Long-Term Effectiveness of Antiretroviral Therapy in China: An Observational Cohort Study from 2003–2014
Abstract
:1. Introduction
2. Methods
2.1. Patients and Treatment Regimens
2.2. Data Collection
2.3. Statistical Analysis
3. Results
| Characteristic | Patients with Baseline CD4 Cell Count Less Than 350 cells/μL | ||||
|---|---|---|---|---|---|
| All Patients (N = 6897) | All Patients (N = 3815) | No ART (N = 1141) | ART (N = 2674) | P | |
| Median Age | 32 (IQR, 27–39) | 33 (28–40) | 32 (26–39) | 33 (28–41) | <0.001 |
| Gender | <0.001 | ||||
| Male | 5768 (83.63%) | 3105 (81.39%) | 984 (86.24%) | 2121 (79.32%) | |
| Female | 1129 (16.37%) | 710 (18.61%) | 157 (13.76%) | 553 (20.68%) | |
| Native Resident | <0.001 | ||||
| Yes | 4841 (72.19%) | 2826 (74.08%) | 739 (64.77%) | 2087 (78.05%) | |
| No | 2056 (27.81%) | 989 (25.92%) | 402 (35.23%) | 587 (21.95%) | |
| Marital Status | <0.001 | ||||
| Unmarried | 3707 (53.75%) | 1863 (48.83%) | 649 (56.88%) | 1214 (45.40%) | |
| Married | 2158 (31.29%) | 1370 (35.91%) | 312 (27.34%) | 1058 (39.57%) | |
| Divorced | 963 (13.96%) | 564 (14.78%) | 173 (15.16%) | 391 (14.62%) | |
| Unknown | 69 (1%) | 18 (0.48%) | 7 (0.62%) | 11 (0.41%) | |
| Infection Route | <0.001 | ||||
| Heterosexual | 3686 (53.44%) | 2166 (56.79%) | 614 (53.81%) | 1552 (58.04%) | |
| Homosexual | 2194 (31.81%) | 1186 (31.09%) | 337 (29.54%) | 849 (31.75%) | |
| Injection Drug Use | 775 (11.24%) | 334 (8.75%) | 165 (14.46%) | 169 (6.32%) | |
| Others | 222 (3.22%) | 121 (3.17%) | 22 (1.93%) | 99 (3.70%) | |
| Unknown | 20 (0.29%) | 8 (0.20%) | 2 (0.18%) | 6 (0.22%) | |
| Baseline AIDS Stage | <0.001 | ||||
| Yes | 2803 (40.64%) | 2409 (63.15%) | 409 (35.85%) | 2000 (74.79%) | |
| No | 4094 (59.36%) | 1406 (36.85%) | 732 (64.15%) | 674 (25.21%) | |
| Baseline Tuberculosis | <0.001 | ||||
| Positive | 310 (4.49%) | 210 (5.50%) | 30 (2.63%) | 180 (6.73%) | |
| Negative | 6587 (95.51%) | 3605 (94.50%) | 1111 (97.37%) | 2494 (93.27%) | |
| Baseline CD4 Cell Count, cells/µL | <0.001 | ||||
| 0–99 | 996 (14.44%) | 996 (26.11%) | 224 (19.63%) | 772 (28.87%) | |
| 100–199 | 894 (12.96%) | 894 (23.43%) | 116 (10.17%) | 778 (29.09%) | |
| 200–349 | 1925 (27.91%) | 1925 (50.46%) | 801 (70.11%) | 1124 (42.07%) | |
| ≥350 | 2441 (35.39%) | - | - | ||
| Unknown | 641 (9.30%) | - | - | ||
| ART | Death | |||
|---|---|---|---|---|
| Hazard Ratio(95% CI) | P | Hazard Ratio(95% CI) | P | |
| Age Group, year | ||||
| 16–25 | 1.00 | - | 1.00 | - |
| 26–35 | 1.60 (1.26–2.02) | <0.001 | 1.13 (0.59–2.18) | 0.699 |
| 36–45 | 2.05 (1.56–2.68) | <0.001 | 1.41 (0.70–2.85) | 0.338 |
| >45 | 2.61 (1.81–3.77) | <0.001 | 1.87 (0.83–4.19) | 0.129 |
| Sex (Female vs.Male) | 2.35 (1.77–3.12) | <0.001 | 0.97 (0.52–1.81) | 0.916 |
| Baseline CD4 Cell Count, cells/µL | ||||
| 0–99 | 1.00 | - | 1.00 | - |
| 100–199 | 0.35 (0.22–0.58) | <0.001 | 0.21 (0.14–0.31) | <0.001 |
| 200–349 | 0.19 (0.12–0.31) | <0.001 | 0.13 (0.09–0.19) | <0.001 |
| ≥350 | 0.02 (0.01–0.03) | <0.001 | 0.10 (0.07–0.14) | <0.001 |
| Latest CD4 Cell Count, cells/µL | ||||
| 0–99 | - | - | 1.00 | |
| 100–199 | - | - | 0.13 (0.07–0.24) | <0.001 |
| 200–349 | - | - | 0.05 (0.02–0.10) | <0.001 |
| ≥350 | - | - | 0.03 (0.02–0.08) | <0.001 |
| Baseline AIDS Stage (Yes vs.No) | 16.40 (12.31–21.86) | <0.001 | 1.79 (0.81–3.94) | 0.148 |
| Baseline Tuberculosis (Yes vs.No) | 1.81 (1.06–3.07) | 0.029 | 1.63 (1.16–2.08) | 0.004 |
| ART (Yes vs.No) | - | - | 0.21 (0.12–0.35) | <0.001 |
| Variable | Outcome | Unweighted Models, No Covariates | Unweighted Models, Baseline and Time-Varying Covariates | Weighted Model Baseline Covariates a | Patients (N) |
|---|---|---|---|---|---|
| Patients with any baseline CD4 cell count | |||||
| ART | Death | 0.25 (0.19–0.38) | 0.21 (0.14–0.31) | 0.18 (0.11–0.27) | 6897 |
| ART | Tuberculosis | 0.34 (0.26–0.43) | 0.29 (0.21–0.38) | 0.27 (0.19–0.37) | 6897 |
| Per additional month of ART | CD4 cell count, cells/µL | 5.67 (5.19–6.01) | 5.83 (5.29–6.41) | 6.52 (6.08–7.12) | 2719 b |
| Patients with baseline CD4 cell count less than 350 cells/µL | |||||
| ART | Death | 0.21 (0.15–0.29) | 0.15 (0.12–0.19) | 0.10 (0.06–0.13) | 3815 |
| ART | Tuberculosis | 0.15 (0.11–0.20) | 0.09 (0.06–0.11) | 0.06 (0.03–0.08) | 3815 |
| Per additional month of ART | CD4 cell count, cells/µL | 10.21 (9.32–11.01) | 4.52 (4.19–4.92) | 5.23 (4.91–5.59) | 1432 b |
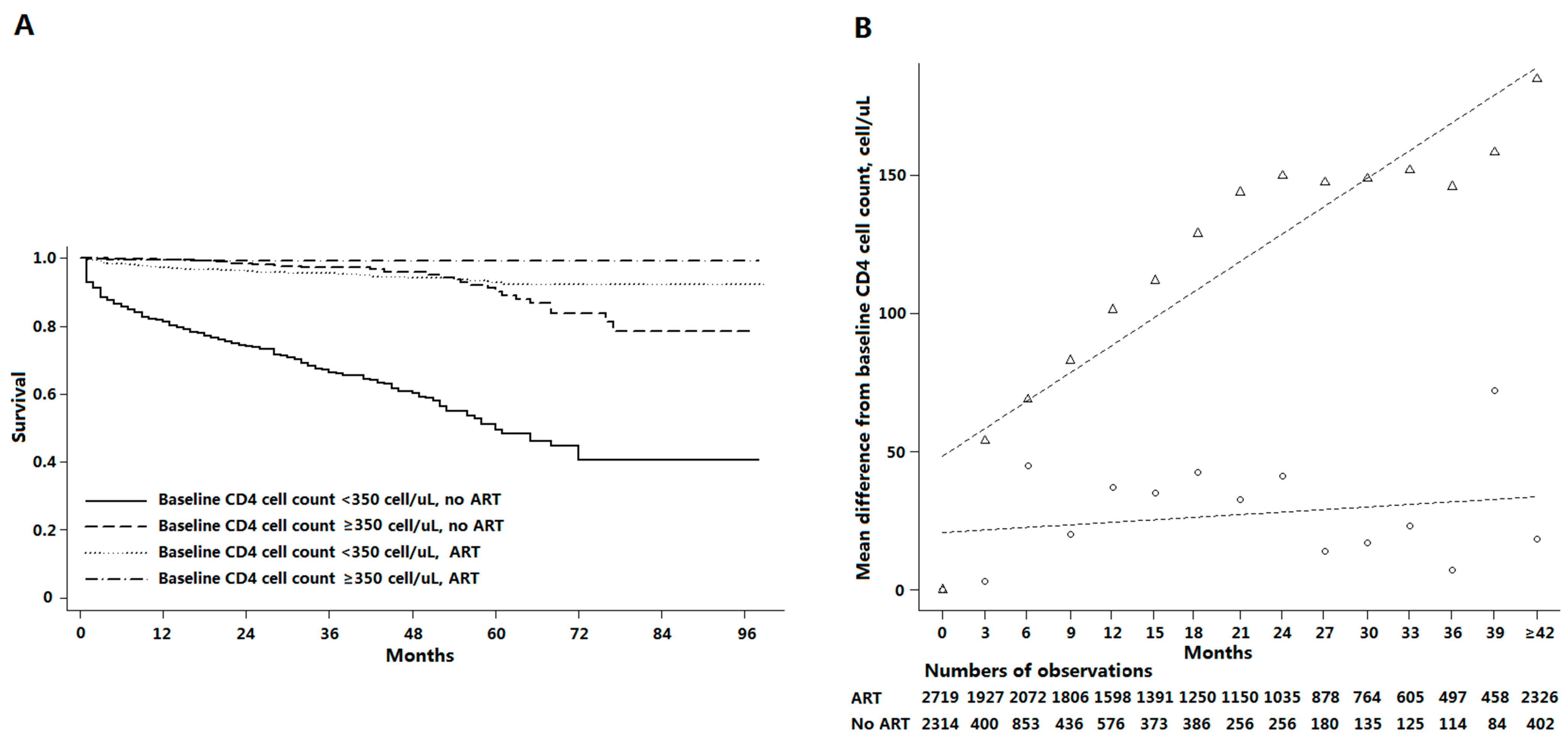
4. Discussion and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wang, N.; Wang, L.; Wu, Z.; Guo, W.; Sun, X.; Poundstone, K.; Wang, Y.; National Expert Group on HIV/AIDS Estimation. Estimating the number of people living with HIV/AIDS in China: 2003–09. Int. J. Epidemiol. 2010, 39, ii21–ii28. [Google Scholar] [CrossRef] [PubMed]
- State Council AIDS Working Committee Office (SCAWCO) and UN Theme Group on AIDS in China (UNTGAC). A Joint Assessment of HIV/AIDS Prevention, Treatment and Care in China (2009); State Council AIDS Working Committee Office (SCAWCO) and UN Theme Group on AIDS in China (UNTGAC): Beijing, China, 2009. [Google Scholar]
- Zhang, F.; Haberer, J.E.; Wang, Y.; Zhao, Y.; Ma, Y.; Zhao, D.; Yu, L.; Goosby, E.P. The Chinese free antiretroviral treatment program: Challenges and responses. AIDS 2007, 21, S143–S148. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Sullivan, S.G.; Wang, Y.; Rotheram-Borus, M.J.; Detels, R. Evolution of China’s response to HIV/AIDS. Lancet 2007, 369, 679–690. [Google Scholar] [CrossRef]
- Zhang, F.; Dou, Z.; Ma, Y.; Zhang, Y.; Zhao, Y.; Zhao, D.; Zhou, S.; Bulterys, M.; Zhu, H.; Chen, R.Y. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: A national observational cohort study. Lancet Infect. Dis. 2011, 11, 516–524. [Google Scholar] [CrossRef]
- Wong, K.-H.; Chan, K.C.-W. HAART for HIV in China—Much achieved, more to be done. Lancet Infect. Dis. 2011, 11, 491–492. [Google Scholar] [CrossRef]
- Ma, Y.; Zhao, D.; Yu, L.; Bulterys, M.; Robinson, M.L.; Zhao, Y.; Dou, Z.; Chiliade, P.; Wei, X.; Zhang, F. Predictors of virologic failure in HIV-1-infected adults receiving first-line antiretroviral therapy in 8 provinces in China. Clin. Infect. Dis. 2010, 50, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Dou, Z.; Ma, Y.; Zhao, Y.; Liu, Z.; Bulterys, M.; Chen, R.Y. Five-year outcomes of the China national free antiretroviral treatment program. Ann. Intern. Med. 2009, 151, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Dou, Z.; Yu, L.; Xu, J.; Jiao, J.H.; Wang, N.; Ma, Y.; Zhao, Y.; Zhao, H.; Chen, R.Y. The effect of highly active antiretroviral therapy on mortality among HIV-infected former plasma donors in China. Clin. Infect. Dis. 2008, 47, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Benson, K.; Hartz, A.J. A comparison of observational studies and randomized, controlled trials. N. Engl. J. Med. 2000, 342, 1878–1886. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Ledergerber, B.; Tilling, K.; Weber, R.; Sendi, P.; Rickenbach, M.; Robins, J.M.; Egger, M. Long-term effectiveness of potent antiretroviral therapy in preventing AIDS and death: A prospective cohort study. Lancet 2005, 366, 378–384. [Google Scholar] [CrossRef]
- Fairall, L.R.; Bachmann, M.O.; Louwagie, G.M.C.; van Vuuren, C.; Chikobvu, P.; Steyn, D.; Staniland, G.H.; Timmerman, V.; Msimanga, M.; Seebregts, C.J.; et al. Effectiveness of antiretroviral treatment in a South African program: A cohort study. Arch. Intern. Med. 2008, 168, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Sun, X.; He, Y.; Tang, Z.; Peng, G.; Liu, A.; Qiao, X.; Li, H.; Chen, Z.; Dou, Z.; et al. Progress of the national pediatric free antiretroviral therapy program in China. AIDS Care 2010, 22, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Gilmour, S.; Zhang, H.; Koyanagi, A.; Shibuya, K. The epidemiological impact and cost-effectiveness of HIV testing, antiretroviral treatment and harm reduction programs. AIDS 2012, 26, 2069–2078. [Google Scholar] [CrossRef] [PubMed]
- Long, L.; Brennan, A.; Fox, M.P.; Ndibongo, B.; Jaffray, I.; Sanne, I.; Rosen, S. Treatment outcomes and cost-effectiveness of shifting management of stable art patients to nurses in South Africa: An observational cohort. PLoS Med. 2011, 8, e1001055. [Google Scholar] [CrossRef] [PubMed]
- Crum, N.F.; Riffenburgh, R.H.; Wegner, S.; Agan, B.K.; Tasker, S.A.; Spooner, K.M.; Armstrong, A.W.; Fraser, S.; Wallace, M.R.; Triservice AIDS Clinical Consortium. Comparisons of causes of death and mortality rates among HIV-infected persons: Analysis of the pre-, early, and late HAART (highly active antiretroviral therapy) eras. J. Acq. Immune Defic. Syndr. 2006, 41, 194–200. [Google Scholar] [CrossRef]
- Lohse, N.; Hansen, A.-B.E.; Pedersen, G.; Kronborg, G.; Gerstoft, J.; Sørensen, H.T.; Væth, M.; Obel, N. Survival of persons with and without hiv infection in Denmark, 1995–2005. Ann. Intern. Med. 2007, 146, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Dou, Z.; Chen, R.Y.; Xu, J.; Ma, Y.; Jiao, J.H.; Durako, S.; Zhao, Y.; Zhao, D.; Fang, H.; Zhang, F. Changing baseline characteristics among patients in the China national free antiretroviral treatment program, 2002–09. Int. J. Epidemiol. 2010, 39, ii56–ii64. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, D.; Carrieri, M.P.; Shepard, D. Treatment and care for injecting drug users with HIV infection: A review of barriers and ways forward. Lancet 2010, 376, 355–366. [Google Scholar] [CrossRef]
- Anglaret, X.; Minga, A.; Gabillard, D.; Ouassa, T.; Messou, E.; Morris, B.; Traore, M.; Coulibaly, A.; Freedberg, K.A.; Lewden, C.; et al. AIDS and non-AIDS morbidity and mortality across the spectrum of CD4 cell counts in HIV-infected adults before starting antiretroviral therapy in Côte d’Ivoire. Clin. Infect. Dis. 2012, 54, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.J.; Bakanda, C.; Birungi, J.; Mwesigwa, R.; Chan, K.; Ford, N.; Hogg, R.S.; Cooper, C. Mortality by baseline CD4 cell count among HIV patients initiating antiretroviral therapy: Evidence from a large cohort in Uganda. AIDS 2011, 25, 851–855. [Google Scholar] [CrossRef] [PubMed]
- UK Collaborative HIV Cohort (UK CHIC) Steering Committee; Sabin, C.A.; Schwenk, A.; Johnson, M.A.; Gazzard, B.; Fisher, M.; Walsh, J.; Orkin, C.; Hill, T.; Gilson, R.; et al. Late diagnosis in the HAART era: Proposed common definitions and associations with mortality. AIDS 2010, 24, 723–727. [Google Scholar] [PubMed]
- Cole, S.R.; Hernán, M.A. Constructing inverse probability weights for marginal structural models. Amer. J. Epidemiol. 2008, 168, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Hernán, M.A.; Hernández-Díaz, S.; Robins, J.M. A structural approach to selection bias. Epidemiology 2004, 15, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Kantor, R.; Diero, L.; DeLong, A.; Kamle, L.; Muyonga, S.; Mambo, F.; Walumbe, E.; Emonyi, W.; Chan, P.; Carter, E.J.; et al. Misclassification of first-line antiretroviral treatment failure based on immunological monitoring of HIV infection in resource-limited settings. Clin. Infect. Dis. 2009, 49, 454–462. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, P.; Tan, J.; Ma, W.; Zheng, H.; Lu, Y.; Wang, N.; Peng, Z.; Yu, R. Long-Term Effectiveness of Antiretroviral Therapy in China: An Observational Cohort Study from 2003–2014. Int. J. Environ. Res. Public Health 2015, 12, 8762-8772. https://doi.org/10.3390/ijerph120808762
Huang P, Tan J, Ma W, Zheng H, Lu Y, Wang N, Peng Z, Yu R. Long-Term Effectiveness of Antiretroviral Therapy in China: An Observational Cohort Study from 2003–2014. International Journal of Environmental Research and Public Health. 2015; 12(8):8762-8772. https://doi.org/10.3390/ijerph120808762
Chicago/Turabian StyleHuang, Peng, Jingguang Tan, Wenzhe Ma, Hui Zheng, Yan Lu, Ning Wang, Zhihang Peng, and Rongbin Yu. 2015. "Long-Term Effectiveness of Antiretroviral Therapy in China: An Observational Cohort Study from 2003–2014" International Journal of Environmental Research and Public Health 12, no. 8: 8762-8772. https://doi.org/10.3390/ijerph120808762





