Modeling the Pathways of Knowledge Management Towards Social and Economic Outcomes of Health Organizations
Abstract
1. Introduction
- RQ1.
- What is the impact of the KM process on organizational-level outcomes in the healthcare context?
- RQ2.
- What is the mechanism through which the KM process is able to enhance the quality of care and social and economic outcomes of health organizations?
2. Theoretical and Empirical Background
2.1. Knowledge Management Process and Organizational Performance
2.2. Healthcare Perspective on Knowledge Management
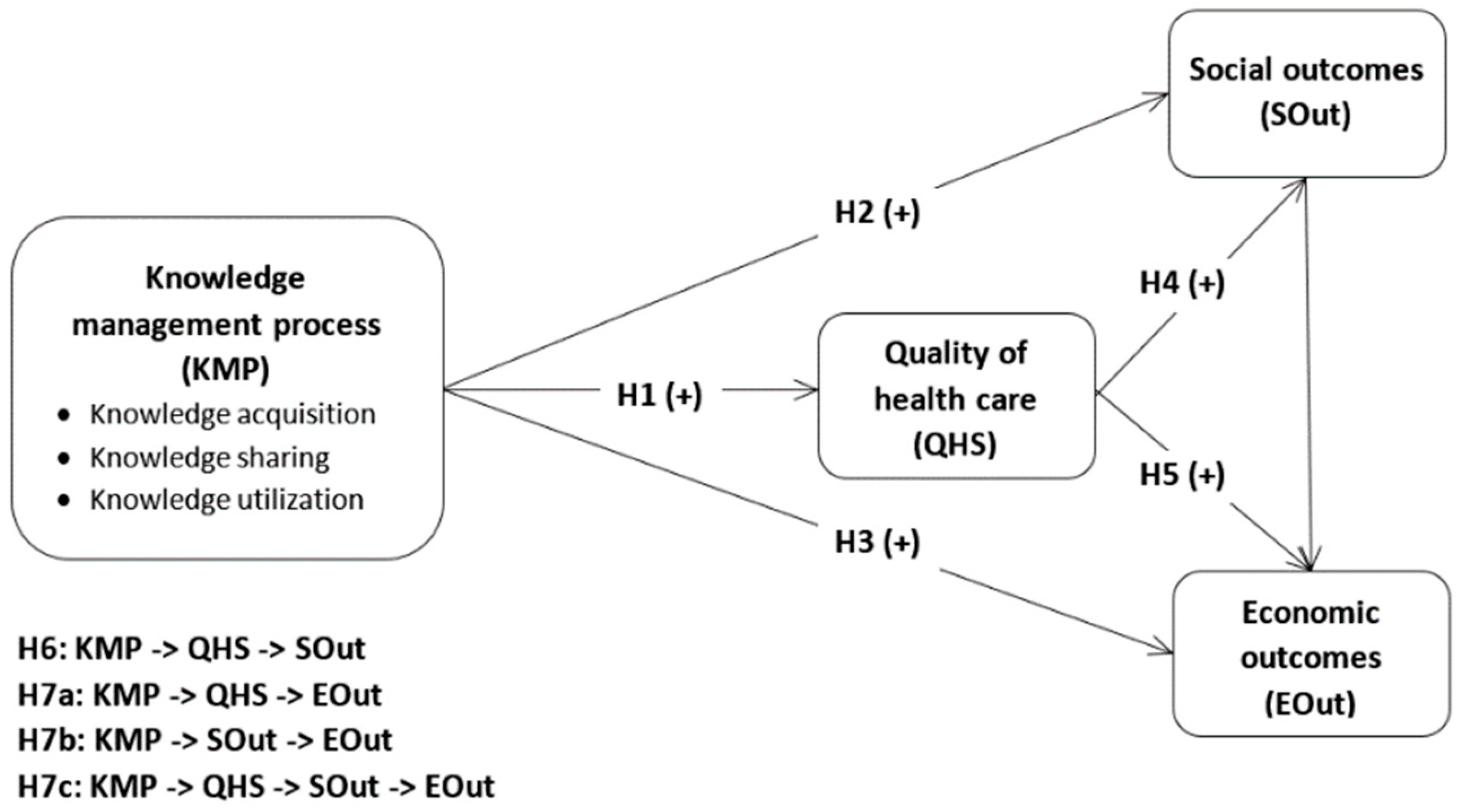
3. Research Hypotheses and Conceptual Model
4. Materials and Methods
4.1. Participants and Procedure
4.2. Measures
4.3. Data Screening
4.4. Data Analysis
5. Results
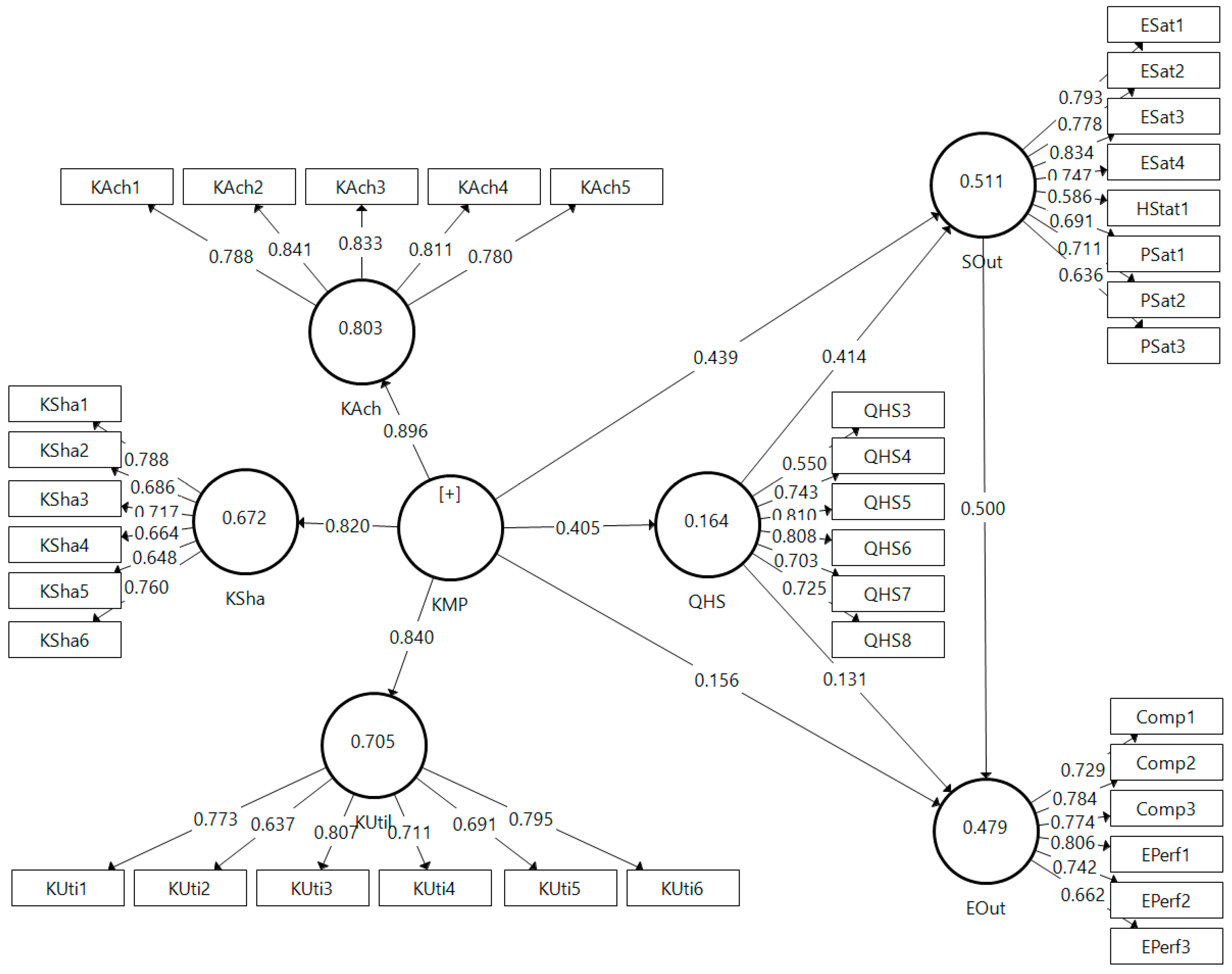
5.1. Measurement Model Assessment
5.2. Structural Model
5.3. Testing Research Hypotheses
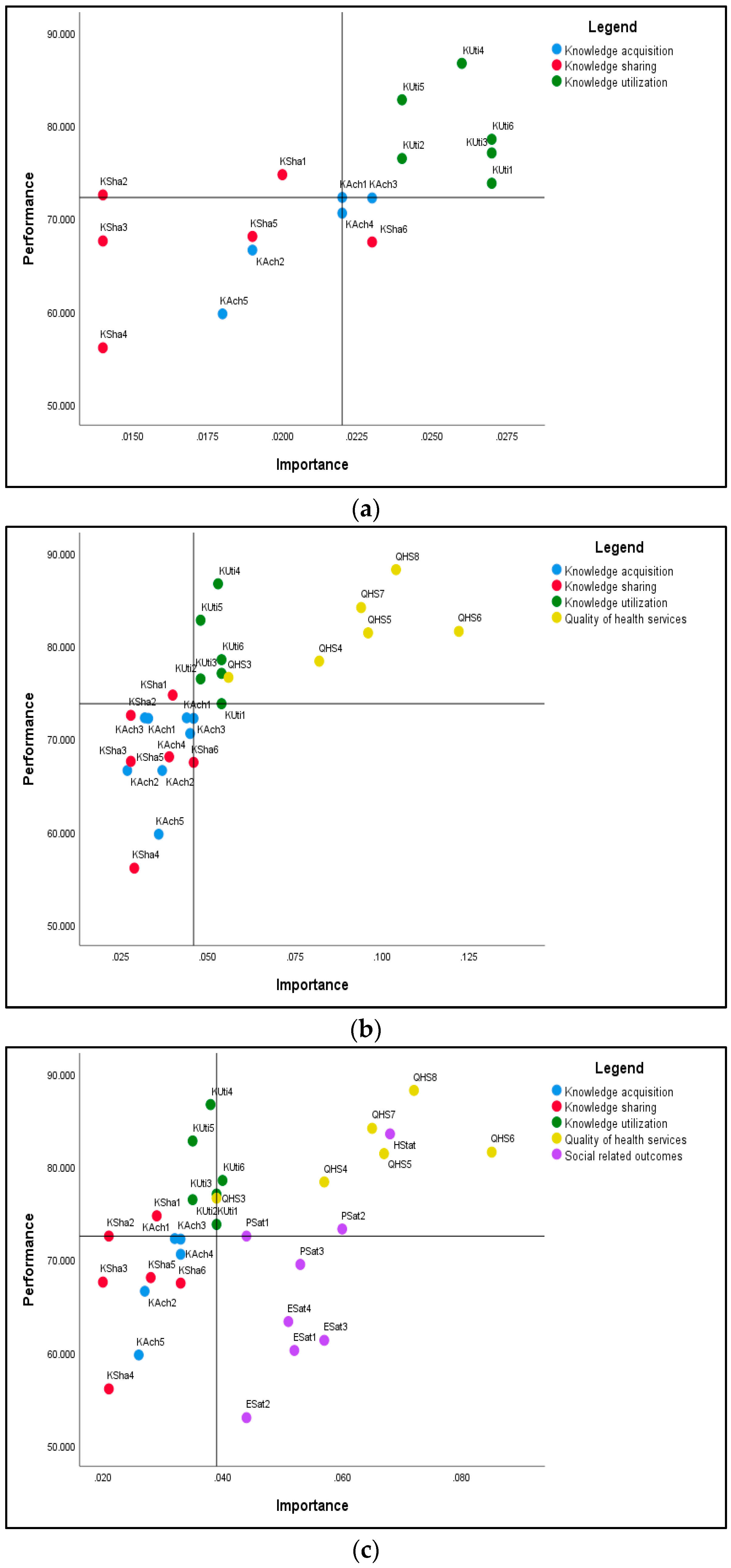
5.4. Importance Performance Matrix Analysis
6. Discussion and Conclusions
6.1. Theoretical and Practical Implications
6.1.1. Quality of Healthcare
6.1.2. Social Outcomes
6.1.3. Economic Outcomes
6.2. Limitations and Directions for Future Research
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Concept | Variable | Item | References |
|---|---|---|---|
| KM process | Within the organization… | ||
| Knowledge acquisition | KAch1 | New sources of information and knowledge are constantly being identified | [18,21,30,34] |
| KAch2 | New information and knowledge are acquired through participation at medical conferences and congresses | ||
| KAch3 | New information and knowledge are acquired by studying relevant literature | ||
| KAch4 | New information and knowledge are acquired by attending training or specialization courses | ||
| KAch5 | New information and knowledge are acquired from high-quality medical centers | ||
| Knowledge sharing | KSha1 | Information and knowledge are frequently shared with department colleagues | [21,25,30,34] |
| KSha2 | Information and knowledge are frequently shared with younger/less experienced colleagues | ||
| KSha3 | Information and knowledge are frequently shared with colleagues from other departments | ||
| KSha4 | Information and knowledge are frequently shared with colleagues from other health organizations | ||
| KSha5 | Information and knowledge are frequently shared by means of formal communication (e.g., meetings) | ||
| KSha6 | Information and knowledge are frequently shared by means of informal communication | ||
| Knowledge utilization | KUti1 | Information and knowledge are cherished for their true value | [21,25,34] |
| KUti2 | Information and knowledge are considered as the organization’s valuable assets | ||
| KUti3 | Different sources of information and knowledge are effectively used within medical practice | ||
| KUti4 | Medical staff knowledge is effectively applied within their medical practice | ||
| KUti5 | In providing medical care, there are effectively used medical protocols, procedures, and instructions existing within the organization | ||
| KUti6 | The information and knowledge existing within the organization are accessible to those who need it | ||
| Quality of health services | |||
| QHS1 a | The organization has a highly skilled medical staff | [56,57,58] | |
| QHS2 a | The medical services provided are accessible in terms of location, price, and waiting time | ||
| QHS3 | Patients positively appreciate the quality of medical services in terms of interpersonal relationships | ||
| QHS4 | Continuity in medical care is ensured | ||
| QHS5 | The medical services provided are efficient | ||
| QHS6 | The medical services provided are considered effective by patients and healthcare professionals | ||
| QHS7 | There are no risks associated with the process of granting medical care | ||
| QHS8 | Patients are provided free choice in terms of medical care | ||
| Social-related outcomes | |||
| Employees satisfaction | ESat1 | The organization frequently measures employee perception of motivating factors | [51,59,60,61] |
| ESat2 | The organization frequently measures employees’ perception of demotivating factors | ||
| ESat3 | Employee satisfaction has, overall, an increasing tendency | ||
| ESat4 | Employee satisfaction is, overall, superior to that recorded in similar organizations | ||
| Health status and quality of life improvement | HStat1 | Medical services provided contribute to improving patient health status | [51,61] |
| LQual1 a | Medical services provided contribute to increasing patient quality of life | ||
| Patient satisfaction | PSat1 | Patient satisfaction with medical services/products is constantly assessed through surveys | [51,59,60,61] |
| PSat2 | Patient satisfaction has, overall, an increasing tendency | ||
| PSat3 | Patient satisfaction is, overall, superior to that recorded in similar organizations | ||
| Economic-related outcomes | |||
| Competitiveness | Comp1 | Evaluation of organization’s competitiveness… … compared with that of the main competitors | [60,61] |
| Comp2 | … compared to five years ago | ||
| Comp3 | … compared with its set objectives | ||
| Economic performance | EPerf1 | Evaluation of organization’s competitiveness… … compared with its set objectives | [60,61] |
| EPerf2 | … compared with that of the main competitors | ||
| EPerf3 | … compared to five years ago | ||
References
- Nicolescu, O.; Nicolescu, C. The specificity and typology of dynamic management studies. J. Organ. Chang. Manag. 2014, 27, 299–313. [Google Scholar] [CrossRef]
- Alavi, M.; Leidner, D.E. Review: Knowledge Management and Knowledge Management Systems: Conceptual Foundations and Research Issues. MIS Q. 2001, 25, 107–136. [Google Scholar] [CrossRef]
- Dalkir, K. Knowledge Management in Theory and Practice, 2nd ed.; The MIT Press: Cambridge, UK, 2011. [Google Scholar]
- Lee, H.; Choi, B. Knowledge management enablers, processes, and organizational performance: An integrative view and empirical examination. J. Manag. Inf. Syst. 2003, 20, 179–228. [Google Scholar] [CrossRef]
- Chang, C.L.; Lin, T.C. The role of organizational culture in the knowledge management process. J. Knowl. Manag. 2015, 19, 433–455. [Google Scholar] [CrossRef]
- Bolisani, E.; Bratianu, C. Emergent Knowledge Strategies: Strategic Thinking in Knowledge Management; Springer International Publishing: Cham, Switzerland, 2018; pp. 23–48. [Google Scholar]
- Van Beveren, J. Does health care for knowledge management? J. Knowl. Manag. 2003, 7, 90–95. [Google Scholar] [CrossRef]
- Orzano, A.J.; McInerney, C.R.; Tallia, A.F.; Scharf, D.; Crabtree, B.F. Family medicine practice performance and knowledge management. Health Care Manag. Rev. 2008, 33, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Bordoloi, P.; Islam, N. Knowledge Management Practices and Healthcare Delivery: A Contingency Framework. Electron. J. Knowl. Manag. 2012, 10, 110–120. [Google Scholar]
- Sibbald, S.L.; Wathen, C.N.; Kothari, A. An empirically based model for knowledge management in health care organizations. Health Care Manag. Rev. 2016, 41, 64–74. [Google Scholar] [CrossRef]
- Gabbay, J.; Le May, A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. Br. Med. J. 2004, 329, 1013–1017. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, N.; Sharma, S.; Gupta, J.N. Creating Knowledge-Based Healthcare Organizations; IGI Global: Hershey, PA, USA, 2005. [Google Scholar]
- Nicolini, D.; Powell, J.; Martinez-Solano, L. Managing knowledge in the healthcare sector. A review. Int. J. Manag. Rev. 2008, 10, 245–263. [Google Scholar] [CrossRef]
- Karamitri, I.; Talias, M.A.; Bellali, T. Knowledge management practices in healthcare settings: A systematic review. Int. J. Health Plan. Manag. 2017, 32, 4–18. [Google Scholar] [CrossRef]
- Kothari, A.; Hovanec, N.; Hastie, R.; Sibbald, S. Lessons from the business sector for successful knowledge management in health care: A systematic review. BMC Health Serv. Res. 2011, 11, 173. [Google Scholar] [CrossRef]
- Shahmoradi, L.; Safadari, R.; Jimma, W. Knowledge Management Implementation and the Tools Utilized in Healthcare for Evidence-Based Decision Making: A Systematic Review. Ethiop. J. Health Serv. 2017, 24, 541–558. [Google Scholar] [CrossRef]
- Lee, H.-S. Knowledge Management Enablers and Process in Hospital Organizations. Osong Public Health Res. Perspect. 2017, 8, 26–33. [Google Scholar] [CrossRef]
- Gowen, C.; Henagan, S.; McFadden, K. Knowledge management as a mediator for the efficacy of transformational leadership and quality management initiatives in U.S. health care. Health Care Manag. Rev. 2009, 34, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Karamat, J.; Shurong, T.; Ahmad, N.; Waheed, A.; Khan, S. Barriers to Knowledge Management in the Health Sector of Pakistan. Sustainability 2018, 10, 4155. [Google Scholar] [CrossRef]
- Karamat, J.; Shurong, T.; Ahmad, N.; Waheed, A.; Mahmood, K. Enablers Supporting the Implementation of Knowledge Management in the Healthcare of Pakistan. Int. J. Environ. Res. Public Health 2018, 15, 2816. [Google Scholar] [CrossRef] [PubMed]
- Gold, A.H.; Malhotra, A.; Segars, A.H. Knowledge management: An organizational capabilities perspective. J. Manag. Inf. Syst. 2001, 18, 185–214. [Google Scholar] [CrossRef]
- Grover, W.; Davenport, T.H. General Perspectives on Knowledge Management: Fostering a Research Agenda. J. Manag. Inf. Syst. 2001, 18, 5–21. [Google Scholar] [CrossRef]
- Zheng, W.; Yang, B.; McLean, G.N. Linking organizational culture, structure, strategy, and organizational effectiveness: Mediating role of knowledge management. J. Bus. Res. 2010, 63, 763–771. [Google Scholar] [CrossRef]
- Abdi, K.; Senin, A.A. The impact of knowledge management on organizational innovation: An empirical study. Asian Soc. Sci. 2015, 11, 153–168. [Google Scholar] [CrossRef]
- Rašula, J.; Vukšić, V.B.; Štemberger, M.I. The Impact of Knowledge Management on Organisational Performance. Econ. Bus. Rev. 2012, 14, 147–168. [Google Scholar]
- Lyu, H.; Zhou, Z.; Zhang, Z. Measuring Knowledge Management Performance in Organizations: An Integrative Framework of Balanced Scorecard and Fuzzy Evaluation. Information 2016, 7, 29. [Google Scholar] [CrossRef]
- Nonaka, K. A Dynamic Theory of Organizational Knowledge Creation. Organ. Sci. 1994, 5, 14–37. [Google Scholar] [CrossRef]
- Nonaka, I.; Takeuchi, H. The Knowledge-Creating Company: How Japanese Companies Create the Dynamics of Innovation; Oxford University Press: New York, NY, USA, 1995. [Google Scholar]
- Simion, C.-P.; Radu, V. Relationship between Organisation Culture and Knowledge Management in SME’s. Rev. Int. Comp. Manag. 2009, 10, 781–790. [Google Scholar]
- Fugate, B.S.; Stank, T.P.; Mentzer, J.T. Linking improved knowledge management to operational and organizational performance. J. Oper. Manag. 2009, 27, 247–264. [Google Scholar] [CrossRef]
- Zack, M.; McKeen, J.; Singh, S. Knowledge management and organizational performance: An exploratory analysis. J. Knowl. Manag. 2009, 13, 392–409. [Google Scholar] [CrossRef]
- Kianto, A.; Vanhala, M.; Heilmann, P. The impact of knowledge management on job satisfaction. J. Knowl. Manag. 2016, 20, 621–636. [Google Scholar] [CrossRef]
- Popa, I.; Ștefan, S.C.; Morărescu, C.; Cicea, C. Research regarding the Influence of Knowledge Management Practices on Employee Satisfaction in the Romanian Healthcare System. Amfiteatru Econ. 2018, 20, 553–566. [Google Scholar] [CrossRef]
- Gholami, M.H.; Nazari-Shirkouhi, S.; Noruzy, A. Investigating the influence of knowledge management practices on organizational performance: An empirical study. Acta Polytech. Hung. 2013, 10, 205–216. [Google Scholar]
- Andreeva, T.; Kianto, A. Does knowledge management really matter? Linking knowledge management practices competitiveness and economic performance. J. Knowl. Manag. 2012, 16, 617–636. [Google Scholar] [CrossRef]
- Orzano, A.J.; McInerney, C.R.; Scharf, D.; Tallia, A.F.; Crabtree, B.F. A knowledge management model: Implications for enhancing quality in health care. J. Am. Soc. Inf. Sci. Technol. 2008, 59, 489–505. [Google Scholar] [CrossRef]
- Van Peursem, K.A.; Pratt, M.J.; Lawrence, S.R. Health management performance: A review of measures and indicators. Account. Audit. Account. J. 1995, 8, 34. [Google Scholar] [CrossRef]
- Leggat, S.G.; Narine, L.; lemieux-Charles, L.; Barnsley, J.; Baker, G.R.; Sicotte, C.; Champagne, F.; Bilodeau, H. A Review of Organizational Performance Assessment in Health Care. Health Serv. Manag. Res. 1998, 11, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Arah, O.A.; Westert, G.P.; Hurst, J.; Klazinga, N.S. A conceptual framework for the OECD Health Care Quality Indicators Project. Int. J. Qual. Health Care 2006, 18 (Suppl. 1), 5–13. [Google Scholar] [CrossRef]
- Bititci, U.; Garengo, P.; Dörfler, V.; Nudurupati, S. Performance Measurement: Challenges for Tomorrow. Int. J. Manag. Rev. 2012, 14, 305–327. [Google Scholar] [CrossRef]
- Nuti, S.; Seghieri, C.; Vainieri, M. Assessing the effectiveness of a performance evaluation system in the public health care sector: Some novel evidence from the Tuscany region experience. J. Manag. Gov. 2013, 17, 59–69. [Google Scholar] [CrossRef]
- Nuti, S.; Noto, G.; Vola, F.; Vainieri, M. Let’s play the patients music: A new generation of performance measurement systems in healthcare. Manag. Decis. 2018, 56, 2252–2272. [Google Scholar] [CrossRef]
- Valmohammadi, C.; Ahmadi, M. The impact of knowledge management practices on organizational performance: A balanced scorecard approach. J. Enterp. Inf. Manag. 2015, 28, 131–159. [Google Scholar] [CrossRef]
- Aidemark, L. The Meaning of Balanced Scorecards in the Health Care Organisation. Financ. Account. Manag. 2001, 17, 23–40. [Google Scholar] [CrossRef]
- Ho, L.A. What affects organizational performance?: The linking of learning and knowledge management. Ind. Manag. Data Syst. 2008, 108, 1234–1254. [Google Scholar] [CrossRef]
- Alaarj, S.; Mohamed, Z.A.; Bustamam, U.S. The Effect of Knowledge Management Capabilities on Performance of Companies: A Study of Service Sector. Int. J. Econ. Res. 2017, 14, 457–470. [Google Scholar]
- Becerra-Fernandez, I.; Sabherwal, R. Organizational Knowledge Management: A Contingency Perspective. J. Manag. Inf. Syst. 2001, 18, 23–55. [Google Scholar] [CrossRef]
- Wyatt, J.C. Management of explicit and tacit knowledge. J. R. Soc. Med. 2001, 94, 6–9. [Google Scholar] [CrossRef]
- Bordoloi, P.; Islam, N. A framework linking knowledge management practices and healthcare delivery performance. In Proceedings of the 8th ICICKM 2011, Bangkok, Thailand, 27–28 October 2011. [Google Scholar]
- El Morr, C.; Subercaze, J. Knowledge management in healthcare. In Handbook of Research On Developments in E-Health and Telemedicine: Technological and Social Perspectives; Cruz-Cunha, M.M., Tavares, A.J., Simoes, R., Eds.; IGI Global: Hershey, PA, USA, 2010; pp. 490–510. [Google Scholar]
- Porter, M.E.; Teisberg, E.O. Redefining Health Care: Creating Value-Based Competition on Results; Harvard Business School Press: Boston, MA, USA, 2006. [Google Scholar]
- Porter, M.E.; Lee, T.H. The Strategy That Will Fix Health Care. Harvard Bus. Rev. 2013, 91, 50–70. [Google Scholar]
- Swayne, L.E.; Duncan, W.J.; Ginter, P.M. Strategic Management of Health Care Organizations, 5th ed.; Blackwell Publishing: Hoboken, NJ, USA, 2006. [Google Scholar]
- Cowing, M.; Davino-Ramaya, C.M.; Ramaya, K.; Szmerekovsky, J. Health Care Delivery Performance: Service, Outcomes, and Resource Stewardship. Perm. J. 2009, 13, 72–78. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, version 25.0; [Computer Program]; IBM Corp.: Armonk, NY, USA, 2017. [Google Scholar]
- Al-Assaf, A.F. Managed Care Quality: A Practical Guide; CRC Press: Boca Raton, FL, USA, 1998. [Google Scholar]
- Donabedian, A. An Introduction to Quality Assurance in Health Care; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Ștefan, S.C.; Popa, Ș.C. Health workers motivation and quality of care. A Path Analysis approach. In Proceedings of the 31st IBIMA Conference—Innovation Management and Education Excellence through Vision 2020, Milan, Italy, 25–26 April 2018; pp. 2384–2390. [Google Scholar]
- Gowen, C.R., III; McFadden, K.L.; Tallon, W.J. On the centrality of strategic human resource management for healthcare quality results and competitive advantage. J. Manag. Dev. 2006, 25, 806–826. [Google Scholar] [CrossRef]
- EIPA. The Common Assessment Framework 2013. Improving Public Organisations through Self-Assessment. 2013. Available online: http://www.eipa.eu/files/File/CAF/CAF_2013.pdf (accessed on 25 January 2016).
- Ștefan, S.C.; Popa, I.; Dobrin, C.O. Towards a Model of Sustainable Competitiveness of Health Organizations. Sustainability 2016, 8, 464. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Hult, G.T.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; SAGE: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Ringle, C.M.; Sarstedt, M. Gain more insight from your PLS-SEM results: The importance-performance map analysis. Ind. Manag. Data Syst. 2016, 116, 1865–1886. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Hair, J.F.; Black, W.C.; Bobin, B.J.; Anderson, N.E. Multivariate Data Analysis, 7th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Ali, Z.; Sun, H.; Ali, M. The Impact of Managerial and Adaptive Capabilities to Stimulate Organizational Innovation in SMEs: A Complementary PLS–SEM Approach. Sustainability 2017, 9, 2157. [Google Scholar] [CrossRef]
- Ali, I.; Musawir, A.U.; Ali, M. Impact of knowledge sharing and absorptive capacity on project performance: The moderating role of social processes. J. Knowl. Manag. 2018, 22, 453–477. [Google Scholar] [CrossRef]
- Wold, H. Soft Modeling: The Basic Design and Some Extensions. In Systems under Indirect Observations: Causality, Structure, Prediction; North-Holland: Amsterdam, The Netherlands, 1982; Chapter Part II; pp. 1–54. [Google Scholar]
- Wetzels, M.; Odekerken-Schröder, G.; Van Oppen, C. Using PLS path modeling for assessing hierarchical construct models: Guidelines and empirical illustration. MIS Q. 2009, 33, 177–195. [Google Scholar] [CrossRef]
- Lowry, P.B.; Gaskin, J. Partial Least Squares (PLS) Structural Equation Modeling (SEM) for Building and Testing Behavioral Causal Theory: When to Choose It and How to Use It. IEEE Trans. Prof. Commun. 2014, 57, 123–146. [Google Scholar] [CrossRef]
- Schloderer, M.P.; Sarstedt, M.; Ringle, C.M. The Relevance of Reputation in the Nonprofit Sector: The Moderating Effect of Socio-Demographic Characteristics. Int. J. Nonprofit Volunt. Sect. Mark. 2014, 19, 110–126. [Google Scholar] [CrossRef]
- Ringle, C.M.; Wende, S.; Becker, J.M. SmartPLS 3.2.7; SmartPLS GmbH: Bönningstedt, Germany, 2015. [Google Scholar]
- Hulland, J. Use of partial least squares (PLS) in strategic management research: A review of four recent studies. Strateg. Manag. J. 1999, 20, 195–204. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Nunnaly, J.C.; Bernstein, I.R. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Gefen, D.; Straub, D.; Boudreau, M.C. Structural Equation Modeling and Regression: Guidelines for Research Practice. Commun. Assoc. Inf. Syst. 2000, 4, 1–77. [Google Scholar] [CrossRef]
- Chin, W. Commentary: Issues and Opinion on Structural Equation Modeling. MIS Q. 1998, 2, VII–XVI. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Tenenhaus, T.; Vinzi, V.E.; Chatelin, Y.M.; Lauro, C. PLS path modeling. Comput. Stat. Data Anal. 2004, 48, 159–205. [Google Scholar] [CrossRef]
- Nitzi, C.; Roldan, J.L.; Cepeda, G. Mediation analysis in partial least squares path modeling: Helping researchers discuss more sophisticated models. Ind. Manag. Data Syst. 2016, 116, 1849–1864. [Google Scholar] [CrossRef]
- Castro, I.; Roldán, J.L. A mediation model between dimensions of social capital. Int. Bus. Rev. 2013, 22, 1034–1050. [Google Scholar] [CrossRef]
- Vuong, Q.-H.; Ho, M.-T.; Vuong, T.-T.; La, V.-P.; Ho, M.-T.; Nghiem, K.-C.P.; Tran, B.X.; Giang, H.-H.; Giang, T.-V.; Latkin, C.; et al. Artificial Intelligence vs. Natural Stupidity: Evaluating AI Readiness for the Vietnamese Medical Information System. J. Clin. Med. 2019, 8, 168. [Google Scholar] [CrossRef] [PubMed]
| Variable | N/Mean | SD (%) | |
|---|---|---|---|
| Profession | Physician | 99 | 21.569 |
| Pharmacist | 115 | 25.054 | |
| Medical staff with higher education (other than physician) | 24 | 5.229 | |
| Nurse | 101 | 22.004 | |
| Nonmedical staff | 95 | 20.697 | |
| Others | 25 | 5.447 | |
| Managerial position | Yes | 66 | 14.379 |
| No | 393 | 85.621 | |
| Seniority within organization (years) | 5.538 | 4.412 | |
| Type of healthcare | Specialized medical care | 141 | 30.719 |
| Hospital | 190 | 41.394 | |
| Pharmacy | 128 | 27.887 | |
| Organization size (employees) | <10 | 87 | 18.954 |
| 10–49 | 40 | 8.715 | |
| 50–249 | 144 | 31.373 | |
| >250 | 188 | 40.959 | |
| Latent Construct (First-Order/Second-Order; Reflective/Formative) | Items | Loadings | SD | t | α | Rho_A | CR | AVE |
|---|---|---|---|---|---|---|---|---|
| KAch—Knowledge acquisition | KAch1 | 0.788 *** | 0.019 | 40.497 | 0.870 | 0.871 | 0.906 | 0.658 |
| (first-order; reflective) | KAch2 | 0.841 *** | 0.016 | 53.782 | ||||
| KAch3 | 0.833 *** | 0.018 | 47.596 | |||||
| KAch4 | 0.811 *** | 0.016 | 50.852 | |||||
| KAch5 | 0.780 *** | 0.021 | 37.084 | |||||
| KSha—Knowledge sharing | KSha1 | 0.788 *** | 0.021 | 37.647 | 0.805 | 0.816 | 0.860 | 0.507 |
| (first-order; reflective) | KSha2 | 0.686 *** | 0.031 | 22.183 | ||||
| KSha3 | 0.717 *** | 0.026 | 27.842 | |||||
| KSha4 | 0.664 *** | 0.034 | 19.548 | |||||
| KSha5 | 0.648 *** | 0.033 | 19.528 | |||||
| KSha6 | 0.760 *** | 0.021 | 35.571 | |||||
| KUtil—Knowledge utilization | KUti1 | 0.773 *** | 0.022 | 35.005 | 0.831 | 0.842 | 0.877 | 0.545 |
| (first-order; reflective) | KUti2 | 0.637 *** | 0.039 | 16.383 | ||||
| KUti3 | 0.807 *** | 0.018 | 44.961 | |||||
| KUti4 | 0.711 *** | 0.028 | 25.318 | |||||
| KUti5 | 0.691 *** | 0.032 | 21.806 | |||||
| KUti6 | 0.795 *** | 0.016 | 49.245 | |||||
| QHS—Quality of health services | QHS3 | 0.550 *** | 0.051 | 10.883 | 0.820 | 0.838 | 0.870 | 0.531 |
| (first-order; reflective) | QHS4 | 0.743 *** | 0.029 | 25.704 | ||||
| QHS5 | 0.810 *** | 0.021 | 39.429 | |||||
| QHS6 | 0.808 *** | 0.019 | 43.494 | |||||
| QHS7 | 0.703 *** | 0.031 | 22.830 | |||||
| QHS8 | 0.725 *** | 0.029 | 25.022 | |||||
| SOut—Social-related outcomes | ESat1 | 0.794 *** | 0.019 | 41.999 | 0.869 | 0.875 | 0.898 | 0.527 |
| (first-order; reflective) | ESat2 | 0.779 *** | 0.024 | 32.619 | ||||
| ESat3 | 0.835 *** | 0.014 | 61.671 | |||||
| ESat4 | 0.746 *** | 0.024 | 31.178 | |||||
| HStat1 | 0.588 *** | 0.040 | 14.578 | |||||
| PSat1 | 0.690 *** | 0.027 | 25.625 | |||||
| PSat2 | 0.709 *** | 0.025 | 28.317 | |||||
| PSat3 | 0.634 *** | 0.030 | 21.377 | |||||
| EOut—Economic-related outcomes | Comp1 | 0.727 *** | 0.022 | 32.810 | 0.845 | 0.849 | 0.885 | 0.564 |
| (first-order; reflective) | Comp2 | 0.781 *** | 0.020 | 39.030 | ||||
| Comp3 | 0.772 *** | 0.023 | 33.777 | |||||
| EPerf1 | 0.808 *** | 0.016 | 49.829 | |||||
| EPerf2 | 0.747 *** | 0.023 | 32.156 | |||||
| EPerf3 | 0.662 *** | 0.031 | 21.079 | |||||
| KMP—Knowledge management process | KAch | 0.896 *** | 0.011 | 84.809 | 0.907 | 0.914 | 0.889 | 0.727 |
| (second-order; reflective) | KSha | 0.820 *** | 0.021 | 39.973 | ||||
| KUtil | 0.840 *** | 0.014 | 58.747 |
| Construct | EOut | KAch | KSha | KUtil | QHS | SOut |
|---|---|---|---|---|---|---|
| EOut | 0.751 | |||||
| KAch | 0.431 | 0.811 | ||||
| KSha | 0.318 | 0.676 | 0.712 | |||
| KUtil | 0.528 | 0.606 | 0.493 | 0.738 | ||
| QHS | 0.488 | 0.276 | 0.135 | 0.571 | 0.728 | |
| SOut | 0.671 | 0.518 | 0.36 | 0.631 | 0.592 | 0.726 |
| Endogenous Construct | R2 | Relationship | f2 | Decision |
|---|---|---|---|---|
| QHS | 0.164 *** | KMP → QHS | 0.203 *** | Medium |
| EOut | 0.479 *** | KMP → EOut | 0.033 | Small |
| QHS → EOut | 0.024 | Small | ||
| SOut | 0.511 *** | KMP → SOut | 0.334 *** | Large |
| QHS → SOut | 0.299 *** | Medium |
| Hypothesis | Relationship | β | SE | t | 95% BC CI | Supported (Yes/No) | |
|---|---|---|---|---|---|---|---|
| CIlow | CIhigh | ||||||
| H1 (+) | KMP → QHS | 0.407 *** | 0.040 | 10.149 | 0.340 | 0.471 | Yes |
| H2 (+) | KMP → SOut | 0.439 *** | 0.030 | 14.747 | 0.390 | 0.488 | Yes |
| H3 (+) | KMP → EOut | 0.156 ** | 0.047 | 3.332 | 0.079 | 0.233 | Yes |
| H4 (+) | QHS → SOut | 0.414 *** | 0.038 | 10.817 | 0.349 | 0.476 | Yes |
| H5 (+) | QHS → EOut | 0.131 ** | 0.054 | 9.278 | 0.051 | 0.214 | Yes |
| Hypothesis | Relationship (Effect Type) | β | SE | t | 95% BC CI | Mediation | Supported (Yes/No) | |
|---|---|---|---|---|---|---|---|---|
| CIlow | CIhigh | |||||||
| H6 | KMP → SOut (Direct Effect) | 0.439 *** | 0.030 | 14.747 | 0.390 | 0.488 | Simple complementary mediation | Yes |
| KMP → QHS → SOut (Indirect Effect) | 0.168 *** | 0.023 | 7.390 | 0.131 | 0.206 | |||
| KMP → SOut (Total Effect) | 0.607 *** | 0.026 | 23.646 | 0.560 | 0.646 | |||
| H7a–H7c | KMP → EOut (Direct Effect) | 0.156 ** | 0.047 | 3.332 | 0.079 | 0.233 | Multiple complementary mediation | Yes |
| KMP → EOut (Total Indirect Effect) | 0.358 *** | 0.028 | 12.888 | 0.309 | 0.400 | |||
| KMP → QHS → EOut (Specific Indirect Effect) | 0.053 * | 0.020 | 2.585 | 0.022 | 0.090 | |||
| KMP → SOut → EOut (Specific Indirect Effect) | 0.220 *** | 0.027 | 8.069 | 0.176 | 0.267 | |||
| KMP → QHS → SOut → EOut (Specific Indirect Effect) | 0.084 *** | 0.015 | 5.625 | 0.062 | 0.111 | |||
| KMP → EOut (Total effect) | 0.513 *** | 0.039 | 13.160 | 0.443 | 0.573 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popa, I.; Ștefan, S.C. Modeling the Pathways of Knowledge Management Towards Social and Economic Outcomes of Health Organizations. Int. J. Environ. Res. Public Health 2019, 16, 1114. https://doi.org/10.3390/ijerph16071114
Popa I, Ștefan SC. Modeling the Pathways of Knowledge Management Towards Social and Economic Outcomes of Health Organizations. International Journal of Environmental Research and Public Health. 2019; 16(7):1114. https://doi.org/10.3390/ijerph16071114
Chicago/Turabian StylePopa, Ion, and Simona Cătălina Ștefan. 2019. "Modeling the Pathways of Knowledge Management Towards Social and Economic Outcomes of Health Organizations" International Journal of Environmental Research and Public Health 16, no. 7: 1114. https://doi.org/10.3390/ijerph16071114
APA StylePopa, I., & Ștefan, S. C. (2019). Modeling the Pathways of Knowledge Management Towards Social and Economic Outcomes of Health Organizations. International Journal of Environmental Research and Public Health, 16(7), 1114. https://doi.org/10.3390/ijerph16071114






