Estimating Health-Related Quality of Life Based on Demographic Characteristics, Questionnaires, Gait Ability, and Physical Fitness in Korean Elderly Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Instrumentation
2.3. Test Procedure
2.3.1. Evaluating QoL Using SF-36
- Physical functioning;
- Role limitations owing to physical health;
- Role limitations caused by emotional problems;
- Pain;
- General health;
- Vitality;
- Emotional well-being;
- Social functioning.
2.3.2. Demographic Characteristics
2.3.3. Assessment Using Other Questionnaires
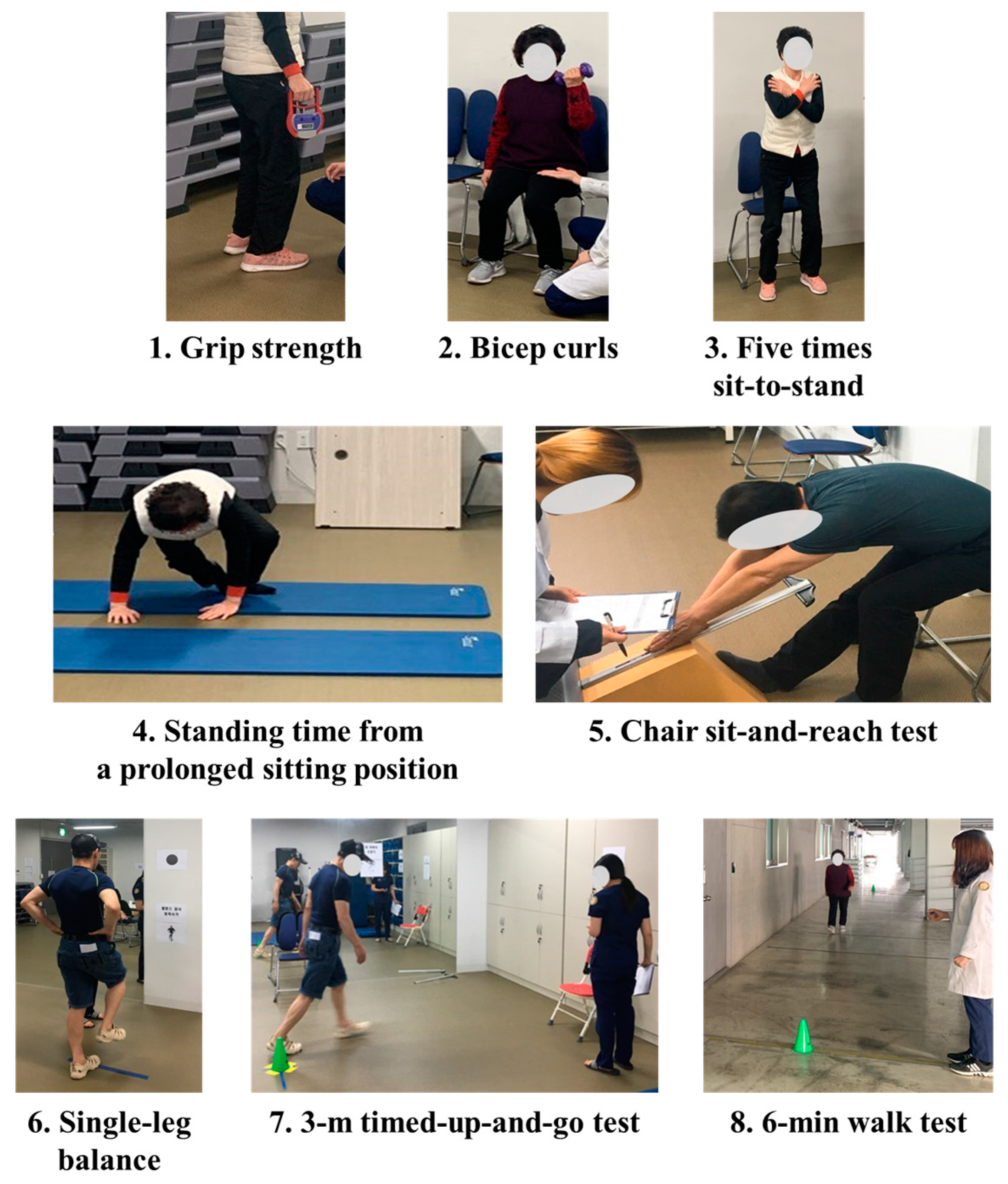
2.3.4. Physical Fitness Test
- Grip strengths of both the hands were measured using an isometric digital handgrip dynamometer (T.K.K. 5401 Grip-D, Takei Scientific Instruments, Tokyo, Japan) to assess the upper body strength;
- Upper body strengths of male and female participants were assessed based on the bicep curls performed using dumbbells weighing 3 kg and 2 kg, respectively;
- Lower body strength was assessed considering the performance of five times sit-to-stand exercises;
- Standing time (ST) from a long sitting position (LSP) was measured to assess the lower body strength;
- Chair sit-and-reach test was conducted to assess the lower body flexibility;
- Single-leg balance (dominant leg) was conducted to assess the static balance;
- A 3-m timed-up-and-go test was conducted to assess the dynamic balance;
- A 6-min walk test (6MWT) was conducted to assess the functional or cardiorespiratory endurance.
2.3.5. Overground Walking Test at Different Speeds
2.4. Data Analysis
2.5. Statistical Analysis
- Subset selection [46] was achieved using the number of features in the optimal model to determine the best combination of features that maximizes the performance.
2.5.1. Data Setup
2.5.2. Feature Rank
- To rank high-dimensional features, feature-by-feature statistical testing with analysis of variance and simple LR for categorical and continuous data, respectively, was performed. The PV-based marginal test, which is a type of filter method, is a pairwise calculation that focuses on the main effect of the feature on the target individually and not the joint effect of the features [48]. After calculating the PVs of the features, we sorted the list in the ascending order (Table S2).
- The FI in RF, computed based on the Gini importance, was used as another feature ranking method [43]. It is a representative ensemble-based ML methodology, with the concept originating from predictive model construction by combining trees [49]. FI considers both the interaction effect among features and the main effect of the feature on the target individually [49,50]. After clarifying the FI, it was arranged in the descending order of the FI (Table S2).
2.5.3. Model Generation: Heuristic Approach
2.5.4. Subset Selection
3. Results
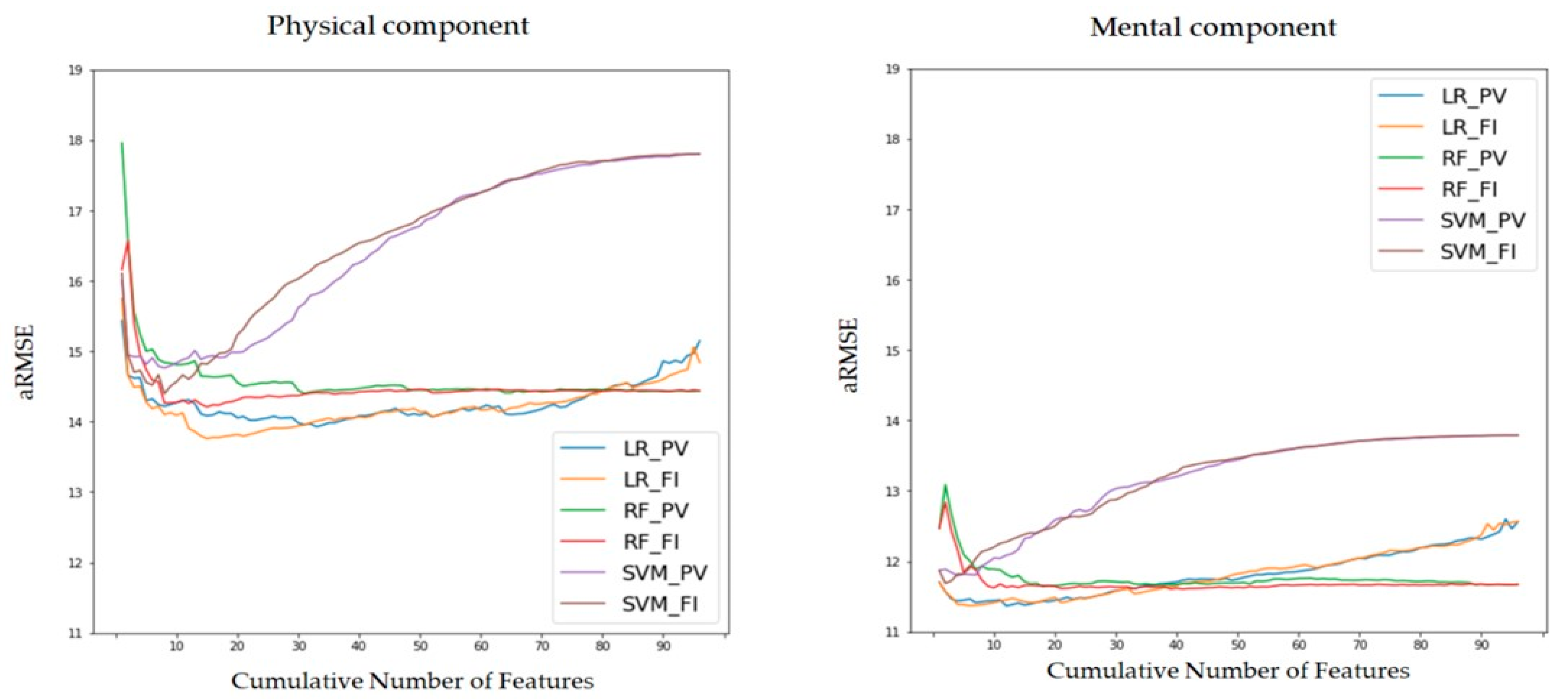
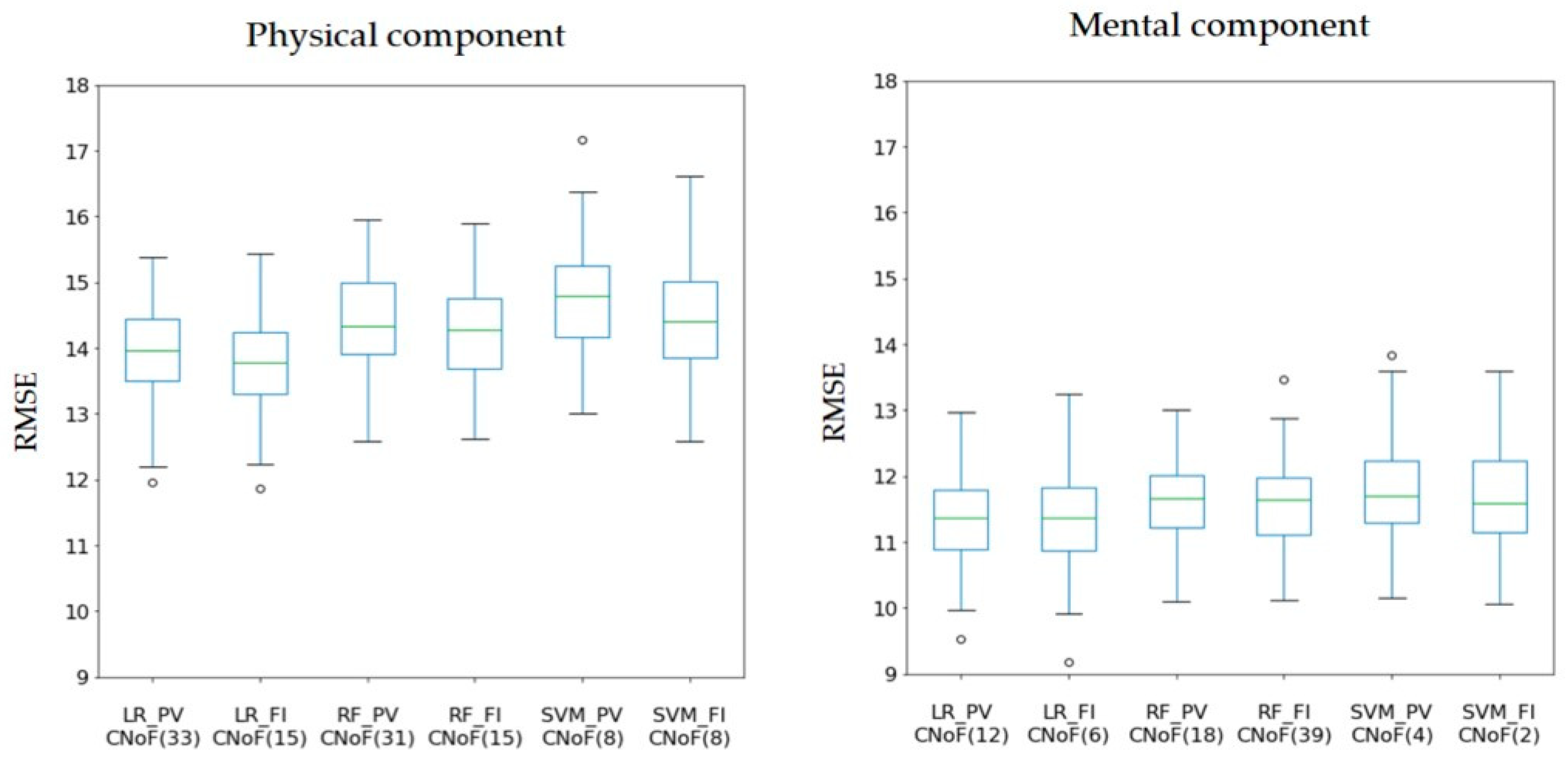
3.1. Model Comparison
- In the case of the physical component, we concluded that the LR model with the FI feature rank is the best performing model with a CNoF of 15. Additionally, this model exhibits dominant statistics, i.e., the aRMSE and median. Conversely, the worst model among the six models in Table 1 is the SVM with the PV feature rank, wherein the CNoF is 8.
- In the case of the mental component, we figured that the LR model with the PV feature rank is the optimal model with a minimum aRMSE and with a CNoF of 12. However, the worst model among the six models in Table 1 is the SVM with the PV feature rank and its CNoF is 4.
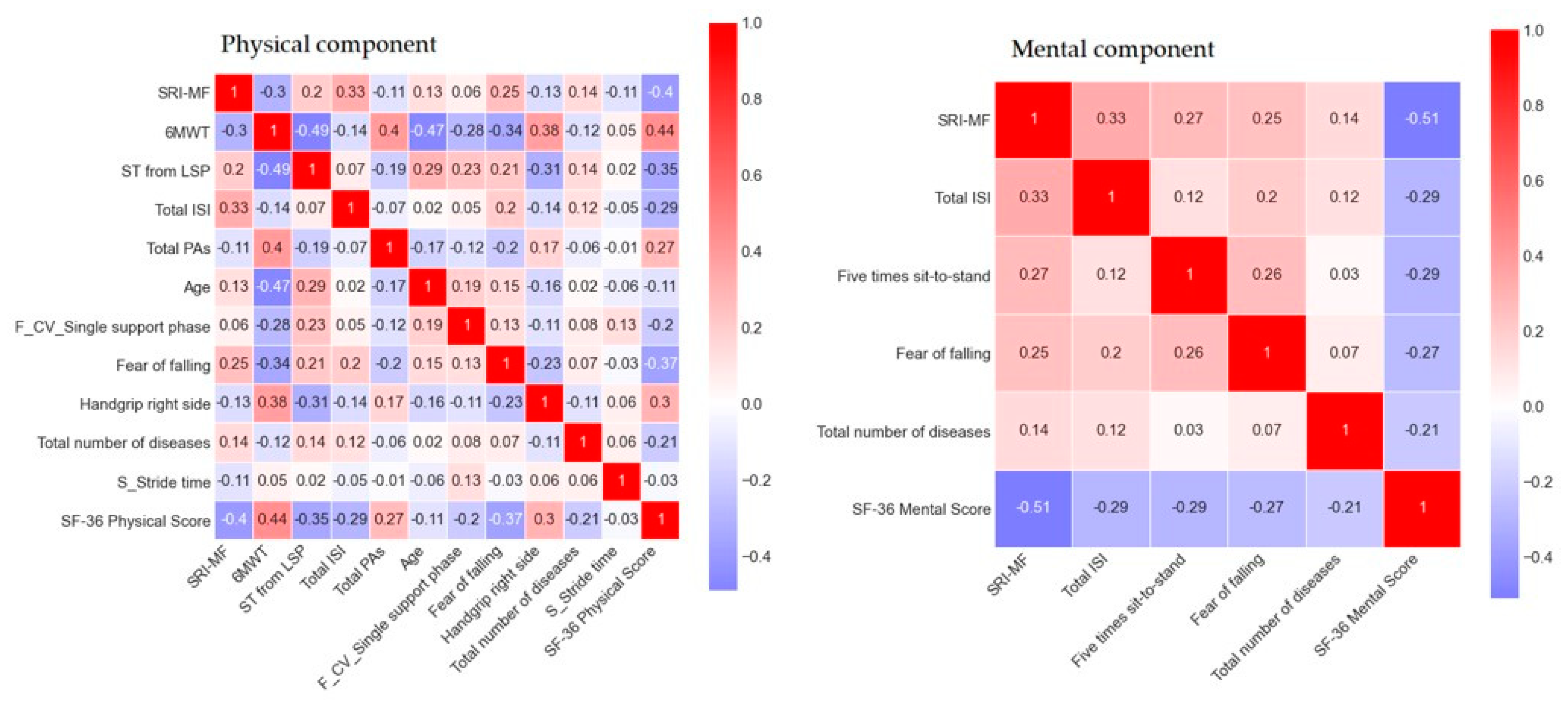
3.2. Best Prediction Model
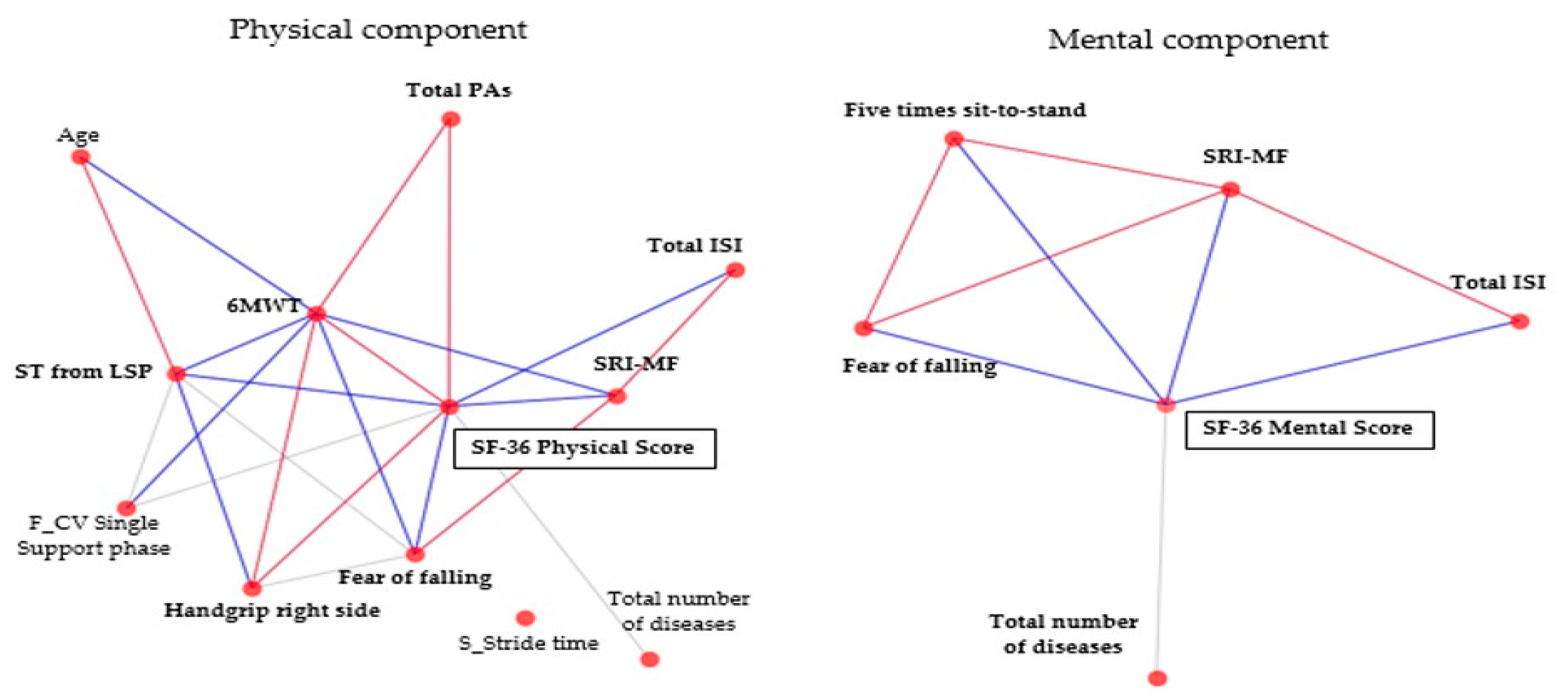
3.3. Input Features of the Best Prediction Model
4. Discussion
- In terms of the physical component, demographic characteristics (age and the total number of diseases), questionnaires (total PAs, total ISI, and total SRI-MF and fear of falling), gait ability (CV of single-support phase at faster speed and stride time at slower speed), and physical fitness (walking distance during 6MWT, ST from LSP, and handgrip) features were identified as significant variables.
- In terms of the mental component, demographic characteristics (total number of diseases), questionnaires (total ISI, total SRI-MF, and fear of falling), and physical fitness (five times sit-to-stand) features were identified as significant variables.
- In particular, the 6MWD, ST from LSP, SRI-MF, fear of falling, and handgrip (r = 0.30–0.44) were highly correlated with the physical component; the total SRI-MF (r = −0.51) was the most highly correlated feature with the mental component. These findings are discussed in detail in the subsequent sections.
4.1. Feature Selection and Machine-Learning Model
4.2. HRQoL in Elderly Adults Based on the Physical Component
4.3. HRQoL in Elderly Adults Based on the Mental Component
4.4. Limitations and Future Applications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. Available online: https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html (accessed on 27 July 2021).
- 2019 Korean Population Census. Available online: http://kostat.go.kr/portal/eng/pressReleases/8/7/index.board (accessed on 29 July 2021).
- World Health Organization. Global Strategy and Action Plan on Ageing and Health; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Bowling, A.; Dieppe, P. What is successful ageing and who should define it? BMJ 2005, 331, 1548–1551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.H.; Choi, I.; Ahn, W.Y.; Shin, E.; Cho, S.I.; Kim, S.; Oh, B. Estimating quality of life with biomarkers among older Korean adults: A machine-learning approach. Arch. Gerontol. Geriatr. 2020, 87, 103966. [Google Scholar] [CrossRef] [PubMed]
- Pequeno, N.P.F.; de Araújo Cabral, N.L.; Marchioni, D.M.; Lima, S.C.V.C.; de Oliveira Lyra, C. Quality of life assessment instruments for adults: A systematic review of population-based studies. Health Qual. Life Outcomes 2020, 18, 1–13. [Google Scholar] [CrossRef]
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 2019, 53, 100903. [Google Scholar] [CrossRef] [PubMed]
- Scollan-Koliopoulos, M.; Bleich, D.; Rapp, K.J.; Wong, P.; Hofmann, C.J.; Raghuwanshi, M. Health-related quality of life, disease severity, and anticipated trajectory of diabetes. Diabetes Educ. 2013, 39, 83–91. [Google Scholar] [CrossRef]
- McHorney, C.A.; Ware, J.E., Jr.; Raczek, A.E. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.A.; Donegan, D.; Albert, T. The 36-item short form. J. Am. Acad. Orthop. Surg. 2007, 15, 126–134. [Google Scholar] [CrossRef]
- Bjerk, M.; Brovold, T.; Skelton, D.A.; Bergland, A. Associations between health-related quality of life, physical function and fear of falling in older fallers receiving home care. BMC Geriatr. 2018, 18, 253. [Google Scholar] [CrossRef]
- Chang, N.T.; Chi, L.Y.; Yang, N.P.; Chou, P. The impact of falls and fear of falling on health-related quality of life in Taiwanese elderly. J. Community Health Nurs. 2010, 27, 84–95. [Google Scholar] [CrossRef]
- Schoene, D.; Heller, C.; Aung, Y.N.; Sieber, C.C.; Kemmler, W.; Freiberger, E. A systematic review on the influence of fear of falling on quality of life in older people: Is there a role for falls? Clin. Interv. Aging 2019, 14, 701. [Google Scholar] [CrossRef] [Green Version]
- Pasco, J.A.; Williams, L.J.; Jacka, F.N.; Henry, M.J.; Coulson, C.E.; Brennan, S.L.; Leslie, E.; Nicholson, G.C.; Kotowicz, M.A.; Berk, M. Habitual physical activity and the risk for depressive and anxiety disorders among older men and women. Int. Psychogeriatr. 2011, 23, 292–298. [Google Scholar] [CrossRef] [Green Version]
- Pasco, J.A.; Williams, L.J.; Jacka, F.N.; Stupka, N.; Brennan-Olsen, S.L.; Holloway, K.L.; Berk, M. Sarcopenia and the common mental disorders: A potential regulatory role of skeletal muscle on brain function? Curr. Osteoporos. Rep. 2015, 13, 351–357. [Google Scholar] [CrossRef]
- Kang, S.Y.; Lim, J.; Park, H.S. Relationship between low handgrip strength and quality of life in Korean men and women. Qual. Life Res. 2018, 27, 2571–2580. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Hurst, C.; Demurtas, J.; Firth, J.; Howden, R.; Yang, L.; Tully, M.A.; Koyanagi, A.; Ilie, P.C.; López-Sánchez, G.F.; et al. Handgrip strength and health outcomes: Umbrella review of systematic reviews with meta-analyses of observational studies. J. Sport Health Sci. 2021, 10, 290–295. [Google Scholar] [CrossRef]
- Wang, D.X.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herssens, N.; Verbecque, E.; Hallemans, A.; Vereeck, L.; Van Rompaey, V.; Saeys, W. Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review. Gait Posture 2018, 64, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Aboutorabi, A.; Arazpour, M.; Bahramizadeh, M.; Hutchins, S.W.; Fadayevatan, R. The effect of aging on gait parameters in able-bodied older subjects: A literature review. Aging Clin. Exp. Res. 2016, 28, 393–405. [Google Scholar] [CrossRef]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stevens, Z.; Barlow, C.; Kendrick, D.; Masud, T.; Skelton, D.A.; Dinan-Young, S.; Iliffe, S. Effectiveness of general practice-based physical activity promotion for older adults: Systematic review. Prim. Health Care Res. Dev. 2014, 15, 190–201. [Google Scholar] [CrossRef] [Green Version]
- Moore, A.; Motagh, S.; Sadeghirad, B.; Begum, H.; Riva, J.J.; Gaber, J.; Dolovich, L. Volunteer impact on health-related outcomes for seniors: A systematic review and meta-analysis. Can. Geriatr. J. 2021, 24, 44. [Google Scholar] [CrossRef]
- Mjolsness, E.; DeCoste, D. Machine learning for science: State of the art and future prospects. Science 2001, 293, 2051–2055. [Google Scholar] [CrossRef] [PubMed]
- Khan, O.; Badhiwala, J.H.; Witiw, C.D.; Wilson, J.R.; Fehlings, M.G. Machine learning algorithms for prediction of health-related quality-of-life after surgery for mild degenerative cervical myelopathy. Spine J. 2020, 21, 1659–1669. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Karnuta, J.M.; Haeberle, H.S.; Rodeo, S.A.; Nwachukwu, B.U.; Williams, R.J., III. Effect of preoperative imaging and patient factors on clinically meaningful outcomes and quality of life after osteochondral allograft transplantation: A machine learning analysis of cartilage defects of the knee. Am. J. Sports Med. 2021, 49, 03635465211015179. [Google Scholar] [CrossRef] [PubMed]
- Noh, B.; Youm, C.; Lee, M.; Park, H. Associating gait phase and physical fitness with global cognitive function in the aged. Int. J. Environ. Res. Public Health 2020, 17, 4786. [Google Scholar] [CrossRef]
- Lee, M.; Youm, C.; Noh, B.; Park, H.; Cheon, S.M. Gait characteristics under imposed challenge speed conditions in patients with Parkinson’s disease during overground walking. Sensors 2020, 20, 2132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, T.; Lee, M.; Youm, C.; Noh, B.; Park, H. Association between gait variability and gait-ability decline in elderly women with subthreshold insomnia stage. Int. J. Environ. Res. Public Health 2020, 17, 5181. [Google Scholar] [CrossRef]
- Noh, B.; Youm, C.; Lee, M.; Park, H. Age-specific differences in gait domains and global cognitive function in older women: Gait characteristics based on gait speed modification. PeerJ 2020, 8, e8820. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.; Youm, C.; Noh, B.; Park, H. Low composite functional movement screen score associated with decline of gait stability in young adults. PeerJ 2021, 9, e11356. [Google Scholar] [CrossRef]
- Joo, J.Y.; Kim, Y.K.; Park, J.Y. Reliability of 3D-inertia measurement unit based shoes in gait analysis. Korean J. Sport Biomech. 2015, 25, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.K.; Joo, J.Y.; Jeong, S.H.; Jeon, J.H.; Jung, D.Y. Effects of walking speed and age on the directional stride regularity and gait variability in treadmill walking. J. Mech. Sci. Technol. 2016, 30, 2899–2906. [Google Scholar] [CrossRef]
- Lee, M.; Youm, C.; Jeon, J.; Cheon, S.M.; Park, H. Validity of shoe-type inertial measurement units for Parkinson’s disease patients during treadmill walking. J. Neuroeng. Rehabil. 2018, 15, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oyeyemi, A.L.; Umar, M.; Oguche, F.; Aliyu, S.U.; Oyeyemi, A.Y. Accelerometer-determined physical activity and its comparison with the International Physical Activity Questionnaire in a sample of Nigerian adults. PLoS ONE 2014, 9, e87233. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Morin, C.M. Insomnia: Psychological Assessment and Management; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Choi, S.M.; Kang, T.Y.; Woo, J.M. Development and validation of a modified form of the stress response inventory for workers. J. Korean Neuropsych. Assoc. 2006, 45, 541–553. [Google Scholar]
- Noh, B.; Youm, C.; Goh, E.; Lee, M.; Park, H.; Jeon, H.; Kim, O.Y. XGBoost based machine learning approach to predict the risk of fall in older adults using gait outcomes. Sci. Rep. 2021, 11, 12183. [Google Scholar]
- Bagherzadeh-Khiabani, F.; Ramezankhani, A.; Azizi, F.; Hadaegh, F.; Steyerberg, E.W.; Khalili, D. A tutorial on variable selection for clinical prediction models: Feature selection methods in data mining could improve the results. J. Clin. Epidemiol. 2016, 71, 76–85. [Google Scholar] [CrossRef]
- Saraswat, M.; Arya, K.V. Feature selection and classification of leukocytes using random forest. Med. Biol. Eng. Comput. 2014, 52, 1041–1052. [Google Scholar] [CrossRef] [PubMed]
- Liaw, A.; Wiener, M. Classification and regression by random forest. R News 2002, 2, 18–22. [Google Scholar]
- Scholkopf, B.; Sung, K.K.; Burges, C.J.; Girosi, F.; Niyogi, P.; Poggio, T.; Vapnik, V. Comparing support vector machines with Gaussian kernels to radial basis function classifiers. IEEE Trans. Signal Process. 1997, 45, 2758–2765. [Google Scholar] [CrossRef] [Green Version]
- Hall, M.A.; Smith, L.A. Practical Feature Subset Selection for Machine Learning. In Proceedings of the 21st Australasian Computer Science Conference ACSC’98, Perth, Australia, 4–6 February 1998; pp. 181–191. [Google Scholar]
- Borgatti, S.P.; Mehra, A.; Brass, D.J.; Labianca, G. Network analysis in the social sciences. Science 2009, 323, 892–895. [Google Scholar] [CrossRef] [Green Version]
- Hsu, H.H.; Hsieh, C.W.; Lu, M.D. Hybrid feature selection by combining filters and wrappers. Expert Syst. Appl. 2011, 38, 8144–8150. [Google Scholar] [CrossRef]
- Hamza, M.; Larocque, D. An empirical comparison of ensemble methods based on classification trees. J. Stat. Comput. Simul. 2005, 75, 629–643. [Google Scholar] [CrossRef]
- Breiman, L. Bagging predictors. Mach. Learn. 1996, 24, 123–140. [Google Scholar] [CrossRef] [Green Version]
- Raschka, S. Model evaluation, model selection, and algorithm selection in machine learning. arXiv 2018, arXiv:1811.12808. [Google Scholar]
- Bolón-Canedo, V.; Sánchez-Maroño, N.; Alonso-Betanzos, A. Recent advances and emerging challenges of feature selection in the context of big data. Knowl. Based Syst. 2015, 86, 33–45. [Google Scholar] [CrossRef]
- Wah, Y.B.; Ibrahim, N.; Hamid, H.A.; Abdul-Rahman, S.; Fong, S. Feature Selection Methods: Case of Filter and Wrapper Approaches for Maximising Classification Accuracy. Pertanika J. Sci. Technol. 2018, 26, 329–340. [Google Scholar]
- Lee, J.D.; Chang, T.C.; Yang, S.T.; Huang, C.H.; Hsieh, F.H.; Wu, C.Y. Prediction of quality of life after stroke reha-bilitation. Neuropsychiatry 2016, 6, 369–375. [Google Scholar]
- Oztekin, A.; Al-Ebbini, L.; Sevkli, Z.; Delen, D. A decision analytic approach to predicting quality of life for lung trans-plant recipients: A hybrid genetic algorithms-based methodology. Eur. J. Oper. Res. 2018, 266, 639–651. [Google Scholar] [CrossRef]
- Yan, X.; Su, X. Linear Regression Analysis: Theory and Computing; World Scientific: Singapore, 2009. [Google Scholar]
- Dietterich, T.G. Ensemble learning. In The Handbook of Brain Theory and Neural Networks; MIT Press: Cambridge, MA, USA, 2002; pp. 110–125. [Google Scholar]
- Agmon, M.; Shochat, T.; Kizony, R. Sleep quality is associated with walking under dual-task, but not single-task performance. Gait Posture 2016, 49, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Arfken, C.L.; Lach, H.W.; Birge, S.J.; Miller, J.P. The prevalence and correlates of fear of falling in elderly persons living in the community. Am. J. Public Health 1994, 84, 565–570. [Google Scholar] [CrossRef] [Green Version]
- Delbaere, K.; Crombez, G.; Vanderstraeten, G.; Willems, T.; Cambier, D. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing 2004, 33, 368–373. [Google Scholar] [CrossRef] [Green Version]
- Yardley, L.; Smith, H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 2002, 42, 17–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giannitsi, S.; Bougiakli, M.; Bechlioulis, A.; Kotsia, A.; Michalis, L.K.; Naka, K.K. 6-minute walking test: A useful tool in the management of heart failure patients. Ther. Adv. Cardiovasc. Dis. 2019, 13, 1753944719870084. [Google Scholar] [CrossRef] [Green Version]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar]
- Troosters, T.; Gosselink, R.; Decramer, M. Six minute walking distance in healthy elderly subjects. Eur. Respir. J. 1999, 14, 270–274. [Google Scholar] [CrossRef] [Green Version]
- Enright, P.L.; Sherrill, D.L. Reference equations for the six-minute walk in healthy adults. Am. J. Respir. Crit. Care Med. 1998, 158, 1384–1387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enright, P.L.; McBurnie, M.A.; Bittner, V.; Tracy, R.P.; McNamara, R.; Arnold, A.; Newman, A.B. The 6-min walk test: A quick measure of functional status in elderly adults. Chest 2003, 123, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Huijben, B.; Van Schooten, K.S.; Van Dieën, J.H.; Pijnappels, M. The effect of walking speed on quality of gait in older adults. Gait Posture 2018, 65, 112–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almarwani, M.; VanSwearingen, J.M.; Perera, S.; Sparto, P.J.; Brach, J.S. Challenging the motor control of walking: Gait variability during slower and faster pace walking conditions in younger and older adults. Arch. Gerontol. Geriatr. 2016, 66, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Rennie, L.; Löfgren, N.; Moe-Nilssen, R.; Opheim, A.; Dietrichs, E.; Franzén, E. The reliability of gait variability measures for individuals with Parkinson’s disease and healthy older adults–The effect of gait speed. Gait Posture 2018, 62, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Davids, J.R. Gait analysis: Normal and pathological function. J. Pediatr. Orthop. 1992, 12, 815. [Google Scholar] [CrossRef]
- Neptune, R.R.; Sasaki, K.; Kautz, S.A. The effect of walking speed on muscle function and mechanical energetics. Gait Posture 2008, 28, 135–143. [Google Scholar] [CrossRef] [Green Version]
- Hausdorff, J.M.; Yogev, G.; Springer, S.; Simon, E.S.; Giladi, N. Walking is more like catching than tapping: Gait in the elderly as a complex cognitive task. Exp. Brain Res. 2005, 164, 541–548. [Google Scholar] [CrossRef]
- Ayoubi, F.; Launay, C.P.; Annweiler, C.; Beauchet, O. Fear of falling and gait variability in older adults: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2015, 16, 14–19. [Google Scholar] [CrossRef]
- Lee, K. The floor: A reinterpretation of the Korean home, focusing on the ondol. Space Cult. 2021, 1206331220976486. [Google Scholar] [CrossRef]
- Patel, D.; Steinberg, J.; Patel, P. Insomnia in the elderly: A review. J. Clin. Sleep Med. 2018, 14, 1017–1024. [Google Scholar] [CrossRef]
- Manrique-Espinoza, B.; Salinas-Rodríguez, A.; Rosas-Carrasco, O.; Gutiérrez-Robledo, L.M.; Avila-Funes, J.A. Sarcopenia is associated with physical and mental components of health-related quality of life in older adults. J. Am. Med. Dir. Assoc. 2017, 18, 636.e1–636.e5. [Google Scholar] [CrossRef] [PubMed]

| Component | Model | CNoF | aRMSE | Std RMSE | Min RMSE | RMSE 25% | RMSE 50% | RMSE 75% | Max RMSE |
|---|---|---|---|---|---|---|---|---|---|
| Physical | LR_PV | 33 | 13.92776 | 0.68349 | 11.96545 | 13.50805 | 13.95991 | 14.44462 | 15.38411 |
| (a) LR_FI | 15 | 13.76088 | 0.71617 | 11.86612 | 13.29279 | 13.78654 | 14.24163 | 15.43223 | |
| RF_PV | 31 | 14.39872 | 0.73950 | 12.57450 | 13.91250 | 14.33669 | 14.98490 | 15.94272 | |
| RF_FI | 15 | 14.20864 | 0.68617 | 12.62523 | 13.68770 | 14.26701 | 14.74725 | 15.90077 | |
| SVM_PV | 8 | 14.76165 | 0.81308 | 12.99783 | 14.15996 | 14.79660 | 15.25064 | 17.17015 | |
| SVM_FI | 8 | 14.39575 | 0.82367 | 12.58128 | 13.84777 | 14.39586 | 15.01643 | 16.60752 | |
| Mental | (b) LR_PV | 12 | 11.36805 | 0.61973 | 9.53575 | 10.89313 | 11.37711 | 11.78536 | 12.96427 |
| LR_FI | 6 | 11.37025 | 0.70205 | 9.17258 | 10.86453 | 11.36144 | 11.82792 | 13.24375 | |
| RF_PV | 18 | 11.64159 | 0.59699 | 10.09463 | 11.21322 | 11.66051 | 12.00546 | 13.00478 | |
| RF_FI | 39 | 11.60706 | 0.62697 | 10.11383 | 11.11899 | 11.63986 | 11.98359 | 13.47048 | |
| SVM_PV | 4 | 11.79612 | 0.76560 | 10.14775 | 11.30421 | 11.70546 | 12.23328 | 13.82748 | |
| SVM_FI | 2 | 11.68649 | 0.75505 | 10.05444 | 11.15436 | 11.58823 | 12.22781 | 13.59275 |
| Physical Component (LR_FI, CNoF = 15). | Beta | Mental Component (LR_PV, CNoF = 12) | Beta |
|---|---|---|---|
| Demographic characteristics | Demographic characteristics | ||
| Age * | −1.88 | Total number of diseases * | −2.78 |
| Total number of diseases * | −3.63 | ||
| Questionnaires | Questionnaires | ||
| Stress response index-modified form (SRI-MF) * | −6.98 | SRI-MF * | −6.91 |
| Total Insomnia severity index (ISI) * | −5.08 | Total ISI * | −3.95 |
| Total Physical activities (PAs) * | 4.69 | Fear of falling * | −3.71 |
| Fear of falling * | −6.42 | ||
| Gait ability | Gait ability | ||
| Preferred speed_coefficient of variance (CV) Single-support phase | −3.28 | Faster speed_Walking speed | 2.92 |
| Faster speed_CV Single-support phase * | −3.53 | ||
| Slower speed_Stride time * | −0.54 | ||
| Physical fitness | Physical fitness | ||
| 6-min walking test (6MWT) * | 7.66 | 6MWT | 3.96 |
| Standing time (ST) from a long sitting position (LSP) * | −6.02 | Five times sit-to-stand * | −3.86 |
| 3-m Timed-up-and-go test right side | −6.83 | 3-m Timed-up-and-go test left side | −3.81 |
| Single-leg stance | 2.30 | 3-m Timed-up-and-go test right side | −3.61 |
| Five times sit-to-stand | −6.06 | Bicep curls right | 3.33 |
| Handgrip right side * | 5.11 | Bicep curls left | 3.24 |
| ST from LSP | −2.83 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.; Noh, Y.; Youm, C.; Kim, S.; Park, H.; Noh, B.; Kim, B.; Choi, H.; Yoon, H. Estimating Health-Related Quality of Life Based on Demographic Characteristics, Questionnaires, Gait Ability, and Physical Fitness in Korean Elderly Adults. Int. J. Environ. Res. Public Health 2021, 18, 11816. https://doi.org/10.3390/ijerph182211816
Lee M, Noh Y, Youm C, Kim S, Park H, Noh B, Kim B, Choi H, Yoon H. Estimating Health-Related Quality of Life Based on Demographic Characteristics, Questionnaires, Gait Ability, and Physical Fitness in Korean Elderly Adults. International Journal of Environmental Research and Public Health. 2021; 18(22):11816. https://doi.org/10.3390/ijerph182211816
Chicago/Turabian StyleLee, Myeounggon, Yoonjae Noh, Changhong Youm, Sangjin Kim, Hwayoung Park, Byungjoo Noh, Bohyun Kim, Hyejin Choi, and Hyemin Yoon. 2021. "Estimating Health-Related Quality of Life Based on Demographic Characteristics, Questionnaires, Gait Ability, and Physical Fitness in Korean Elderly Adults" International Journal of Environmental Research and Public Health 18, no. 22: 11816. https://doi.org/10.3390/ijerph182211816











