Beliefs about Vaccinations: Comparing a Sample from a Medical School to That from the General Population
Abstract
:1. Introduction
- To what extent do people agree with supporting (pro) and opposing (anti) statements regarding vaccinations?
- Do people categorize these statements as facts or beliefs? Rabinowitz and colleagues [8] argued that categorizing a statement as a fact, as opposed to a belief, is related to people’s views of social norms; people tend to categorize statements as facts when they think that most people would agree with it. Therefore, the categorization question goes beyond just whether people agree with a statement or not.
- Do people agree as to what is a fact and what is a belief?
- Are people accurate in predicting what the general adult population would believe?
- Do the answers to the above four questions vary between medical affiliates (i.e., a population more versed in domain-specific knowledge) and the general population?
2. Method
Materials and Procedure
3. Results
3.1. Participants
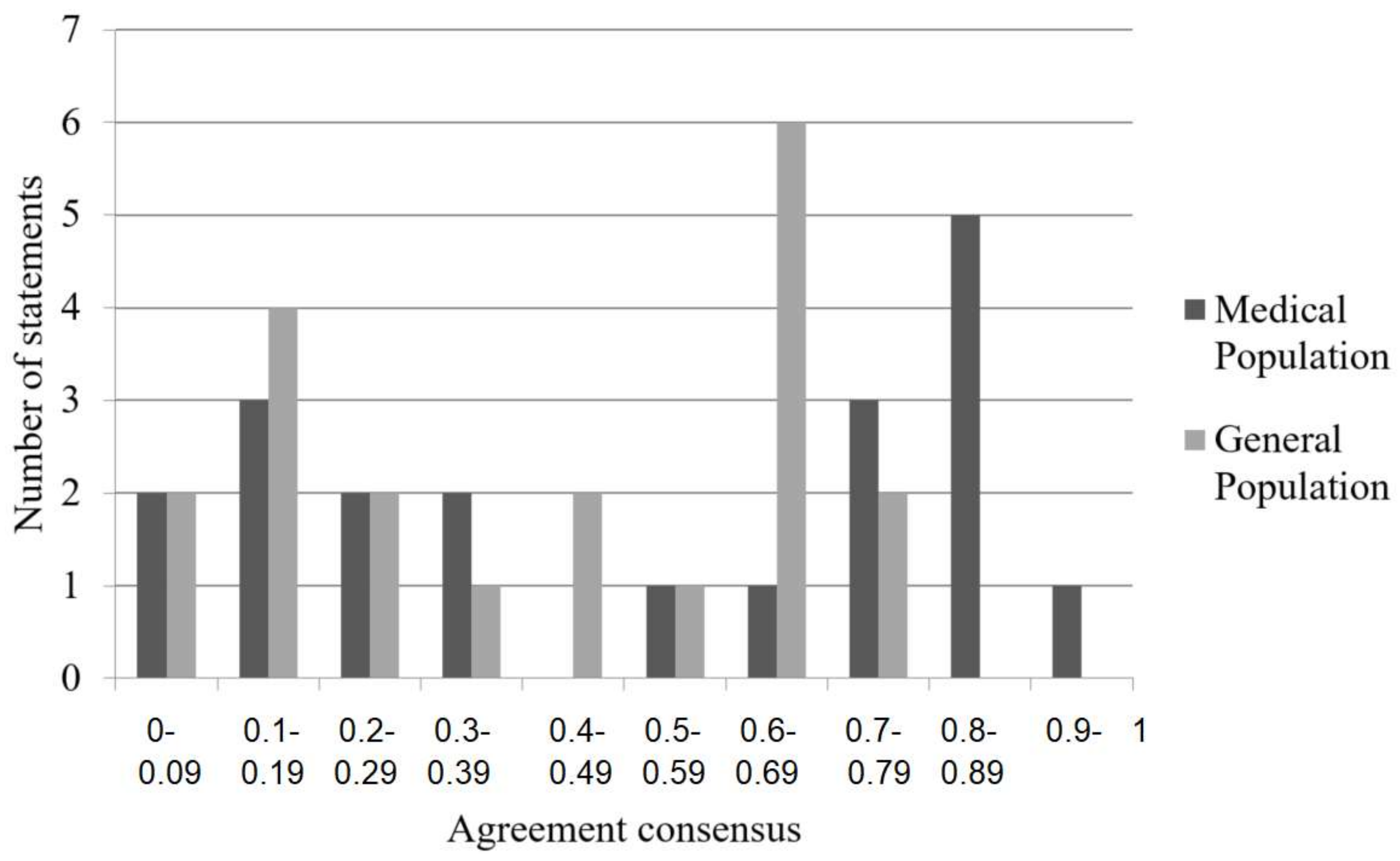
3.2. Agreement for the Vaccination Statements
3.3. Categorization of Facts and Beliefs
3.4. Do People Agree as to What Is a Fact and What Is a Belief?
3.5. Accuracy of Predictions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
Appendix A
- A hammer is primarily used to pound nails.
- Children are happy and carefree.
- Dogs are animals.
- A pen is for writing.
- The telephone is the greatest invention of all time.
- There are three colors in the American flag.
- There are seven days in a week.
- Christmas is a holiday primarily for children.
- Sleeping with the window open is good for you.
- Thermometers are used to record temperature.
- A driver’s license is required for driving a car.
- Books may be borrowed from the library.
- Rich people are happy people.
- Cats are friendly animals.
- Rock music has a bad influence on young people.
- It is okay to lie.
- The longer you stay in school the smarter you will be.
- The earth revolves around the sun.
- Comic strips are funny.
- The shape of a ball is round.
Appendix B
- Eighty to 90% of a population needs to be vaccinated in order for an entire community to be fully protected against a disease.
- Delaying or refusing vaccinations leaves children unprotected against many dangerous diseases.
- Vaccinations against dangerous diseases have saved more lives than drugs in the late 20th century, such as the development and use of antibiotics.
- The amount of ingredients used to create vaccinations is safe.
- It is very rare to have an adverse reaction to a vaccine.
- Mothers who are vaccinated protect their unborn children from viruses that can cause birth defects, such as mental disabilities, heart problems, and hearing and vision loss.
- Vaccinations are necessary for eliminating vaccine-preventable diseases.
- Vaccinations mobilize antibodies and proteins that are mimicked in the body’s natural immune defenses.
- The creation of vaccinations consists of a long process in order to determine whether or not it is safe and effective for public use.
- There is no direct link between vaccinations and Autism Spectrum Disorder or other mental disabilities.
- The increased number of vaccinations prior to a child’s second birthday is the reason why there has been an increase in Autism Spectrum Disorder in children.
- Vaccinations expose children to mercury through the use of thimerosal, which is a reason for the rise in Autism Spectrum Disorder.
- Vaccinations can have serious side effects that cause more harm than some of the diseases that they are supposed to prevent.
- Vaccines introduce toxic chemicals to the body that are not found in the natural immune defenses.
- Even if people are vaccinated, there is still a risk of contracting the disease that the vaccination was intended to protect against.
- Vaccinating a child before his/her immune system is fully developed can cause harm to that child.
- An increase in hygiene and improved living conditions are the reasons why the prevalence of diseases has declined; it is not a result of an increase in vaccinations.
- The use of aluminum in vaccinations is a risk for Alzheimer’s disease, dementia, and seizures.
- Vaccinations do not lead to life-long immunity, whereas contracting a disease, such as chicken pox does result in life-long immunity due to the body’s natural defense mechanisms.
- Due to political ties and economic incentives, pharmaceutical companies are not trustworthy sources to regulate the safety of vaccinations.
References
- McKee, C.; Bohannon, K. Exploring the reasons behind parental refusal of vaccines. J. Pediatr. Pharmacol. Ther. 2016, 21, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Elam-Evans, L.D.; Yankey, D.; Singleton, J.A.; Kolasa, M. National, state, and selected local area vaccination coverage among children aged 19–35 months—United States, 2013. Morb. Mortal. Wkly. Rep. 2014, 63, 741–748. [Google Scholar]
- Glanz, J.M.; Newcomer, S.R.; Narwaney, K.J.; Hambidge, S.J.; Daley, M.F.; Wagner, N.M.; McClure, D.L.; Xu, S.; Rowhani-Rahbar, A.; Lee, G.M.; et al. A population-based cohort study of undervaccination in 8 managed care organizations across the United States. JAMA Pediatr. 2013, 167, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Hinman, A. Eradication of vaccine-preventable diseases. Annu. Rev. Public Health 1999, 20, 211–229. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, A.M.; Brown, C.J.; Gust, D.A. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005, 120, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Sachse, K. Dr. Jekyll or Mr. Hyde? (How) the internet influences vaccination decisions: Recent evidence and tentative guidelines for online vaccine communication. Vaccine 2012, 30, 3723–3726. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.A.; Weinstein, N.D.; Colditz, G.A.; Emmons, K. Explanations for side effect aversion in preventive medical treatment decisions. Health Psychol. 2009, 28, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, M.; Latella, L.; Stern, C.; Jost, J.T. Beliefs about childhood vaccination in the United States: Political ideology, false consensus, and the illusion of uniqueness. PLoS ONE 2016, 11, e0158382. [Google Scholar] [CrossRef] [PubMed]
- Opel, D.J.; Heritage, J.; Taylor, J.A.; Mangione-Smith, R.; Sala, H.S.; DeVere, V.; Zhou, C.; Robinson, J.D. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics 2013, 132, 1037–1046. [Google Scholar] [CrossRef] [PubMed]
- Henrikson, N.B.; Opel, D.J.; Grothaus, L.; Nelson, J.; Scrol, A.; Dunn, J.; Faubion, T.; Roberts, M.; Marcuse, E.K.; Grossman, D.C. Physician communication training and parental vaccine hesitancy: A randomized trial. Pediatrics 2015, 36, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Leask, J.; Kinnersley, P. Physician communication with vaccine-hestiant parents: The start, not the end, of the story. Pediatrics 2015, 136, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Gore, P.; Madhavan, S.; Curry, D.; McClung, G.; Castiglia, M.; Rosenbluth, S.A.; Smego, R.A. Predictors of childhood immunization completion in a rural population. Soc. Sci. Med. 1999, 48, 1011–1027. [Google Scholar] [CrossRef]
- Sturm, L.A.; Mays, R.M.; Zimet, G.D. Parental beliefs and decision making about child and adolescent immunization: From polio to sexually transmitted infections. J. Dev. Behav. Pediatr. 2002, 26, 441–452. [Google Scholar] [CrossRef]
- Opel, D.J.; Mangione-Smith, R.; Robinson, J.D.; Heritage, J.; DeVere, V.; Salas, H.S.; Zhous, C.; Taylor, J.A. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. Am. J. Public Health 2015, 105, 1998–2004. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.; Jadad, A.R.; Ross, C.; Wilson, K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J. Clin. Epidemiol. 2005, 58, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Berkhof, M.; van Rijssen, H.J.; Schellart, A.J.; Anema, J.R.; van der Beek, A.J. Effective training strategies for teaching communication skills to physicians: An overview of systematic reviews. Patient Educ. Couns. 2011, 84, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Zolnierek, K.B.H.; DiMatteo, M.R. Physician communication and patient adherence to treatment: A meta-analysis. Med. Care 2009, 47, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Levinson, W.; Lesser, C.S.; Epstein, R.M. Developing physician communication skills for patient-centered care. Health Aff. 2010, 29, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Grice, H.P. Logic and conversation. In Syntax and Semantics: Speech Acts; Cole, P., Morgan, J.L., Eds.; Academic Press: New York, NY, USA, 1975; Volume 3, pp. 41–58. [Google Scholar]
- Clark, H.H.; Brennan, S.E. Grounding in communication. In Perspectives on Socially Shared Cognition; Resnick, L.B., Levine, J.M., Teasley, S.D., Eds.; American Psychological Association: Washington, DC, USA, 1991; pp. 127–149. [Google Scholar]
- Clark, H.H.; Haviland, S.E. Comprehension and the given-new contract. In Discourse Production and Comprehension: Advances in Research and Theory; Freedle, R.O., Ed.; Ablex Publishing Corporation: New York, NY, USA, 1977; Volume 1, pp. 1–40. [Google Scholar]
- Nückles, M.; Bromme, R. Internet experts’ planning of explanations for laypersons: A web experimental approach in the internet domain. Exp. Psychol. 2002, 49, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Hinds, P.J. The curse of expertise: The effects of expertise and debiasing methods on predictions of novice performance. J. Exp. Psychol. Appl. 1999, 5, 205–221. [Google Scholar] [CrossRef]
- Nathan, M.J.; Koedinger, K.R. An investigation of teachers’ beliefs of students’ algebra development. Cogn. Instr. 2000, 18, 209–237. [Google Scholar] [CrossRef]
- Nückles, M.; Wittwer, J.; Renkl, A. Information about a layperson’s knowledge supports experts in giving effective and efficient online advice to laypersons. J. Exp. Psychol. Appl. 2005, 11, 219–236. [Google Scholar] [CrossRef] [PubMed]
- Nickerson, R.S.; Baddeley, A.; Freeman, B. Are people’s estimates of what other people know influenced by what they themselves know? Acta Psychol. 1987, 64, 245–259. [Google Scholar] [CrossRef]
- Fussell, S.R.; Krauss, R.M. Accuracy and bias in estimates of others’ knowledge. Eur. J. Soc. Psychol. 1991, 21, 445–454. [Google Scholar] [CrossRef]
- Fussell, S.R.; Krauss, R.M. Coordination of knowledge in communication: Effects of speakers’ assumptions about what others know. J. Pers. Soc. Psychol. 1992, 62, 378–391. [Google Scholar] [CrossRef] [PubMed]
- Bromme, R.; Rambow, R.; Nückles, M. Expertise and estimating what other people know: The influence of professional experience and type of knowledge. J. Exp. Psychol. Appl. 2001, 7, 317–330. [Google Scholar] [CrossRef] [PubMed]
- Wittwer, J.; Nückles, M.; Renkl, A. Is underestimation less detrimental than overestimation? The impact of experts’ beliefs about a layperson’s knowledge on learning and question asking. Instr. Sci. 2008, 38, 27–52. [Google Scholar] [CrossRef]
- Benin, A.L.; Wisler-Scher, D.J.; Colson, E.; Shapiro, E.D.; Holmboe, E.S. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics 2006, 117, 1532–1541. [Google Scholar] [CrossRef] [PubMed]
- Connors, J.T.; Slotwinski, K.L.; Hodges, E.A. Provider-parent communication when discussing vaccines: A Systematic Review. J. Pediatr. Nurs. 2017, 33, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, D.D.; Davis, T.C.; Arnold, C.L.; Kennen, E.M.; Humiston, S.G.; Cross, J.T.; Bocchini, J.A. Childhood immunization refusal: Provider and parent perceptions. Fam. Med. 2004, 36, 431–439. [Google Scholar] [PubMed]
- Krueger, J.; Clement, R.W. The truly false consensus effect: An ineradicable and egocentric bias in social perception. J. Pers. Soc. Psychol. 1994, 68, 579–610. [Google Scholar] [CrossRef]
- Ross, L.; Greene, D.; House, P. The “false consensus effect”: An egocentric bias in social perception and attribution processes. J. Exp. Soc. Psychol. 1997, 13, 279–301. [Google Scholar] [CrossRef]
- Stern, C.; West, T.V.; Schmitt, P.G. The liberal illusion of uniqueness. Psychol. Sci. 2014, 25, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, M.; Acevedo, M.; Casen, S.; Rosengarten, M.; Kowalczyk, M.; Portnoy, L. Distinguishing facts from beliefs: Fuzzy categories. Psychol. Lang. Commun. 2013, 17, 241–267. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Talking with Parents about Vaccines for Infants: Strategies for Health Care Professionals. Available online: https://www.cdc.gov/vaccines/hcp/conversations/downloads/talk-infants-color-office.pdf (accessed on 5 March 2018).
- Marks, G. Thinking one’s abilities are unique and one’s opinions are common. Pers. Soc. Psychol. Bull. 1984, 10, 203–208. [Google Scholar] [CrossRef]
- Stehr, N.; Ericson, R. (Eds.) The Culture and Power of Knowledge: Inquiries into Contemporary Societies; Walter de Gruyter: Berlin, Germany, 1992; pp. 3–19. [Google Scholar]
- Mawson, A.R.; Ray, B.D.; Bhuiyan, A.R.; Jacob, B. Pilot comparative study on the health of vaccinated and unvaccinated 6 to 12 year old U.S. children. J. Transl. Sci. 2017, 3, 1–12. [Google Scholar] [CrossRef]
- Bovier, P.A.; Chamot, E.; Gallacchi, M.; Loutan, L. Importance of patients’ perceptions and general practitioners’ recommendations in understanding missed opportunities for immunizations in Swiss adults. Vaccine 2001, 19, 4760–4767. [Google Scholar] [CrossRef]
- Gellin, B.G.; Maibach, E.W.; Marcuse, E.K. Do parents understand immunizations? A national telephone survey. Pediatrics 2000, 106, 1097–1102. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Medical Population n = 58 | % | General Population n = 177 | % |
|---|---|---|---|---|
| Gender | ||||
| Male | 28 | 48.30 | 55 | 31.10 |
| Female | 30 | 51.70 | 122 | 68.90 |
| Ethnicity | ||||
| Caucasian | 48 | 82.8 | 125 | 76.3 |
| Asian/Pacific Islander | 7 | 12.1 | 15 | 9.5 |
| African American | 1 | 1.7 | 13 | 7.3 |
| Hispanic | 1 | 1.7 | 9 | 5.1 |
| Other | 1 | 1.7 | 11 | 2.8 |
| Medical Level | ||||
| Professor | 15 | 25.9 | - | - |
| Student | 43 | 74.1 | - | - |
| Education Level | ||||
| High School Diploma | 0 | 0 | 62 | 35 |
| BA/BS | 0 | 0 | 77 | 43.5 |
| Master’s degree | 0 | 0 | 27 | 15.3 |
| Other | 58 | 100 | 11 | 6.2 |
| Supporting Statements | Medical Population (M) | General Population (M) |
| Eighty to 90% of a population needs to be vaccinated in order for an entire community to be fully protected against a disease. | 0.78 | 0.45 |
| Delaying or refusing vaccinations leaves children unprotected against many dangerous diseases. | 0.83 | 0.70 |
| Vaccinations against dangerous disease have saved more lives than drugs, such as antibiotics in the late 20th century. | 0.69 | 0.62 |
| The amount of ingredients used to create vaccinations is safe. | 0.26 | 0.29 |
| It is very rare to have an adverse reaction to a vaccine. | 0.85 | 0.72 |
| Mothers who are vaccinated protect their unborn children from viruses that can cause birth defects, such as mental disabilities, heart problems, and hearing and vision loss. | 0.26 | 0.19 |
| Vaccinations are necessary for eliminating vaccine-preventable diseases. | 0.77 | 0.62 |
| Vaccinations mobilize antibodies and proteins that are mimicked in the body’s natural immune defenses. | 0.91 | 0.70 |
| There is no direct link between vaccinations and autism spectrum disorder or other mental disabilities. | 0.79 | 0.61 |
| Vaccinations go through a long process in order to determine whether or not it is safe and effective for public use. | 0.86 | 0.74 |
| Opposing Statements | Medical Population (M) | General Population (M) |
| The increased number of vaccinations prior to a child’s second birthday is the reason why there has been an increase in autism spectrum disorder in children. | 0.05 | 0.05 |
| Vaccinating a child before his/her immune system is fully developed can cause harm to that child. | 0.85 | 0.53 |
| Vaccinations can have serious side effects that cause more harm than some of the diseases that they are supposed to prevent. | 0.35 | 0.28 |
| Vaccines introduce toxic chemicals that are not found in the natural immune defenses. | 0.57 | 0.39 |
| Even if people are vaccinated, there is still a risk of contracting the disease that the vaccination was intended to protect against. | 0.83 | 0.63 |
| Vaccinations do not lead to life-long immunity, whereas contracting a disease, such as chicken pox does result in life-long immunity due to the body’s natural defense mechanisms. | 0.35 | 0.40 |
| An increase in hygiene and improved living conditions are the reasons why the prevalence of diseases have declined, rather than an increase in vaccinations | 0.10 | 0.15 |
| The use of aluminum in vaccinations is a risk for Alzheimer’s disease, dementia, and seizures. | 0.16 | 0.20 |
| Due to political ties and economic incentives, pharmaceutical companies are not trustworthy. | 0.16 | 0.19 |
| Vaccinations expose children to mercury through the use of thimerosal which is a reason for the rise in autism spectrum disorder. | 0.05 | 0.09 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Latella, L.E.; McAuley, R.J.; Rabinowitz, M. Beliefs about Vaccinations: Comparing a Sample from a Medical School to That from the General Population. Int. J. Environ. Res. Public Health 2018, 15, 620. https://doi.org/10.3390/ijerph15040620
Latella LE, McAuley RJ, Rabinowitz M. Beliefs about Vaccinations: Comparing a Sample from a Medical School to That from the General Population. International Journal of Environmental Research and Public Health. 2018; 15(4):620. https://doi.org/10.3390/ijerph15040620
Chicago/Turabian StyleLatella, Lauren E., Robert J. McAuley, and Mitchell Rabinowitz. 2018. "Beliefs about Vaccinations: Comparing a Sample from a Medical School to That from the General Population" International Journal of Environmental Research and Public Health 15, no. 4: 620. https://doi.org/10.3390/ijerph15040620
APA StyleLatella, L. E., McAuley, R. J., & Rabinowitz, M. (2018). Beliefs about Vaccinations: Comparing a Sample from a Medical School to That from the General Population. International Journal of Environmental Research and Public Health, 15(4), 620. https://doi.org/10.3390/ijerph15040620




