Breastfeeding, Bottle Feeding Practices and Malocclusion in the Primary Dentition: A Systematic Review of Cohort Studies
Abstract
:1. Introduction
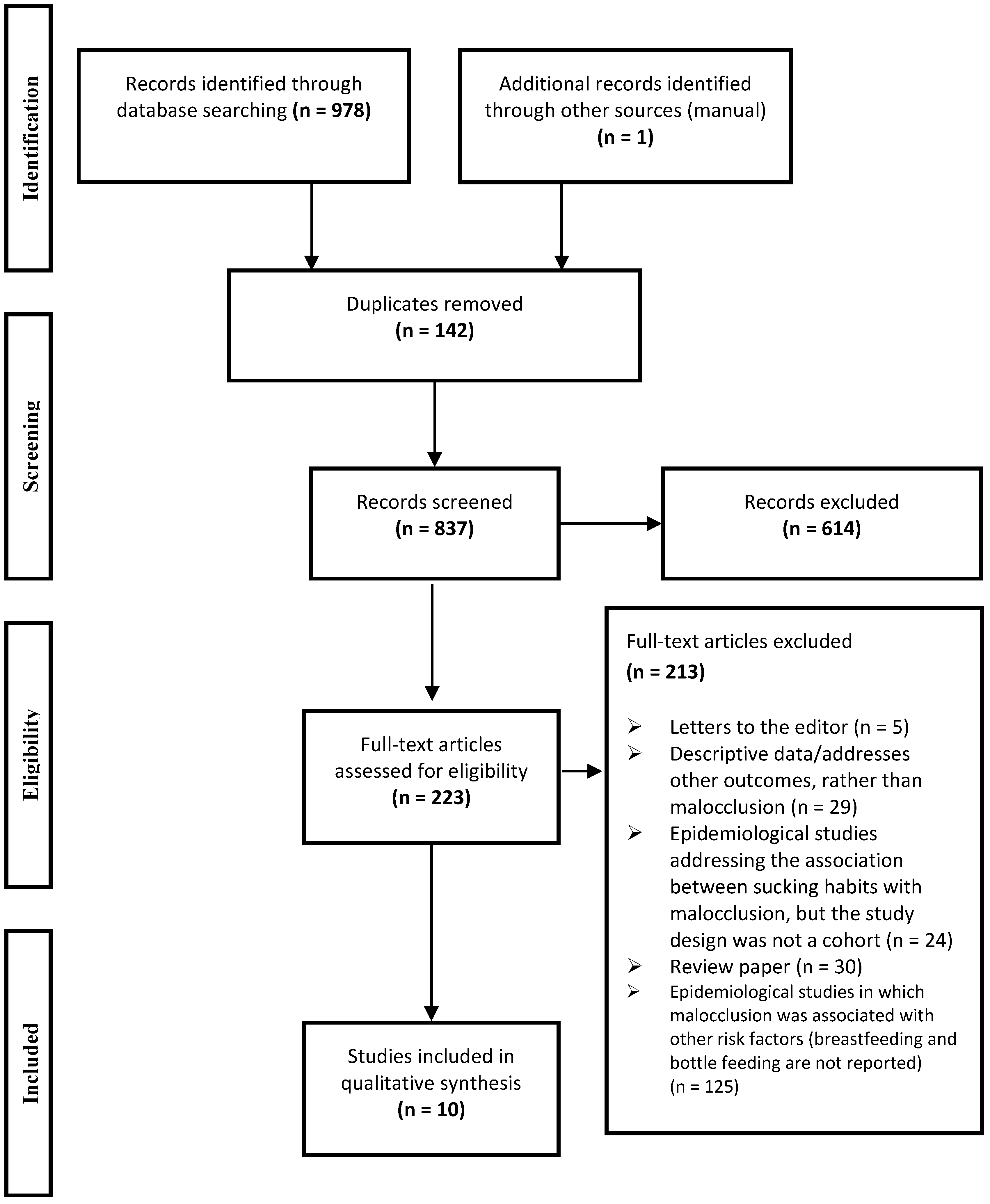
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
| Criteria | Cohort Studies and Their Assessment Ratings | |||||||||
| Davis & Bell, 1991 [16] | Karjalainen et al., 1999 [17] | Warren & Bishara, 2002 * [12] | Viggiano et al., 2004 [18] | Bishara et al., 2006 * [19] | Vásquez-Nava et al., 2006 [7] | Peres et al., 2007a * [13] | Peres et al., 2007b * [14] | Caramez da Silva et al., 2012 [20] | Moimaz et al., 2014 [21] | |
| Sample Selection Criteria | ||||||||||
| (1) Representativeness of the exposed cohort (bottle-fed) (a) Truly representative sample ★ (b) Somewhat representative of the average community (e.g., hospital) ★ (c) Potential for selection biases or not satisfying requirements in part (a) (d) No description of the derivation of the cohort | b (★) | c | b (★) | a (★) | b (★) | a (★) | a (★) | a (★) | b (★) | b (★) |
| (2) Selection of the non-exposed cohort (breastfeeding) (a) Drawn from the same community as the exposed cohort ★ (b) Drawn from a different source (c) No description of the derivation of the non-exposed cohort | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) |
| (3) Ascertainment of exposure (bottle feeding) (a) Data was collected periodically through questionnaires ★ (b) No mention related to the time interval of the feeding habit evaluation/data was collected only once (c) No description | a (★) | a (★) | a (★) | b | a (★) | b | a (★) | a (★) | a (★) | a (★) |
| (4) Demonstration that malocclusion was not present at the start of study (a) yes ★ (b) no description | b | b | b | b | b | b | b | b | b | b |
| Comparability of Cohorts on the Basis of the Design or Analysis | ||||||||||
| (1) Control for confounders (a) The exposure of interest (malocclusion) is adjusted for the one confounder ★ (b) The exposure of interest (malocclusion) is adjusted for two or more confounders ★★ (c) No description related to the adjustment analysis for confounding factors | c | c | c | a (★) | c | b (★★) | b (★★) | b (★★) | b (★★) | c |
| Outcome—Evaluation of Malocclusion | ||||||||||
| (1) Diagnosis of malocclusion (a) Clinical examination reporting the use of an index/report of observer agreement—kappa ★ (b) Satisfying requirements in (a) and independent blind assessment ★★ (c) Based on self-reports or not satisfying requirements in part (a, b) (d) No description | c | c | a (★) | c | a (★) | c | a (★) | a (★) | b (★★) | a (★) |
| (2) Was follow-up long enough for outcomes (malocclusion) to occur (a) Yes ★ (b) No | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) | a (★) |
| (3) Adequacy of follow up of cohorts (a) Complete follow up—all subjects accounted for ★ (b) Subjects lost to follow up unlikely to introduce bias, follow up rate ≥ 80% ★ (c) Follow up rate < 80 % or not stated | c | b (★) | c | b (★) | c | c | b (★) | b (★) | c | b (★) |
| Summary Score (Stars) | 4/10 | 4/10 | 5/10 | 5/10 | 5/10 | 5/10 | 8/10 | 8/10 | 8/10 | 6/10 |
| Authors | Country | Local Setting (Initial and Final Date) | Sample | Children’s Age at Dental Examination | Dental Examination Criteria/Index (Calibration) | Types of Malocclusion Analyzed | Instrument and Time Interval of Feeding Habit Evaluation | Statistics (Adjusted for Confounders) | Outcomes(OR; 95% CI) or (p-value) | QualityScore |
|---|---|---|---|---|---|---|---|---|---|---|
| Davis & Bell, 1991 [16] | Canada | National database (Beginning with newborns in 1983 and the children were examined in 1988) | Initial = 670 Final = 108 | 5 years | Does not report the use of an index/criteria (NR †) | Molar relationships, crossbite, overjet, overbite, crowding, drifting | Questionnaires answered by mothers, monthly, from 1983 to 1988 | Chi-square and Kruskal-Wallis (no) | No significant association between malocclusion and feeding method (p > 0.05) except for overjet which was associated with exclusive bottle feeding (RR ‡‡ = 6.62; p = 0.006) | 4 (10) |
| Karjalainen et al., 1999 [17] | Finland | Recruited from a prospective baby trial (NR †) | Initial = 179 Final = 148 | 3 years | Does not report the use of an index/criteria (NR †) | Posterior crossbite, anterior open bite, overjet | Parent interviews recorded 10 times at 1–3 month intervals until the child reached 3 years of age | Chi-square tests and covariance analysis (no) | Children breastfed for 4.7 months had greater frequency of posterior crossbite than children breastfed for 7.6 months (p < 0.01). Breastfeeding was not associated with overjet or anterior open bite (p > 0.05) | 4 (10) |
| Warren & Bishara, 2002 [12] * | USA | Recruited from hospitals (began with newborns in 1992–1995 and the children were examined at 4.5–5 years of age) | Initial = 700 Final = 372 | 4.5–5 years | Study models evaluated using Angle classification (NR †) | Primary canine relationship, anterior and posterior crossbite, anterior open bite, overjet, overbite | Questionnaires answered by mothers at 3, 6, 9, 12, 16, 20 and 24 months of age and yearly thereafter | ANOVA(no) | No significant association between malocclusion and duration of breastfeeding (p ≥ 0.05) | 5 (10) |
| Viggiano et al., 2004 [18] | Italy | Recruited from a school (began with newborns in 1993–1995 and the children were examined in 1998) | Initial = 1130 Final = 1099 | 3–5 years | Does not report the use of an index/criteria (NR †) | Molar relationships, posterior crossbite, anterior open bite | Structured questionnaire. The data was collected only once | Logistic regression(NNSH ‡) | Bottle feeding associated with crossbite (OR: 2.54; 95% CI: 1.66–4.03), but not with open bite (OR: 0.93; 95% CI: 0.65, 1.33) or malocclusion (OR: 1.28; 95% CI: 0.99, 1.66) | 5 (10) |
| Bishara et al., 2006 [19] * | USA | Recruited from hospitals (began with newborns in 1992–1995 and the children were examined at 4.5–5 years of age) | Initial = 547 Final = 372 | 4.5–5 years | Study models evaluated using Angle classification (NR†) | Molar relationships, posterior crossbite, overjet, overbite, anterior open bite | Questionnaires answered by mothers at 3, 6, 9, 12, 16, 20 and 24 months and yearly thereafter | McNemar test (no) | No significant difference between children breastfed for 6–12 months without NNSH and children who were not breastfed but had NNSH <12 months (p > 0.05) | 5 (10) |
| Vázquez-Nava et al., 2006 [7] | Mexico | NR † | Initial = NR † Final = 1160 | 4–5 years | Does not report the use of an index/criteria (NR †) | Anterior open bite, posterior cross bite | Validated questionnaire. The data was collected only once | Qui-square and logistic regression (NNSH ‡, allergic rhinitis) | Bottle feeding associated with malocclusion (OR: 1.37; 95% CI: 1.06, 1.78) and crossbite (OR: 1.95; 95% CI: 1.07, 3.54). Bottle feeding was not associated with open bite (OR: 1.27; 95% CI: 0.98, 1.64) | 5 (10) |
| Peres et al., 2007 [13] * | Brazil | Recruited from hospitals (began with newborns in 1993 and the children were examined in 1999) | Initial = 400 Final = 359 | 6 years | Foster and Hamilton criteria (Kappa ≥ 0.85) | Open bite | Interviews with mothers at 1, 3, 6 and 12 months (1993) and in the child’s fifth year of life | Multivariate analysis (NNSH ‡: pacifier/finger sucking, socioeconomic indicators, maternal characteristics) | Open bite was not associated with bottle feeding at 5 years of age in the adjusted analysis (p > 0.05). Open bite was associated with breastfeeding <9 months (OR: 2.7; 95% CI: 1.4,6.8, adjusted for dental caries, NNSH‡ , maternal schooling and maternal behavioral characteristics) | 8 (10) |
| Peres et al., 2007 [14] * | Brazil | Recruited from hospitals (began with newborns in 1993 and the children were examined in 1999) | Initial = 400 Final = 359 | 6 years | Foster and Hamilton criteria(Kappa ≥ 0.85) | Anterior open bite, posterior crossbite | Interviews with mothers at 1, 3, 6 and 12 months (1993) and in the child’s fifth year of life | Multivariate analysis, Poisson regression (Time of breastfeeding and NNSH ‡‡: pacifier/finger sucking, gender, maternal schooling) | Posterior crossbite was associated with duration of breastfeeding (p = 0.036). Posterior crossbite was associated with duration of breastfeeding even after adjustment for the time of NNSH ‡ (OR = 7.6; 95% CI: 1.5, 39.5). Anterior open bite was associated with breastfeeding <9 months (p = 0.004). After adjustment for the use of pacifier, breastfeeding duration lost significance (OR = 1.2; 95% CI: 0.8, 1.7). | 8 (10) |
| Caramez da Silva et al., 2012 [20] | Brazil | Recruited from a hospital (began with newborns in 1993 and the children were examined between 3–5 years-old | Initial = 220 Final = 153 | 3–5 years | Foster and Hamilton criteria (NR †) | Distocclusion (Class II) | Interview with mothers at 7, 30, 60, 120, 180 days of life and between 3–5 years | Chi-square and Poisson regression (adjusted for duration of pacifier use and bottle-feeding) | Breastfeeding for 12 months or longer protects against canine Class II relation (PR ††: 0.44; 95% CI: 0.23, 0.82) | 8 (10) |
| Moimaz et al., 2014 [21] | Brazil | Recruited from a program of prenatal care (began with newborns in November 2008 and the children were examined in May 2010) | Initial = 120 Final = 80 | 30 months | Own criteria(Kappa = 0.92) | Posterior crossbite, anterior crossbite, open bite | Interviews (semi-structured questionnaires) with mothers at 12, 18 and 30 months | Chi-square test and Fisher’s exact test (no) | Posterior crossbite was associated with bottle feeding at 12 and 30 months (p = 0.02 and p = 0.04, respectively). Overjet > 3mm was associated with breastfeeding at 12 and 18 months (p < 0.0001) and at 30 months (p = 0.01). Open bite was associated with breastfeeding at 12, 18 and 30 months (p < 0.001, p = 0.001 and p = 0.01, respectively) | 6 (10) |
2.3. Assessment of Methodological Quality
2.4. Data Synthesis
3. Results
3.1. Characteristics of Studies
3.2. Qualitative Analysis
3.2.1. Type of Feeding Habit and Type of Malocclusion
3.2.2. Duration of Breastfeeding and Malocclusion
3.3. Quality Assessment
4. Discussion
4.1. Assessment of Bias
4.2. Assessment of Quality
4.3. Strength of Evidence
| Criteria | Definitions | Causal Relationship between Bottle Feeding/Breastfeeding and Malocclusion |
|---|---|---|
| Strength | How strong is the association between the cause and the effect? |
|
| Consistency | The association is consistent when results are replicated in studies in different settings using different methods |
|
| Specificity | The cause leads to a single effect. The more specific an association between a factor and an effect is, the bigger the probability of a causal relationship |
|
| Temporality | The cause precedes the effect |
|
| Biological gradient | Also known as dose response. Greater exposure should generally lead to greater risk of the disease/ effect |
|
| Plausibility | The effect must have biologic plausibility |
|
| Coherence | Coherence between epidemiological and laboratory findings increases the likelihood of an effect |
|
| Experimental evidence | Experimental or semi-experimental evidence exists to support the causation hypothesis |
|
| Analogy | The effect of similar factors may be considered |
|
5. Conclusions
Supplementary Files
Supplementary File 1Acknowledgements
Author Contributions
Conflicts of Interest
References
- WHO. Exclusive Breastfeeding for Six Months Best for Babies Everywhere. Available online: http://www.who.int/mediacentre/news/statements/2011/breastfeeding_20110115/en/ (accessed on 3 November 2014).
- Kramer, M.S.; Kakuma, R. Optimal duration of exclusive breastfeeding. Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012, 8. [Google Scholar] [CrossRef]
- Corruccini, R.S.; Whitley, L.D. Occlusal variation in a rural Kentucky community. Amer. J. Orthod. 1981, 79, 250–262. [Google Scholar] [CrossRef]
- Palmer, B. The influence of breastfeeding on the development of the oral cavity: A commentary. J. Hum. Lact. 1998, 14, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Dimberg, L.; Arnrup, K.; Bondemark, L. The impact of malocclusion on the quality of life among children and adolescents: A systematic review of quantitative studies. Eur. J. Orthod. 2014. [Google Scholar] [CrossRef]
- Aznar, T.; Galan, A.F.; Marín, I.; Domínquez, A. Dental arch diameters and relationships to oral habits. Angle Orthodont. 2006, 76, 441–445. [Google Scholar] [PubMed]
- Vázquez-Nava, F.; Quezada-Castillo, J.A.; Oviedo-Treviño, S.; Saldivar-González, A.H.; Sánchez-Nuncio, H.R.; Beltrán-Guzmán, F.J.; Vázquez-Rodríguez, E.M.; Vázquez Rodríguez, C.F. Association between allergic rhinitis, bottle feeding, non-nutritive sucking habits, and malocclusion in the primary dentition. Arch. Dis. Child. 2006, 91, 836–840. [Google Scholar] [CrossRef] [PubMed]
- Melink, S.; Vagner, M.V.; Hocevar-Boltezar, I.; Ovsenik, M. Posterior crossbite in the deciduous dentition period, its relation with sucking habits, irregular orofacial functions, and otolaryngological findings. Amer. J. Orthod. Dent. Orthop. 2010, 138, 32–40. [Google Scholar] [CrossRef]
- Ogaard, B.; Larsson, E.; Lindsten, R. The effect of sucking habits, cohort, sex, intercanine arch widths, and breast or bottle feeding on posterior crossbite in Norwegian and Swedish 3-year-old children. Amer. J. Orthod. Dent. Orthop. 1994, 106, 161–166. [Google Scholar] [CrossRef]
- Romero, C.C.; Scavone-Junior, H.; Garib, D.G.; Cotrim-Ferreira, F.A.; Ferreira, R.I. Breastfeeding and non-nutritive sucking patterns related to the prevalence of anterior open bite in primary dentition. J. Appl. Oral Sci. 2011, 19, 161–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luz, C.L.; Garib, D.G.; Arouca, R. Association between breastfeeding duration and mandibular retrusion: A cross-sectional study of children in the mixed dentition. Amer. J. Orthod. Dent. Orthop. 2006, 130, 531–534. [Google Scholar] [CrossRef]
- Warren, J.J.; Bishara, S.E. Duration of nutritive and nonnutritive sucking behaviors and their effects on the dental arches in the primary dentition. Amer. J. Orthod. Dent. Orthop. 2002, 121, 347–356. [Google Scholar] [CrossRef]
- Peres, K.G.; Barros, A.J.; Peres, M.A.; Victora, C.G. Effects of breastfeeding and sucking habits on malocclusion in a birth cohort study. Rev. Saude Publ. 2007, 41, 343–350. [Google Scholar] [CrossRef]
- Peres, K.G.; de Oliveira Latorre Mdo, R.; Sheiham, A.; Peres, M.A.; Victora, C.G.; Barros, F.C. Social and biological early life influences on the prevalence of open bite in Brazilian 6-year-olds. Int. J. Paediatr. Dent. 2007, 17, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.M.; Scavone, H., Jr.; Ferreira, R.I.; Garib, D.G. Relationship between breastfeeding duration and prevalence of posterior crossbite in the deciduous dentition. Amer. J. Orthod. Dent. Orthop. 2010, 137, 54–58. [Google Scholar] [CrossRef]
- Davis, D.W.; Bell, P.A. Infant feeding practices and occlusal outcomes: A longitudinal study. J. Can. Dent. Assn. 1991, 57, 593–594. [Google Scholar]
- Karjalainen, S.; Rönning, O.; Lapinleimu, H.; Simell, O. Association between early weaning, non-nutritive sucking habits and occlusal anomalies in 3-year-old Finnish children. Int. J. Paediatr. Dent. 1999, 9, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Viggiano, D.; Fasano, D.; Monaco, G.; Strohmenger, L. Breast feeding, bottle feeding, and non-nutritive sucking: Effects on occlusion in deciduous dentition. Arch. Dis. Child. 2004, 89, 1121–1123. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Warren, J.J.; Broffitt, B.; Levy, S.M. Changes in the prevalence of nonnutritive sucking patterns in the first 8 years of life. Amer. J. Orthod. Dent. Orthop. 2006, 130, 31–36. [Google Scholar] [CrossRef]
- Caramez da Silva, F.; Justo Giugliani, E.R.; Capsi Pires, S. Duration of breastfeeding and distoclusion in the deciduous dentition. Breastfeed. Med. 2012, 7, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Moimaz, S.A.; Garbin, A.J.; Lima, A.M.; Lolli, L.F.; Saliba, O.; Garbin, C.A. Longitudinal study of habits leading to malocclusion development in childhood. BMC Oral Health 2014, 14, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Available online: www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 3 November 2014).
- Biljana, M.; Jelena, M.; Branislav, J.; Milorad, R. Bias in meta-analysis and funnel plot asymmetry. Stud. Health Technol. Inform. 1999, 68, 323–328. [Google Scholar] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in metaanalysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.B. The environment and disease: Association or causation? Proc. R Soc. Med. 1965, 58, 295–300. [Google Scholar] [PubMed]
- American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): Classifications, consequences, and preventive strategies. Pediatr. Dent. 2008, 30, 40–43. [Google Scholar]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hermont, A.P.; Martins, C.C.; Zina, L.G.; Auad, S.M.; Paiva, S.M.; Pordeus, I.A. Breastfeeding, Bottle Feeding Practices and Malocclusion in the Primary Dentition: A Systematic Review of Cohort Studies. Int. J. Environ. Res. Public Health 2015, 12, 3133-3151. https://doi.org/10.3390/ijerph120303133
Hermont AP, Martins CC, Zina LG, Auad SM, Paiva SM, Pordeus IA. Breastfeeding, Bottle Feeding Practices and Malocclusion in the Primary Dentition: A Systematic Review of Cohort Studies. International Journal of Environmental Research and Public Health. 2015; 12(3):3133-3151. https://doi.org/10.3390/ijerph120303133
Chicago/Turabian StyleHermont, Ana Paula, Carolina C. Martins, Lívia G. Zina, Sheyla M. Auad, Saul M. Paiva, and Isabela A. Pordeus. 2015. "Breastfeeding, Bottle Feeding Practices and Malocclusion in the Primary Dentition: A Systematic Review of Cohort Studies" International Journal of Environmental Research and Public Health 12, no. 3: 3133-3151. https://doi.org/10.3390/ijerph120303133





