Implementation of the International Classification of Functioning, Disability, and Health (ICF) Core Sets for Children and Youth with Cerebral Palsy: Global Initiatives Promoting Optimal Functioning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Brazil—Group Level Application—Congenital ZIKA Virus
- Context: The outbreak of Zika in Brazil in 2015–16 has had harmful medical, financial, and social consequences for many children and their families and significantly increased the statistics of Brazilian children with disabilities being followed up at rehabilitation centers. Many families face additional challenges in their daily lives due to poverty as well as structural issues related to the provision of health care and social security. From 2000 to 2014, 2464 live births with microcephaly were recorded in Brazil, with an annual average of 164 cases. In 2015, the number of cases increased nine times in relation to this average, totaling 1608 cases, which led the Ministry of Health to declare a public health emergency [32]. Seventy-one percent of live births with microcephaly were from the Northeast region of the country [33].
- Purpose: To describe the profile of functioning and disability of children with microcephaly following congenital Zika virus infection using an ICF-based tool.
- Participants and Procedures: The convenience sample consisted of 34 children with ZIKV-associated microcephaly in two states of northeastern Brazil, treated at four rehabilitation services in Paraíba and Rio Grande do Norte states. The Brazilian Portuguese version of the Brief Common ICF Core Set for CP was used. Each ICF category was assigned a qualifier, which ranged from 0 to 4 (no problem, mild problem, moderate problem, severe problem, complete problem).Training raters: each participating center held ICF and ICF Core Set training workshops using the ICF educational e-tool (http://learn.phsa.ca/shhc/icf/story_html5.html), as developed by Schiariti et al., 2015 [27]. Training was conducted by E.L. and H.F. (co-authors). The goal of the workshops was to consolidate the ICF theoretical and practical concepts, and to ensure the high inter-rater reliability of the qualifiers in each ICF Core Set category. Overall, a 16-h educational module was completed by health professionals that were involved in the study.Translating clinical information into ICF qualifiers in Brazil: The qualifiers to obtain the functional profile were generated through sensitive, reliable and validated instruments in Brazil [34], such as: Pediatric Evaluation of Disability Inventory (PEDI); Gross Motor Function Measure (GMFM—88); Visual Analog Scale (EVA); Infant Sleep Questionnaire (ISQ); Modified Ashworth Scale and Goniometry. Most of these measures are recommended in the ICF-based toolbox of measures aligning with the content of the CP core sets [35]. Scores were converted into ICF qualifiers either using clinical judgment—teamwork—or from visual response cards. For the categories that did not have available tools, a specific questionnaire was applied to parents or caregivers, whose responses were converted through the visual response cards into ICF qualifiers. The socio-demographic characteristics, cephalic perimeter, and other clinical data were collected through medical records, physical exams, imaging reports, and interviews with the children and their respective parents. Using the ICF-based documentation form, the ICF Core Set for CP was populated to create the profile of functioning of the sample [36]. Licensed physiotherapists in each center, who were familiar with each standardized test and completed the ICF training, were in charge of administering the tests and also translating the information into the ICF qualifiers. They were supervised by professor E.L. (co-author).Some examples on how clinical information was translated into the ICF qualifiers is provided below:
- ○
- The category s110 (structure of brain) was determined while considering the results of imaging exams (Nuclear Magnetic Resonance, Computed Tomography, or Trans fontanel Ultrasonography). For example, Computed Tomography demonstrating multiple calcifications at the cortical-white matter, predominating in temporal lobes, the qualifier 3 was assigned.
- ○
- The category d710 (Basic interpersonal interactions) was captured by the PEDI, using the Social function area, items F and G, interactive social game, and interaction with friends, respectively. When the answer was 0, the qualifier 4 was assigned.
- ○
- The category e120 (Products and technology for personal indoor and outdoor mobility and transportation) was assessed by a self-developed question: “Does the child need assistive devices to help in locomotion? How much does this help or hinder the child’s functioning?” To translate this information into the ICF language, firstly, the caregiver stated if the assistive device was considered to be a facilitator or a barrier. Secondly, the caregiver’s perspective on how much this environmental factor influenced the child’s functioning was captured while using the study visual response card. The caregiver’s response was mapped into the ICF qualifier (facilitator or barrier) [34].
2.2. Russia—System Level Application
- Context: CP represents a leading cause of childhood physical disability in Russia with an estimated prevalence of 2–4 cases per 1000 live births [37] (the multiple health and social services for CP available in the country, there is no systematic or standardized care pathway for this population. To obtain national and internationally comparable data in the assessment of CP, and to evaluate the effectiveness of rehabilitation efforts for children with CP, standardized tools are required).
- Purpose: To adopt the ICF Core Set in Russia as a guiding tool to design rehabilitation and habilitation programs for children with CP.
- Participants and Procedures: Participants were recruited from the Medical Social Expertise Service in St. Petersburg and Voronezh region. Overall rehabilitation programmes for 142 children were developed. Participants ages ranged from 1.5 to 18 years old, 34.4% of them were children under six years old, 36.6% were from seven to 13 and 28.8% were from 14 to 18.
- A rehabilitation algorithm was designed for CP, as follows:
- ○
- Identification of key concerns impacting daily functioning.
- ○
- Application of the Comprehensive and Common Brief ICF Core Sets for CP to be used as guiding framework for assessments and evaluations.
- ○
- Building a profile of functioning for each child, and subsequently identifying rehabilitation tasks, including key ICF categories to target as goals for intervention.
- ○
- Selection of rehabilitation instruments and therapeutic interventions aligning with the rehabilitation plan.
2.3. Poland—Rehabilitation Center Application
- Context: The Step by Step Association for help of disabled children in Zamość (Poland) was established in 1990 and is a non-governmental organization uniting parents, caregivers, and friends of children, adolescents and disabled adults. (complete information here http://www.spdn.pl/) The center was founded by Dr Maria Krol, physician and mother of a young man with CP. Her caring and passionate work has provided a supportive and exceptional educational and rehabilitation center for children and youth with disabilities and their families in Zamość. The city of Zamość is in southeastern Poland; with a population of approximately 70,000 people. The historical centre of Zamość was added to the UNESCO World Heritage List in 1992. The Step by Step Association for help of disabled children is unique in the region of south-eastern Poland and leads professional activities in the field of integrated rehabilitation, education and social support of children, adolescents, and disabled adults with early brain damage. It includes comprehensive rehabilitation, education, and care for approximately 2000 people (150 children in daily care system—primarily the Integrated Rehabilitation System, 100 disabled people are covered by daily occupational therapy, and 1,800 people are in outpatient care). Services in the region are provided in eight facilities (Zamość centre, Biłgoraj centre, Occupation Therapy Workshops in Zamość and Biłgoraj, Centres for Social Activation in Zamość and Białobrzegi, Day Care Centre for Adults in Białobrzegi and Therapy and Recreation Park in Bondyrz). The Zamość centre leads day care, pre-school education, primary, secondary, and high school classes, which prepare adolescents for vocational training and employment.
- Purpose: To incorporate the ICF Core Sets for CP to guide the assessment process of children and youth with CP.
- Participants and Procedures: Children and youth with neurodevelopmental disabilities, including CP, spina bifida, and acquired brain injuries, attend the Step by Step Association for help of disabled children. The Zamość centre serves children from infancy to young adults (until the age of 25 years). Children are referred to the centre by physicians, psychologists, and other specialists, and they can also come directly without referral. Since the publication of the ICF Core Sets for children and youth with CP in 2015, the Step by Step has validated the tools using caregivers’ and clients’ perspectives. Following the ICF Core Sets user instructions, the team uses the ICF Core Sets as a condition-specific framework to select the most appropriate valid and reliable assessment tools. The child or youth’ perspectives about his/her functional abilities and expectations are incorporated as goals for interventions.
2.4. Malawi—Community-Based Rehabilitation Application
- Context: Malawi is a low-income country and it sits among the poorest countries in the world. Despite Malawian’s efforts to improve health care in the last years, there still exists barriers to accessing health system. The World Report on Disability from WHO shows that besides 83.4% of people needs health services, but only 61% really receive it. The same challenge is seen in the provision of rehabilitation services: 59.6% people with disabilities need rehabilitation services, but only 23.8% of them receive it. There are no data from CP prevalence in Malawi, but some studies in African countries shows a prevalence of 2–10 per 1000 children in community-based samples. Moreover, there is no national data regarding the impact of CP on everyday functioning and disability in pediatric populations.
- Purpose: To inspect the feasibility of the implementation of the ICF Core Sets for CP in a Malawian pediatric population diagnosed with CP.
- Participants and Procedures: Participants consisted of children between 0 to 18 years, recruited from the CBR program of an NGO operating in Malawi. Recruitment included 18 children and youth with CP. All participants were recruited in a rural area, where secondary and tertiary health care services are only in nearby cities, about two or three hours away A health care professional, familiar with the use of the ICF guided the assessments (C.V.). A local team collaborated in the project (D.S., M.M.). Information was gathered during clinical interviews and examinations. Additional information that was provided by the children and/or caregivers was also collected and linked to the ICF. The content validity of the ICF Core Sets was evaluated while using the frequency and percentage of subjects who had a strength/problem in each category.
3. Results
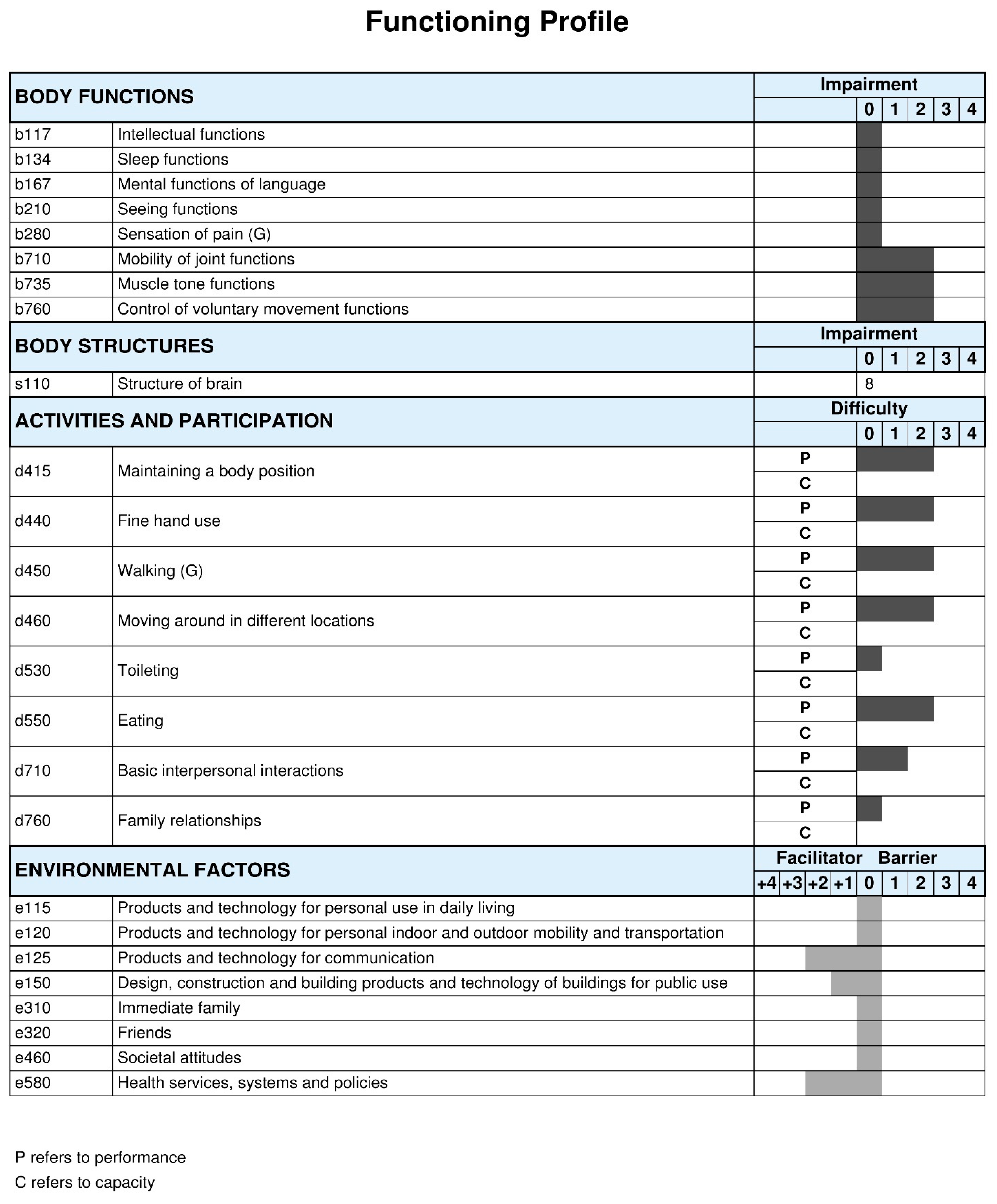
3.1. Brazil—Group Level
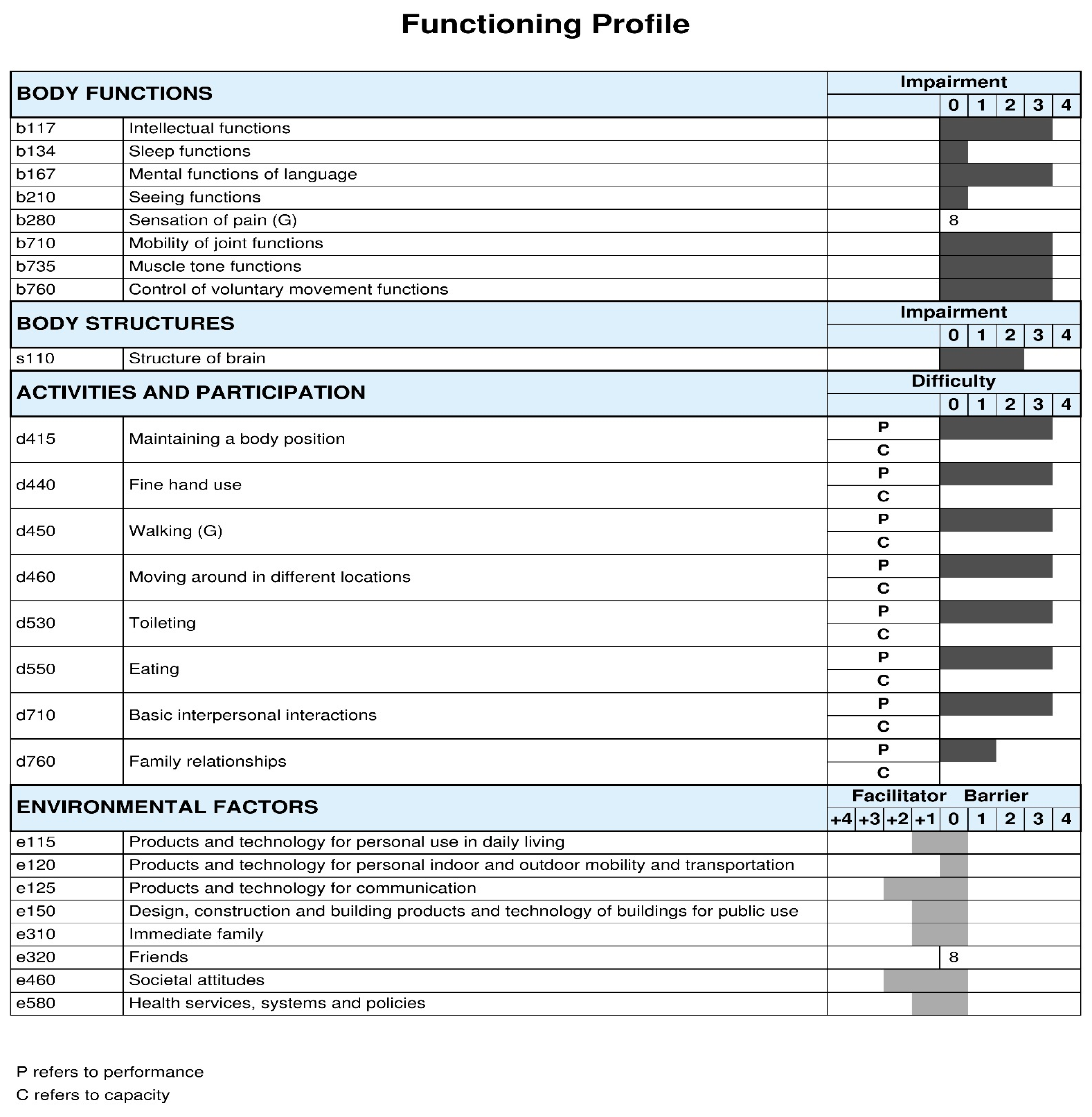
3.2. Russia–-System Level Applilcation
3.3. Poland—Rehabilitation Center Application
3.3.1. Service Delivery Model and the ICF in Zamość
3.3.2. Service Delivery Model and the ICF Core Sets for CP in Zamość
3.4. Malawi—Community-Based Rehabilitation Application
4. Discussion
4.1. Contributions and Challenges of Using the ICF Core Sets for CP
4.2. ICF Core Sets for CP and Impact on Outcomes, Clinical Pracice, and Policy-Making
4.3. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A Report: The Definition and Classification of Cerebral Palsy April 2006. Dev. Med. Child Neurol. 2007, 109, 8–14. [Google Scholar]
- Mesterman, R.; Leitner, Y.; Yifat, R.; Gilutz, G.; Levi-Hakeini, O.; Bitchonsky, O.; Rosenbaum, P.; Harel, S. Cerebral Palsy--Long-Term Medical, Functional, Educational, and Psychosocial Outcomes. J. Child Neurol. 2010, 25, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Majnemer, A.; Shevell, M.; Law, M.; Poulin, C.; Rosenbaum, P.L. Indicators of Distress in Families of Children with Cerebral Palsy. Developmental Medicine and Child Neurology. In Proceedings of the 64th Annual Meeting of the American Academy for Cerebral Palsy and Developmental Medicine, Washington, DC, USA, 22–25 September 2010; Volume 52, pp. 32–33. [Google Scholar]
- BourkeTaylor, H.; Lalor, A.; Farnworth, L.; Pallant, J.F.; Knightbridge, E.; Mclelland, G. Investigation of the Self-Reported Health and Health-Related Behaviours of Victorian Mothers of School-Aged Children. Aust. J. Prim. Health 2015, 21, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Eker, L.; Tuzun, E.H. An Evaluation of Quality of Life of Mothers of Children with Cerebral Palsy. Disabil. Rehabil. 2004, 26, 1354–1359. [Google Scholar] [CrossRef] [PubMed]
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S. Cerebral Palsy. Nat. Rev. Dis. Primers 2016. [Google Scholar] [CrossRef]
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jette, N.; Pringsheim, T. An Update on the Prevalence of Cerebral Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, M. A Review of the Incidence and Prevalence, Types and Aetiology of Childhood Cerebral Palsy in Resource-Poor Settings. Ann. Trop. Paediatr. 2010, 30, 181–196. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, B.; Hagberg, G.; Olow, I.; van Wendt, L. The Changing Panorama of Cerebral Palsy in Sweden. VII. Prevalence and Origin in the Birth Year Period 1987–1990. Acta Paediatr. 1996, 85, 954–960. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Hines, M.; Goldsmith, S.; Barclay, R. Clinical Prognostic Messages from a Systematic Review on Cerebral Palsy. Pediatrics 2012, 130, e1285–e1312. [Google Scholar] [CrossRef] [PubMed]
- Shih, S.T.F.; Tonmukayakul, U.; Imms, C.; Reddihough, D.; Graham, H.K.; Cox, L.; Carter, R. Economic Evaluation and Cost of Interventions for Cerebral Palsy: A Systematic Review. Dev. Med. Child Neurol. 2018, 60, 543–558. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Masse, L.C. Identifying Relevant Areas of Functioning in Children and Youth with Cerebral Palsy using the ICF-CY Coding System: From Whose Perspective? Eur. J. Paediatr. Neurol. 2014, 18, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Sauve, K.; Klassen, A.F.; O’Donnell, M.; Cieza, A.; Masse, L.C. ‘He does Not See Himself as being Different’: The Perspectives of Children and Caregivers on Relevant Areas of Functioning in Cerebral Palsy. Dev. Med. Child Neurol. 2014, 56, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; Davis, E.; Ronen, G.M.; Rosenbaum, P.; Livingston, M.; Saigal, S. Quality of Life Instruments for Children and Adolescents with Neurodisabilities: How to Choose the Appropriate Instrument. Dev. Med. Child Neurol. 2009, 51, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, M.F.; Nor, N.M.; Mohd Ali, S.Z.; Ismail Bukhary, N.B.; Amat, A.; Latif, L.A.; Hasnan, N.; Omar, Z. Validation of the Comprehensive ICF Core Sets for Diabetes Mellitus: A Malaysian Perspective. Ann. Acad. Med. Singap. 2011, 40, 168. [Google Scholar] [PubMed]
- James, S.; Ziviani, J.; Boyd, R. A Systematic Review of Activities of Daily Living Measures for Children and Adolescents with Cerebral Palsy. Dev. Med. Child Neurol. 2014, 56, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Klassen, A.F.; Cieza, A.; Sauve, K.; O’Donnell, M.; Armstrong, R.; Masse, L.C. Comparing Contents of Outcome Measures in Cerebral Palsy using the International Classification of Functioning (ICF-CY): A Systematic Review. Eur. J. Paediatr. Neurol. 2014, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Mcintyre, S.; Morgan, C.; Campbell, L.; Dark, L.; Morton, N.; Stumbles, E.; Wilson, S.-A.; Goldsmith, S. A Systematic Review of Interventions for Children with Cerebral Palsy: State of the Evidence. Dev. Med. Child Neurol. 2013, 55, 885–910. [Google Scholar] [CrossRef] [PubMed]
- WHO (World Health Organization). International Classification of Functioning Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- WHO (World Health Organization). International Classification of Functioning Disability and Health Children Youth Version; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Schiariti, V.; Selb, M.; Cieza, A.; O’Donnell, M. International Classification of Functioning, Disability and Health Core Sets for Children and Youth with Cerebral Palsy: A Consensus Meeting. Dev. Med. Child Neurol. 2015, 57, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Bolte, S.; Mahdi, S.; de Vries, P.J.; Granlund, M.; Robison, J.E.; Shulman, C.; Swedo, S.; Tonge, B.; Wong, V.; Zwaigenbaum, L. The Gestalt of Functioning in Autism Spectrum Disorder: Results of the International Conference to Develop Final Consensus International Classification of Functioning, Disability and Health Core Sets. Autism 2018. [Google Scholar] [CrossRef]
- Bolte, S.; Mahdi, S.; Coghill, D.; Gau, S.S.F.; Granlund, M.; Holtmann, M.; Karande, S.; Levy, F.; Rohde, L.A.; Segerer, W. Standardised Assessment of Functioning in ADHD: Consensus on the ICF Core Sets for ADHD. Eur. Child Adolesc. Psychiatry 2018, 1–21. [Google Scholar] [CrossRef]
- Schiariti, V.; Mahdi, S.; Bolte, S. International Classification of Functioning, Disability and Health Core Sets for Cerebral Palsy, Autism Spectrum Disorder, and Attention-Deficit-Hyperactivity Disorder. Dev. Med. Child Neurol. 2018, 60, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Selb, M.; Cieza, A.; O’Donnell, M. International Classification of Functioning, Disability and Health Core Sets for Children and Youth with CP: Contributions to Clinical Practice. Dev. Med. Child Neurol. 2015, 57, 203–204. [Google Scholar] [CrossRef] [PubMed]
- Schiarit, V.; Tatla, S.; Dunn, A.; Sauve, K.; O’Donnell, M. ICF Educational e-Tool. Available online: http://learn.phsa.ca/shhc/icf/story_html5.html (accessed on 10 January 2016).
- Liao, H.F.; Hwang, A.W.; Liou, T.; Yen, C.F.; Chi, W.C.; Schiariti, V.; Hung, H.C.; Teng, S. Validating the ICF Core Set for Cerebral Palsy by using National Disability Sample in Taiwan. In Proceedings of the 27th Annual Meeting of the European Academy of Childhood Disability, Copenhagen, Denmark, 27–30 May 2015. [Google Scholar]
- Shoshmin, A.; Besstrashnova, Y.; Schiariti, V. Development of National (Re)Habilitation Guidelines Based on the ICF Core Sets for Children and Youth with Cerebral Palsy in Russia: A Novel Approach. WHOFIC Booklet, 2016. Available online: www.who.int/classifications/network/2017_WHOFIC_Poster_Booklet.zip?ua=1 (accessed on 2 February 2017).
- Schiariti, V.; Ibrahim, S.; Bhattacharya, A.; Król, M. ICF Core Sets for Children and Youth with CP: Embracing Cultural Differences. WHOFIC Booklet, 2016. Available online: www.who.int/classifications/network/2017_WHOFIC_Poster_Booklet.zip?ua=1 (accessed on 2 February 2017).
- Raji, P.; Hassani Mehraban, A.; Aliabadi, F.; Ahmadi, M.; Schiariti, V. Content Validity of the Comprehensive ICF Core Set for Children with Cerebral Palsy Aged 0–6 Years: Iranian Occupational Therapists Perspective. Iran. J. Child Neurol. 2018, 12, 40–58. [Google Scholar] [PubMed]
- Kleber de Oliveira, W.; CortezEscalante, J.; De Oliveira, W.T.; do Carmo, G.M.; Henriques, C.M.; Coelho, G.E.; Araujo de Franca, G.V. Increase in Reported Prevalence of Microcephaly in Infants Born to Women Living in Areas with Confirmed Zika Virus Transmission during the First Trimester of Pregnancy—Brazil, 2015. Morb. Mortal. Wkly. Rep. 2016, 65, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Van der Linden, V.; Pessoa, A.; Dobyns, W.; Barkovich, A.J.; Junior, H.V.; Filho, E.L.; Ribeiro, E.M.; Leal, M.C.; Coimbra, P.P.; Aragao, M.F. Description of 13 Infants Born during October 2015-January 2016 with Congenital Zika Virus Infection without Microcephaly at Birth—Brazil. Morb. Mortal. Wkly. Rep. 2016, 65, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, H.N.C.; Schiariti, V.; Regalado, I.C.R.; Sousa, K.G.; Pereira, S.A.; Fechine, C.P.N.S.; Longo, E. Functioning and Disability Profile of Children with Microcephaly Associated with Congenital Zika Virus Infection. Int. J. Environ. Res. Public Health 2018, 15, 1107. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Tatla, S.; Sauve, K.; O’Donnell, M. Toolbox of Multiple-Item Measures Aligning with the ICF Core Sets for Children and Youth with Cerebral Palsy. Eur. J. Paediatr. Neurol. 2017, 21, 252–263. [Google Scholar] [CrossRef] [PubMed]
- ICF Research Branch. ICF-Based Documentation Form. Available online: https://www.icf-core-sets.org/ (accessed on 5 December 2017).
- Ministry of Health of the Russian Federation. Consequences of Perinatal Involvement of the Central Nervous System with Atonic-Astatic Syndrome. Russian Clinical Guidelines. 2017. Available online: http://cr.rosminzdrav.ru/#!/schema/240 (accessed on 5 January 2018).
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and Reliability of a System to Classify Gross Motor Function in Children with Cerebral Palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.J.; Rosenbaum, P.; Bartlett, D.; Livingston, M.H. Content Validity of the Expanded and Revised Gross Motor Function Classification System. Dev. Med. Child Neurol. 2008, 50, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Shoshmin, A.; Ponomarenko, G. ICF in Rehabilitation; CIACAN and R-COPY: St. Petersburg, Russia, 2018; ISBN 978-5-6041435-4-4. [Google Scholar]
- Schiariti, V.; Fowler, E.; Brandenburg, J.E.; Levey, E.; Mcintyre, S.; Sukal-Moulton, T.; Ramey, S.L.; Rose, J.; Sienko, S.; Stashinko, E. A Common Data Language for Clinical Research Studies: The National Institute of Neurological Disorders and Stroke and American Academy for Cerebral Palsy and Developmental Medicine Cerebral Palsy Common Data Elements Version 1.0 Recommendations. Dev. Med. Child. Neurol. 2018. [Google Scholar] [CrossRef]
- Schiariti, V.; Fowler, E.; Brandenburg, J.E.; Levey, E.; Mcintyre, S.; Sukal-Moulton, T.; Ramey, S.L.; Rose, J.; Sienko, S.; Stashinko, E. Standardized Care and Individualized Care: Do they Complement or Oppose each Other? Reply to Commentary by Charlie Fairhurst. Dev. Med. Child Neurol. 2018, in press. [Google Scholar]



| BRAZIL N = 34 | RUSSIA N = 142 | MALAWI N = 18 | |
|---|---|---|---|
| AGE (years) | Mean = 1.8 ± SD 6 | Mean = 5.4 ± SD 3.74 | 8.6 ± SD 5.0 |
| Gender | Male 47% | Male 65% | Male 44% |
| GMFCS level (%) | IV (32.4%), V (67.6%) | I (4%) II (16%) III (32%) IV (21%) V (26%) | III (27.8%), IV (27.8%), V (44.4%) |
| Type of CP (%) | Spastic Bilateral (76.5%) | Spastic Bilateral (72%) | NA |
| Comorbidities | |||
| Intellectual disabilities | 97.1% | 29% | NA |
| Learning or behavioural disabilities | NA | 33% | NA |
| Vision difficulties | 67.6% | 4% | NA |
| Epilepsy | NA | 12% | 11.1% |
| Caregiver characteristics | Monthly Income Up to 300 US dollars = 67.7% 300 to 600 US dollars = 35.3% | NA | NA |
| Schooling Complete elementary education = 17.6% Incomplete elementary education = 14.7% Complete secondary education = 47.1% Others = 20.6% | Incomplete elementary education = 14.3 % (including home education = 0.9%) Incomplete secondary education = 50.0 % (including home education = 22.3%) Others = 12.5% | NA |
| Brief ICF Core Set for CP | ICF Qualifiers, % Distribution among Children GMFCS Levels I to III | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 8 | 9 | |||||
| b117 | 66.67 | 22.22 | 7.41 | 3.70 | 0.00 | 0.00 | 0.00 | ||||
| b134 | 96.43 | 3.57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| b167 | 39.29 | 21.43 | 35.71 | 3.57 | 0.00 | 0.00 | 0.00 | ||||
| b210 | 75.00 | 25.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| b280 | 53.57 | 0.00 | 0.00 | 0.00 | 0.00 | 46.43 | 0.00 | ||||
| b710 | 0.00 | 10.71 | 71.43 | 17.86 | 0.00 | 0.00 | 0.00 | ||||
| b735 | 0.00 | 0.00 | 71.43 | 28.57 | 0.00 | 0.00 | 0.00 | ||||
| b760 | 0.00 | 0.00 | 74.07 | 22.22 | 3.70 | 0.00 | 0.00 | ||||
| 0 | 1 | 2 | 3 | 4 | 8 | 9 | |||||
| s110 | degree | 10.71 | 14.29 | 21.43 | 0.00 | 0.00 | 53.57 | 0.00 | |||
| nature of the change | 11.11 | 14.81 | 22.22 | 0.00 | 0.00 | 51.85 | 0.00 | ||||
| location | 11.11 | 14.81 | 22.22 | 0.00 | 0.00 | 51.85 | 0.00 | ||||
| 0 | 1 | 2 | 3 | 4 | 8 | 9 | |||||
| d415 | Р | 0.00 | 0.00 | 75.00 | 21.43 | 3.57 | 0.00 | 0.00 | |||
| d440 | Р | 7.14 | 0.00 | 64.29 | 25.00 | 3.57 | 0.00 | 0.00 | |||
| d450 | Р | 0.00 | 0.00 | 65.38 | 30.77 | 3.85 | 0.00 | 0.00 | |||
| d460 | Р | 0.00 | 0.00 | 70.37 | 25.93 | 3.70 | 0.00 | 0.00 | |||
| d530 | Р | 67.86 | 25.00 | 0.00 | 7.14 | 0.00 | 0.00 | 0.00 | |||
| d550 | Р | 10.71 | 7.14 | 67.86 | 10.71 | 3.57 | 0.00 | 0.00 | |||
| d710 | Р | 29.63 | 48.15 | 18.52 | 3.70 | 0.00 | 0.00 | 0.00 | |||
| d760 | Р | 71.43 | 25.00 | 3.57 | 0.00 | 0.00 | 0.00 | 0.00 | |||
| 4 | 3 | 2 | 1 | 0 | 1 | 2 | 3 | 4 | 8 | 9 | |
| e115 | 0 | 0.00 | 32.14 | 14.29 | 53.57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| e120 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 |
| e125 | 0 | 0.00 | 62.50 | 12.50 | 25.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| e150 | 0 | 0.00 | 3.57 | 35.71 | 50.00 | 0.00 | 0.00 | 0.00 | 0.00 | 10.71 | 0.00 |
| e310 | 10.71 | 0.00 | 7.14 | 14.29 | 60.71 | 3.57 | 0.00 | 0.00 | 0.00 | 3.57 | 0.00 |
| e320 | 0 | 4.00 | 0.00 | 8.00 | 72.00 | 4.00 | 0.00 | 0.00 | 0.00 | 12.00 | 0.00 |
| e460 | 0 | 0.00 | 0.00 | 0.00 | 87.50 | 12.50 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| e580 | 0 | 0.00 | 37.50 | 25.00 | 37.50 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Brief ICF Core Set for CP | ICF Qualifiers, % Distribution among Children GMFCS Levels IV to V | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | 0 | 1 | 2 | 3 | 4 | 8 | 9 | ||||
| b117 | 3.03 | 9.09 | 21.21 | 51.52 | 15.15 | 0.00 | 0.00 | ||||
| b134 | 75.76 | 15.15 | 9.09 | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| b167 | 9.09 | 9.09 | 15.15 | 51.52 | 15.15 | 0.00 | 0.00 | ||||
| b210 | 63.64 | 30.30 | 0.00 | 0.00 | 6.06 | 0.00 | 0.00 | ||||
| b280 | 39.39 | 0.00 | 0.00 | 0.00 | 0.00 | 60.61 | 0.00 | ||||
| b710 | 3,03 | 0.00 | 33.33 | 48.48 | 15.15 | 0.00 | 0.00 | ||||
| b735 | 0.00 | 0.00 | 6.06 | 66.67 | 27.27 | 0.00 | 0.00 | ||||
| b760 | 0.00 | 0.00 | 0.00 | 69.70 | 30.30 | 0.00 | 0.00 | ||||
| 0 | 1 | 2 | 3 | 4 | 8 | 9 | |||||
| s110 | degree | 3.03 | 6.06 | 33.33 | 24.24 | 3.03 | 30.30 | 0.00 | |||
| nature of the change | 3.03 | 6.06 | 33.33 | 24.24 | 3.03 | 30.30 | 0.00 | ||||
| location | 3.03 | 6.06 | 33.33 | 24.24 | 3.03 | 30.30 | 0.00 | ||||
| 0 | 1 | 2 | 3 | 4 | 8 | 9 | |||||
| d415 | Р | 0.00 | 0.00 | 0.00 | 68.75 | 31.25 | 0.00 | 0.00 | |||
| d440 | Р | 0.00 | 0.00 | 0.00 | 68.75 | 31.25 | 0.00 | 0.00 | |||
| d450 | Р | 0.00 | 0.00 | 3.23 | 67.74 | 29.03 | 0.00 | 0.00 | |||
| d460 | Р | 0.00 | 0.00 | 0.00 | 68.75 | 31.25 | 0.00 | 0.00 | |||
| d530 | Р | 6.25 | 6.25 | 0.00 | 53.13 | 9.38 | 25.00 | 0.00 | |||
| d550 | Р | 0.00 | 6.25 | 6.25 | 59.38 | 28.13 | 0.00 | 0.00 | |||
| d710 | Р | 0.00 | 9.38 | 15.63 | 65.63 | 9.38 | 0.00 | 0.00 | |||
| d760 | Р | 25.00 | 50.00 | 9.38 | 12.50 | 3.13 | 0.00 | 0.00 | |||
| 4 | 3 | 2 | 1 | 0 | 1 | 2 | 3 | 4 | 8 | 9 | |
| e115 | 0 | 6.25 | 31.25 | 59.38 | 3.13 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| e120 | 0 | 0 | 2.82 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 96.48 |
| e125 | 0 | 28.57 | 28.57 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 28.57 | 14.29 |
| e150 | 0 | 0.00 | 0.00 | 77.42 | 9.68 | 0.00 | 0.00 | 0.00 | 0.00 | 12.90 | 0.00 |
| e310 | 3,03 | 0.00 | 21.21 | 51.52 | 18.18 | 0.00 | 0.00 | 0.00 | 0.00 | 6.06 | 0.00 |
| e320 | 0 | 0.00 | 0.00 | 37.50 | 9.38 | 0.00 | 0.00 | 0.00 | 0.00 | 46.88 | 6.25 |
| e460 | 0 | 25.00 | 0.00 | 25.00 | 25.00 | 25.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| e580 | 0 | 20.00 | 0.00 | 60.00 | 20.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schiariti, V.; Longo, E.; Shoshmin, A.; Kozhushko, L.; Besstrashnova, Y.; Król, M.; Neri Correia Campos, T.; Náryma Confessor Ferreira, H.; Verissimo, C.; Shaba, D.; et al. Implementation of the International Classification of Functioning, Disability, and Health (ICF) Core Sets for Children and Youth with Cerebral Palsy: Global Initiatives Promoting Optimal Functioning. Int. J. Environ. Res. Public Health 2018, 15, 1899. https://doi.org/10.3390/ijerph15091899
Schiariti V, Longo E, Shoshmin A, Kozhushko L, Besstrashnova Y, Król M, Neri Correia Campos T, Náryma Confessor Ferreira H, Verissimo C, Shaba D, et al. Implementation of the International Classification of Functioning, Disability, and Health (ICF) Core Sets for Children and Youth with Cerebral Palsy: Global Initiatives Promoting Optimal Functioning. International Journal of Environmental Research and Public Health. 2018; 15(9):1899. https://doi.org/10.3390/ijerph15091899
Chicago/Turabian StyleSchiariti, Verónica, Egmar Longo, Alexander Shoshmin, Ludmila Kozhushko, Yanina Besstrashnova, Maria Król, Taynah Neri Correia Campos, Haryelle Náryma Confessor Ferreira, Cláudia Verissimo, Daniel Shaba, and et al. 2018. "Implementation of the International Classification of Functioning, Disability, and Health (ICF) Core Sets for Children and Youth with Cerebral Palsy: Global Initiatives Promoting Optimal Functioning" International Journal of Environmental Research and Public Health 15, no. 9: 1899. https://doi.org/10.3390/ijerph15091899
APA StyleSchiariti, V., Longo, E., Shoshmin, A., Kozhushko, L., Besstrashnova, Y., Król, M., Neri Correia Campos, T., Náryma Confessor Ferreira, H., Verissimo, C., Shaba, D., Mwale, M., & Amado, S. (2018). Implementation of the International Classification of Functioning, Disability, and Health (ICF) Core Sets for Children and Youth with Cerebral Palsy: Global Initiatives Promoting Optimal Functioning. International Journal of Environmental Research and Public Health, 15(9), 1899. https://doi.org/10.3390/ijerph15091899






