Comparison of Factors Associated with Fear of Falling between Older Adults with and without a Fall History
Abstract
:1. Introduction
2. Materials and Methods
2.1. Description of Data Sources
2.2. Design and Sample
2.3. Ethical Considerations
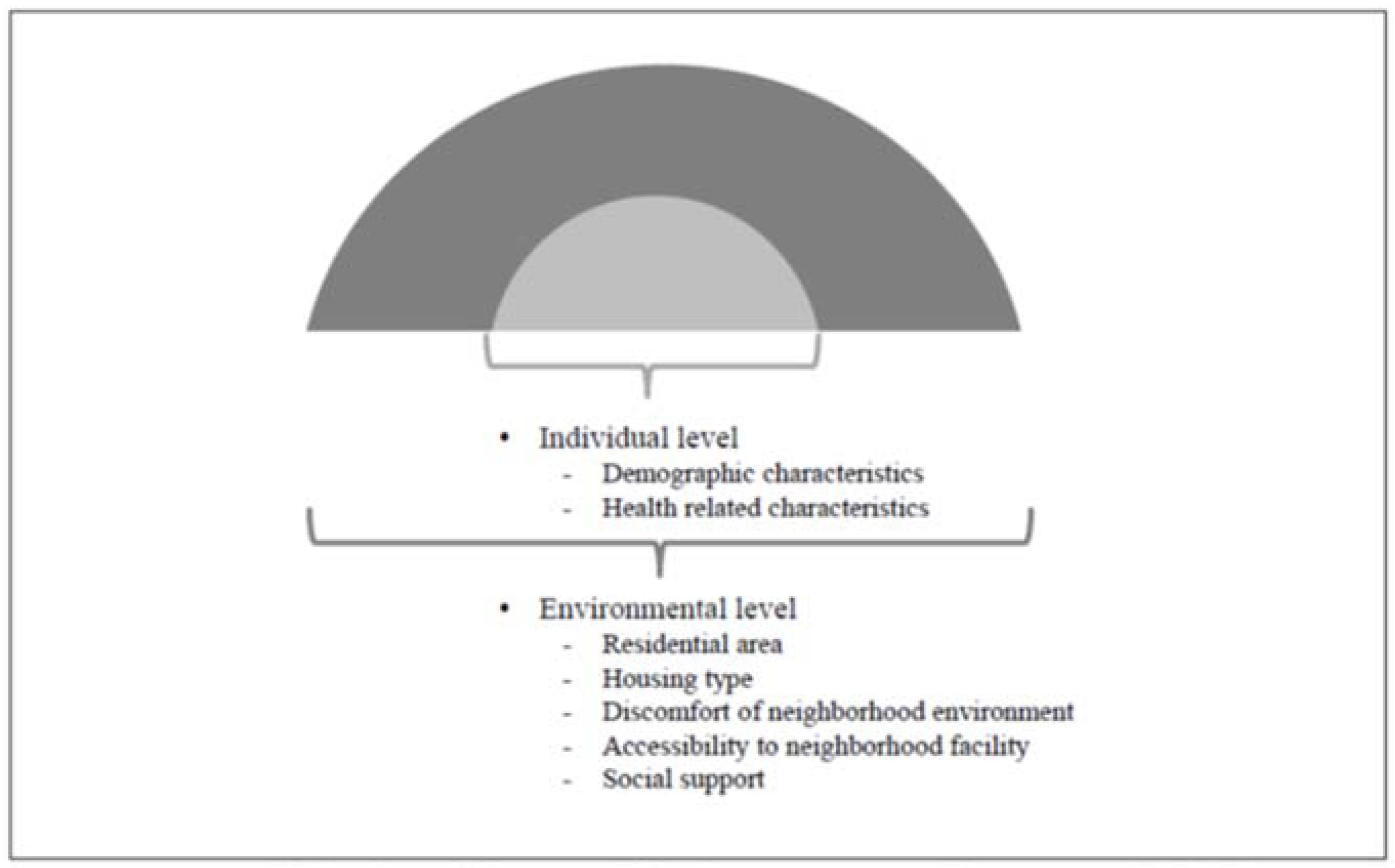
2.4. Measurements
2.4.1. Fear of Falling
2.4.2. Individual Level Characteristics
2.4.3. Environmental Level Characteristics
2.4.4. Fall History
2.5. Data Analysis
3. Results
3.1. Differences in FOF According to Individual Characteristics of Participants with and without a Fall History
3.2. Differences in FOF According to Environmental Characteristics of the Participants with and without a Fall History
3.3. Associations between Fall History and Individual and Environment Characteristics
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Verma, S.K.; Willetts, J.L.; Corns, H.L.; Marucci-Wellman, H.R.; Lombardi, D.A.; Courtney, T.K. Falls and fall-related injuries among community-dwelling adults in the United States. PLoS ONE 2016, 11, e0150939. [Google Scholar] [CrossRef] [PubMed]
- Gazibara, T.; Kurtagic, I.; Kisic-Tepavcevic, D.; Nurkovic, S.; Kovacevic, N.; Gazibara, T.; Pekmezovic, T. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics 2017, 17, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Manemann, S.M.; Chamberlain, A.M.; Boyd, C.; Weston, S.A.; Jiang, R.; Roger, V.L. Fall risk and outcomes in cardiovascular disease-A community study. Circulation 2016, 134 (Suppl. 1), A15665. [Google Scholar]
- Chang, H.T.; Chen, H.C.; Chou, P. Fear of falling and mortality among community-dwelling older adults in the Shih-Pai study in Taiwan: A longitudinal follow-up study. Geriatr. Gerontol. Int. 2017, 17, 2216–2223. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Falls Fact Sheets: Fall. Available online: http://www.who.int/mediacentre/factsheets/fs344/en/ (accessed on 12 April 2017).
- Burns, E.R.; Stevens, J.A.; Lee, R. The direct costs of fatal and non-fatal falls among older adults-United States. J. Saf. Res. 2016, 58, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Mishra, N.; Mishra, A.K.; Bidija, M. A study on correlation between depression, fear of fall and quality of life in elderly individuals. Int. J. Res. Med. Sci. 2017, 5, 1456–1460. [Google Scholar] [CrossRef]
- Gaxatte, C.; Nguyen, T.; Chourabi, F.; Salleron, J.; Pardessus, V.; Delabrière, I.; Thévenon, A.; Puisieux, F. Fear of falling as seen in the multidisciplinary falls consultation. Ann. Phys. Rehabil. Med. 2011, 54, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Bruce, D.; Hunter, M.; Peters, K.; Davis, T.; Davis, W. Fear of falling is common in patients with type 2 diabetes and is associated with increased risk of falls. Age Ageing 2015, 44, 687–690. [Google Scholar] [CrossRef] [PubMed]
- Rantakokko, M.; Manty, M.; Iwarsson, S.; Tormakangas, T.; Leinonen, R.; Heikkinen, E.; Rantanen, T. Fear of moving outdoors and development of outdoor walking difficulty in older people. J. Am. Geriatr. Soc. 2009, 57, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Ayesha, A.; Sadia, M.; Nawaz, M.A. Relationship between fear fall & balance in community dwelling older adults. Pak. J. Neurol. Sci. 2015, 10, 5–8. [Google Scholar]
- Dierking, L.; Markides, K.; Al Snih, S.; Kristen Peek, M. Fear of falling in older Mexican Americans: A longitudinal study of incidence and predictive factors. J. Am. Geriatr. Soc. 2016, 64, 2560–2565. [Google Scholar] [CrossRef] [PubMed]
- Oh, E.; Hong, G.R.S.; Lee, S.; Han, S. Fear of falling and its predictors among community-living older adults in Korea. Aging Ment. Health 2017, 21, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Filiatrault, J.; Desrosiers, J.; Trottier, L. An exploratory study of individual and environmental correlates of fear of falling among community-dwelling seniors. J. Aging Health 2009, 21, 881–894. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; So, W.Y. Prevalence and correlates of fear of falling in Korean community-dwelling elderly subjects. Exp. Gerontol. 2013, 48, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Denkinger, M.D.; Lukas, A.; Nikolaus, T.; Hauer, K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: A systematic review. Am. J. Geriatr. Psychiatry 2015, 23, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Scheffer, A.C.; Schuurmans, M.J.; Van Dijk, N.; Van der Hooft, T.; De Rooij, S.E. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008, 37, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Jung, D. Fear of falling in older adults: Comprehensive review. Asian Nurs. Res. 2008, 2, 214–222. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Report on Fall Prevention in Older Age. Available online: http://www.who.int/ageing/publications/Falls_prevention7March.pdf (accessed on 21 August 2017).
- Chaudhury, H.; Campo, M.; Michael, Y.; Mahmood, A. Neighbourhood environment and physical activity in older adults. Soc. Sci. Med. 2016, 149, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Haselwandter, E.M.; Corcoran, M.P.; Folta, S.C.; Hyatt, R.; Fenton, M.; Nelson, M.E. The built environment, physical activity, and aging in the United States: A state of the science review. J. Aging Phys. Act. 2015, 23, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Nicklett, E.J.; Lohman, M.C.; Smith, M.L. Neighborhood environment and falls among community-dwelling older adults. Int. J. Environ. Res. Public Health 2017, 14, 175. [Google Scholar] [CrossRef] [PubMed]
- Kenny, R.; Rubenstein, L.Z.; Tinetti, M.E.; Brewer, K.; Cameron, K.A.; Capezuti, L.; John, D.P.; Lamb, S.E.; Martin, F.; Rockey, P.H. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef]
- Kumar, A.; Carpenter, H.; Morris, R.; Iliffe, S.; Kendrick, D. Which factors are associated with fear of falling in community-dwelling older people? Age Ageing 2014, 43, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Chippendale, T.; Boltz, M. The neighborhood environment: Perceived fall risk, resources, and strategies for fall prevention. Gerontologist 2015, 55, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Ko, Y. Characteristics associated with fear of falling and activity restriction in South Korean older adults. J. Aging Health 2015, 27, 1066–1083. [Google Scholar] [CrossRef] [PubMed]
- Hong, I.; Simpson, A.N.; Logan, S.; Woo, H.S. Longitudinal trends in fall accidents in community dwelling Korean adults: The 2008–2013 Korean community health survey. Ann. Rehabil. Med. 2016, 40, 657–665. [Google Scholar] [CrossRef] [PubMed]
- The Korea Institute for Health and Social Affairs. 2014 A National Survey on the Living Status and Welfare Needs of the Aged; The Korea Institute for Health and Social Affairs: Seoul, Korea, 2015. [Google Scholar]
- Kim, T.H.; Jhoo, J.H.; Park, J.H.; Kim, J.L.; Ryu, S.H.; Moon, S.W.; Choo, I.H.; Lee, D.W.; Yoon, J.C.; Do, Y.J.; et al. Korean Version of Mini Mental Status Examination for Dementia Screening(MMSE-DS) and its short form. Psychiatry Investig. 2010, 7, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Jeon, G.S.; Cho, S.I. Prospective study on the impact of fear of falling on functional decline among community dwelling elderly women. Int. J. Environ. Res. Public Health 2017, 14, 469. [Google Scholar] [CrossRef] [PubMed]
- Won, C.W.; Yang, K.Y.; Rho, Y.G.; Kim, S.Y.; Lee, E.; Yoon, J.L.; Cho, K.H.; Shin, H.C.; Cho, B.R.; Oh, J.R.; et al. The development of Korean Activities of Daily Living(K-ADL) and Korean Instrumental Activities of Daily Living(K-IADL) Scale. Ann. Geriatr. Med. Res. 2002, 6, 107–120. [Google Scholar]
- Cho, M.J.; Bae, J.N.; Suh, G.H.; Hahm, B.J.; Kim, J.K.; Lee, D.W.; Kang, M.H. Validation of Geriatric Depression Scale (GDS), Korean version in the assessment of DSM-III-R major depression. J. Korean Neuropsychiatr. Assoc. 1999, 38, 48–63. [Google Scholar]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W. Lancet Physical Activity Series Working Group. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Hwang, K.H.; Kim, S.R. The centrality and core factors of the elderly’s social activities: With the reference of neighborhood facilities. Korean J. Local Govern. Stud. 2016, 20, 375–401. [Google Scholar] [CrossRef]
- Inoue, S.; Ohya, Y.; Odagiri, Y.; Takamiya, T.; Ishii, K.; Lee, J.S.; Shimomitsu, T. Reliability of the abbreviated neighborhood environment walkability scale Japanese version. Jpn. J. Phys. Fit. Sports Med. 2009, 58, 453–461. [Google Scholar] [CrossRef]
- Inoue, S.; Ohya, Y.; Odagiri, Y.; Takamiya, T.; Kamada, M.; Okada, S.; Oka, K.; Kitabatake, Y.; Nakaya, T.; Sallis, J.F.; et al. Perceived neighborhood environment and walking for specific purposes among ederly Japanese. J. Epidemiol. 2011, 21, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.C.; Kneebone, I.I.; Jones, F.; Brady, B. A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int. Psychogeriatr. 2015, 27, 1071–1087. [Google Scholar] [CrossRef] [PubMed]
- Hull, S.L.; Kneebone, I.I.; Farquharson, L. Anxiety, depression, and fall-related psychological concerns in community-dwelling older people. Am. J. Geriatr. Psychiatry 2013, 21, 1287–1291. [Google Scholar] [CrossRef] [PubMed]
- Hauer, K.; Lamb, S.E.; Jorstad, E.C.; Todd, C.; Becker, C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing 2006, 35, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Bhala, R.P.; Odonnell, J.; Thoppil, E. Ptophobia-phobic fear of falling and its clinical management. Phys. Ther. 1982, 62, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Isaacs, B. The post-fall syndrome: A study of 36 elderly patients. Gerontology 1982, 28, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, O.A.; Cronin, H.; Savva, G.M.; O’Regan, C.; Kenny, R.A. Effects of fear of falling and activity restriction on normal and dual task walking in community dwelling older adults. Gait Posture 2013, 38, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Christian, H.; Knuiman, M.; Bull, F.; Timperio, A.; Foster, S.; Divitini, M.; Middleton, N.; Giles-Corti, B. A new urban planning code’s impact on walking: The residential environments project. Am. J. Public Health 2013, 103, 1219–1228. [Google Scholar] [CrossRef] [PubMed]
- Jørstad, E.C.; Hauer, K.; Becker, C.; Lamb, S.E. Measuring the psychological outcomes of falling: A systematic review. J. Am. Geriatr. Soc. 2005, 53, 501–510. [Google Scholar] [CrossRef] [PubMed]
| Individual Variables | Classification | Total | With Fall History | Without Fall History | t or χ2 | |
|---|---|---|---|---|---|---|
| (n = 1804) | (n = 5926) | |||||
| n (%) or | n (%) or | |||||
| M ± SD | M ± SD | |||||
| Demographic characteristics | Age (years) | 65–74 | 4616 (59.7) | 961 (53.3) | 3655 (61.7) | 40.631 *** |
| ≥75 | 3114 (40.3) | 843 (46.7) | 2271 (38.3) | |||
| Sex | Male | 3154 (40.8) | 503 (27.9) | 2651 (44.7) | 162.616 *** | |
| Female | 4576 (59.2) | 1301 (72.4) | 3275 (55.3) | |||
| Marital status | Living with spouse | 4851 (62.8) | 943 (52.3) | 3908 (65.9) | 110.635 *** | |
| Living without spouse | 2879 (37.2) | 861 (47.7) | 2018 (34.1) | |||
| Educational level (years) | 0–6 | 5089 (65.8) | 1356 (75.2) | 3733 (63.0) | 91.107 *** | |
| ≥7 | 2641 (34.2) | 448 (24.8) | 2193 (37.0) | |||
| Public assistance | Yes | 520 (6.7) | 154 (8.5) | 366 (6.2) | 12.280 *** | |
| No | 7210 (93.3) | 1650 (91.5) | 5560 (93.8) | |||
| Current driving status | Yes | 1306 (16.9) | 158 (8.8) | 1148 (19.4) | 110.964 *** | |
| No | 6424 (83.1) | 1646 (91.2) | 4778 (80.6) | |||
| Health-related characteristics | Subjective health status | Poor | 5140 (66.5) | 1469 (81.4) | 3671 (61.9) | 235.623 *** |
| Good | 2590 (33.5) | 335 (18.6) | 2255 (38.1) | |||
| Limitation of ADLs | Yes | 291 (3.8) | 126 (7.0) | 165 (2.8) | 67.344 *** | |
| No | 7439 (96.2) | 1678 (93.0) | 5761 (97.2) | |||
| Limitation of IADLs | Yes | 988 (12.8) | 364 (20.2) | 624 (10.5) | 115.468 *** | |
| No | 6742 (87.2) | 1440 (79.8) | 5302 (89.5) | |||
| Trouble with vision | Yes | 3062 (39.6) | 861 (46.7) | 2201 (37.1) | 64.788 *** | |
| No | 4668 (60.4) | 943 (53.3) | 3725 (62.9) | |||
| Trouble with hearing | Yes | 1676 (21.7) | 494 (27.4) | 1182 (19.9) | 45.053 *** | |
| No | 6054 (78.3) | 1310 (72.6) | 4744 (80.1) | |||
| Hypertension | Yes | 4415 (57.1) | 1103 (61.1) | 3312 (55.9) | 15.578 *** | |
| No | 3315 (42.9) | 701 (38.9) | 2614 (44.1) | |||
| Diabetes mellitus | Yes | 1682 (21.8) | 441 (24.4) | 1241 (20.9) | 9.974 ** | |
| No | 6048 (78.2) | 1363 (75.6) | 4685 (79.1) | |||
| Arthritis | Yes | 2728 (35.3) | 856 (47.5) | 1872 (31.6) | 152.343 *** | |
| No | 5002 (64.7) | 948 (52.5) | 4054 (68.4) | |||
| Depression † | 6.61 ± 4.57 | 4.57 ± 4.25 | 17.578 *** | |||
| Environmental Variables | Classification | Total (N = 7730) | With Fall History | Without Fall History | |
|---|---|---|---|---|---|
| (n = 1804) | (n = 5926) | t or χ2 | |||
| n (%) or M ± SD | n (%) or M ± SD | ||||
| Residential area | Urban | 5296 (68.4) | 1203 (66.7) | 4093 (77.3) | 3.642 |
| Rural | 2434 (31.6) | 601 (33.3) | 1833 (22.7) | ||
| Housing type | Apartment | 2249 (29.1) | 522 (28.9) | 1727 (29.1) | 0.029 |
| House | 5481 (70.9) | 1282 (71.1) | 4199 (70.9) | ||
| Discomfort with the neighborhood environment † | 2.13 ± 0.87 | 1.96 ± 0.96 | 6.802 *** | ||
| Accessibility to neighborhood facilities † | 2.28 ± 1.53 | 2.35 ± 1.48 | −1.687 | ||
| Social support † | 2.10 ± 0.86 | 2.19 ± 0.84 | −4.040 *** | ||
| Level | Variables | With Fall History | Without Fall History |
|---|---|---|---|
| (Comparison Group) | OR (95% CI) | OR (95% CI) | |
| Individual | Age (≥75 years) | 1.680 (0.886–3.186) | 2.047 (1.738–2.412) *** |
| Sex (Female) | 5.100 (2.488–10.456) *** | 3.337 (2.810–3.962) *** | |
| Marital status | 0.538 (0.259–1.119) | 1.075 (0.898–1.288) | |
| Educational level (0–6 years) | 1.158 (0.612–2.194) | 1.221 (1.045–1.426) * | |
| Public assistance (Yes) | 2.124 (0.456–9.893) | 0.930 (0.648–1.336) | |
| Current driving status (Non-driver) | 1.557 (0.773–3.139) | 1.490 (1.250–1.775) *** | |
| Subjective health status (Poor) | 1.910 (1.000–3.646) | 1.651 (1.418–1.921) *** | |
| Limitation of ADLs (Yes) | 0.554 (0.098–3.122) | 1.029 (0.495–2.140) | |
| Limitation of IADLs (Yes) | 1.145 (0.299–4.380) | 1.347 (0.915–1.983) | |
| Trouble with vision (Yes) | 1.923 (0.971–3.809) | 1.409 (1.206–1.646) *** | |
| Trouble with hearing (Yes) | 1.433 (0.675–3.044) | 1.158 (0.953–1.406) | |
| Hypertension (Yes) | 1.292 (0.718–2.325) | 1.073 (0.931–1.236) | |
| Diabetes mellitus (Yes) | 1.075 (0.521–2.218) | 1.295 (1.074–1.562) ** | |
| Arthritis (Yes) | 1.772 (0.855–3.672) | 1.490 (1.240–1.790) *** | |
| Depression † | 1.081 (0.995–1.174) | 1.094 (1.070–1.118) *** | |
| Environmental | Residential area (Rural) | 1.230 (0.624–2.426) | 0.968 (0.819–1.143) |
| Housing type (House) | 1.173 (0.632–2.175) | 1.146 (0.979–1.341) | |
| Discomfort with neighborhood environment † | 1.387 (1.026–1.875) * | 1.305 (1.211–1.406) *** | |
| Accessibility to neighborhood facilities † | 0.839 (0.687–1.025) | 0.895 (0.852–0.941) *** | |
| Social support † | 0.995 (0.700–1.415) | 0.842 (0.772–0.919) *** |
| Level | Variables (Comparison Group) | Model I Adjusted OR (95% CI) | Model II Adjusted OR (95% CI) |
|---|---|---|---|
| Individual | Age × Fall history | 0.753 (0.398–1.426) | 0.742 (0.389–1.417) |
| Sex × Fall history | 1.205 (0.627–2.318) | 1.153 (0.595–2.233) | |
| Educational level × Fall history | 1.011 (0.550–1.856) | 0.952 (0.508–1.784) | |
| Current driving status × Fall history | 1.058 (0.536–2.089) | 1.014 (0.500–2.057) | |
| Subjective health status × Fall history | 1.138 (0.599–2.160) | 1.181 (0.618–2.255) | |
| Trouble with vision × Fall history | 1.339 (0.684–2.623) | 1.351 (0.686–2.663) | |
| Diabetes mellitus × Fall history | 0.888 (0.427–1.847) | 0.816 (0.391–1.701) | |
| Arthritis × Fall history | 1.192 (0.570–2.492) | 1.160 (0.550–2.445) | |
| Depression × Fall history | 0.980 (0.905–1.061) | 0.987 (0.909–1.072) | |
| Environmental | Discomfort with the neighborhood environment × Fall history | 1.051 (0.776–1.425) | |
| Accessibility to neighborhood facilities × Fall history | 0.933 (0.768–1.133) | ||
| Social support × Fall history | 1.191 (0.833–1.704) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Oh, E.; Hong, G.-R.S. Comparison of Factors Associated with Fear of Falling between Older Adults with and without a Fall History. Int. J. Environ. Res. Public Health 2018, 15, 982. https://doi.org/10.3390/ijerph15050982
Lee S, Oh E, Hong G-RS. Comparison of Factors Associated with Fear of Falling between Older Adults with and without a Fall History. International Journal of Environmental Research and Public Health. 2018; 15(5):982. https://doi.org/10.3390/ijerph15050982
Chicago/Turabian StyleLee, Seonhye, Eunmi Oh, and Gwi-Ryung Son Hong. 2018. "Comparison of Factors Associated with Fear of Falling between Older Adults with and without a Fall History" International Journal of Environmental Research and Public Health 15, no. 5: 982. https://doi.org/10.3390/ijerph15050982
APA StyleLee, S., Oh, E., & Hong, G.-R. S. (2018). Comparison of Factors Associated with Fear of Falling between Older Adults with and without a Fall History. International Journal of Environmental Research and Public Health, 15(5), 982. https://doi.org/10.3390/ijerph15050982





