Outbreak of Cholera Due to Cyclone Kenneth in Northern Mozambique, 2019
Abstract
:1. Introduction
2. Sources and Documental Analysis
3. Mozambique
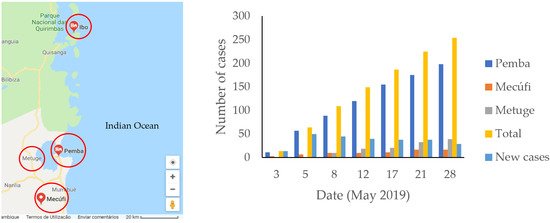
4. Overview of Cyclone Kenneth
5. Epidemiological Accounts
6. Outbreak Response
7. Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Isbell, T.; Bhoojedhur, S. Cyclones Add to Mozambique’s Public Health Challenges. Available online: https://www.afrobarometer.org/publications/ad297-cyclones-add-mozambiques-public-health-challenges (accessed on 4 June 2019).
- Anjichi-Kodumbe, T.; Abreu, S.; van Vliet, T. Southern Africa: Tropical Cyclone Kenneth Flash Update No. 11. Available online: https://reliefweb.int/report/mozambique/southern-africa-tropical-cyclone-kenneth-flash-update-no-11-8-may-2019 (accessed on 29 May 2019).
- Taylor, H.T.; Ward, B.; Willis, M.; Zaleski, W.J.N.O. The Saffir-Simpson Hurricane Wind Scale; Atmospheric Administration: Washington, DC, USA, 2010. [Google Scholar]
- Anjichi-Kodumbe, T.; Abreu, S.; van Vliet, T. Southern Africa: Tropical Cyclone Kenneth Flash Update No. 7. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/ROSEA_20190501_SouthernAfrica_TCKenneth_FlashUpdate7_FINAL.pdf (accessed on 29 May 2019).
- Anjichi-Kodumbe, T.; Abreu, S.; van Vliet, T. Southern Africa: Tropical Cyclone Kenneth Flash Update No. 8. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/ROSEA_20190503_SouthernAfrica_TCKenneth_FlashUpdate8_DRAFT.pdf (accessed on 29 May 2019).
- Agence France-Presse. Mozambique Records First Cholera Cases after Cyclone Kenneth. Available online: https://medicalxpress.com/news/2019-05-mozambique-cholera-cases-cyclone-kenneth.html (accessed on 31 May 2019).
- Langa, J.P.; Sema, C.; De Deus, N.; Colombo, M.M.; Taviani, E. Epidemic waves of cholera in the last two decades in Mozambique. J. Infect. Dev. Ctries. 2015, 9, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Chissaque, A.; De Deus, N.; Vubil, D.; Mandomando, I. The Epidemiology of Diarrhea in Children Under 5 Years of Age in Mozambique. Curr. Trop. Med. Rep. 2018, 5, 115–124. [Google Scholar] [CrossRef]
- Chitio, J.J.E.; Langa, J.P.M. Frequência e perfil de susceptibilidade de Aeromonas spp. isolados de surtos de cólera nas regiões centro e norte de Moçambique, 2014–2015. Rev. Moçambicana Ciências Saúde 2018, 4, 29. [Google Scholar]
- Paulo, M.; Gurjal, L.; Cardoso, N. Investigação de surto de cólera, na comunidade de Casacone, na província de Nampula, Novembro 2017. Moçambicana Ciências Saúde 2018, 4, 134. [Google Scholar]
- Marrufo, T.; Salomão, C.; Chicumbe, S.; Muianga, C.; Cardoso, N.; Baltazar, C.; Langa, J.P. Avaliação de determinantes ambientais (água, saneamento e higiene) na cidade de Nampula em 2016. Moçambicana Ciências Saúde 2018, 4, 66. [Google Scholar]
- Mesa, F.; Simbine, E.; Faranguana, A.C. Análise de casos de diarreias agudas e óbitos no Hospital Distrital de Mocuba-Junho a Julho de 2015. Moçambicana Ciências Saúde 2018, 4, 190. [Google Scholar]
- Vanormelingen, K.; Le Pechoux, M.; Bonde, T. Cholera Outbreaks in Tete, Sofala, Zambezia, Nampula and Niassa Provinces. Available online: www.unicef.org/appeals/files/UNICEF_Mozambique_SitRep_26_March_2015.pdf (accessed on 2 June 2019).
- Salomão, C.; Langa, J.; Bertil, A.; Baltazar, C. Vacina oral contra cólera, conhecimentos atitudes e práticas, diferenças e igualdades em duas campanhas, Tete 2017 e 2018. Moçambicana Ciências Saúde 2018, 4, 282. [Google Scholar]
- Schnoering, K. Mozambique Cyclone Idai Response; UN Migration: Le Grand-Saconnex, Switzerland, 2019. [Google Scholar]
- U.S. Agency for International Development. Southern Africa-Tropical Cyclone Idai-Fact Sheet #4 FY2019. Available online: https://www.usaid.gov/cyclone-idai/fy19/fs4 (accessed on 31 May 2019).
- National Health Institute; World Health Organization. Tropical Cyclones Idai and Kenneth, Mozambique National Situation Report 1; National Health Institute, Ministry of Health: Maputo, Mozambique, 2019; p. 12.
- Anjichi-Kodumbe, T.; Abreu, S.; van Vliet, T. Southern Africa: Tropical Cyclone Kenneth Flash Update No. 10. Available online: https://reliefweb.int/report/mozambique/southern-africa-tropical-cyclone-kenneth-flash-update-no-10-6-may-2019 (accessed on 29 May 2019).
- Cabral, D.; Balde, T.; Schmachtel, C. Tropical Cyclone Idai, Mozambique: Donor Alert; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- United Nations Office for the Coordination of Humanitarian Affairs. Mozambique: Brave Mothers in the Midst of Hardship. Available online: https://www.unocha.org/story/mozambique-brave-mothers-midst-hardship (accessed on 12 June 2019).
- United Nations Office for the Coordination of Humanitarian Affairs. Cyclones Idai and Kenneth. Available online: https://www.unocha.org/southern-and-eastern-africa-rosea/cyclones-idai-and-kenneth (accessed on 12 June 2019).
- Anjichi-Kodumbe, T.; Abreu, S.; van Vliet, T. Southern Africa: Tropical Cyclone Kenneth Flash Update No. 9. Available online: https://reliefweb.int/report/mozambique/southern-africa-tropical-cyclone-kenneth-flash-update-no-9-5-may-2019 (accessed on 29 May 2019).
- Anjichi-Kodumbe, T.; Abreu, S.; van Vliet, T. Southern Africa: Tropical Cyclone Kenneth Flash Update No. 13. Available online: https://reliefweb.int/report/mozambique/southern-africa-tropical-cyclone-kenneth-flash-update-no-13-12-may-2019 (accessed on 29 May 2019).
- Miller, B.; Adebayo, B. Cyclone Kenneth: Thousands Evacuated as Mozambique is Hit with the Strongest Storm in its History. Available online: https://edition.cnn.com/2019/04/25/africa/cyclone-kenneth-mozambique-evacuation-intl/index.html (accessed on 30 May 2019).
- Public Health Agency of Canada. Outbreak Reporting Guide, 2015-Canada.ca. Available online: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2015-41/ccdr-volume-41-04-april-2-2015/ccdr-volume-41-04-april-2-2015-1.html (accessed on 24 July 2019).
- Edgar, C. A glance at Mozambican dairy research. Afr. J. Agric. Res. 2018, 13, 2945–2956. [Google Scholar] [CrossRef]
- Channel, B.B. Mozambique Country Profile. Available online: https://www.bbc.com/news/world-africa-13890416 (accessed on 8 August 2019).
- Alvaro. File: Location Mozambique AU Africa.svg. Available online: https://commons.wikimedia.org/wiki/File:Location_Mozambique_AU_Africa.svg (accessed on 24 July 2019).
- World Health Organization. Mozambique’s Health System. Available online: https://www.who.int/countries/moz/areas/health_system/en/index1.html (accessed on 8 August 2019).
- Brown, J.; Cumming, O.; Bartram, J.; Cairncross, S.; Ensink, J.; Holcomb, D.; Knee, J.; Kolsky, P.; Liang, K.; Liang, S.; et al. A controlled, Before-and-After Trial of an Urban Sanitation Intervention to Reduce Enteric Infections in Children: Research Protocol for the Maputo Sanitation (MapSan) study, Mozambique. BMJ Open 2015, 5, e008215. [Google Scholar] [CrossRef] [PubMed]
- United Nations Office for the Coordination of Humanitarian Affairs. CERF allocates US$13M to provide a lifeline to people hit by Tropical Cyclone Kenneth in Comoros and Mozambique. Available online: https://www.unocha.org/story/cerf-allocates-us13m-provide-lifeline-people-hit-tropical-cyclone-kenneth-comoros-and (accessed on 12 June 2019).
- United Nations Office for the Coordination of Humanitarian Affairs. Cyclone Kenneth: Stories of Resilience and Generosity Amid the Destruction. Available online: https://www.unocha.org/story/cyclone-kenneth-stories-resilience-and-generosity-amid-destruction (accessed on 12 June 2019).
- National Health Institute; World Health Organization. Tropical Cyclones Idai and Kenneth, Mozambique National Situation Report 2; National Health Institute, Ministry of Health: Maputo, Mozambique, 2019; p. 12.
- United Nations Office for the Coordination of Humanitarian Affairs. Mozambique: “Aid is free and sexual exploitation and abuse are unacceptable”. Available online: https://www.unocha.org/story/mozambique-aid-free-and-sexual-exploitation-and-abuse-are-unacceptable (accessed on 12 June 2019).
- National Health Institute; World Health Organization. Tropical Cyclones Idai and Kenneth, Mozambique National Situation Report 4; National Health Institute, Ministry of Health: Maputo, Mozambique, 2019; p. 12.
- National Health Institute; World Health Organization. Tropical Cyclones Idai and Kenneth, Mozambique National Situation Report 3; National Health Institute, Ministry of Health: Maputo, Mozambique, 2019; p. 12.
- United Nations Office for the Coordination of Humanitarian Affairs. 2018–2019 Mozambique Humanitarian Response Plan: Revised following Cyclone Idai; United Nations Office for the Coordination of Humanitarian Affairs: New York, NY, USA, 2019. [Google Scholar]
- World Health Organization. WHO | Cholera Case Fatality Rate. Available online: https://www.who.int/gho/epidemic_diseases/cholera/case_fatality_rate_text/en/ (accessed on 31 May 2019).
- Chingwaru, W. Letters to the Editor: How to Keep Cholera and Typhoid at Bay in the Post Cyclone Idai Period. Available online: https://www.chronicle.co.zw/letters-to-the-editor-how-to-keep-cholera-and-typhoid-at-bay-in-the-post-cyclone-idai-period/ (accessed on 31 May 2019).
- United Nations Office for the Coordination of Humanitarian Affairs. Moçambique: Ciclone Kenneth-Pessoas Beneficiadas Pela Assistência Humanitária. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/ocha_kenneth_distributions_20190526.pdf (accessed on 12 June 2019).
- Wheeler, J.; Agha, S. Use of Certeza point-of-use water treatment product in Mozambique. J. Water Sanit. Hyg. Dev. 2013, 3, 341–348. [Google Scholar] [CrossRef]
- Save the Children. What You Need to Know About Cyclone Kenneth. Available online: https://www.savethechildren.org/us/what-we-do/emergency-response/cyclone-kenneth-mozambique (accessed on 24 July 2019).
- UNFPA Procurement Services Branch. UNFPA Basic Dignity Kit. Available online: https://www.unfpa.org/resources/unfpa-basic-dignity-kit (accessed on 12 June 2019).
- Pool, R.; Munguambe, K.; Macete, E.; Aide, P.; Juma, G.; Alonso, P.; Menéndez, C. Community response to intermittent preventive treatment delivered to infants (IPTi) through the EPI system in Manhiça, Mozambique. Trop. Med. Int. Health 2006, 11, 1670–1678. [Google Scholar] [CrossRef] [PubMed]
- Carlos, I. Perfil sociodemográfico e cultural dos munícipes da cidade de Gurué, sua relação com a epidemiologia de cólera. Rev. Moçambicana Ciências Saúde 2018, 4, 256. [Google Scholar]
- Victorino, J.; Savaio, L.; António, M. Mitos e boatos da cólera na província de Nampula Janeiro-Março 2018. Rev. Moçambicana Ciências Saúde 2018, 4, 149. [Google Scholar]
- Knutson, T.R.; McBride, J.L.; Chan, J.C.L.; Emanuel, K.; Holland, G.; Landsea, C.; Held, I.; Kossin, J.P.; Srivastava, A.K.; Sugi, M. Tropical cyclones and climate change. Nat. Geosci. 2010, 3, 157–163. [Google Scholar] [CrossRef] [Green Version]
- Mendelsohn, R.; Emanuel, K.; Chonabayashi, S.; Bakkensen, L. The impact of climate change on global tropical cyclone damage. Nat. Clim. Chang. 2012, 2, 205–209. [Google Scholar] [CrossRef]
- Walsh, K.J.E.; McBride, J.L.; Klotzbach, P.J.; Balachandran, S.; Camargo, S.J.; Holland, G.; Knutson, T.R.; Kossin, J.P.; Lee, T.C.; Sobel, A.; et al. Tropical cyclones and climate change. Wiley Interdiscip. Rev. Clim. Chang. 2016, 7, 65–89. [Google Scholar] [CrossRef]
- Levy, K.; Woster, A.P.; Goldstein, R.S.; Carlton, E.J. Untangling the impacts of climate change on waterborne diseases: A systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ. Sci. Technol. 2016, 50, 4905–4922. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Lu, Y.; Zhou, S.; Chen, L.; Xu, B. Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ. Int. 2016, 86, 14–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, K.; Smith, S.M.; Carlton, E.J. Climate Change Impacts on Waterborne Diseases: Moving Toward Designing Interventions. Curr. Environ. Health Rep. 2018, 5, 272–282. [Google Scholar] [CrossRef] [PubMed]
- O’Dwyer, J.; Dowling, A.; Adley, C. The Impact of Climate Change on the Incidence of Infectious Waterborne Disease. In Urban Water Reuse Handbook; CRC Press: Boca Raton, FL, USA, 2016; pp. 1053–1062. [Google Scholar]


© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cambaza, E.; Mongo, E.; Anapakala, E.; Nhambire, R.; Singo, J.; Machava, E. Outbreak of Cholera Due to Cyclone Kenneth in Northern Mozambique, 2019. Int. J. Environ. Res. Public Health 2019, 16, 2925. https://doi.org/10.3390/ijerph16162925
Cambaza E, Mongo E, Anapakala E, Nhambire R, Singo J, Machava E. Outbreak of Cholera Due to Cyclone Kenneth in Northern Mozambique, 2019. International Journal of Environmental Research and Public Health. 2019; 16(16):2925. https://doi.org/10.3390/ijerph16162925
Chicago/Turabian StyleCambaza, Edgar, Edson Mongo, Elda Anapakala, Robina Nhambire, Jacinto Singo, and Edsone Machava. 2019. "Outbreak of Cholera Due to Cyclone Kenneth in Northern Mozambique, 2019" International Journal of Environmental Research and Public Health 16, no. 16: 2925. https://doi.org/10.3390/ijerph16162925