Assessment of the Range of Movement of the Lower Limb in Sport: Advantages of the ROM-SPORT I Battery
Abstract
:1. Introduction
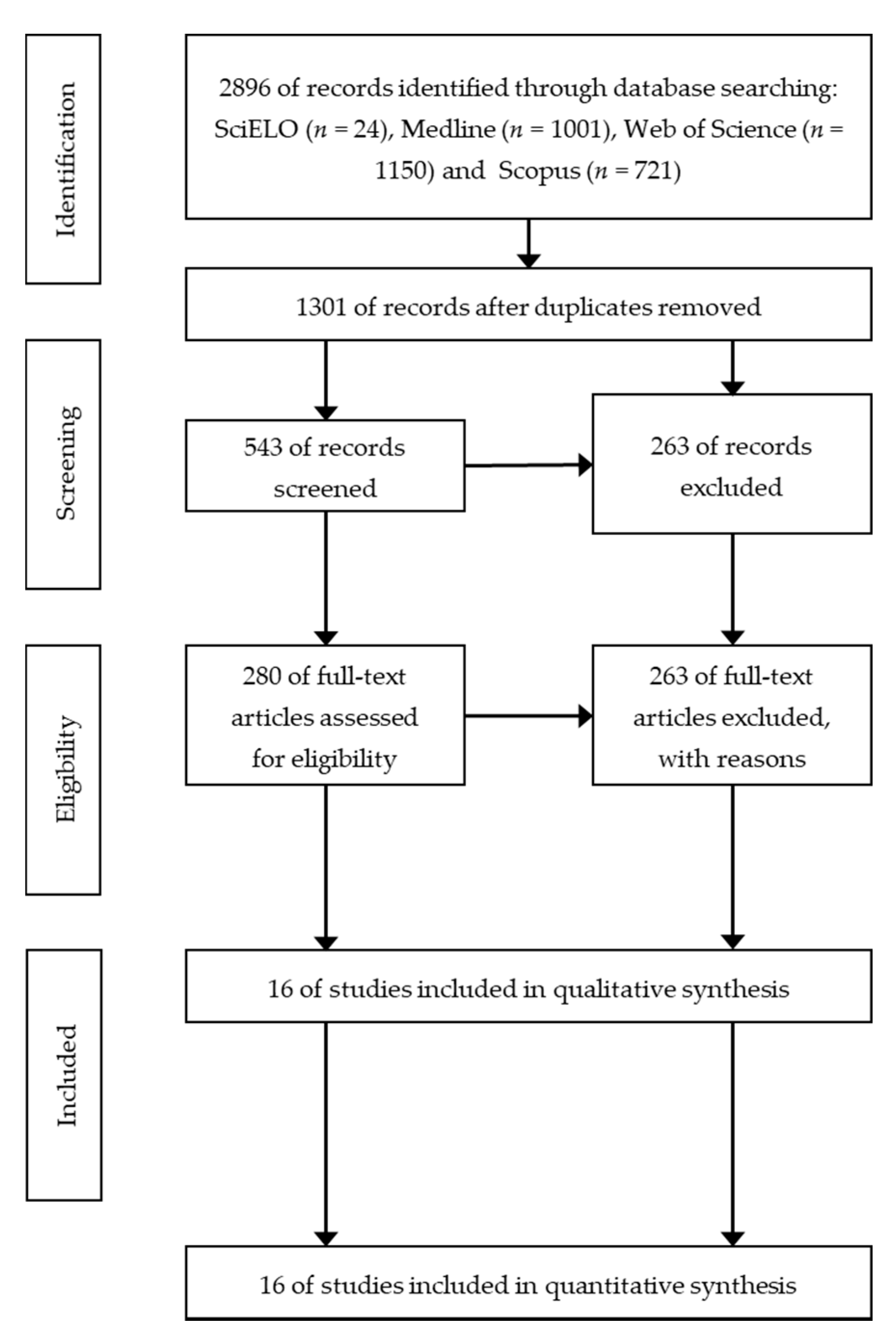
2. Methods
Systematic Review
3. Results
3.1. Estimated Time for Testing
3.2. Warm-Up before Testing
3.3. Participant’s Starting Position
3.4. Movement Testing
3.5. Measurement Procedure (Instruments, Material and Human Resources)
3.6. Types of ROM Evaluated
3.7. Criteria for End-Of Test
3.8. Control of Compensatory Movements
3.9. Number of Assessment Sessions and Repetitions
3.10. Validity
3.11. Reliability
4. Discussion
5. Practical Guidelines
- −
- To accurately quantify the ROM measures of the major lower extremity joints (hip, knee, and ankle);
- −
- To identify athletes with limited or restricted joint ROM values. This knowledge may help in the decision-making process regarding the identification of athletes at high risk of sustaining an injury (mainly soft tissue injury);
- −
- To detect those athletes (e.g., rhythmic gymnasts, figure skaters, and diving) that should improve their ROM values to successfully perform the technical actions that are awarded the highest points by a judge;
- −
- To monitor the efficacy of intervention programs (e.g., stretching exercises and foam rolling) designed to maintain or improve lower extremity joints ROM;
- −
- Furthermore, in rehabilitation processes, the ROM-SPORT I battery may be used to determine if the ROM of the injured joint has been fully restored, which may help to achieve a safe return to play (athletes) or activities of daily life (general population).
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Holt, L.; Pelham, T.; Holt, J. Flexibility: A Concise Guide To Conditioning, Performance Enhancement, Injury Prevention, and Rehabilitation; Humana Press: Totowa, NJ, USA, 2009. [Google Scholar]
- Magnusson, P.; Renström, P. The European College of Sports Sciences position statement: The role of stretching exercises in sports. Eur. J. Sport Sci. 2006, 6, 87–91. [Google Scholar] [CrossRef]
- García-Pinillos, F.; Ruiz-Ariza, A.; Moreno del Castillo, R.; Latorre-Román, P. Impact of limited hamstring flexibility on vertical jump, kicking speed, sprint, and agility in young football players. J. Sports Sci. 2015, 33, 1293–1297. [Google Scholar] [CrossRef] [PubMed]
- Hahn, T.; Foldspang, A.; Vestergaard, E.; Ingemann-Hansen, T. Active knee joint flexibility and sports activity. Scand. J. Med. Sci. Sports 1999, 9, 74–80. [Google Scholar] [CrossRef]
- De la Fuente, A.; Gómez-Landero, L. Motor differences in cadet taekwondo athletes according to competition level. Rev. Int. Med. Cienc. Act. Fis. Deport. 2019, 19, 63–75. [Google Scholar] [CrossRef]
- Gerhardt, J.; Cocchiarella, L.; Lea, R. The Practical Guide to Range of Motion Assessment; American Medical Association: Chicago, IL, USA, 2002. [Google Scholar]
- Cejudo, A.; Robles-Palazón, F.; Sainz De Baranda, P. Fútbol sala de élite: Diferencias de flexibilidad según sexo. E-Balonmano.com Rev. Cienc. Deport. 2019, 15, 37–48. [Google Scholar]
- Verrall, G.; Slavotinek, J.; Barnes, P.; Esterman, A.; Oakeshott, R.; Spriggins, A. Hip joint range of motion restriction precedes athletic chronic groin injury. J. Sci. Med. Sport 2007, 10, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Arnason, A.; Sigurdsson, S.; Gudmundsson, A.; Holme, I.; Engebretsen, L.; Bahr, R. Risk Factors for Injuries in Football. Am. J. Sports Med. 2004, 32 (Suppl. S1), 5S–16S. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Murrell, G.; Knapman, P. Adductor Strain and Hip Range of Movement in Male Professional Soccer Players. J. Orthop. Surg. 2007, 15, 46–49. [Google Scholar] [CrossRef]
- Shah, S.; Testa, E.; Gammal, I.; Sullivan, J.; Gerland, R.; Goldstein, J.; Cohn, R. Hip Range of Motion: Which Plane of Motion Is More Predictive of Lower Extremity Injury in Elite Soccer Players? A Prospective Study. J. Surg. Orthop. Adv. 2019, 28, 201–208. [Google Scholar]
- Witvrouw, E.; Danneels, L.; Asselman, P.; D’Have, T.; Cambier, D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players: A prospective study. Am. J. Sports Med. 2003, 31, 41–46. [Google Scholar] [CrossRef]
- Okamura, S.; Wada, N.; Tazawa, M.; Sohmiya, M.; Ibe, Y.; Shimizu, T.; Usuda, S.; Shirakura, K. Injuries and disorders among young ice skaters: Relationship with generalized joint laxity and tightness. Open Access J. Sport. Med. 2014, 5, 191–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Witvrouw, E.; Bellemans, J.; Lysens, R.; Danneels, L.; Cambier, D. Intrinsic Risk Factors for the Development of Patellar Tendinitis in an Athletic Population. Am. J. Sports Med. 2001, 29, 190–195. [Google Scholar] [CrossRef]
- VandenBerg, C.; Crawford, E.; Enselman, E.; Robbins, B.; Wojtys, E.; Bedi, A. Restricted Hip Rotation Is Correlated With an Increased Risk for Anterior Cruciate Ligament Injury. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Murray, E.; Birley, E.; Twycross-Lewis, R.; Morrissey, D. The relationship between hip rotation range of movement and low back pain prevalence in amateur golfers: An observational study. Phys. Ther. Sport 2009, 10, 131–135. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Cejudo, A.; Ayala, F.; Santonja, F. Perfil óptimo de flexibilidad del miembro inferior en jugadoras de fútbol sala. Rev. Int. Med. Cienc. Act. Fis. Deport. 2015, 15, 647–662. [Google Scholar] [CrossRef] [Green Version]
- Vad, V.; Bhat, A.; Basrai, D.; Gebeh, A.; Aspergren, D.; Andrews, J. Low Back Pain in Professional Golfers: The Role of Associated Hip and Low Back Range-of-Motion Deficits. Am. J. Sports Med. 2004, 32, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Witvrouw, E.; Van Tiggelen, D.; Willems, T. Risk factors and prevention of anterior knee pain. In Anterior Knee Pain and Patellar Instability; Springer: London, UK, 2005; pp. 135–145. [Google Scholar] [CrossRef]
- Koga, H.; Nakamae, A.; Shima, Y.; Bahr, R.; Krosshaug, T. Hip and Ankle Kinematics in Noncontact Anterior Cruciate Ligament Injury Situations Video Analysis Using Model-Based Image Matching. Am. J. Sports Med. 2018, 46, 333–340. [Google Scholar] [CrossRef]
- McLean, S.; Walker, K.; van den Bogert, A.; den Bogert, V. Effect of Gender on Lower Extremity Kinematics during Rapid Direction Changes: An Integrated Analysis of Three Sports Movements. J. Sci. Med. Sport 2005, 8, 411–422. [Google Scholar] [CrossRef] [Green Version]
- Herrington, L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee 2014, 21, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Kawałek, K.; Garsztka, T. An analysys of muscle balance in professional field hockey players. TRENDS Sport Sci. 2013, 4, 181–187. [Google Scholar]
- Cejudo, A.; Moreno-Alcaraz, V.J.; Izzo, R.; Santonja-Medina, F.; Sainz de Baranda, P. External and Total Hip Rotation Ranges of Motion Predispose to Low Back Pain in Elite Spanish Inline Hockey Players. Int. J. Environ. Res. Public Health 2020, 17, 4858. [Google Scholar] [CrossRef] [PubMed]
- Butler, D.; Moseley, G. Explain Pain Course Description, 2nd ed.; Noigroup publications: Adelaide, Australia, 2013. [Google Scholar]
- Fridén, J.; Lieber, R. Eccentric exercise-induced injuries to contractile and cytoskeletal muscle fibre components. Acta Physiol. Scand. 2001, 171, 321–326. [Google Scholar] [CrossRef] [Green Version]
- Worrell, T.; Perrin, D. Hamstring muscle injury: The influence of strength, flexibility, warm-up, and fatigue. J. Orthop. Sports Phys. Ther. 1992, 16, 12–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Battista, R.; Pivarnik, J.; Dummer, G.; Sauer, N.; Malina, R. Comparisons of physical characteristics and performances among female collegiate rowers. J. Sports Sci. 2007, 25, 651–657. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, J.; Pérez, A.; Boada, P.; García, M.; Moreno, C.; Carretero, M. Estudio de la flexibilidad de luchadores de kickboxing de nivel internacional. Arch. Med. Deport. 2014, 31, 85–91. [Google Scholar]
- Newlands, C.; Reid, D.; Parmar, P. The prevalence, incidence and severity of low back pain among international-level rowers. Artic. Br. J. Sport. Med. 2015, 49, 951–956. [Google Scholar] [CrossRef]
- Wattie, N.; Cobley, S.; Macpherson, A.; Howard, A.; Montelpare, W.; Baker, J. Injuries in Canadian youth ice hockey: The influence of relative age. Pediatrics 2007, 120, 142–148. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.; Garraway, M. Epidemiological comparison of injuries in school and senior club rugby. Br. J. Sport. Med. 1996, 30, 213–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orchard, J.; Wood, T.; Seward, H.; Broad, A. Comparison of injuries in elite senior and junior Australian football. J. Sci. Med. Sport 1998, 1, 83–88. [Google Scholar] [CrossRef]
- Hogg, J.; Schmitz, R.; Nguyen, A.; Shultz, S. Lumbo-Pelvic-Hip Complex Passive Hip Range-of-Motion Values Across Sex and Sport. J. Athl. Train. 2018, 53, 560–567. [Google Scholar] [CrossRef]
- Moreno, A.; Gómez, E.; Martín, A. Valoración de la flexibilidad de tronco mediante el test del cajón en diferentes modalidades deportivas. Sel. Rev. Esp. Iberoam. Med. Educ. Fis. Deport. 2004, 13, 148–154. [Google Scholar]
- Kang, M.-H.; Park, K.-H.; Oh, J.-S. Association of Ankle Kinematics and Performance on the Y-Balance Test with Inclinometer Measurements on the Weight-Bearing-Lunge Test. J. Sport Rehabil. 2015, 24, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Aslan, H.; Buddhadev, H.; Suprak, D.; San Juan, J. Acute effects of two hip flexor stretching techniques on knee joint position sense and balance. Int. J. Sports Phys. Ther. 2018, 13, 846–859. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Etnyre, B.; Poindexter, H.; Sokol, D.; Toon, T. Flexibility characteristics of elite female and male volleyball players. J. Sports Med. Phys. Fit. 1989, 29, 49–51. [Google Scholar]
- Faiss, R.; Terrier, P.; Praz, M.; Fuchslocher, J.; Gobelet, C.; Deriaz, O. Influence of Initial Foot Dorsal Flexion on Vertical Jump and Running Performance. Artic. J. Strength Cond. Res. 2009, 24, 2352–2357. [Google Scholar] [CrossRef]
- Cejudo, A.; Sainz De Baranda, P.; Ayala, F.; Santonja, F. Normative data of lower-limb muscle flexibility in futsal players. Rev. Int. Med. Cienc. Act. Fis. Deport. 2014, 14, 509–525. [Google Scholar]
- Chandler, T.; Kibler, W.; Uhl, T.; Wooten, B.; Kiser, A.; Stone, E. Flexibility comparisons of junior elite tennis players to other athletes. Am. J. Sports Med. 1990, 18, 134–136. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, A.; Moreno-Alcaraz, V.J.; Croix, M.D.S.; Santonja-Medina, F.; Sainz de Baranda, P. Lower-Limb Flexibility Profile Analysis in Youth Competitive Inline Hockey Players. Int. J. Environ. Res. Public Health 2020, 17, 4338. [Google Scholar] [CrossRef]
- Oberg, B.; Ekstrand, J.; Moller, M.; Gillquist, J. Muscle strength and flexibility in different positions of soccer players. Int. J. Sports Med. 1984, 5, 213–216. [Google Scholar] [CrossRef]
- Bloomfield, J.; Polman, R.; O´Donoghue, P. Physical demands of different positions in FA Premier League soccer. J. Sport. Sci. Med. 2007, 6, 63–70. [Google Scholar]
- Cejudo, A.; Robles-Palazón, F.; Ayala, F.; De Ste Croix, M.; Ortega-Toro, E.; Santonja, F.; Sainz de Baranda, P. Age-related differences in flexibility in soccer players 8-19 years old. PeerJ 2019, 2019, e6236. [Google Scholar] [CrossRef]
- Ellenbecker, T.; Ellenbecker, G.; Roetert, E.; Silva, R.; Keuter, G.; Sperling, F. Descriptive profile of hip rotation range of motion in elite tennis players and professional baseball pitchers. Am. J. Sports Med. 2007, 35, 1371–1376. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, N.; Ocarino, J.; Sorrentino, F.; Jales, F.; Gabriel, S.; Mendonça, L.; Fonseca, S. Normative data for muscle flexibility in male soccer players. Br. J. Sports Med. 2014, 48, 568–569. [Google Scholar] [CrossRef]
- Gannon, L.; Bird, H.; Gan Non, L. The quantification of joint laxity in dancers and gymnasts The quantification of joint laxity in dancers and gymnasts. J. Sports Sci. 1999, 17, 743–750. [Google Scholar] [CrossRef]
- Cejudo, A. El perfil óptimo de flexibilidad en jóvenes jugadores de fútbol durante su periodo sensible del desarrollo físico. Batería ROM-SPORT. JUMP 2020, 2, 16–25. [Google Scholar] [CrossRef]
- Bradley, P.; Portas, M. The relationship between preseason range of motion and muscle strain injury in elite soccer players. J. Strength Cond. Res. 2007, 21, 1155–1159. [Google Scholar]
- Gabbe, B.; Bennell, K.; Wajswelner, H.; Finch, C. Reliability of common lower extremity musculoskeletal screening tests. Phys. Ther. Sport 2004, 5, 90–97. [Google Scholar] [CrossRef]
- Cejudo, A.; Moreno-Alcaraz, V.J.; Izzo, R.; Robles-Palazón, F.J.; Sainz de Baranda, P.; Santonja-Medina, F. Flexibility in Spanish Elite Inline Hockey Players: Profile, Sex, Tightness and Asymmetry. Int. J. Environ. Res. Public Health 2020, 17, 3295. [Google Scholar] [CrossRef] [PubMed]
- Fourchet, F.; Materne, O.; Horobeanu, C.; Hudacek, T.; Buchheit, M. Reliability of a novel procedure to monitor the flexibility of lower limb muscle groups in highly-trained adolescent athletes. Phys. Ther. Sport 2013, 14, 28–34. [Google Scholar] [CrossRef]
- Bozic, P.; Pazin, N.; Berjan, B.; Planic, N.; Cux, I. Evaluation of the field tests of flexibility of the lower extremity: Reliability and the concurrent and factorial validity. J. Strength Cond. Res. 2010, 24, 2523–2531. [Google Scholar] [CrossRef]
- Ekstrand, J.; Gillquist, J. The frequency of muscle tightness and injuries in soccer players. Am. J. Sports Med. 1982, 10, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Nussbaumer, S.; Leunig, M.; Glatthorn, J.; Stauffacher, S.; Gerber, H.; Maffiuletti, N. Validity and test-retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet. Disord. 2010, 11, 194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norkin, C.; White, D. Measurement of Joint Motion: A Guide to Goniometry; FA Davis: Philadelphia, PA, USA, 2016. [Google Scholar]
- Hopkins, W.; Marshall, S.; Batterham, A.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sport. Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopkins, W. How to interpret changes in an athletic performance test. Sport Sci. 2004, 8, 1–7. [Google Scholar]
- Cejudo, A. Deporte y Flexibilidad: Rendimiento Deportivo sin Riesgo de Lesión. Ph.D. Thesis, Universidad de Murcia, Murcia, Spain, 2015. [Google Scholar]
- Sainz De Baranda, P.; Cejudo, A.; Ayala, F.; Santonja, F. Perfil de flexibilidad de la extremidad inferior en jugadoras senior de fútbol sala. Rev. Esp. Educ. Fis. Deport. 2015, 409, 35–48. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Cejudo, A.; Sainz de Baranda, P.; Ayala, F.; Santonja, F. Test-retest reliability of seven common clinical tests for assessing lower extremity muscle flexibility in futsal and handball players. Phys. Ther. Sport 2015, 16, 107–113. [Google Scholar] [CrossRef]
- Möller, M.; Öberg, B.; Gillquist, J. Effect of Stretching on Range of Motion in the Lower Extremity in Connection with Soccer Training. Int. J. Sports Med. 1985, 6, 50–52. [Google Scholar] [CrossRef]
- Reid, D.C.; Burnham, R.S.; Saboe, L.A.; Kushner, S.F. Lower extremity flexibility patterns in classical ballet dancers and their correlation to lateral hip and knee injuries. Am. J. Sports Med. 1987, 15, 347–352. [Google Scholar] [CrossRef]
- Clapper, M.; Wolf, S. Comparison of the reliability of the Orthoranger and the standard goniometer for assessing active lower extremity range of motion. Phys. Ther. 1988, 68, 214–218. [Google Scholar] [CrossRef]
- Wang, S.; Whitney, S.; Burdett, R.; Janosky, J. Lower extremity muscular flexibility in long distance runners. J. Orthop. Sports Phys. Ther. 1993, 17, 102–107. [Google Scholar] [CrossRef] [Green Version]
- Gogia, P.; Braatz, J.; Rose, S.; Norton, B. Reliability and Validity of Goniometric Measurements at the Knee. Phys. Ther. 1987, 67, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Hershkovitz, I.; Peleg, S.; Dar, G.; Masharawi, Y.; Heim, M.; Siev-Ner, I. Range of joint movement in female dancers and nondancers aged 8 to 16 years: Anatomical and clinical implications. Am. J. Sports Med. 2006, 34, 814–823. [Google Scholar] [CrossRef] [PubMed]
- Pua, Y.; Wrigley, T.; Cowan, S.; Bennell, K. Intrarater test-retest reliability of hip range of motion and hip muscle strength measurements in persons with hip osteoarthritis. Arch. Phys. Med. Rehabil. 2008, 89, 1146–1154. [Google Scholar] [CrossRef]
- Tainaka, K.; Takizawa, T.; Kobayashi, H.; Umimura, M. Limited hip rotation and non-contact anterior cruciate ligament injury: A case–control study. Knee 2014, 21, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, A.; Ayala, F.; Sainz de Baranda, P.; Santonja, F. Reliability of two methods of clinical examination of the flexibility of the hip adductor muscles. Int. J. Sports Phys. Ther. 2015, 10, 976–983. [Google Scholar]
- Grazette, N.; McAllister, S.; Ong, C.W.; Sunderland, C.; Nevil, M.E.; Morri, J.G. Reliability of a musculoskeletal profiling test battery in elite academy soccer players. PLoS ONE 2020, 15, e0236341. [Google Scholar] [CrossRef]
- Ekstrand, J.; Wiktorsson, M.; Oberg, B.; Gillquist, J. Lower extremity goniometric measurements: A study to determine their reliability. Arch. Phys. Med. Rehabil. 1982, 63, 171–175. [Google Scholar]
- Enwemeka, C. Radiographic verification of knee goniometry. Scand. J. Rehabil. Med. 1986, 18, 47–49. [Google Scholar]
- Greene, W.; Heckman, J. Clinical Assessment of Joint Movement; Edika Med.: Barcelona, Spain, 1997. [Google Scholar]
- Hopkins, W. Measures of Reliability in Sports Medicine and Science. Sport. Med. 2000, 30, 1–15. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.; Cosgrave, C. To stretch or not to stretch: The role of stretching in injury prevention and performance. Scand. J. Med. Sci. Sports 2009, 20, 169–181. [Google Scholar] [CrossRef]
- Iwata, M.; Yamamoto, A.; Matsuo, S.; Hatano, G.; Miyazaki, M.; Fukaya, T.; Fujiwara, M.; Asai, Y.; Suzuki, S. Dynamic Stretching Has Sustained Effects on Range of Motion and Passive Stiffness of the Hamstring Muscles. J. Sport. Sci. Med. 2019, 18, 13–20. [Google Scholar]
- Magnusson, S.; Simonsen, E.; Aagaard, P.; Gleim, G.; McHugh, M.; Kjaer, M. Viscoelastic response to repeated static stretching in the human hamstring muscle. Scand. J. Med. Sci. Sports 1995, 5, 342–347. [Google Scholar] [CrossRef]
- Ayala, F.; Moreno-Perez, V.; Vera-Garcia, F.; Moya, M.; Sanz-Rivas, D.; Fernandez-Fernandez, J. Acute and time-course effects of traditional and dynamic warm-up routines in young elite junior tennis players. PLoS ONE 2016, 11, e0152790. [Google Scholar] [CrossRef] [Green Version]
- Magee, D. Orthopedic Physical Assessment; Elsevier Health Sciences: Philadelphia, PA, USA, 2013. [Google Scholar]
- Cejudo, A.; Ginés-Díaz, A.; Sainz de Baranda, P. Asymmetry and Tightness of Lower Limb Muscles in Equestrian Athletes: Are They Predictors for Back Pain? Symmetry (Basel) 2020, 12, 1679. [Google Scholar] [CrossRef]
- Santonja-Medina, F.; Santonja-Renedo, S.; Cejudo, A.; Ayala, F.; Ferrer, V.; Pastor, A.; Collazo-Diéguez, M.; Rodríguez-Ferrán, O.; Andújar, P.; Sainz de Baranda, P. Straight Leg Raise Test: Influence of Lumbosant© and Assistant Examiner in Hip, Pelvis Tilt and Lumbar Lordosis. Symmetry (Basel) 2020, 12, 927. [Google Scholar] [CrossRef]
- Bohannon, R.; Gajdosik, R.; Leveau, B. Contribution of pelvic and lower limb motion to increases in the angle of passive straight leg raising. Phys. Ther. 1985, 65, 474–476. [Google Scholar] [CrossRef]
- Cameron, D.; Bohannon, R.; Owen, S. Influence of hip position on measurements of the straight leg raise test. J. Orthop. Sports Phys. Ther. 1994, 19, 168–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cejudo, A.; Sainz De Baranda, P.; Ayala, F.; Santonja, F. A simplified version of the weight-bearing ankle lunge test: Description and test-retest reliability. Man. Ther. 2014, 19, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Fredriksen, H.; Dagfinrud, H.; Jacobsen, V.; Maehlum, S. Passive knee extension test to measure hamstring muscle tightness. Scand. J. Med. Sci. Sports 1997, 7, 279–282. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz de Baranda, P.; De Ste Croix, M.; Santonja, F. Reproducibility and criterion-related validity of the sit and reach test and toe touch test for estimating hamstring flexibility in recreationally active young adults. Phys. Ther. Sport 2012, 13, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Jiménez, F.; Ayala, F.; Cejudo, A.; Sainz de Baranda, P.; Santonja, F. Efecto del nivel de experiencia clínica del examinador sobre la validez de criterio y fiabilidad inter-sesión de cinco medidas del rango de movimiento de la flexión. Cuad. Psicol. del Deport. 2015, 15, 123–134. [Google Scholar] [CrossRef] [Green Version]
- Robles-Palazón, F.; Ayala, F.; Cejudo, A.; De Ste Croix, M.; Sainz de Baranda, P.; Santonja, F. Effects of age and maturation on lower extremity range of motion in male youth soccer players. J. Strength Cond. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- López-Valenciano, A.; Ayala, F.; Vera-García, F.; De Ste Croix, M.; Hernández-Sánchez, S.; Ruiz-Pérez, I.; Cejudo, A.; Santonja, F. Comprehensive profile of hip, knee and ankle ranges of motion in professional football players. J. Sports Med. Phys. Fit. 2019, 59, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Rey, E.; Padrón-Cabo, A.; Barcala-Furelos, R.; Mecías-Calvo, M. Effect of High and Low Flexibility Levels on Physical Fitness and Neuromuscular Properties in Professional Soccer Players. Int. J. Sports Med. 2016, 37, 878–883. [Google Scholar] [CrossRef]
- Fousekis, K.; Tsepis, E.; Poulmedis, P.; Athanasopoulos, S.; Vagenas, G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: A prospective study of 100 professional players. Br. J. Sports Med. 2011, 45, 709–714. [Google Scholar] [CrossRef] [Green Version]
- Ayala, F.; Sainz de Baranda, P.; De Ste Croix, M.; Santonja, F. Comparison of active stretching technique in males with normal and limited hamstring flexibility. Phys. Ther. Sport 2013, 14, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Santonja, F.; Sainz De Baranda, P.; García, P.; López-Miñarro, P.; Jordana, M. Effects of frequency of static stretching on straight-leg raise in elementary school children. J. Sport. Med. Phys. Fit. 2007, 47, 304–308. [Google Scholar]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar]
- Perret, C.; Poiraudeau, S.; Fermanian, J.; Colau, M.; Benhamou, M.; Revel, M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch. Phys. Med. Rehabil. 2001, 82, 1566–1570. [Google Scholar] [CrossRef]
| Reference | Estimate Time for Testing | Warm-up before Testing | Participant´s Starting Position | Movement Testing | Measurement Procedure (Instruments, Material and Human Resources) | Types of Range of Movement (ROM) Evaluated | Criteria for End-of Test | Control of Compensatory Movements | Number of Assessment Sessions and Repetitions | Validity | Reliability |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ekstrand et al. [55] | No detail | No | Supine | Hip extension | 2-examiners Velcro bands Anatomical landmark Standard GM Leighton flexometer | Passive | Maximum ROM | APT | 2 testing sessions 1 rep | No detail | CV = 1.2% |
| Supine | Hip flexion, knee extension | PPT Contralateral hip flexion | CV = 1.4% | ||||||||
| Supine | Hip abduction, knee flexion | No detail | CV = 2.5% | ||||||||
| Supine | Knee flexion | APT | CV = 1.1% | ||||||||
| Standing | Ankle dorsiflexion, neutral knee | Knee flexion, heel on the ground | CV = 2.5% | ||||||||
| Standing | Ankle dorsiflexion, maximum knee flexion | Heel on the ground | CV = 2.6% | ||||||||
| Moller et al. [64] | No detail | Yes | Supine | Hip extension | 2-examiners Velcro bands Anatomical landmark Standard GM | Passive | Maximum ROM | APT | 2 testing sessions 1 rep | No detail | CV = 1.2% |
| Supine | Hip flexion, knee extension | PPT, contralateral hip flexion | CV = 1.4% | ||||||||
| Supine | Hip abduction, knee flexion | No detail | CV = 2.5% | ||||||||
| Supine | Knee flexion | APT | CV = 1.1% | ||||||||
| Standing | Ankle dorsiflexion, neutral knee | Knee flexion, heel on the ground | CV = 2.5% | ||||||||
| Standing | Ankle dorsiflexion, maximum knee flexion | Heel on the ground | CV = 2.6% | ||||||||
| Reid et al. [65] | No detail | Yes | Supine | Hip extension, knee relax | 2-examiners Velcro bands Anatomical landmark Standard GM | Passive | Compensation movements | APT | 3 testing sessions, alternate days 3 reps | No detail | CV = 4.3% |
| Supine | Hip flexion, knee flexion | No detail | No detail | ||||||||
| Supine | Hip abduction, neutral knee | No detail | No detail | ||||||||
| Lateral | Hip adduction (Ober test) | No detail | No detail | ||||||||
| Sitting | Hip internal rotation | No detail | No detail | ||||||||
| Sitting | Hip external rotation | No detail | No detail | ||||||||
| Clapper et al. [66] | No detail | No detail | Supine | Hip flexion | 2-examiners Anatomical landmark Standard GM Orthoranger pendulum oriented perpendicular to the long axis of the moving segment | Active | No detail | No detail | 3 testing sessions (3-week apart) 3 reps | No detail | ICC GM = 0.95 ICC ORR = 0.89 |
| Prone | Hip extension, neutral knee | ICC GM = 0.83 ICC ORR = 0.72 | |||||||||
| Standing | Hip abduction | ICC GM = 0.86 ICC ORR = 0.79 | |||||||||
| Standing | Hip adduction | ICC GM = 0.80 ICC ORR = 0.77 | |||||||||
| Supine | Hip internal rotation | ICC GM = 0.92 ICC ORR = 0.86 | |||||||||
| Supine | Hip external rotation | ICC GM = 0.80 ICC ORR = 0.86 | |||||||||
| Supine | Knee flexion | ICC GM = 0.95 ICC ORR = 0.91 | |||||||||
| Supine | Knee extension | ICC GM = 0.85 ICC ORR = 0.80 | |||||||||
| Supine | Ankle dorsiflexion | ICC GM = 0.92 ICC ORR = 0.80 | |||||||||
| Supine | Ankle plantar flexion | ICC GM = 0.96 ICC ORR = 0.93 | |||||||||
| Wang et al. [67] | No detail | Yes | Supine | Hip extension, neutral knee | 2-examiners Bledsoe knee brace Anatomical landmark Standard GM | Passive | Compensation movements | APT | 2 testing sessions (1–2 days apart) No detail | No detail | ICC = 0.97 |
| Supine | Hip extension, 90° knee flexion | No detail | ICC = 0.97 | ||||||||
| Supine | Hip flexion, neutral knee | PPT | ICC = 0.90 | ||||||||
| Supine | Ankle dorsiflexion, neutral knee | Maximun ROM | No detail | ICC = 0.98 | |||||||
| Prone | Ankle dorsiflexion, 90° knee flexion | No detail | ICC = 0.93 | ||||||||
| Witvrouw et al. [12] | No detail | No detail | Supine | Hip flexion, knee flexion | 2-examiners Anatomical landmark Standard GM | Passive | No detail | No detail | No detail | Based on the study by Gogia et al. [68] | No detail |
| Supine | Hip abduction | Compensation movements | Hip rotation | ||||||||
| Prone | Knee flexion | Maximum ROM | No detail | ||||||||
| Standing | Ankle dorsiflexion, neutral knee | Compensation movements | Heel on the floor | ||||||||
| Steinberg et al. [69] | No detail | No | Prone | Hip extension, knee extension | 2-examiners Anatomical landmark Standard GM | Active | Compensation movements | Stabilized pelvis | Two testing sessions (1 day apart) consecutive days No detail | No detail | Pearson r = 0.91 |
| Supine | Hip abduction, knee extension | Passive | Hip rotation | Pearson r = 0.96 | |||||||
| Prone | Hip internal rotation, 90° knee flexion | Stabilized pelvis | Pearson r = 0.89 | ||||||||
| Prone | Hip external rotation, 90° knee flexion | Stabilized pelvis | Pearson r = 0.89 | ||||||||
| Supine | Hip flexion, knee flexion | PPT | Pearson r = 0.95 | ||||||||
| Supine | Knee flexion | No | Pearson r = 0.93 | ||||||||
| Supine | Ankle dorsiflexion, neutral knee | Passive | Compensation movements | Ankle and foot neutral position | Pearson r = 0.90 | ||||||
| Supine | Ankle plantarflexion, neutral knee | Pearson r = 0.91 | |||||||||
| Bradley and Portas [50] | No detail | No detail | Prone | Hip extension, neutral knee | 2-examiners Reflective skin markers Software for 2-dimensional image-based analysis Video camera | Passive | Feeling of stretching | No detail | No detail 1 rep | No detail | ICC Hip = 0.92 |
| Supine | Hip flexion, flexion knee | ||||||||||
| Supine | Knee flexion, hip flexion | ICC knee = 0.95 | |||||||||
| Supine | Knee extension, hip flexion | ||||||||||
| Supine | Ankle plantarflexion, neutral knee | ICC ankle = 0.91 | |||||||||
| Supine | Ankle dorsiflexion, neutral knee | ||||||||||
| Pua et al. [70] | No detail | No detail | Supine | Hip extension, 80° flexion knee | 1-examiner Strap Anatomical landmark Extendable GM Electronic inclinometer | Passive | Firm end sensation Presence of pain | PPT, flattened lumbar spine | 2 testing sessions (at least 1 week) 2 reps | No detail | MDC (90% IC) = 10.5° |
| Supine | Hip extension, knee unconstrained | MDC (90% IC) = 11° | |||||||||
| Supine | Hip abduction, neutral knee | Stabilized pelvis | MDC (90% IC) = 7.3° | ||||||||
| Sitting | Hip internal rotation | No detail | MDC (90% IC) = 7.8° | ||||||||
| Sitting | Hip external rotation | MDC (90% IC) = 7.1° | |||||||||
| Supine | Hip flexion, flexion knee | APT, contralateral hip flexion | MDC (90% IC) = 8.2° | ||||||||
| Bozic et al. [54] | 25 min/group muscle | Yes | Supine | Hip abduction, neutral knee | 2-examiners (a) Anatomical landmark Kinanthropometry, ruler and protractor Trigonometric calculations (b) Reflective markers 3D kinematic analysis system | Passive | Maximum ROM | No detail | 2 testing sessions (1 week apart) 3 reps | Concurrent validity 3D kinematic analysis system vs Field methods ICC: 0.66 to 0.96 CV: 0.8 to 3.5% | ICC = 0.87; CV = 3.4% |
| Supine | Hip flexion, neutral knee | ICC = 0.87; CV = 2.1% | |||||||||
| Standing | Single-legged knee bend | Active | ICC = 0.57; CV = 3.9% | ||||||||
| Standing | Sideward leg splits | Active | ICC = 0.89; CV = 2.3% | ||||||||
| Sitting | Sit and reach | Passive | ICC = 0.94; CV = 6.7% | ||||||||
| Standing | Sideways leg splits | Active | ICC = 0.88; CV = 2.4% | ||||||||
| Standing | Lengthwise leg splits | Active | ICC = 0.85; CV = 3% | ||||||||
| Nussbaumer et al. [56] | No detail | No detail | Supine | Hip adduction, neutral knee | 2-examiners (a) Anatomical landmark Standard GM Longitudinal axis (b) Anatomical landmark and sensor location ETS (electromagnetic tracking system) | Passive | Force application | No detail | 2 testing sessions (1 week apart) 3 reps | Concurrent validity LOA: 3.3° ICC:0.53 | GM (ICC = 0.84; CV = 6.7%) ETS (ICC = 0.82; CV = 6.3%) |
| Hip abduction, knee extension | Concurrent validity LOA: 1.9° ICC:0.93 | GM (ICC = 0.92; CV = 5.8%) ETS (ICC = 0.94; CV = 5.6%) | |||||||||
| Hip internal rotation, 90° hip and knee flexion | Concurrent validity LOA: 8.1° ICC:0.87 | GM (ICC = 0.95; CV = 7.7%) ETS (ICC = 0.90; CV = 10.2%) | |||||||||
| Hip external rotation, 90° flexion hip and knee | Concurrent validity LOA: 3.5° ICC: 0.54 | GM (ICC = 0.91; CV = 5.2%) ETS (ICC = 0.93; CV = 5.1%) | |||||||||
| Hip flexion, flexion knee | Construct validity (not differ between FAI and control) Concurrent validity (LOA: 18.9°; ICC: 0.44) | GM (ICC = 0.91; CV = 3.1%) ETS (ICC = 0.94; CV = 2.6%) | |||||||||
| Fourchet et al. [53] | No detail | No detail | Supine | Hip abduction, neutral knee | Two examiners Anatomical landmarks Hand-held dynamometer Force application Video capture digital Digital motion analysis software | Passive | Force application | No detail | 2 testing sessions (3 days apart) No detail | No detail | CV (90% IC) = 7.2%; ICC = 0.85 |
| Hip extension, knee flexion | CV (90% IC) = 2.6%; ICC = 0.51 | ||||||||||
| Hip internal rotation | CV (90% IC) = 9.6%; ICC = 0.92 | ||||||||||
| Hip external rotation | CV (90% IC) = 12.4%; ICC = 0.91 | ||||||||||
| Knee flexion, neutral hip | CV (90% IC) = 8.3%; ICC = 0.86 | ||||||||||
| Knee extension, 90° hip flexion | CV (90% IC) = 2.6%; ICC = 0.51 | ||||||||||
| Prone | Ankle dorsiflexion, neutral knee | CV (90% IC) = 4.5%; ICC = 0.93 | |||||||||
| Ankle dorsiflexion, 90° knee flexion | CV (90% IC) = 5.7%; ICC = 0.66 | ||||||||||
| Tainaka et al. [71] | No detail | No detail | Prone | Hip extension, neutral knee | 1-examiner Anatomical landmarks Standard GM | Active | No detail | Stabilized pelvis and spine | 2 testing sessions (1-week apart) 3 reps | No detail | Pearson r > 0.85 |
| Supine | Hip adduction | ||||||||||
| Hip abduction, neutral knee | |||||||||||
| Hip internal rotation, 90° hip and knee flexion | |||||||||||
| Hip external rotation, 90° flexion hip and knee | |||||||||||
| Hip flexion, knee flexion | |||||||||||
| Cejudo et al. [45] | 1 min | Yes | Supine | Hip extension, knee flexion | Two examiners Lumbar support “Lumbosant” (Imucot Traumatología SL, Murcia, Spain) Longitudinal axis (imaginary bisector line) Inclinometer with atelescopic rod | Passive | Firm end sensation Compensatory movements (lumbar spine, pelvis or lower limb) Feeling of stretching | APT | 3 testing sessions (2-week apart) 2 or 3 (variation > 5%) | Content validity by American medical organizations | SEM = 1.3°; MDC = 3.7°; ICC = 0.96 Cejudo et al. [63] |
| Supine | Hip adduction, 90° knee flexion | Transversal pelvis rotation | SEM = 1.8°; MDC = 4.5°; ICC = 0.92 Unpublished data | ||||||||
| Supine | Hip abduction, neutral knee | Frontal pelvis rotation, contralateral knee extension, transversal hip rotation | SEM = 1.8° MDC = 5.5°; ICC = 0.93; Cejudo et al. [63,72] | ||||||||
| Supine | Hip abduction, 90° hip and knee flexion | Transversal pelvis rotation | SEM = 2.1°; MDC = 5.8°; ICC = 0.99 Cejudo et al. [72] | ||||||||
| Supine | Hip flexion, extension knee | PPT, knee flexion, hip rotation, contralateral hip flexion | SEM = 1.9°; MDC = 6.1°; ICC: 0.91; Cejudo et al. [63] | ||||||||
| Supine | Hip flexion, flexion knee | SEM = 2.5°; MDC = 6.2°; ICC = 0.90 Cejudo et al. [63] | |||||||||
| Supine | Knee flexion, neutral hip | APT, hip rotation | SEM = 2.8°; MDC = 6.9°; ICC = 0.89; Cejudo et al. [63] | ||||||||
| Prone | Hip internal rotation, neutral hip and 90° knee flexion | Transversal pelvis rotation, hip abduction | SEM = 2.5°; MDC = 6.8°; ICC = 0.92 Unpublished data | ||||||||
| Prone | Hip external rotation, neutral hip and 90° knee flexion | Transversal pelvis rotation, hip abduction | SEM = 2.5°; MDC = 6.8° ICC = 0.92 Unpublished data | ||||||||
| Standing | Ankle dorsiflexion, neutral knee | Heel on the floor, Knee flexion | SEM = 1.7°; MDC = 4.7°; ICC = 0.95 Cejudo et al. [63] | ||||||||
| Standing | Ankle dorsiflexion, Knee flexion | Heel on the floor | SEM = 1.8°; MDC = 5°; ICC = 0.95 Cejudo et al. [63] | ||||||||
| Shah et al. [11] | No detail | Yes | Prone | Hip extension | 2-examiners Lateral midline of the thigh and horizontal axis of the body 2-examiners Bony landmark Standard GM | Passive | No detail | No details | 2 testing sessions 1 rep | No detail | ICC = 0.62 |
| Supine | Hip flexion | Compensation movements Maximum ROM | ICC = 0.77 | ||||||||
| Hip internal rotation, 90° flexion hip and knee | Transversal pelvis rotation, lumbar lateral flexion | ICC = 0.77 | |||||||||
| Hip external rotation, 90° flexion hip and knee | ICC = 0.90 | ||||||||||
| Grazette et al. [73] | No detail | No detail | Standing | Ankle dorsiflexion, knee flexion | Centimeters measurement units | Passive | Maximum ROM | Heel on the floor, knee flexion, foot pronation, foot supination, pelvic rotation, knee valgus or varus | 2 testing sessions (3–7 days apart) No detail | No detail | ICC = 0.95 CV = 35.9° |
| Supine | Medial hip rotation, 90˚ hip and knee | 2-examiners Standard GM | Passive | Firm end sensation | No detail | ICC = 0.72 CV = 8.3° | |||||
| Prone | Hip internal rotation | Passive | ICC = 0.70 CV = 36.5° | ||||||||
| Supine | Hip external rotation | Active | ICC = 0.82 CV = 49° | ||||||||
| Supine | Knee extension (Hamstring 90/90) | Passive | ICC = 0.47 CV = 65.3° |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cejudo, A.; Sainz de Baranda, P.; Ayala, F.; De Ste Croix, M.; Santonja-Medina, F. Assessment of the Range of Movement of the Lower Limb in Sport: Advantages of the ROM-SPORT I Battery. Int. J. Environ. Res. Public Health 2020, 17, 7606. https://doi.org/10.3390/ijerph17207606
Cejudo A, Sainz de Baranda P, Ayala F, De Ste Croix M, Santonja-Medina F. Assessment of the Range of Movement of the Lower Limb in Sport: Advantages of the ROM-SPORT I Battery. International Journal of Environmental Research and Public Health. 2020; 17(20):7606. https://doi.org/10.3390/ijerph17207606
Chicago/Turabian StyleCejudo, Antonio, Pilar Sainz de Baranda, Francisco Ayala, Mark De Ste Croix, and Fernando Santonja-Medina. 2020. "Assessment of the Range of Movement of the Lower Limb in Sport: Advantages of the ROM-SPORT I Battery" International Journal of Environmental Research and Public Health 17, no. 20: 7606. https://doi.org/10.3390/ijerph17207606





