Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives
Abstract
:1. Introduction
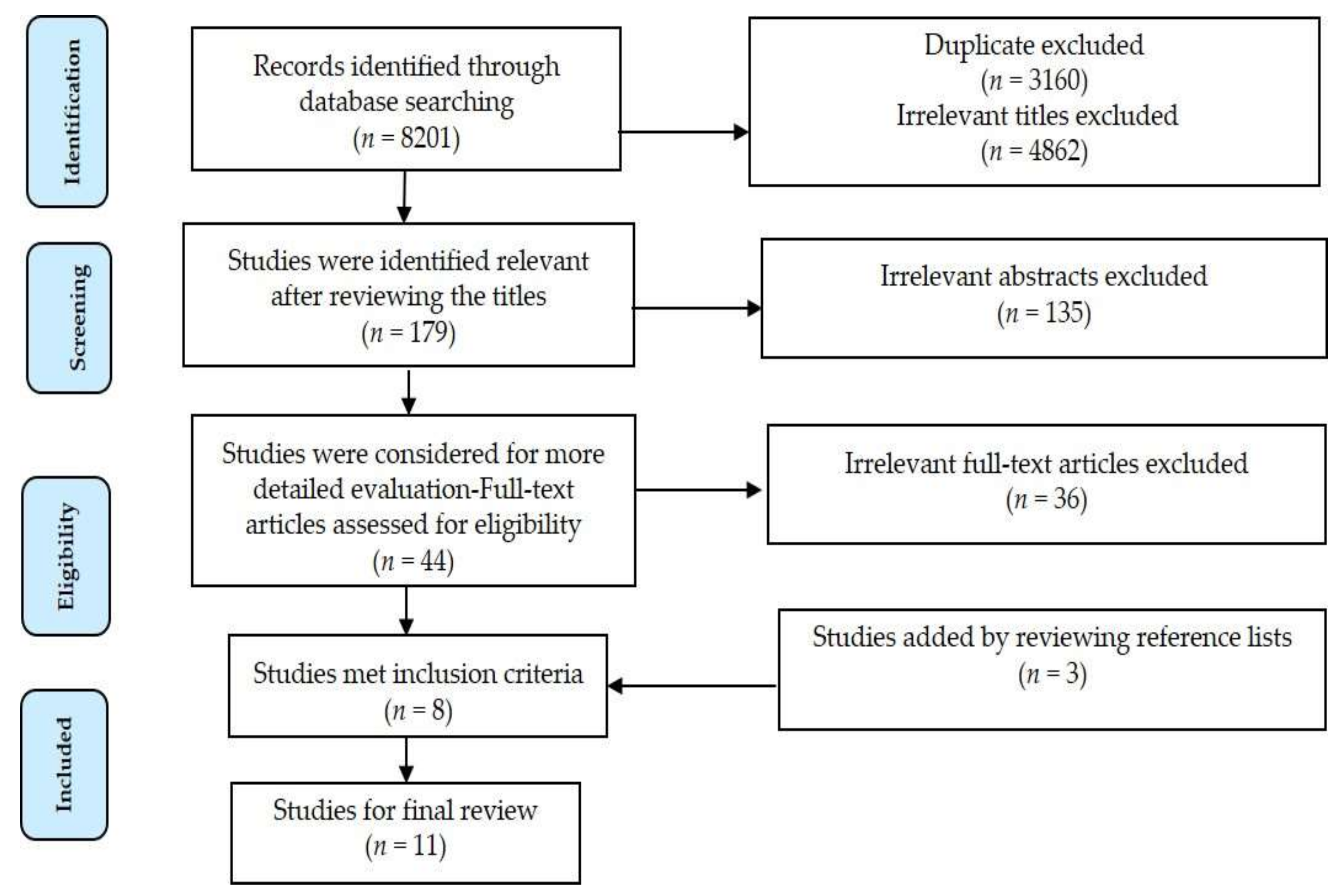
2. Materials and Methods
3. Data Sources
4. Inclusion Criteria
5. Data Collection and Analysis
6. Results
6.1. Statistical Methods
6.2. Temperature and GI Infections
6.3. Variability of Causes of Gastrointestinal Infections
7. Discussion
8. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Database Name | Search Strategy |
|---|---|
| Embase | |
| Final S | “gastrointestinal infection” OR “diarrhea”/exp OR diarrhea OR “diarrhea”/exp OR diarrhoea OR “diarrhea/exp” AND (“temperature”/exp OR temperature OR “climate”/exp OR climate OR “weather”/exp OR weather OR “heatwave”) |
| Web of Science | |
| Final S | ((“gastrointestinal infection” OR diarrhea OR diarrhoea) AND (climate change OR temperature OR climate OR weather OR “heat wave”)) |
| Scopus | |
| Final S | (TITLE-ABS-KEY (“gastrointestinal infection” OR diarrhea OR diarrhoea) AND TITLE-ABS-KEY (temperature OR climate OR weather OR “heat wave” OR “climate change”)) |
| Medline | |
| Final S | (“gastrointestinal infection” OR diarrhea OR diarrhoea) AND (temperature OR climate OR weather) |
References
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The challenge of emerging and re-emerging infectious diseases. Nature 2004, 430, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Fleurat, M. Pediatric Emergency Medicine Practice Acute Gastroenteritis—An Update. Pediatr. Emerg. Med. Pract. 2010, 7, 1–12. [Google Scholar]
- Onozuka, D.; Hashizume, M.; Hagihara, A. Effects of weather variability on infectious gastroenteritis. Epidemiol. Infect. 2010, 138, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Sun, M.; Fitzgerald, E.; Hwang, S.A. Did summer weather factors affect gastrointestinal infection hospitalizations in New York State? Sci. Total Environ. 2016, 550, 38–44. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Diarrhoeal Disease. Available online: http://data.unicef.org/child-health/diarrhoeal-disease.html (accessed on 2 March 2018).
- Harley, D.; Bi, P.; Hall, G.; Swaminathan, A.; Tong, S.; Williams, C. Climate Change and Infectious Diseases in Australia: Future Prospects, Adaptation Options, and Research Priorities. Asia Pac. J. Public Health 2011, 23, 54S–66S. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, R.M.; Becker, N.G.; Hall, G.; Moodie, K.B. Does ambient temperature affect foodborne disease? Epidemiology 2004, 15, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Akil, L.; Ahmad, H.A.; Reddy, R.S. Effects of Climate Change on Salmonella Infections. Foodborne Pathog. Dis. 2014, 11, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Sheffield, P.E.; Hu, W.; Su, H.; Yu, W.; Qi, X.; Tong, S. Climate change and children’s health—A call for research on what works to protect children. Int. J. Environ. Res. Public Health 2012, 9, 3298–3316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manser, C.N.; Paul, M.; Rogler, G.; Held, L.; Frei, T. Heat waves, incidence of infectious gastroenteritis, and relapse rates of inflammatory bowel disease: A retrospective controlled observational study. Am. J. Gastroenterol. 2013, 108, 1480–1485. [Google Scholar] [CrossRef] [PubMed]
- Checkley, W.; Epstein, L.D.; Gilman, R.H.; Figueroa, D.; Cama, R.I.; Patz, J.A.; Black, R.E. Effects of EI Niño and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet 2000, 355, 442–450. [Google Scholar] [CrossRef]
- Xu, Z.; Etzel, R.A.; Su, H.; Huang, C.; Guo, Y.; Tong, S. Impact of ambient temperature on children’s health: A systematic review. Environ. Res. 2012, 117, 120–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eze, J.I.; Scott, E.M.; Pollock, K.G.; Stidson, R.; Miller, C.A.; Lee, D. The association of weather and bathing water quality on the incidence of gastrointestinal illness in the west of Scotland. Epidemiol. Infec. 2014, 142, 1289–1299. [Google Scholar] [CrossRef] [PubMed]
- Hall, G.; Hanigan, I.; Dear, K.; Vally, H. The influence of weather on community gastroenteritis in Australia. Epidemiol. Infect. 2011, 139, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.T. The association between climatic factors and childhood illnesses presented to hospital emergency among young children. Int. J. Environ. Health Res. 2007, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- McIver, L.; Hashizume, M.; Kim, H.; Honda, Y.; Pretrick, M.; Iddings, S.; Pavlin, B. Assessment of climate-sensitive infectious diseases in the Federated States of Micronesia. Trop. Med. Health 2015, 43, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Onozuka, D.; Hashizume, M. Weather variability and paediatric infectious gastroenteritis. Epidemiol. Infect. 2011, 139, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Phung, D.; Rutherford, S.; Chu, C.; Wang, X.; Nguyen, M.; Nguyen, N.H.; Huang, C. Temperature as a risk factor for hospitalisations among young children in the Mekong Delta Area, Vietnam. Occup. Environ. Med. 2015, 72, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Zhou, Y.; Chen, R.; Ma, W.; Deng, H.; Kan, H. High temperature as a risk factor for infectious diarrhea in Shanghai, China. J. Epidemiol. 2013, 23, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Ma, X.; Gan, L.; Wei, Y.; Sun, P.; Zhang, D. Research on the application of medical-meteorological forecast model of infectious diarrhea disease in Beijing. In Proceedings of the 2010 IEEE 5th International Conference on Bio-Inspired Computing: Theories and Applications (BIC-TA), Liverpool, UK, 23–26 September 2010; pp. 100–103. [Google Scholar]
- Mancer, C.N.; Kraus, A.; Frei, T.; Rogler, G.; Held, L. The impact of cold spells on the incidence of infectious gastrenterities and relapse rates of inflammatory bowel disease: A retropsective controlled observational study. Inflamm. Intest. Dis. 2017, 2, 124–130. [Google Scholar] [CrossRef]
- McMichael, A.J. Globalization, climate change, and human health. N. Engl. J. Med. 2013, 368, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Intergovernmental Panel on Climate Change. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Stocker, T.F., Qin, D., Plattner, G.-K., Tignor, M., Allen, S.K., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2013. [Google Scholar]
- McMichael, A.J.; Woodruff, R.E.; Hales, S. Climate change and human health: Present and future risks. Lancet 2006, 367, 859–869. [Google Scholar] [CrossRef]
- Kendrovski, V.; Gjorgjev, D. Climate Change: Implication for Food-Borne Diseases (Salmonella and Food Poisoning Among Humans in R. Macedonia); INTECH Open Access Publisher: London, UK, 2012. [Google Scholar]
- Carlton, E.J.; Woster, A.P.; DeWitt, P.; Goldstein, R.S.; Levy, K. A systematic review and meta-analysis of ambient temperature and diarrhoeal diseases. Int. J. Epidemiol. 2016, 45, 117–130. [Google Scholar] [CrossRef] [PubMed]
- Jofre, J.; Blanch, A.R.; Lucena, F. Water-borne infectious disease outbreaks associated with water scarcity and rainfall events. In Water Scarcity in the Mediterranean; Springer: Berlin, Germany, 2009; pp. 147–159. [Google Scholar]
- Levy, K.; Hubbard, A.E.; Eisenberg, J.N. Seasonality of rotavirus disease in the tropics: A systematic review and meta-analysis. Int. J. Epidemiol. 2009, 38, 1487–1496. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.M.; Pitzer, V.E.; Alonso, W.J.; Vera, D.; Lopman, B.; Tate, J.; Parashar, U.D. Global seasonality of rotavirus disease. Pediatr. Infect. Dis. J. 2013, 32, e134–e147. [Google Scholar] [CrossRef] [PubMed]
- Toloo, G.S.; Guo, Y.; Turner, L.; Qi, X.; Aitken, P.; Tong, S. Socio-demographic vulnerability to heatwave impacts in Brisbane, Australia: A time series analysis. Aust. N. Z. J. Public Health 2014, 38, 430–435. [Google Scholar] [CrossRef] [PubMed]
| Study | Location and Time | Unit of Data | Spatial Scale | Weather Variables | Research Design and Statistical Analysis | Outcome(s) | Key Finding(s) |
|---|---|---|---|---|---|---|---|
| [14] | West of Scotland 1998–2008 | Monthly | 2 Scottish National Health Service (NHS) board areas (Same coastal line) | Temperature Humidity | Time-series; Generalized additive models (GAM) | Incidence of GI illness | Rising temperature increases incidence of non-viral GI infections with peak in July. Decreasing temperature increases incidence of viral GI infections with peak in May. Rising humidity increases incidence of non-viral GI infections with peak in July. Decreasing humidity increases incidence of viral GI infections with peak in May. |
| [15] | Australia, 2001–2002 (Observation period) | Daily (Random selection) | Country | Temperature Rainfall Humidity | Time-series; Distributed Lag Model (DLM) | Community-acquired GI infections are substantially affected by weather. | Every 1 °C increase of temperature is associated with increase from the baseline (2.48%) of GI infections. Rainfall and humidity significantly correlated to GI infections. |
| [16] | Western region of Sydney, Australia, 2001–2002 | Daily | City | Temperature Humidity Rainfall | Time-series; Autoregressive Integrated Moving Average (ARIMA) | Emergency department visits due to GI infections (children less than 6 years) | Every 1 °C increase in maximum temperature was associated with an 11% increase in the number of emergency department visits secondary to GI infections. Relative humidity and rainfall were not significantly associated with emergency department visits for GI infections |
| [4] | New York state, USA, 1991–2004 | Daily | State level | Temperature Humidity Rainfall | Time-series; Generalized Additives Models (GAM) with a Poisson distribution and log link function | Hospitalization due to GI infection (long-term trend, seasonality, and calendar effects) | Every 1 °C increase in temperature is correlated to a 0.70–0.96% increase in daily hospitalization for GI infections, particularly bacterial infections, with lags from 1 to 4 days. Rainfall was significantly associated with hospitalization of GI infections, especially bacterial infections in a same lag period. |
| [10] | Zurich, Switzerland, 2001–2005 | Daily | University Hospital of Zurich | Temperature | Retrospective controlled observational, Poisson regression | The effect of heat waves on incidence of infectious gastroenteritis | Hospitalizations due to GI infections increased during heat waves |
| [17] | The Federated States of Micronesia, Asia Pacific Region, 2000–2010 | Daily | Country | Temperature Rainfall El Niño | Time-series; Generalized linear Poisson models | Relationship between weather variables and infectious diarrheal disease | Significant association were identified. |
| [3] | Fukuoka, Japan, 1999–2007 | Weekly | City | Temperature | Time-series; Generalized linear Poisson models | Impacts of weather variability on GI infections | Every 1 °C increase in the average temperature was correlated to 7.7% increase in the weekly number of GI infections. Every 1% decrease in relative humidity was correlated to a 2.3% increase in the weekly number of GI infections. |
| [18] | Fukuoka, Japan, 2000–2008 | Weekly | City | Temperature Humidity | Time-series; Generalized linear Poisson models | Hospital admission secondary to GI infections | Every 1 °C increase in temperature below 13 °C was correlated to a 23.2% increase in childhood GI infections among children under 15 years of age, while every 1 °C increase in temperature above 13 °C was correlated to an 11.8% decrease in childhood GI infections. Every 1% decrease of relative humidity was associated with 3.9% increase of childhood GI infections. |
| [19] | Mekong Delta, Vietnam, 2008–2011 | Daily | City | Temperature Rainfall Humidity | Time-series; Poisson regression and constrained distributed lag model (DLM) | Hospitalization due to GI infections among young children | Incidence of hospitalization among 0–5-year-old children increases with rising temperature above 24 °C During the wet season with mean rainfall of 3.8 mm and mean humidity of 82%, hospital admissions increased |
| [21] | Beijing, China, 2004–2006 | Daily | City | Temperature Humidity Water vapor pressure RainfallWind speed See level pressure | Epidemic risk level evaluation, Classical regression technique | Association between infectious diarrhea disease and meteorological factors | High association between infectious diarrhea disease and meteorological factors |
| [20] | Shanghai, China 2008–2010 | Daily | City | Temperature Humidity Rainfall | Time-series; quasi-Poisson regression model | High temperature as a risk factor for infectious diarrhea disease in outpatients | High temperature is correlated to increased risk of GI infections among outpatients. Study did not find any correlation between increased risk of GI infections and rainfall. However, it found that humidity is associated to increased risk of GI infections among outpatients |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghazani, M.; FitzGerald, G.; Hu, W.; Toloo, G.; Xu, Z. Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives. Int. J. Environ. Res. Public Health 2018, 15, 766. https://doi.org/10.3390/ijerph15040766
Ghazani M, FitzGerald G, Hu W, Toloo G, Xu Z. Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives. International Journal of Environmental Research and Public Health. 2018; 15(4):766. https://doi.org/10.3390/ijerph15040766
Chicago/Turabian StyleGhazani, Maryam, Gerard FitzGerald, Wenbiao Hu, Ghasem (Sam) Toloo, and Zhiwei Xu. 2018. "Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives" International Journal of Environmental Research and Public Health 15, no. 4: 766. https://doi.org/10.3390/ijerph15040766
APA StyleGhazani, M., FitzGerald, G., Hu, W., Toloo, G., & Xu, Z. (2018). Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives. International Journal of Environmental Research and Public Health, 15(4), 766. https://doi.org/10.3390/ijerph15040766






