Elimination of Mother-To-Child Transmission of HIV Infection: The Drug Resource Enhancement against AIDS and Malnutrition Model
Abstract
:1. Introduction
2. Methods (Implementation of the DREAM eMTCT Program in Mozambique)

3. Results (Description and Outcomes following DREAM Program Implementation in Mozambique)



4. Discussion: Challenges and Potential Solutions
Cost-Effectiveness of the DREAM Program
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Plano Estrategico Nacional de Resposta ao HIV e Sida 2010–2014—Republica de Moçambique. Available online: http://www.cncs.org.mz/.../PlanoEstrategicoNacional_PENIII_2010junho.pdf (acessed on 5 April 2015).
- Joint United Nations Program on HIV and AIDS—UNAIDS. UNAIDS Report on the Global AIDS Epidemic 2013. Available online: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf (accessed on 2 April 2015).
- UNAIDS World AIDS Day Report 2011. Available online: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/JC2216_WorldAIDSday_report_2011_en.pdf (accessed on 5 April 2015).
- WHO—EMTCT Strategic Vision 2010/2015 Preventing Mother-to-Child Transmission of HIV to Reach the UNGASS and Millennium Development Goals, February 2010. Available online: http://www.who.int/hiv/pub/mtct/strategic_vision/en/index.html (accessed on 5 April 2015).
- UNICEF—Mozambique. HIV/AIDS in Children. Available online: http://www.unicef.org/mozambique/hiv_aids_2968.html (accessed on 6 April 2015).
- Bulterys, M.; Ellington, S.; Kourtis, A.P. HIV-1 and breastfeeding: Biology of transmission and advances in prevention. Clin. Perinatol. 2010, 37, 807–824. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.F.; Stinson, K.; Newell, M.L.; Bland, R.M.; Moultrie, H.M.; Davies, M.; Rehle, T.M.; Dorrington, R.E. The contribution of maternal HIV seroconversion during late pregnancy and breastfeeding to mother-to-child transmission of HIV. J. Acquir. Immune Defic. Syndr. 2011, 59, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Newell, M.L.; Coovadia, H.; Cortina-Borja, M.; Rollins, N.; Gaillard, P.; Dabis, F. Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: A pooled analysis. Lancet 2004, 364, 1236–1243. [Google Scholar] [CrossRef]
- Raguenaud, M.E.; Isaakidis, P.; Zachariah, R.; Te, V.; Soeung, S.; Akao, K.; Kumar, V. Excellent outcomes among HIV+ children on ART, but unacceptably high pre-ART mortality and losses to follow-up: A cohort study from Cambodia. BMC Pediatr. 2009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brady, M.T.; Oleske, J.M.; Williams, P.L.; Elgie, C.; Mofenson, L.M.; Dankner, W.M.; van Dyke, R.B. Declines in mortality rates and changes in causes of death in HIV-1-infected children during the HAART era. J. Acquir. Immune Defic. Syndr. 2010, 53, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Violari, A.; Cotton, M.F.; Gibb, D.M.; Babiker, A.G.; Steyn, J.; Madhi, S.A.; Jean-Philippe, P.; McIntyre, J.A. Early antiretroviral therapy and mortality among HIV-infected infants. N. Engl. J. Med. 2008, 359, 2233–2244. [Google Scholar] [CrossRef] [PubMed]
- United Nations General Assembly Special Session on HIV and AIDS—Progress Report 2008/2009—Mozambique, 2010. Available online: http://www.unaids.org/en/dataanalysis/monitoringcountryprogress/2010progressreportssubmittedbycountries/mozambique_2010_country_progress_report_en.pdf (accessed on 3 April 2015).
- UNAIDS—WHO, 2011. WHO—UNAIDS Technical Guidance Note for Global Fund HIV Proposals—EMTCT–2011. Available online: http://www.unaids.org/en/media/unaids/contentassets/documents/programmes/programmeeffectivenessandcountrysupportdepartment/gfresourcekit/20110927_Technical_brief_EMTCT.pdf (accessed on 4 April 2015).
- De Schacht, C.; Hoffman, H.J.; Mabunda, N.; Lucas, C.; Alons, C.L.; Madonela, A.; Vubil, A.; Ferreira, O.C., Jr.; Calu, N.; Santos, I.S.; et al. High rates of HIV seroconversion in pregnant women and low reported levels of HIV testing among male partners in Southern Mozambique: Results from a mixed methods study. PLoS ONE 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazzi, M.C.; Liotta, G.; Nielsen-Saines, K.; Haswell, J.; Magid, N.A.; Buonomo, E.; Scarcella, P.; Altan, A.M.D.; Mancinelli, S.; Palombi, L. Extended antenatal antiretroviral use correlates with improved infant outcomes throughout the first year of life. AIDS 2010, 24, 2819–2826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazzi, M.C.; Palombi, L.; Nielsen-Saines, K.; Haswell, J.; Zimba, I.; Magid, N.A.; Buonomo, E.; Scarcella, P.; Ceffa, S.; Paturzo, G.; et al. Extended antenatal use of triple antiretroviral therapy in resource-limited settings for prevention of HIV-1 mother-to-child transmission correlates with favorable pregnancy outcomes. AIDS 2011, 25, 1611–1618. [Google Scholar] [CrossRef] [PubMed]
- Marazzi, M.C.; Nielsen-Saines, K.; Buonomo, E.; Scarcella, P.; Germano, P.; Majid, N.A.; Zimba, I.; Ceffa, S.; Palombi, L. Increased infant human immunodeficiency virus type one free survival at one year of age in SubSaharan Africa with maternal use of highly active antiretroviral therapy during breastfeeding. Pediatr. Infect. Dis. J. 2009, 28, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Palombi, L.; Marazzi, M.C.; Voetberg, A.; Magid, N.A. The DREAM Program Prevention of Mother-To-Child Transmission Team. Treatment acceleration program and the experience of the DREAM program in prevention of mother-to-child transmission of HIV. AIDS 2007, 21, S65–S71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazzi, C.M.; Germano, P.; Giuseppe, L.; Guidotti, G.; Loureiro, S.; da Cruz Gomes, A.; valls Blazquez, M.C.; Narciso, P.; Perno, C.F.; Mancinelli, S.; et al. Implementing antiretroviral triple therapy to prevent HIV mother-to-child transmission: A public health approach in resource-limited settings. Eur. J. Pediatr. 2007, 166, 1305–1307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO Africa. Prevention of Mother to Child Transmission. Mozambique. Available online: http://www.afro.who.int/en/mozambique/country-programmes/mother-and-child-health/prevention-of-mother-to-child-transmission.html (accessed on 29 September 2015).
- Marazzi, M.C.; Bartolo, M.; Emberti Gialloreti, L.; Germano, P.; Guidotti, G.; Liotta, G.; Magnano San Lio, M.; Mancinelli, S.; Modolo, M.A.; Narciso, P.; et al. Improving adherence to highly active anti-retroviral therapy in Africa: The DREAM programme in Mozambique. Health Educ. Res. 2006, 21, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Magnano San Lio, M.; Mancinelli, S.; Palombi, L.; Buonomo, E.; Doro Altan, A.; Germano, P.; Magid, N.A.; Pesaresi, A.; Renzi, E.; Scarcella, P.; et al. The DREAM model’s effectiveness in health promotion of AIDS patients in Africa. Health Promot. Int. 2009, 24, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Palombi, L.; Dorrucci, M.; Zimba, I.; Scarcella, P.; Mancinelli, S.; Buonomo, E.; Guidotti, G.; Marazzi, M.C.; Rezza, G. Immunologic response to highly active antiretroviral therapy and mortality reduction in a cohort of human immunodeficiency virus-positive persons in Mozambique. Am. J. Trop. Med. Hyg. 2010, 83, 1128–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazzi, M.C.; Liotta, G.; Germano, P.; Guidotti, G.; Doro Altan, A.; Ceffa, S.; Magnano San Lio, M.; Nielsen-Saines, K.; Palombi, L. Excessive early mortality in the first year of treatment in HIV type 1-infected patients initiating antiretroviral therapy in resource-limited settings. AIDS Res. Hum. Retrovir. 2008, 24, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Palombi, L.; Marazzi, M.C.; Guidotti, G.; Germano, P.; Buonomo, E.; Scarcella, P.; Doro Altan, A.; Zimba, I.D.V.M.; Manano San Lio, M.; de Luca, A.; et al. Incidence and predictors of death, retention, and switch to second line regimens in antiretroviral-treated patients in sub-Saharan African sites with comprehensive monitoring availability. Clin. Infect. Dis. 2009, 48, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Bellocchi, M.C.; Forbici, F.; Palombi, L.; Gori, C.; Coelho, E.; Svicher, V.; D’Arrigo, R.; Emberti-Gialloreti, L.; Ceffa, S.; Erba, F.; et al. Subtype analysis and mutations to antiviral drugs in HIV-1-infected patients from Mozambique before initiation of antiretroviral therapy: Results from the DREAM programme. J. Med. Virol. 2005, 76, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Liotta, G.; Mancinelli, S.; Gennaro, E.; Scarcella, P.; Nielsen-Saines, K.; Magid, N.A. Is Highly Active Antiretroviral Therapy (HAART) in Pregnancy Protective against Maternal Mortality? Results from a Large DREAM Cohort in Malawi and Mozambique. In Proceedings of the 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention, Rome, Italy, 17–20 July 2011.
- UNICEF. UNICEF Millenium Development Goals-5: Improve Maternal Health, 2010. Available online: http://www.unicef.org/mdg/maternal.html (accessed on 6 April 2015).
- Palombi, L.; Luhanga, R.; Galluzzo, C.; Andreotti, M.; Liotta, G.; Ceffa, S.; Haswell, J.; Marazzi, M.C.; Vella, S.; Giuliano, M. Limited risk of drug resistance after discontinuation of antiretroviral prophylaxis for the prevention of breastfeeding transmission of HIV. J. Acquir. Immune Defic. Syndr. 2011, 57, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Marazzi, M.C.; Palombi, L.; Doro Altan, A.M.; Liotta, G.; Bernava, M.; Majid, M.A.; Buonomo, E.; Scarcella, P.; Germano, P.; Nielsen-Saines, K. Maternal Outcomes Following Interruption of Highly Active Antiretroviral Therapy (HAART) for Prevention of Mother-to-Child Transmission (EMTCT): A DREAM Program Prospective Cohort from Sub Saharan Africa. In Proceedings of the 16th Conference on Retroviruses and Opportunistic Infections, Montreal, Canada, 8–11 February 2009.
- Liotta, G.; Mancinelli, S.; Nielsen-Saines, K.; Gennaro, E.; Scarcella, P.; Magid, N.A.; Germano, P.; Jere, H.; Guidotti, G.; Buonomo, E.; et al. Reduction of maternal mortality with Highly Active Antiretroviral Therapy in a large cohort of HIV-Infected pregnant women in Malawi and Mozambique. PLoS ONE 2013. [Google Scholar] [CrossRef]
- WHO UNICEF, UNFPA, World Bank (2012) Trends in Maternal Mortality: 1990–2010. WHO, UNICEF, UNFPA, and the World Bank Estimates. Available online: http://www.who.int/reproductivehealth/publications/monitoring/9789241503631/en/index.html (accessed on 29 September 2015).
- Liotta, G.; Bernava, G.; Nucita, A.; Giglio, P.; Buonomo, E.; Scarcella, P.; Ceffa, S.; Nielsen-Saines, K.; Palombi, L.; Marazzi, M.C. A Model for Patient Evaluation which Expedites Triple ART Initiation and Significantly Reduces Attrition Rates: Odessy® (Original DEcision Support SYstem) Data from a Drug Resource Enhancement Against AIDS and Malnutrition Cohort. In Proceedings of the 19th Conference on Retroviruses and Opportunistic Infections, Seattle, WA, USA, 5–8 March 2012.
- World Health Organization. Rapid Advice: Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants. November 2009. Available online: http://www.who.int/hiv/pub/mtct/advice/en/ (accessed on 3 April 2015).
- Scarcella, P.; Buonomo, E.; Zimba, I.; Doro Altan, A.M.; Germano, P.; Palombi, L.; Marazzi, M.C. The impact of integrating food supplementation, nutritional education and HAART (Highly Active Antiretroviral Therapy) on the nutritional status of patients living with HIV/AIDS in Mozambique: Results from the DREAM Programme. Ig. Sanita Pubblica 2011, 67, 41–52. [Google Scholar]
- Marazzi, M.C.; Germano, P.; Liotta, G.; Buonomo, E.; Guidotti, G.; Palombi, L. Pediatric highly active antiretroviral therapy in Mozambique: An integrated model of care. Minerva Pediatr. 2006, 58, 483–490. [Google Scholar] [PubMed]
- Buonomo, E.; de Luca, S.; Tembo, D.; Scarcella, P.; Germano, P.; Doro Altan, A.M.; Palombi, L.; Liotta, G.; Nielsen-Saines, K.; Erba, F.; et al. Nutritional rehabilitation of HIV-exposed infants in Malawi: Results from the drug resource Enhancement against AIDS and Malnutrition program. Int. J. Environ. Res. Pub. Health 2012, 9, 421–434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
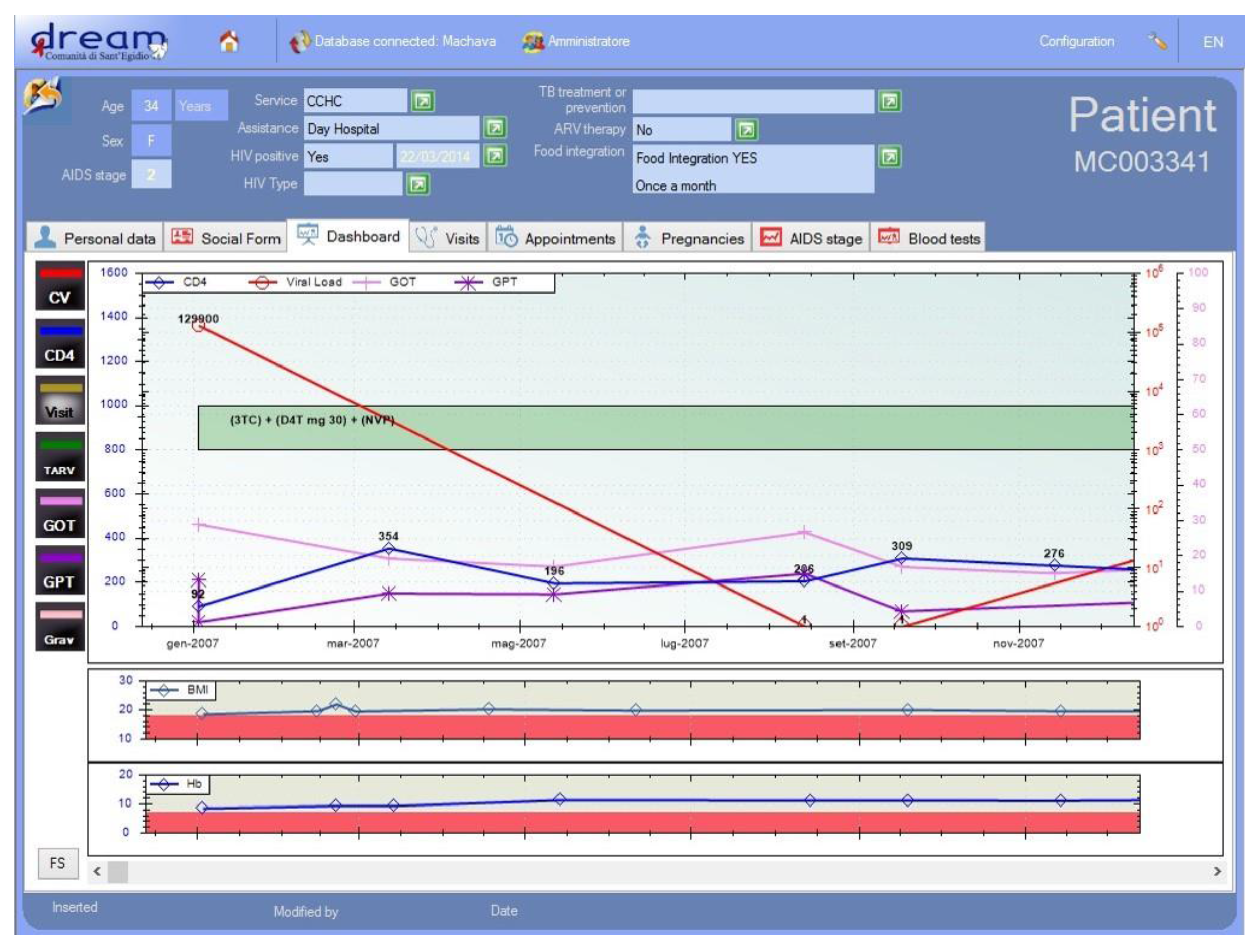
- Nucita, A.; Bernava, G.M.; Bartolo, M.; Di Pane Masi, F.; Giglio, P.; Peroni, M.; Pizzimenti, G.; Palombi, L. A global approach to the management of EMR (electronic medical records) of patients with HIV/AIDS in sub-Saharan Africa: The experience of DREAM software. BMC Med. Inf. Decis. Mak. 2009. [Google Scholar] [CrossRef] [PubMed]
- Nielsen-Saines, K.; Melo, M.; Varella, I.; Fonseca, R.; Lira, R.; Turella, M.L.; Canti, I.; Campello, C.; Moreira, A.M.; Santos, B.R. Primary HIV-1 infection during pregnancy: High rate of HIV-1 MTCT in a cohort of patients in southern Brazil. Retrovirology 2008, 5. [Google Scholar] [CrossRef]
- Orlando, S.; Marazzi, M.C.; Mancinelli, S.; Liotta, G.; Ceffa, S.; Giglio, P.; Alumando, E.; Ziegler, I.; Shawa, M.; Palombi, L. Cost-effectiveness of using HAART in prevention of Mother-To-Child transmission in the DREAM programme. J. Acquir. Immune Defic. Syndr. 2010, 55, 631–634. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liotta, G.; Marazzi, M.C.; Mothibi, K.E.; Zimba, I.; Amangoua, E.E.; Bonje, E.K.; Bossiky, B.N.B.; Robinson, P.A.; Scarcella, P.; Musokotwane, K.; et al. Elimination of Mother-To-Child Transmission of HIV Infection: The Drug Resource Enhancement against AIDS and Malnutrition Model. Int. J. Environ. Res. Public Health 2015, 12, 13224-13239. https://doi.org/10.3390/ijerph121013224
Liotta G, Marazzi MC, Mothibi KE, Zimba I, Amangoua EE, Bonje EK, Bossiky BNB, Robinson PA, Scarcella P, Musokotwane K, et al. Elimination of Mother-To-Child Transmission of HIV Infection: The Drug Resource Enhancement against AIDS and Malnutrition Model. International Journal of Environmental Research and Public Health. 2015; 12(10):13224-13239. https://doi.org/10.3390/ijerph121013224
Chicago/Turabian StyleLiotta, Giuseppe, Maria Cristina Marazzi, Khethimipilo E. Mothibi, Ines Zimba, Evelyne E. Amangoua, Esther K. Bonje, Bernard N. B. Bossiky, Precious A. Robinson, Paola Scarcella, Kebby Musokotwane, and et al. 2015. "Elimination of Mother-To-Child Transmission of HIV Infection: The Drug Resource Enhancement against AIDS and Malnutrition Model" International Journal of Environmental Research and Public Health 12, no. 10: 13224-13239. https://doi.org/10.3390/ijerph121013224






