Medical Efforts and Injury Patterns of Military Hospital Patients Following the 2013 Lushan Earthquake in China: A Retrospective Study
Abstract
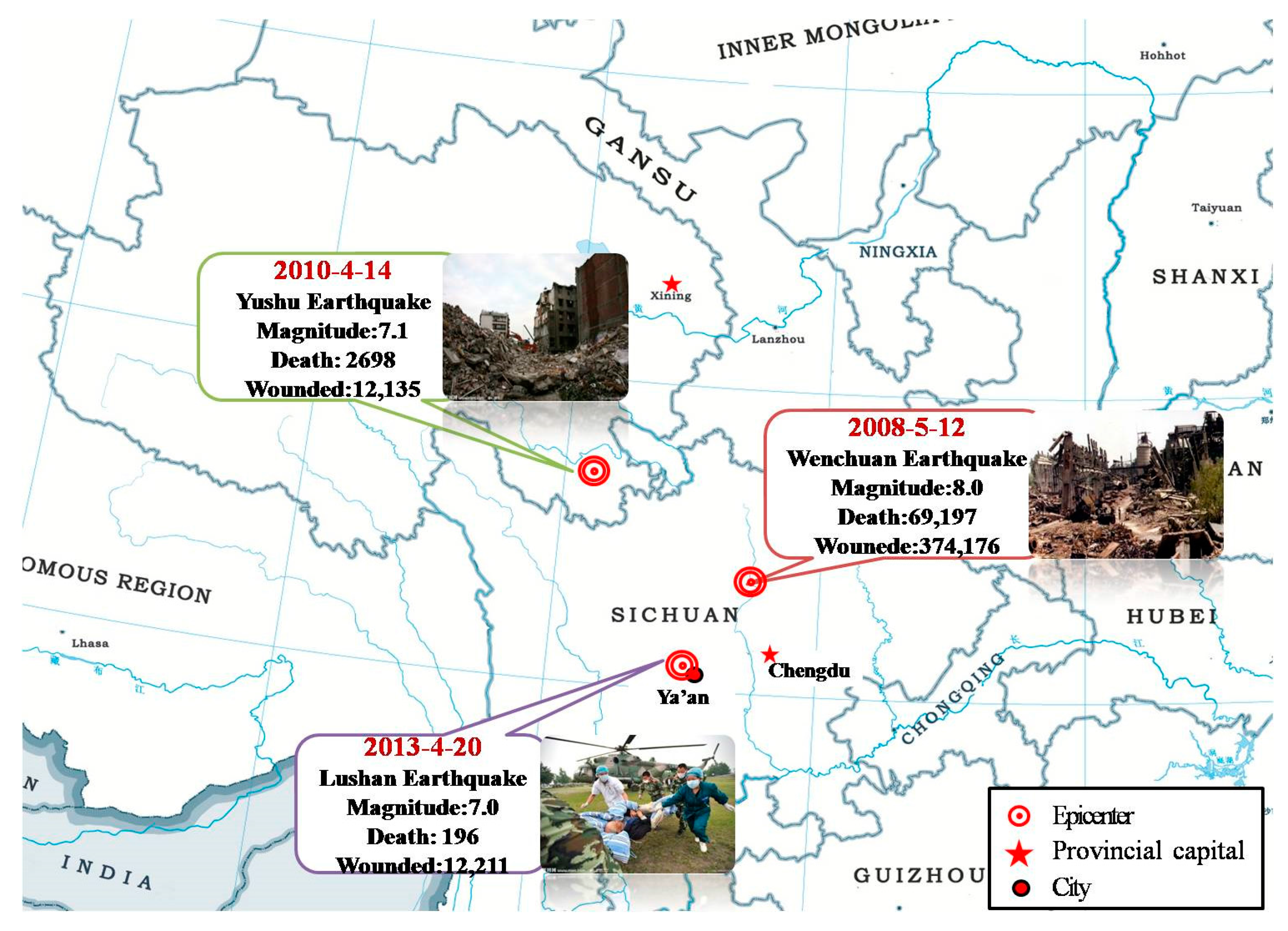
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Key Variables
2.4. Injury Coding
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
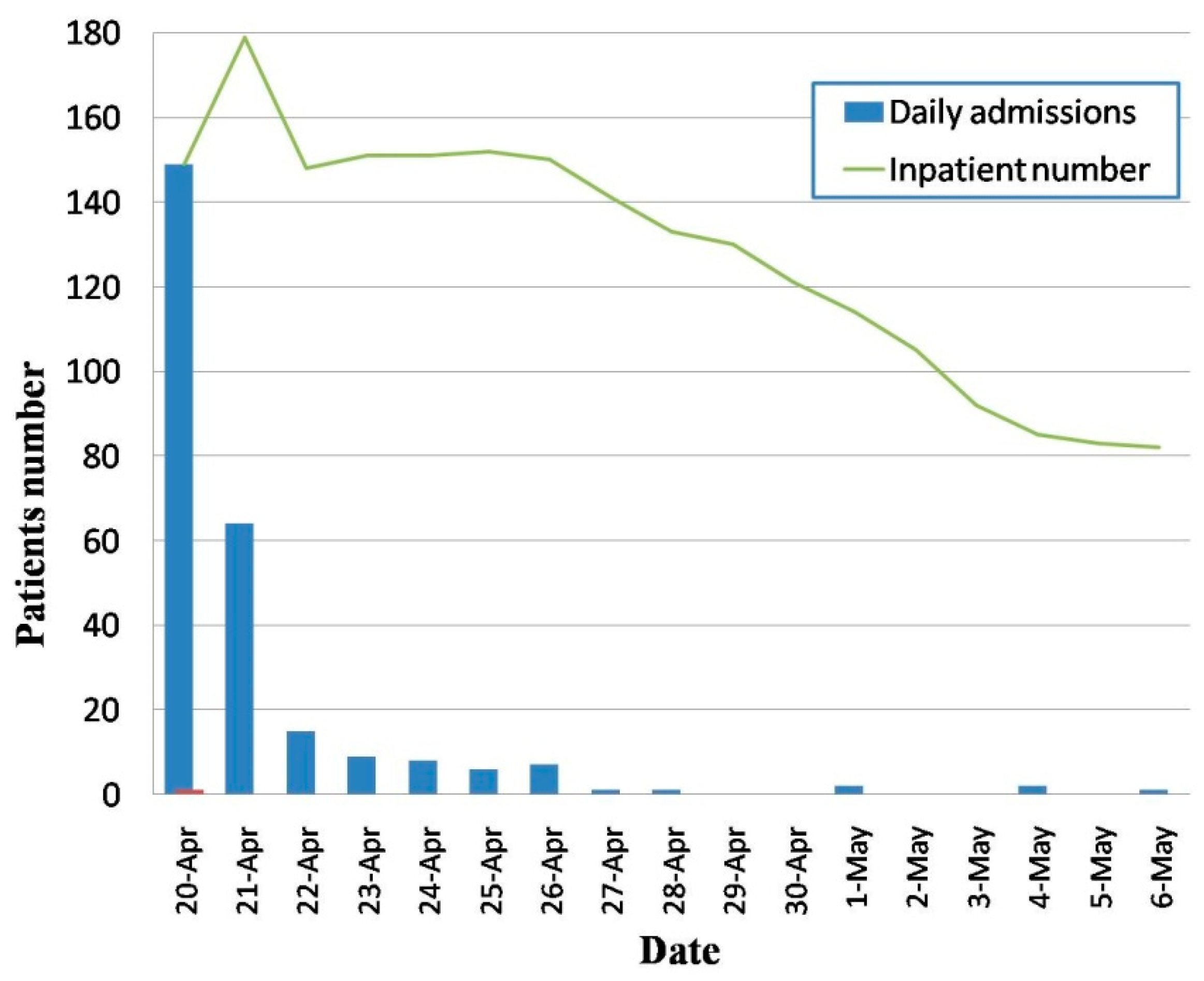
3.1. Medical Evacuation and Admission
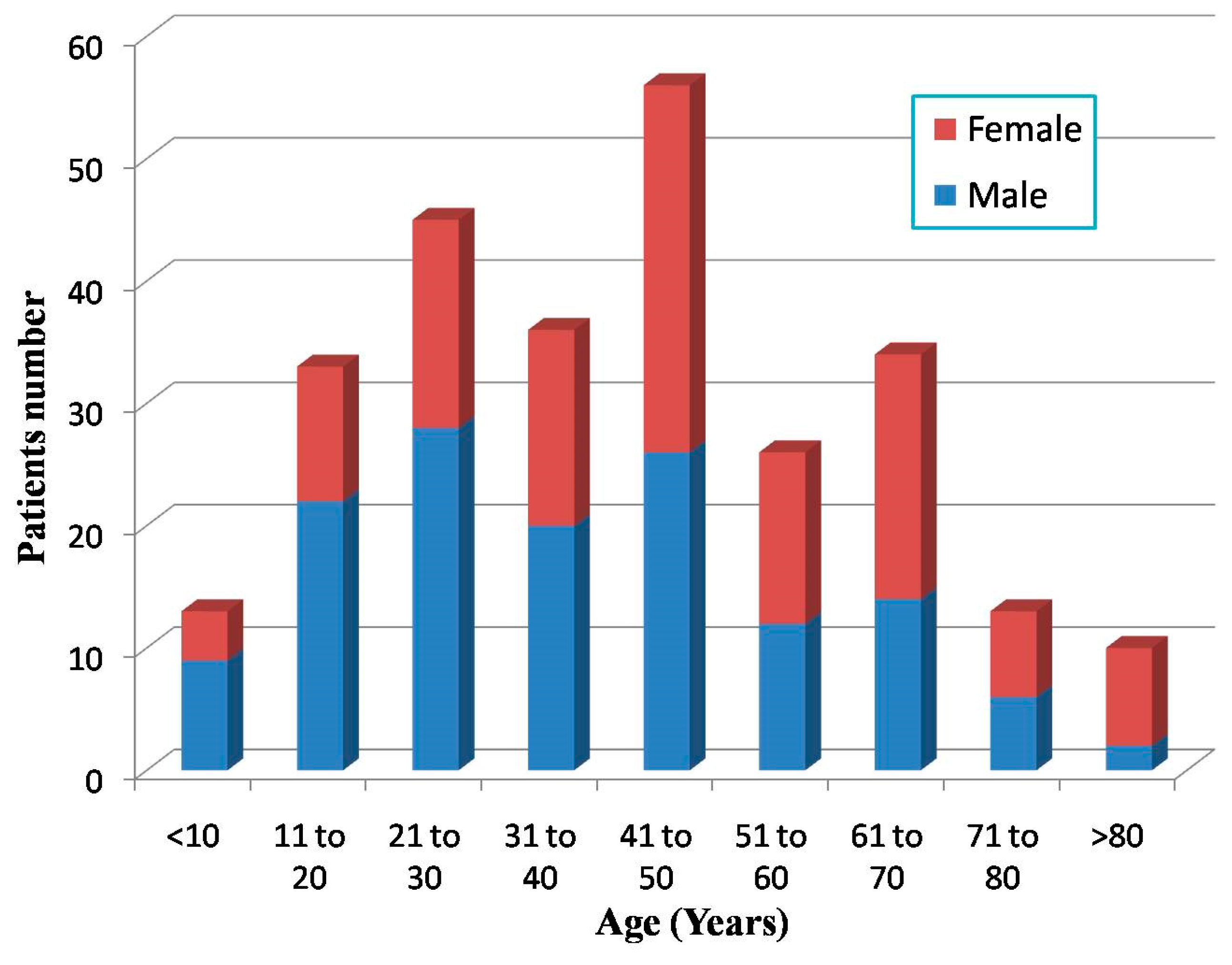
3.2. General Injury Profile
| Number of Injury Diagnoses | Number (%) |
|---|---|
| 1 | 118 (44.4) |
| 2 | 73 (27.4) |
| 3 | 45 (16.9) |
| >3 | 30 (11.3) |
| Injury Diagnoses | Body Region | Total Number (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Head | Face | Thorax | Spine | Upper Extremities | Lower Extremities and Pelvis | Abdomen | Body Surface and Others | ||
| Fracture | 7 | 11 | 25 | 50 | 21 | 102 | 0 | 0 | 216 (41.5) |
| Soft tissue injury | 6 | 3 | 2 | 1 | 11 | 29 | 1 | 90 | 143 (27.5) |
| Contusion & Laceration | 57 | 13 | 10 | 0 | 13 | 33 | 2 | 2 | 130 (25.0) |
| Crush injury | 0 | 0 | 1 | 0 | 1 | 4 | 0 | 0 | 6 (1.2) |
| Burns and Scalds | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 1 | 5 (1.0) |
| Closed injury | 3 | 1 | 7 | 0 | 0 | 0 | 1 | 0 | 12 (2.3) |
| Dislocation | 0 | 0 | 0 | 1 | 2 | 6 | 0 | 0 | 9 (1.7) |
| Total Number (%) | 73 (14.0) | 28 (5.4) | 45 (8.6) | 52 (10.0) | 48 (9.2) | 178 (34.2) | 4 (0.8) | 93 (17.9) | 521 (100) |
| Cause of Injury | Body Region | Total Number (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Head | Face | Thorax | Spine | Upper Extremities | Lower Extremities and Pelvis | Abdomen | Body Surface and Others | ||
| Hit/trapped by objects | 39 | 11 | 18 | 13 | 6 | 44 | 1 | 44 | 176 (33.8) |
| Motor vehicle | 1 | 3 | 1 | 0 | 1 | 8 | 0 | 3 | 17 (3.3) |
| Burns/scalds | 0 | 0 | 2 | 0 | 0 | 6 | 0 | 1 | 9 (1.7) |
| Fall/slip | 7 | 4 | 5 | 11 | 11 | 24 | 1 | 10 | 73 (14.0) |
| Cutting/piercing | 0 | 0 | 0 | 0 | 11 | 1 | 0 | 1 | 13 (2.5) |
| Injured during rescue | 3 | 0 | 5 | 2 | 6 | 8 | 0 | 8 | 32 (6.1) |
| Others | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 (0.2) |
| AIS Score | Body Region | Total Number (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Head | Face | Thorax | Spine | Upper Extremities | Lower Extremities and Pelvis | Abdomen | Surface Area $ Others | ||
| 1 (minor) | 44 | 18 | 9 | 1 | 23 | 60 | 2 | 83 | 240 (46.1) |
| 3 | 7 | 2 | 18 | 3 | 5 | 29 | 0 | 1 | 65 (12.5) |
| 4 | 3 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 6 (1.2) |
| 5 | 2 | 0 | 0 | 2 | 0 | 3 | 0 | 0 | 7 (1.3) |
| 6 (fatal) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) |
| Associated Injury Diagnoses | Number (%) |
|---|---|
| Contusion & Laceration, Soft Tissue Injury | 26 (35.6) |
| Head, body surface | 13 |
| Lower extremities, body surface | 5 (6.5) |
| Upper extremities | 3 (3.9) |
| Head, lower extremities | 2 (2.6) |
| Head, upper extremities | 1 (1.3) |
| Head, Abdomen | 1 (1.3) |
| Upper extremities, body surface | 1 (1.3) |
| Fracture, Soft Tissue Injury | 14 (19.2) |
| Spine, body surface | 5 (6.5) |
| Spine, lower extremities | 3 (3.9) |
| Lower extremities | 1 (1.3) |
| Upper extremities | 1 (1.3) |
| Lower & upper extremities | 1 (1.3) |
| Lower extremities, head | 1 (1.3) |
| Lower extremities, body surface | 1 (1.3) |
| Rips, body surface | 1 (1.3) |
| Two Fractures | 11 (15.1) |
| Lower extremities | 7 (9.1) |
| Spine | 2 (2.6) |
| Lower extremities, face | 1 (1.3) |
| Lower & upper extremities | 1 (1.3) |
| Two Contusion & Laceration Injuries | 6 (8.2) |
| Upper extremities | 1 (1.3) |
| Head | 1 (1.3) |
| Face | 1 (1.3) |
| Head, face | 1 (1.3) |
| Head, Lower extremities | 1 (1.3) |
| Head, Thorax | 1 (1.3) |
| Fracture, Contusion & Laceration | 4 (5.4) |
| Lower extremities | 3 (3.9) |
| Lower extremities, face | 1 (1.3) |
| Fracture, Dislocation | 4 (5.4) |
| Lower extremities | 3 (3.9) |
| Upper extremities | 1 (1.3) |
| Closed injury, Soft Tissue Injury | 3 (4.1) |
| Head, body surface | 2 (2.6) |
| Thorax, body surface | 1 (1.3) |
| Fracture, Closed Injury | 2 (2.7) |
| Thorax | 2 (2.6) |
| Fracture, Closed Injury | 1 (1.3) |
| Lower extremities | 1 (1.3) |
| Two Soft Tissue Injuries | 1 (1.3) |
| Thorax, lower extremities | 1 (1.3) |
| Dislocation, Soft Tissue Injury | 1 (1.3) |
| Spine, body surface | 1 (1.3) |
4. Discussion
5. Conclusions
Key Messages
- Emergency transportation for severe injuries in the early phase after the earthquakes played a crucial role in decrease the mortality and morbidity.
- It is necessary for hospitals to initiate effective emergency measures while facing the peak admission flow within the initial 48-hour period.
- The injuries caused by earthquakes were always complex and of various patterns, which presented sudden and serious crisis for health management and treatment centers
- More attention should be paid to the importance of instructing correct methods of self-rescue to avoid unnecessary injuries when aftershock occurs.
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Reitherman, R. How to prepare a hospital for an earthquake. J. Emerg. Med. 1986, 4, 119–131. [Google Scholar] [CrossRef]
- Mahoney, L.E.; Reutershan, T.P. Catastrophic disasters and the design of disaster medical care systems. Ann. Emerg. Med. 1987, 16, 1085–1091. [Google Scholar] [CrossRef]
- Li, T.; Jiang, X.; Chen, H.; Yang, Z.; Wang, X.; Wang, M. Orthopaedic injury analysis in the 2010 Yushu, Shina earthquake. Injury 2012, 43, 886–890. [Google Scholar] [CrossRef] [PubMed]
- Bartels, S.A.; VanRooyen, M.J. Medical complications associated with earthquakes. Lancet 2012, 379, 748–757. [Google Scholar] [CrossRef]
- Doocy, S.; Daniels, A.; Packer, C.; Dick, A.; Kirsch, T.D. The human impact of earthquakes: A historical review of events 1980–2009 and systematic literature review. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Lu-Ping, Z.; Rodriguez-Llanes, J.M.; Qi, W.; van den Oever, B.; Westman, L.; Albela, M.; Liang, P.; Gao, C.; de-Sheng, Z.; Hughes, M. Multiple injuries after earthquakes: A retrospective analysis on 1871 injured patients from the 2008 Wenchuan earthquake. Crit. Care 2012, 16. [Google Scholar] [CrossRef] [PubMed]
- Doocy, S.; Jacquet, G.; Cherewick, M.; Kirsch, T.D. The injury burden of the 2010 Haiti earthquake: A stratified cluster survey. Injury 2013, 44, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Zhang, L. Ya’an earthquake. Lancet 2013, 381, 1984–1985. [Google Scholar] [CrossRef]
- Palmer, C.S.; Niggemeyer, L.E.; Charman, D. Double coding and mapping using Abbreviated Injury Scale 1998 and 2005: Identifying issues for trauma data. Injury 2010, 41, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Osler, T.; Baker, S.P.; Long, W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J. Trauma. 1997, 43, 922–926. [Google Scholar] [CrossRef] [PubMed]
- Foreman, B.P.; Caesar, R.R.; Parks, J.; Madden, C.; Gentilello, L.M.; Shafi, S.; Carlile, M.C.; Harper, C.R.; Diaz-Arrastia, R.R. Usefulness of the abbreviated injury score and the injury severity score in comparison to the glasgow coma scale in predicting outcome after traumatic brain injury. J. Trauma. Acute. Care. Surg. 2007, 62, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Vallier, H.A.; Le, T.T.; Bedi, A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): Plating versus intramedullary nailing. J. Orthop. Trauma 2008, 22, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Khatod, M.; Botte, M.J.; Hoyt, D.B.; Meyer, R.S.; Smith, J.M.; Akeson, W.H. Outcomes in open tibia fractures: Relationship between delay in treatment and infection. J. Trauma. Acute. Care. Surg. 2003, 55, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, N.; Lebel, E.; Merin, O.; Levy, G.; Bar-On, E. Skeletal injuries sustained during the Haiti earthquake of 2010: A radiographic analysis of the casualties admitted to the Israel defense forces field hospital. Eur. J. Trauma Emerg. Surg. 2013, 39, 117–122. [Google Scholar] [CrossRef]
- Peek-Asa, C.; Ramirez, M.; Seligson, H.; Shoaf, K. Seismic, structural, and individual factors associated with earthquake related injury. Inj. Prev. 2003, 9, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Mulvey, J.; Awan, S.; Qadri, A.; Maqsood, M. Profile of injuries arising from the 2005 Kashmir earthquake: The first 72h. Injury 2008, 39, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, H.; Carlton, J.R.; Ursano, R. The injury profile after the 2008 earthquakes in China. Injury 2009, 40, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Rao, G.; Jia, D.; Yan, B.; Ren, Z. Co-seismic strike-slip surface rupture and displacement produced by the 2010 Mw 6.9 Yushu earthquake, China, and implications for Tibetan tectonics. J. Geodynamics 2011, 52, 249–259. [Google Scholar] [CrossRef]
- Kang, P.; Zhang, L.; Liang, W.; Zhu, Z.; Liu, Y.; Liu, X.; Yang, H. Medical evacuation management and clinical characteristics of 3255 inpatients after the 2010 Yushu earthquake in China. J. Trauma. Acute. Care. Surg. 2012, 72, 1626–1633. [Google Scholar] [CrossRef] [PubMed]
- Baxt, W.G.; Moody, P.; Cleveland, H.C.; Fischer, R.P.; Kyes, F.N.; Leicht, M.J.; Rouch, F.; Wiest, P. Hospital-based rotorcraft aeromedical emergency care services and trauma mortality: A multicenter study. Ann. Emerg. Med. 1985, 14, 859–864. [Google Scholar] [CrossRef]
- Baxt, W.G.; Moody, P. The impact of a rotorcraft aeromedical emergency care service on trauma mortality. JAMA 1983, 249, 3047–3051. [Google Scholar] [CrossRef] [PubMed]
- Salimi, J.; Abbasi, M.; Khaji, A.; Zargar, M. Analysis of 274 patients with extremity injuries caused by the Bam earthquake. Chin. J. Traumatol. 2009, 12, 10–13. [Google Scholar] [PubMed]
- Nakamori, Y.; Tanaka, H.; Oda, J.; Kuwagata, Y.; Matsuoka, T.; Yoshioka, T. Burn injuries in the 1995Hanshin-Awaji earthquake. Burns 1997, 23, 319–322. [Google Scholar] [CrossRef]
- Ad-El, D.D.; Engelhard, D.; Beer, Y.; Dudkevitz, I.; Benedeck, P. Earthquake related scald injuries—Experience from the IDF field hospital in Duzce, Turkey. Burns 2001, 27, 401–403. [Google Scholar] [CrossRef]
- Bulut, M.; Fedakar, R.; Akkose, S.; Akgoz, S.; Ozguc, H.; Tokyay, R. Medical experience of a university hospital in turkey after the 1999 Marmara earthquake. Emerg. Med. J. 2005, 22, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Collins, A.J. Kidney dialysis treatment for victims of the Armenian earthquake. N. Engl. J. Med. 1989, 320, 1291–1292. [Google Scholar] [CrossRef] [PubMed]
- Kuwagata, Y.; Oda, J.; Tanaka, H.; Iwai, A.; Matsuoka, T.; Takaoka, M.; Kishi, M.; Morimoto, F.; Ishikawa, K.; Mizushima, Y. Analysis of 2702 traumatized patients in the 1995 Hanshin-Awaji earthquake. J. Trauma. Acute. Care. Surg. 1997, 43, 427–432. [Google Scholar] [CrossRef]
- Tanaka, H.; Oda, J.; Iwai, A.; Kuwagata, Y.; Matsuoka, T.; Takaoka, M.; Kishi, M.; Morimoto, F.; Ishikawa, K.; Mizushima, Y. Morbidity and mortality of hospitalized patients after the 1995 Hanshin-Awaji earthquake. Am. J. Emerg. Med. 1999, 17, 186–191. [Google Scholar] [CrossRef]
- Maruo, S.; Matumoto, M. Spinal fractures resulting from the 1995 Great Hanshin Earthquake of the Kobe-Osaka area of Japan. Spinal. Cord. 1996, 34, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Naghi, T.M.; Kambiz, K.; Shahriar, J.M.; Afshin, T.; Reza, S.K.; Behnam, P.; Bahador, A.H. Musculoskeletal injuries associated with earthquake: A report of injuries of Iran’s December 26, 2003 Bam earthquake casualties managed in tertiary referral centers. Injury 2005, 36, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Iwai, A.; Oda, J.; Kuwagata, Y.; Matsuoka, T.; Shimazu, T.; Yoshioka, T. Overview of evacuation and transport of patients following the 1995 Hanshin-Awaji earthquake. J. Emerg. Med. 1998, 16, 439–444. [Google Scholar] [CrossRef]
- Whittaker, R.; Farmed, D.; Green, P.; Barry, P.; Borge, A.; Fletes-Barrios, R. Earthquake disaster in Nicaragua: Reflections on the initial management of massive casualties. J Trauma Acute Care Surg. 1974, 14, 37–43. [Google Scholar] [CrossRef]
- Rizzo, B.G.L. Earthquake injuries related to housing in a Guatemalan village. Science 1977, 197, 638–643. [Google Scholar]
- Gavalya, A.S. Reactions to the 1985 Mexican earthquake: case vignettes. Hosp. Community Psychiatry 1987, 38, 1327–1330. [Google Scholar] [CrossRef] [PubMed]
- Bird, J.; Bommer, J.; Bray, J.; Sancio, R.; Spence, R. Comparing loss estimation with observed damage in a zone of ground failure: A study of the 1999 Kocaeli earthquake in Turkey. Bull. Earthq. Eng. 2004, 2, 329–360. [Google Scholar] [CrossRef]
- Petal, M. Evidence-Based Public Education for Disaster Prevention: Causes of Deaths and Injuries in the 1999 Kocaeli Earthquake. Available online: https://www.morebooks.de/store/gb/book/evidence-based-public-education-for-disaster-prevention/isbn/978-3-639-13297-7 (accessed on 29 August 2015).
- Armenian, H.K.; Melkonian, A.; Noji, E.K.; Hovanesian, A.P. Deaths and injuries due to the earthquake in Armenia: A cohort approach. Int. J. Epidemio. 1997, 26, 806–813. [Google Scholar] [CrossRef]
- Phalkey, R.; Reinhardt, J.D.; Marx, M. Injury epidemiology after the 2001 Gujarat earthquake in India: A retrospective analysis of injuries treated at a rural hospital in the Kutch district immediately after the disaster. Glob. Health Action 2011, 4. [Google Scholar] [CrossRef] [PubMed]
- Behrman, S.W.; Fabian, T.C.; Kudsk, K.A.; Taylor, J.C. Improved outcome with femur fractures: Early vs. Delayed fixation. J. Trauma. Acute. Care. Surg. 1990, 30, 792–798. [Google Scholar] [CrossRef]
- Hildebrand, F.; Giannoudis, P.; Kretteck, C.; Pape, H.-C. Damage control: Extremities. Injury 2004, 35, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Bose, D.; Tejwani, N. Evolving trends in the care of polytrauma patients. Injury 2006, 37, 20–28. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, P.; Tang, B.; Liu, Y.; Liu, X.; Liu, Z.; Lv, Y.; Zhang, L. Medical Efforts and Injury Patterns of Military Hospital Patients Following the 2013 Lushan Earthquake in China: A Retrospective Study. Int. J. Environ. Res. Public Health 2015, 12, 10723-10738. https://doi.org/10.3390/ijerph120910723
Kang P, Tang B, Liu Y, Liu X, Liu Z, Lv Y, Zhang L. Medical Efforts and Injury Patterns of Military Hospital Patients Following the 2013 Lushan Earthquake in China: A Retrospective Study. International Journal of Environmental Research and Public Health. 2015; 12(9):10723-10738. https://doi.org/10.3390/ijerph120910723
Chicago/Turabian StyleKang, Peng, Bihan Tang, Yuan Liu, Xu Liu, Zhipeng Liu, Yipeng Lv, and Lulu Zhang. 2015. "Medical Efforts and Injury Patterns of Military Hospital Patients Following the 2013 Lushan Earthquake in China: A Retrospective Study" International Journal of Environmental Research and Public Health 12, no. 9: 10723-10738. https://doi.org/10.3390/ijerph120910723






