppen, J., Haltaufderheide, M., Hengel, P., Blümel, M., & Busse, R. (2022). Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey. International Journal of Environmental Research and Public Health, 19(24), 16711. https://doi.org/10.3390/ijerph192416711





