Statistical Analysis of Absenteeism in a University Hospital Center between 2007 and 2019
Abstract
:1. Introduction
2. Method
2.1. Study Design
2.2. Study Population: Eligibility Criteria
2.3. Judging Criteria
2.3.1. Primary Judgement Criteria
2.3.2. Secondary Judgement Criteria
3. Statistics
4. Results
4.1. Description of the Population
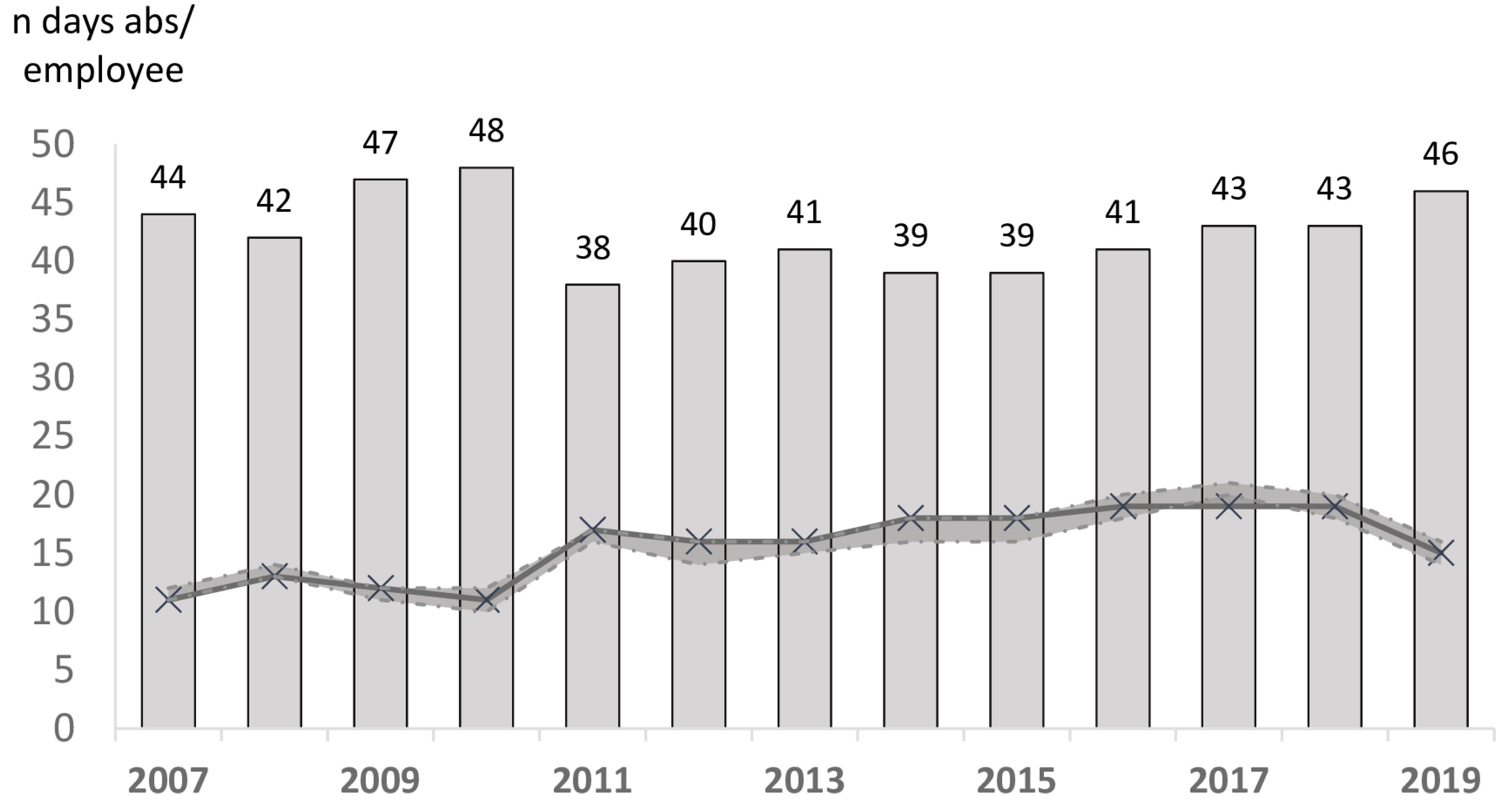
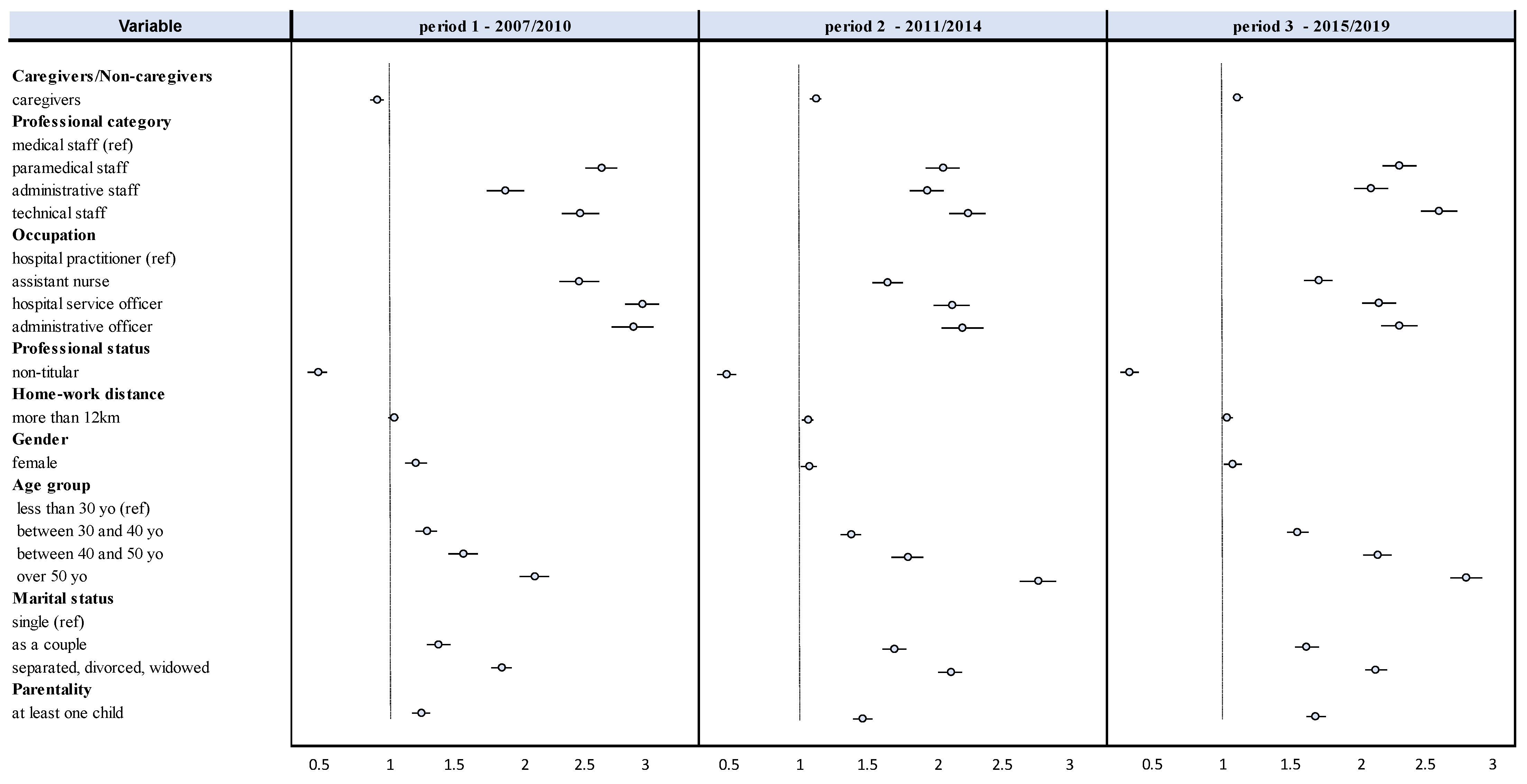
4.2. Study of Absenteeism—Overall Model and by Time Period
4.3. Professional Characteristics
Sociodemographic Characteristics
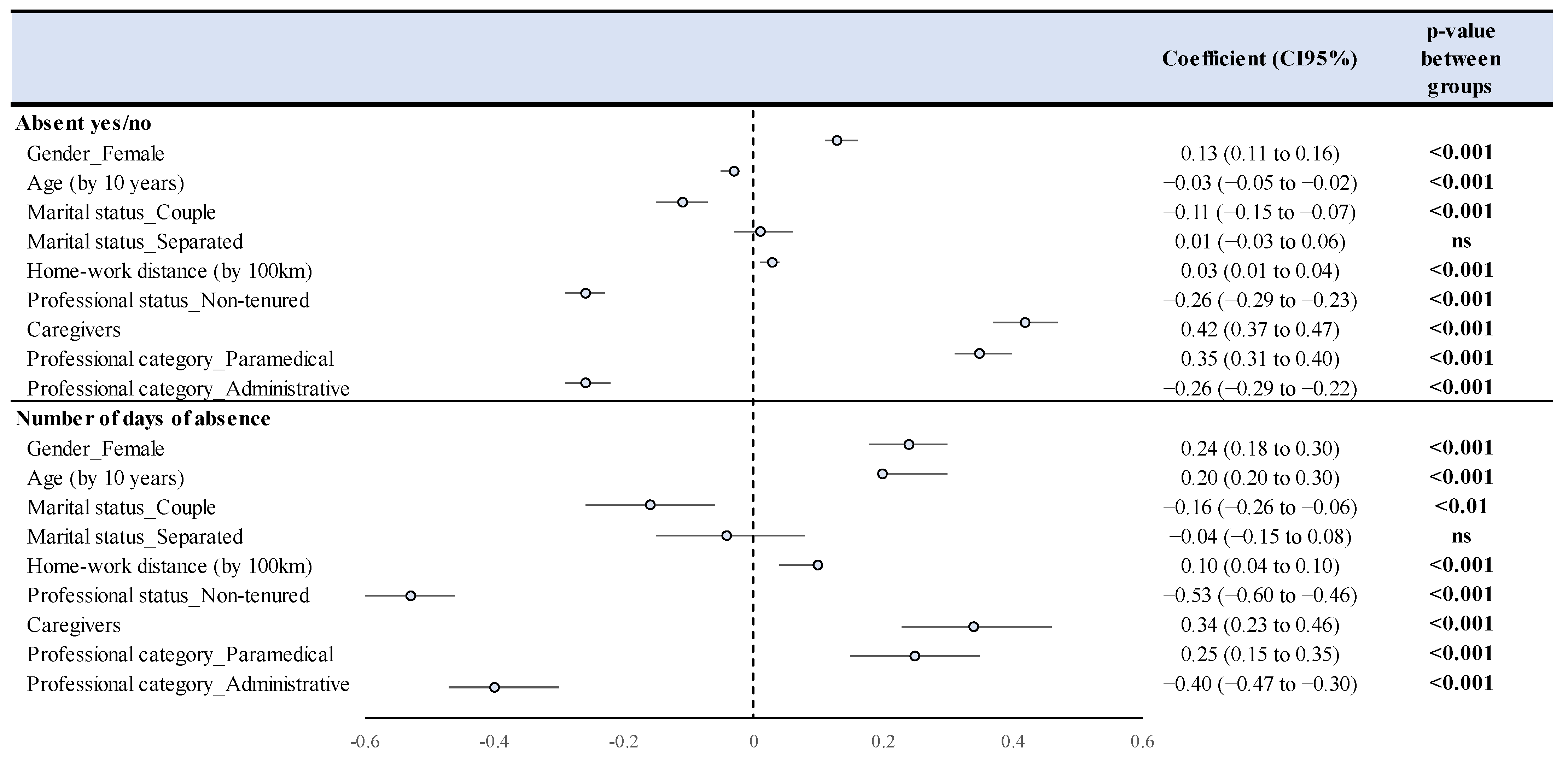
4.4. Study of Compressible Absenteeism—Multivariate Analyses
5. Discussion
- ❖
- A high prevalence of absences and an increase in absenteeism over time for most of the groups studied.
- ❖
- Paramedical personnel remain particularly at risk of absences even if new absentees emerge (administrative staff).
- ❖
- The involvement of sociodemographic factors in the occurrence of compressible absences.
5.1. Prevalence of Absences and Evolution
5.2. Occupational Risk Factors
5.3. Sociodemographic Factors and Absenteeism
6. Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Howard, K.J.; Howard, J.T.; Smyth, A.F. The Problem of Absenteeism and Presenteeism in the Workplace. In Handbook of Occupational Health and Wellness; Gatchel, R.J., Schultz, I.Z., Eds.; Springer: Boston, MA, USA, 2012; pp. 151–179. [Google Scholar] [CrossRef]
- Halbesleben, J.; Whitman, M.V.; Crawford, W.S. A dialectical theory of the decision to go to work: Bringing together absenteeism and presenteeism. Hum. Resour. Manag. Rev. 2014, 24, 177–192. [Google Scholar] [CrossRef]
- Patton, E. The devil is in the details: Judgments of responsibility and absenteeism from work. J. Occup. Organ. Psychol. 2011, 84, 759–779. [Google Scholar] [CrossRef]
- Brami, L.; Damart, S.; Kletz, F. Réformes de l’hôpital, crise à l’hôpital: Une étude des liens entre réformes hospitalières et absentéisme des personnels soignants. Polit. Manag. Public 2012, 29, 541–561. [Google Scholar]
- Strömberg, C.; Aboagye, E.; Hagberg, J.; Bergström, G.; Lohela-Karlsson, M. Estimating the Effect and Economic Impact of Absenteeism, Presenteeism, and Work Environment–Related Problems on Reductions in Productivity from a Managerial Perspective. Value Health 2017, 20, 1058–1064. [Google Scholar]
- Brami, L.; Damart, S.; Kletz, F. Santé au travail et travail en santé. La performance des établissements de santé face à l’absentéisme et au bien-être des personnels soignants. Manag. Avenir. 2013, 61, 168–189. [Google Scholar]
- Duclay, E.; Hardouin, J.; Sébille, V.; Anthoine, E.; Moret, L. Exploring the impact of staff absenteeism on patient satisfaction using routine databases in a university hospital. J. Nurs. Manag. 2014, 23, 833–841. [Google Scholar] [CrossRef]
- Moret, L.; Anthoine, E.; Paillé, C.; Tricaud-Vialle, S.; Gerbaud, L.; Giraud-Roufast, A.; Michel, P.; Lombrail, P. Relationship between inpatient satisfaction and nurse absenteeism: An exploratory study using WHO-PATH performance indicators in France. BMC Res. Notes 2012, 5, 83–87. [Google Scholar] [CrossRef] [Green Version]
- Pollak, C.; Ricroch, L. Les disparités d’absentéisme à l’hôpital sont-elles associées à des différences de conditions de travail? Rev. Francaise Econ. 2016, 4, 181–220. [Google Scholar]
- Al, S.S.; Haxhe, J.J. A study on absenteeism among hospital personnel.—Abstract—Europe PMC. Acta Hosp. 1987, 27, 31–39. [Google Scholar]
- Brborović, H.; Daka, Q.; Dakaj, K.; Brborović, O. Antecedents and associations of sickness presenteeism and sickness absenteeism in nurses: A systematic review. Int. J. Nurs. Pract. 2017, 23, e12598. [Google Scholar] [CrossRef]
- Burmeister, E.A.; Kalisch, B.J.; Xie, B.; Doumit, M.A.A.; Lee, E.; Ferraresion, A.; Terzioglu, F.; Bragadóttir, H. Determinants of nurse absenteeism and intent to leave: An international study. J. Nurs. Manag. 2018, 27, 143–153. [Google Scholar] [CrossRef] [Green Version]
- Davey, M.M.; Cummings, G.; Newburn-Cook, C.V.; Lo, E.A. Predictors of nurse absenteeism in hospitals: A systematic review. J. Nurs. Manag. 2009, 17, 312–330. [Google Scholar]
- Bouville, G. Absentéisme et conditions de travail au féminin: Une frontière méconnue au sein des organisations. RIMHE Rev. Interdiscip. Manag. Homme Entrep. 2014, 11, 3–22. [Google Scholar]
- VandenHeuvel, A.; Wooden, M. Do Explanations of Absenteeism Differ for Men and Women? Hum. Relat. 1995, 48, 1309–1329. [Google Scholar]
- Chaupain-Guillot, S.; Guillot, O. Les déterminants individuels de l’absentéisme au travail. Rev. Econ. 2011, 62, 419–427. [Google Scholar]
- Huver, B.; Richard, S.; Vaneecloo, N.; Bierla, I. Âge, absence-maladie et présentéisme au travail: Le cas d’un établissement de santé régional. Manag. Avenir. 2014, 70, 97–114. [Google Scholar]
- Dolan, S.; Arsenault, A.; Lizotte, J.-P.; Abenhaim, L. L’absentéisme hospitalier au Québec: Aspects culturels et socio-démographiques. Relat. Ind. Ind. Relat. 1983, 38, 45–57. [Google Scholar]
- Bouville, G. La Progression de l’Absentéisme: Nouveaux Comportements des Salariés ou Nouvelles Contraintes Organisationnelles? Université de Rennes 1: Rennes, France, 2010. [Google Scholar]
- Charles-Pauvers, B.; Comeiras, N.; Peyrat-Guillard, D.; Roussel, P. Les Déterminants Psychologiques de la Performance au Travail. Un Bilan des Connaissances et Proposition de Voies de Recherche. 2006. Available online: https://halshs.archives-ouvertes.fr/halshs-00096949 (accessed on 16 January 2021).
- Bouville, G. L’Influence de l’Organisation et des Conditions de Travail sur l’Absentéisme. Analyse Quantitative et Étude de cas [Internet]. Post-Print. HAL; nov. (Post-Print). Report No.: hal-00653592. 2009. Available online: https://ideas.repec.org/p/hal/journl/hal-00653592.html (accessed on 16 January 2021).
- Kottwitz, M.U.; Schade, V.; Burger, C.; Radlinger, L.; Elfering, A. Time Pressure, Time Autonomy, and Sickness Absenteeism in Hospital Employees: A Longitudinal Study on Organizational Absenteeism Records. Saf. Health Work 2017, 9, 109–114. [Google Scholar] [CrossRef]
- Lipszyc, B.; Laurent, S. L’absentéisme dans une institution hospitalière: Les facteurs déterminants. Bruss Econ. Rev. 2021, 166, 131–170. [Google Scholar]
- Vandenberghe, C.; Stordeur, S.; d’Hoore, W. Une analyse des effets de la latitude de décision, de l’épuisement émotionnel et de la satisfaction au travail sur l’absentéisme au sein des unités de soins infirmiers. Trav. Hum. 2009, 72, 209–228. [Google Scholar]
- Estryn-Béhar, M. Santé et Satisfaction des Soignants au Travail en France et en Europe. Presses de l’EHESP. 2008. Available online: http://www.cairn.info/sante-et-satisfaction-des-soignants-au-travail--9782859529468.htm (accessed on 16 January 2021).
- Brami, L.; Damart, S.; Detchessahar, M.; Devigne, M.; Habib, J.; Kletz, F.; Krohmer, C. L’Absentéisme des Personnels Soignants à l’Hôpital. 2014. Available online: https://hal-upec-upem.archives-ouvertes.fr/hal-01130767 (accessed on 16 January 2021).
- Colombat, P.; Altmeyer, A.; Barruel, F.; Bauchetet, C.; Blanchard, P.; Colombat, P.; Copel, L.; Ganem, G.; Rodrigues, M.; Ruszniewski, M. Syndrome d’épuisement professionnel des soignants. Oncologie 2011, 13, 845–863. [Google Scholar]
- Ticharwa, M.; Cope, V.; Murray, M. Nurse absenteeism: An analysis of trends and perceptions of nurse unit managers. J. Nurs. Manag. 2018, 27, 109–116. [Google Scholar] [CrossRef]
- Mudaly, P.; Nkosi, Z.Z. Factors influencing nurse absenteeism in a general hospital in Durban, South Africa. J. Nurs. Manag. 2013, 23, 623–631. [Google Scholar] [CrossRef]
- Stordeur, S.; Vandenberghe, C.; D’hoore, W. Predicteurs de l’epuisementprofessionnel des infirmières: Une etude dans un hopital universitaire. Rech. Soins Infirm. 1999, 59, 57–66. [Google Scholar]
- Garrosa, E.; Moreno-Jiménez, B.; Liang, Y.; González, J.L. The relationship between socio-demographic variables, job stressors, burnout, and hardy personality in nurses: An exploratory study. Int. J. Nurs. Stud. 2008, 45, 418–427. [Google Scholar] [CrossRef]
- Loriol, M. La construction sociale de la fatigue au travail. St. Conjug. 2005, 32, 52–62. [Google Scholar]
- Dutheil, F.; Trousselard, M.; Perrier, C.; Lac, G.; Chamoux, A.; Duclos, M.; Naughton, G.; Mnatzaganian, G.; Schmidt, J. Urinary Interleukin-8 Is a Biomarker of Stress in Emergency Physicians, Especially with Advancing Age—The JOBSTRESS* Randomized Trial. PLoS ONE 2013, 8, e71658. [Google Scholar] [CrossRef]
- Dutheil, F.; Aubert, C.; Pereira, B.; Dambrun, M.; Moustafa, F.; Mermillod, M.; Baker, J.S.; Trousselard, M.; Lesage, F.-X.; Navel, V. Suicide among physicians and health-care workers: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0226361. [Google Scholar] [CrossRef] [Green Version]
- Pronk, N.P.; Martinson, B.; Kessler, R.C.; Beck, A.L.; Simon, G.E.; Wang, P. The Association Between Work Performance and Physical Activity, Cardiorespiratory Fitness, and Obesity. J. Occup. Environ. Med. 2004, 46, 19–25. [Google Scholar] [CrossRef]
- Merrill, R.M.; Aldana, S.G.; Pope, J.E.; Anderson, D.R.; Coberley, C.R.; Grossmeier, J.J.; Whitmer, R.W. Self-Rated Job Performance and Absenteeism According to Employee Engagement, Health Behaviors, and Physical Health. J. Occup. Environ. Med. 2013, 55, 10–18. [Google Scholar] [CrossRef] [Green Version]
- Côté, D.; Haccoun, R.R. L’absentéisme des femmes et des hommes: Une méta-analyse. Can. J. Adm. Sci. Rev. Can. Sci. Adm. 1991, 8, 130–139. [Google Scholar]
- Mastekaasa, A.; Olsen, K.M. Gender, Absenteeism, and Job Characteristics: A Fixed Effects Approach. Work Occup. 1998, 25, 195–228. [Google Scholar]
- Barmby, T.A.; Ercolani, M.G.; Treble, J.G. Sickness Absence: An International Comparison. Econ. J. 2002, 112, F315–F331. [Google Scholar] [CrossRef]
- El Khamali, R.; Mouaci, A.; Valera, S.; Cano-Chervel, M.; Pinglis, C.; Sanz, C. Effects of a Multimodal Program Including Simulation on Job Strain Among Nurses Working in Intensive Care Units: A Randomized Clinical Trial. JAMA 2018, 320, 1988–1997. [Google Scholar]
- Linton, S.J.; Boersma, K.; Traczyk, M.; Shaw, W.; Nicholas, M. Early Workplace Communication and Problem Solving to Prevent Back Disability: Results of a Randomized Controlled Trial Among High-Risk Workers and Their Supervisors. J. Occup. Rehabil. 2015, 26, 150–159. [Google Scholar] [CrossRef] [Green Version]
- Brox, J.I.; Frøystein, O. Health-related quality of life and sickness absence in community nursing home employees: Randomized controlled trial of physical exercise. Occup. Med. 2005, 55, 558–563. [Google Scholar] [CrossRef] [Green Version]
- Christensen, J.R.; Overgaard, K.; Hansen, K.; Søgaard, K.; Holtermann, A. Effects on Presenteeism and Absenteeism From a 1-Year Workplace Randomized Controlled Trial Among Health Care Workers. J. Occup. Environ. Med. 2013, 55, 1186–1190. [Google Scholar]
- Jakobsen, M.D.; Sundstrup, E.; Brandt, M.; Jay, K.; Aagaard, P.; Andersen, L.L. Physical exercise at the workplace prevents deterioration of work ability among healthcare workers: Cluster randomized controlled trial. BMC Public Health 2015, 15, 1174. [Google Scholar] [CrossRef] [Green Version]
- Andersen, L.N.; Juul-Kristensen, B.; Roessler, K.K.; Herborg, L.G.; Sørensen, T.L.; Søgaard, K. Efficacy of ‘Tailored Physical Activity’ on reducing sickness absence among health care workers: A 3-months randomised controlled trial. Man. Ther. 2015, 20, 666–671. [Google Scholar] [CrossRef]
- Svensson, A.L.; Strøyer, J.; Ebbehøj, N.E.; Schultz-Larsen, K.; Marott, J.L.; Mortensen, O.S.; Suadicani, P. Multidimensional intervention and sickness absence in assistant nursing students. Occup. Med. 2009, 59, 563–569. [Google Scholar] [CrossRef]


| Agents with ≥1 Absence/Year | p-Value between Groups | Effect Size between Groups with CI | Zero Inflated Negative Binomial (ZINB) | |||||
|---|---|---|---|---|---|---|---|---|
| Variables | n | n Agents | n Days of Absence | Incidence Risk Ratio (IRR) | ||||
| (%) | Median (Range) | Count Model | Inflation Model | |||||
| Caregivers/non-caregivers | ||||||||
| Caregivers | 4310 | (39%) | 13 (4 to 47) | <0.001 | ref. | ref. | ||
| Non-caregivers | 12103 | (44%) | 16 (5 to 55) | 0.03 [0.01;0.04] | 1.19 *** | 0.73 *** | ||
| Professional category | ||||||||
| Medical | 4861 | (35%) | 8 (2 to 24) | <0.001 | ref. | ref. | ||
| Paramedical | 7640 | (46%) | 19 (6 to 64) | 0.27 [0.25;0.29] | 2.31 *** | 0.64 *** | ||
| Administrative | 2542 | (37%) | 12 (3 to 42) | 0.17 [0.15;0.19] | 1.96 *** | 1.08 * | ||
| Technical | 2713 | (42%) | 15 (5 to 53) | 0.28 [0.25;0.30] | 2.29 *** | 0.82 *** | ||
| Occupation | ||||||||
| Hospital practitioner | 443 | (31%) | 8 (1 to 29) | <0.001 | ref. | ref. | ||
| Assistant nurse | 2263 | (50%) | 20 (7 to 64) | 0.23 [0.18;0.27] | 1.89 *** | 0.40 *** | ||
| Cleaners | 1324 | (54%) | 20 (7 to 68) | 0.33 [0.28;0.37] | 2.36 *** | 0.33 *** | ||
| Administrative officer | 870 | (46%) | 13 (4 to 42) | 0.38 [0.33;0.43] | 2.44 *** | 0.50 *** | ||
| Professional status | ||||||||
| Tenured | 8338 | (27%) | 19 (5 to 66) | <0.001 | ref. | ref. | ||
| Non-tenured | 11739 | (23%) | 8 (3 to 24) | 0.32 [0.30;0.33] | 0.36 *** | 1.56 *** | ||
| Home-work distance | ||||||||
| <12 km | 9040 | (40%) | 14 (4 to 45) | <0.001 | ref. | ref. | ||
| >12 km | 6558 | (44%) | 17 (5 to 57) | 0.05 [0.04;0.06] | 1.04 * | 0.76 *** | ||
| Gender | ||||||||
| Male | 4382 | (36%) | 11 (3 to 38) | <0.001 | ref. | ref. | ||
| Female | 12031 | (43%) | 15 (5 to 52) | 0.09 [0.07;0.1] | 1.12 *** | 0.66 *** | ||
| Age | ||||||||
| <30 years old | 8655 | (40%) | 10 (3 to 35) | <0.001 | ref. | ref. | ||
| 30–40 years old | 5506 | (44%) | 15 (5 to 48) | 0.15 [0.13;0.17] | 1.43 *** | 1.01 | ||
| 40–50 year old | 4705 | (43%) | 15 (5 to 48) | 0.21 [0.19;0.23] | 1.87 *** | 1.00 | ||
| >50 years old | 4298 | (44%) | 18 (5 to 66) | 0.32 [0.30;0.34] | 2.60 *** | 0.87 *** | ||
| Marital status | ||||||||
| Single | 8592 | (24%) | 10 (3 to 31) | <0.001 | ref. | ref. | ||
| Couple | 8415 | (26%) | 17 (5 to 59) | 0.18 [0.17;0.19] | 1.58 *** | 0.74 *** | ||
| Separated/widowed | 1859 | (29%) | 20 (7 to 69) | 0.35 [0.33;0.37] | 2.03 *** | 0.61 *** | ||
| Parentality | ||||||||
| No children | 9498 | (39%) | 12 (4 to 38) | <0.001 | ref. | ref. | ||
| ≥1 children | 8890 | (44%) | 16 (5 to 52) | 0.16 [0.15;0;17] | 1.48 *** | 0.82 *** | ||
| Period 1—2007/2010 | Period 2—2011/2014 | Period 3—2015/2019 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n(%) Agents with ≥1 Absence/Year | Median (Range) | n | n(%) Agents with ≥1 Absence/Year | Median (Range) | n | n(%) Agents with ≥1 Absence/Year | Median (Range) | |||
| Caregivers/non-caregivers | |||||||||||
| Caregivers | 6829 | 45 | 13 (4–43) | 7051 | 41 | 18 (5–62) | 8462 | 45 | 18 (5–61) | ||
| Non-caregivers | 2808 | 46 | 8 (2–32) | 2583 | 36 | 14 (4–49) | 2655 | 36 | 19 (6–63) | ||
| Professional category | |||||||||||
| Medical | 1987 | 34 | 8 (4–17) | 2000 | 29 | 10 (3–29) | 2916 | 40 | 8 (1–25) | ||
| Paramedical | 4842 | 47 | 14 (4–49) | 5051 | 44 | 20 (6–68) | 5546 | 46 | 21 (7–73) | ||
| Administrative | 1484 | 44 | 6 (2–28) | 1438 | 33 | 13 (4–46) | 1504 | 34 | 18 (5–57) | ||
| Technical | 1324 | 48 | 11 (3–38) | 1145 | 40 | 15 (5–54) | 1151 | 39 | 20 (6–75) | ||
| Occupation | |||||||||||
| Hospital practitioner | 247 | 33 | 7 (2–25) | 270 | 23 | 13.5 (6–33) | 318 | 34 | 6 (1–31) | ||
| Assistant nurse | 1437 | 51 | 17 (5–55) | 1488 | 49 | 22 (7–79) | 1602 | 51 | 23 (8–79) | ||
| Cleaners | 649 | 53 | 18 (7–57) | 684 | 52 | 21 (7–80) | 735 | 56 | 25 (8–88) | ||
| Administrative officer | 499 | 53 | 7 (2–27) | 461 | 41 | 14 (4–44) | 420 | 44 | 21 (7–64) | ||
| Professional status | |||||||||||
| Tenured | 5719 | 29 | 13 (3–46) | 6083 | 25 | 20 (6–71) | 6433 | 26 | 25 (8–81) | ||
| Non-tenured | 3918 | 23 | 8 (3–22) | 3551 | 20 | 9 (3–29) | 4684 | 25 | 7 (2–22) | ||
| Home-work distance | |||||||||||
| <12 km | 4368 | 46 | 11 (3–39) | 5087 | 37 | 15 (5–55) | 6361 | 40 | 16 (5–55) | ||
| >12 km | 3605 | 48 | 12 (3–46) | 4139 | 42 | 18 (5–61) | 4643 | 45 | 21 (6–69) | ||
| Gender | |||||||||||
| Male | 2414 | 42 | 9 (2–31) | 2324 | 34 | 13 (4–47) | 2878 | 36 | 14 (4–48) | ||
| Female | 7223 | 46 | 12 (4–42) | 7310 | 41 | 18 (5–61) | 8239 | 44 | 19 (6–64) | ||
| Age | |||||||||||
| <30 years old | 3566 | 39 | 10 (4–31) | 3520 | 38 | 11 (3–43) | 4673 | 42 | 10 (3–33) | ||
| 30–40 years old | 2133 | 46 | 12 (3–41) | 2158 | 41 | 16 (5–53) | 2372 | 44 | 18 (5–58) | ||
| 40–50 year old | 2121 | 47 | 11 (3–39) | 2017 | 39 | 17 (6–56) | 2046 | 42 | 21 (7–69) | ||
| >50 years old | 1817 | 50 | 13 (3–50) | 1939 | 41 | 22 (7–96) | 2026 | 42 | 28 (9–94) | ||
| Marital status | |||||||||||
| Single | 3735 | 25 | 9 (3–25) | 3676 | 21 | 10.5 (3–33) | 4933 | 26 | 11 (3–33) | ||
| Couple | 5018 | 28 | 12 (3–43) | 5054 | 25 | 19 (6–65) | 5298 | 26 | 21 (6–70) | ||
| Separated/widowed | 855 | 31 | 14 (5–50) | 859 | 28 | 21 (7–73) | 812 | 29 | 25 (9–84) | ||
| Parentality | |||||||||||
| No children | 4237 | 27 | 10 (4–34) | 4222 | 24 | 14 (4–48) | 5452 | 27 | 12 (3–39) | ||
| ≥1 children | 5400 | 29 | 12 (3–42) | 5412 | 25 | 18 (5–62) | 5665 | 26 | 22 (7–71) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Millot, C.; Pereira, B.; Miallaret, S.; Clinchamps, M.; Vialatte, L.; Guillin, A.; Bailly, Y.; Ugbolue, U.C.; Navel, V.; Baker, J.S.; et al. Statistical Analysis of Absenteeism in a University Hospital Center between 2007 and 2019. Int. J. Environ. Res. Public Health 2022, 19, 12966. https://doi.org/10.3390/ijerph191912966
Millot C, Pereira B, Miallaret S, Clinchamps M, Vialatte L, Guillin A, Bailly Y, Ugbolue UC, Navel V, Baker JS, et al. Statistical Analysis of Absenteeism in a University Hospital Center between 2007 and 2019. International Journal of Environmental Research and Public Health. 2022; 19(19):12966. https://doi.org/10.3390/ijerph191912966
Chicago/Turabian StyleMillot, Charlène, Bruno Pereira, Sophie Miallaret, Maëlys Clinchamps, Luc Vialatte, Arnaud Guillin, Yan Bailly, Ukadike Chris Ugbolue, Valentin Navel, Julien Steven Baker, and et al. 2022. "Statistical Analysis of Absenteeism in a University Hospital Center between 2007 and 2019" International Journal of Environmental Research and Public Health 19, no. 19: 12966. https://doi.org/10.3390/ijerph191912966









