Water-Borne Diseases and Extreme Weather Events in Cambodia: Review of Impacts and Implications of Climate Change
Abstract
:1. Introduction

- To synthesize the literature on the water-borne health impacts of floods, droughts and typhoons in Cambodia.
- To explore the relationship between flooding and diarrhoeal disease in Cambodian children.
2. Experimental Section
2.1. Literature Review of Extreme Weather Events (Floods, Droughts and Typhoons) and Water-Borne Health Impacts in Cambodia
2.2. Flood Events and Diarrhoeal Disease in Cambodia
| Year | Event (Month/s) | No. of provinces affected | Impacts |
|---|---|---|---|
| 1991 | Flood (August) | 10 |
|
| 1994 | Drought (June) |
| |
| Flood (July) | 6 |
| |
| 1996 | Flood (September) | 10 |
|
| 1997 | Typhoon (November) | 1 |
|
| 1997–1998 | Drought (“Late 1997–Early 1998”) |
| |
| 1999 | Flood (July–August) | 7 |
|
| Flood (November) | 6 |
| |
| 2000 | Flood (July–November) | 22 |
|
| 2001 | Drought (“Most of the year”) | 12 |
|
| Flood (August–October) | 18 |
| |
| 2002 | Drought (January–August) | 24 |
|
| Flood (August) | 6 |
| |
| 2004–2005 | Drought (October 2004–April 2005) | 14 |
|
| 2006 | Tropical Storm Prapiroon, Flood (August–September) | 9 |
|
| 2007 | Flood (June) | 1 | |
| Tropical Storm Pabuk, Flood (August) | 8 |
| |
| 2008 | Flood (August) | 1 | |
| Drought (September) | 1 | ||
| 2009 | Drought (August) | 7 |
|
| Typhoon Ketsana, Flood (September–October) | 14 |
| |
| Typhoon Mirinae (November) | 1 |
| |
| 2009–2010 | Drought (November 2009–July 2010) | ||
| Flood (October–November) | 8 |
| |
| 2011 | Flood (August–November) | 18 |
|
| 2012 | Tropical Storm Pakhar (March–April) | 1 |
|
| Drought (July–August) | 14 |
| |
| Flood (September–October) | 8 |
| |
| Tropical Storm Gaemi (October) | 7 | ||
| 2013 | Flood (August) | 4 |
|
| Flood, Typhoon Usagi, Tropical Storm Krosa (September–October) | 21 |
|
3. Results
3.1. Extreme Weather Events (Floods, Droughts and Typhoons) in Cambodia
3.2. Review of Water-Borne Diseases and Extreme Weather Events in Cambodia
Other Water-Related Diseases
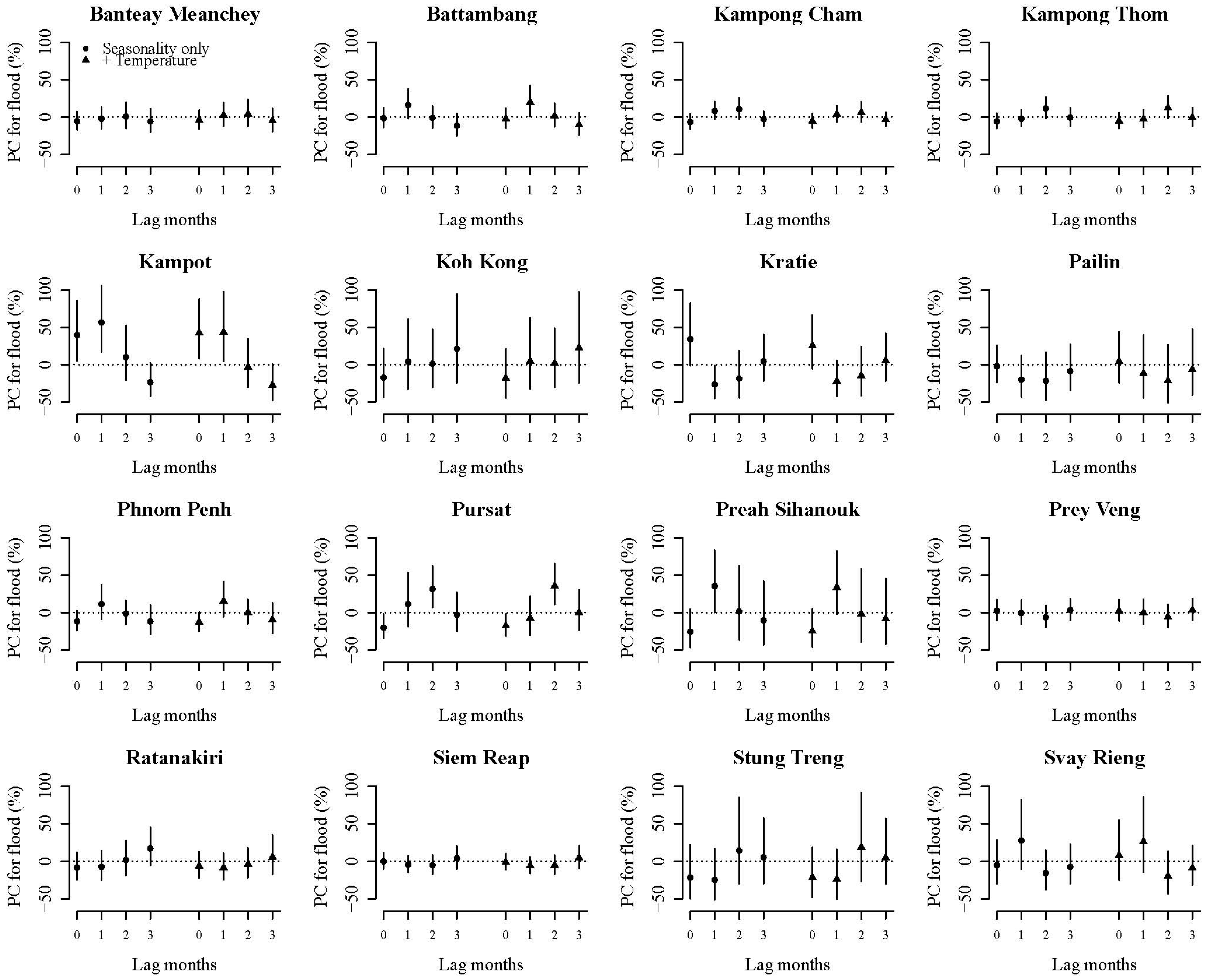
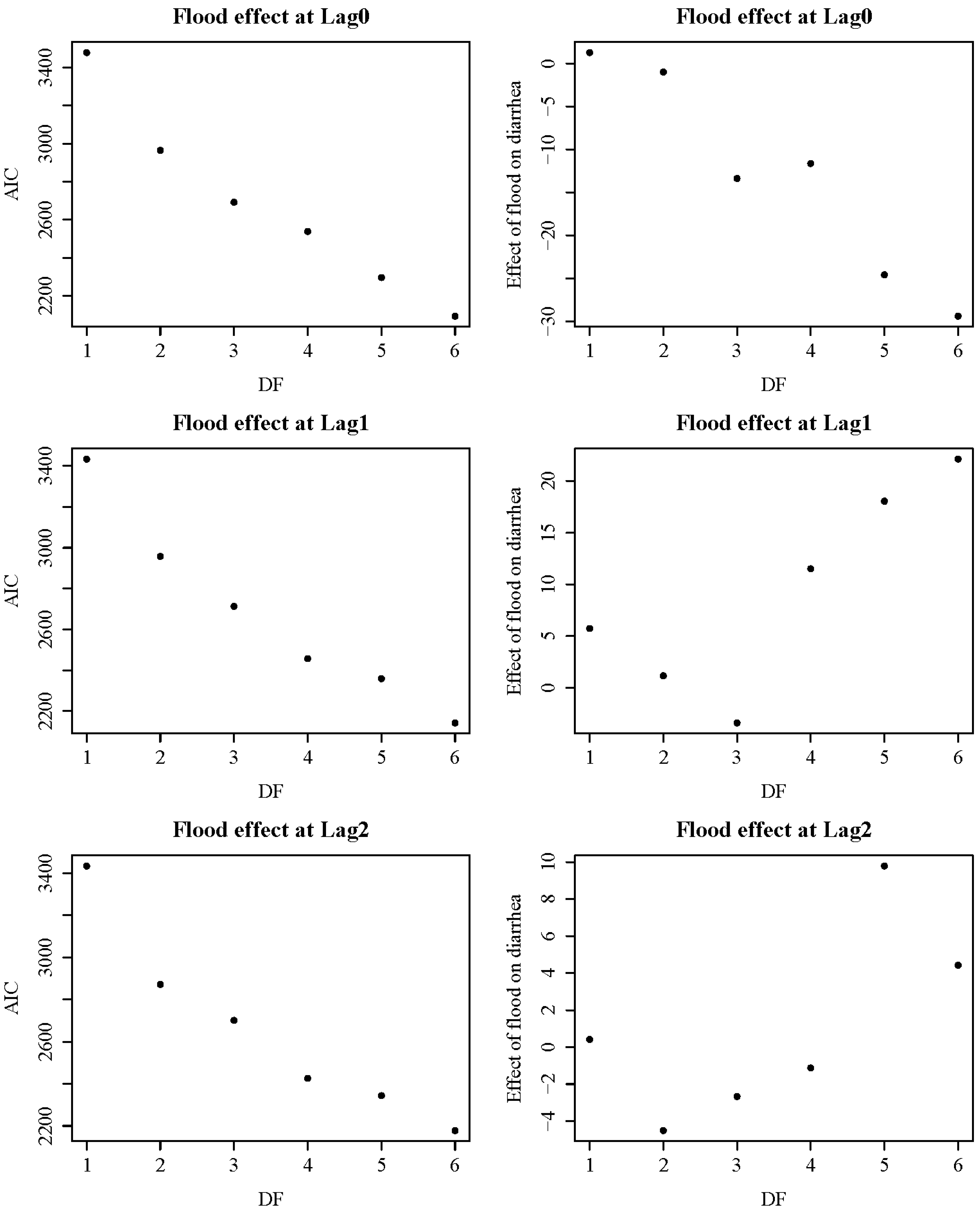
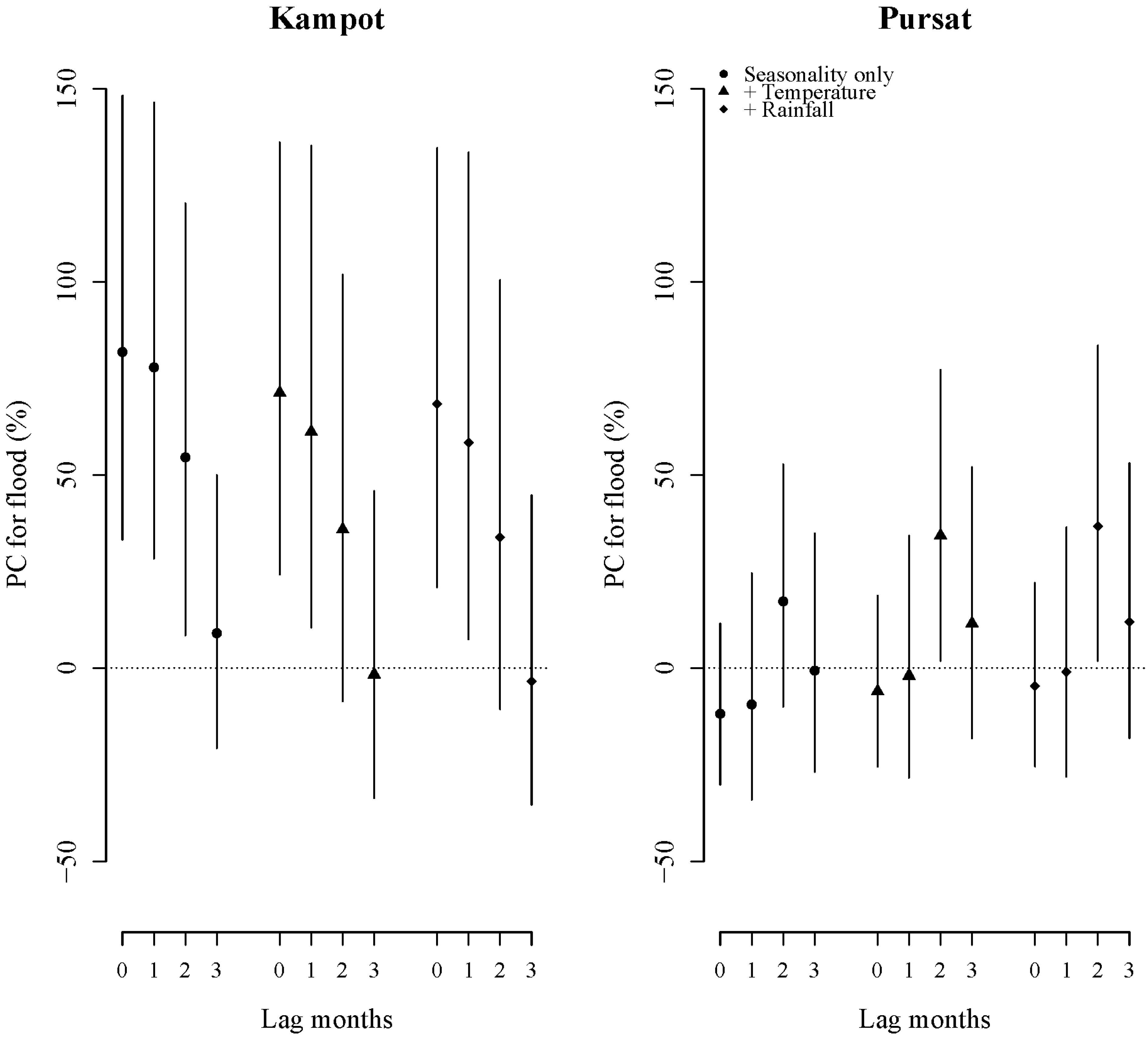
3.3. Floods and Diarrhoeal Disease in Cambodian Children
| Provinces | Study Period | Mean Monthly No. of Diarrhoea Cases in Children up to 14 Years a | No. of Months Affected by Flooding b | Rainfall c (mm) | Mean Temperature c (ºC) | ||
|---|---|---|---|---|---|---|---|
| Non-flood | Flood | Median (IQR) | Max | ||||
| Banteay Meanchey | 2001–2012 | 828 | 871 | 13 | 88.5 (149.3) | 452.2 | 28.4 |
| Battambang | 2001–2012 | 747 | 845 | 14 | 82.6 (142.8) | 353.3 | 28.3 |
| Kampong Thom | 2001–2012 | 620 | 569 | 15 | 99.4 (180.3) | 497.2 | 27.6 |
| Kampot | 2001–2012 | 243 | 237 | 11 | 131.4 (209.1) | 629.1 | 28.1 |
| Koh Kong | 2001–2012 | 101 | 90 | 6 | 197.5 (354.4) | 1600.8 | 27.7 |
| Kratie | 2001–2012 | 267 | 380 | 10 | 126.7 (221.7) | 537.8 | 28.5 |
| Pailin | 2007–2012 | 135 | 109 | 6 | 106.2 (128.3) | 374.8 | 27.6 |
| Phnom Penh | 2001–2012 | 650 | 705 | 12 | 98.0 (168.1) | 410.3 | 28.9 |
| Pursat | 2001–2012 | 180 | 219 | 11 | 105.6 (165.9) | 398.6 | 28.4 |
| Prey Veng | 2001–2012 | 1719 | 1587 | 8 | 108.8 (169.0) | 544.8 | 28.3 |
| Ratanakiri | 2004–2008 | 385 | 434 | 3 | 57.6 (263.3) | 746.7 | 26.8 |
| Siem Reap | 2001–2012 | 885 | 1517 | 10 | 90.5 (197.1) | 512.8 | 28.4 |
| Stung Treng | 2001–2012 | 54 | 45 | 8 | 74.5 (215.2) | 552.8 | 28.4 |
| Svay Rieng | 2001–2012 | 507 | 524 | 7 | 127.5 (211.1) | 499.1 | 28.2 |
| Kampong Cham | 2001–2012 | 2319 | 1990 | 10 | 80.5 (101.0) | 170.0 | 28.2 |
| Preah Sihanouk | 2001–2012 | 152 | 135 | 3 | 86.5 (81.5) | 182.0 | 28.0 |
4. Discussion
4.1. Key Findings
4.2. Vulnerabilities of the Cambodian Population

4.3. Limitations
4.4. Future Considerations and Opportunities
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Yusuf, A.; Francisco, H. Hotspots! Mapping Climate Change Vulnerability in Southeast Asia; Economic and Environment Program for Southeast Asia: Singapore, 2010. [Google Scholar]
- Yusuf, A.A.; Francisco, H. Climate Change Vulnerability Mapping for Southeast. Asia; EEPSEA Special and Technical Paper tp200901s1; Economy and Environment Program for Southeast Asia (EEPSEA): Singapore, 2009. [Google Scholar]
- Maplecroft. 6th Annual Climate Change and Environmental Risk Atlas. Available online: http://reliefweb.int/sites/reliefweb.int/files/resources/Climate_Change_Vulnerability_Index_%202014_Map_0.pdf (accessed on 11 October 2014).
- McSweeney, C.; New, M.; Lizcano, G. UNDP Climate Change Country Profiles: Cambodia. Available online: http://www.geog.ox.ac.uk/research/climate/projects/undp-cp/UNDP_reports/Cambodia/Cambodia.lowres.report.pdf (accessed on 1 July 2014).
- Kazama, S.; Aizawa, T.; Watanabe, T.; Ranjan, P.; Gunawardhana, L.; Amano, A. A quantitative risk assessment of waterborne infectious disease in the inundation area of a tropical monsoon region. Sustain. Sci. 2012, 7, 45–54. [Google Scholar]
- O’Brien, N.; Seima, K.; Born, B.C.; Lavy, Y.; Piseth, E.; Phalla, P.; Touch, C.; Sarun, M.; Savuth, S. CARE: Risk Mitigation and Disaster Management Among Rural Communities in Cambodia. CARE International Cambodia: Phnom Penh, Cambodia, 2001. [Google Scholar]
- Cambodia Disaster Information Management and Database. Available online: http://www.em-dat.net/documents/bangkok06/CambodiaDisInfoMgmtDb.pdf (accessed on 11 October 2014).
- Adamson, P.; Bird, J. The Mekong, a drought-prone tropical environment? Int. J. Water Resour. Dev. 2010, 26, 579–594. [Google Scholar] [CrossRef]
- Agricultural Development and Climate Change: The Case of Cambodia; Cambodia Development Resource Institute: Phnom Penh, Cambodia, 2011.
- Oxfam Cambodia; Graduate School of Global Environmental Studies of Kyoto University. Drought Management Considerations for Climate Change Adaptation: Focus on the Mekong Region; CAMBODIA Report; Kyoto University: Kyoto, Japan, 2008, 2008. [Google Scholar]
- Chinvanno, S. Results from regional climate modelling and their future use in analysis of hydrologic impacts in Mekong River Basin. In Proceedings of the First AIACC Regional Workshop and Open Meeting for Asia-Pacific, Bangkok, Thiland, 24–27 March 2003.
- DanChurch Aid/Christian Aid. Public Perceptions of Climate Change in Cambodia; DanChurch Aid/Christian Aid: Phnom Penh, Cambodia, 2009. [Google Scholar]
- Haines, A.; Kovats, R.S.; Campbell-Lendrum, D.; Corvalan, C. Climate change and human health: Impacts, vulnerability and public health. Public Health 2006, 120, 585–596. [Google Scholar] [CrossRef]
- Murphy, T.; Irvine, K.; Sampson, M. The stress of climate change on water management in Cambodia with a focus on rice production. Climate Dev. 2013, 5, 77–92. [Google Scholar] [CrossRef]
- Climate Change and Health in Cambodia: A Vulnerability and Adaptation Assessment; Preventative Medicine Department, Cambodia Ministry of Health: Phnom Penh, Cambodia, 2011.
- DRIP-SWICCH: Developing Research and Innovative Policies Specific to the Water-related Impacts of Climate Change on Health; Cambodian Ministry of Health, World Health Organisation Cambodia: Phnom Penh, Cambodia, 2014.
- Annual Health Statistics 2012 Cambodia; Cambodian Ministry of Health, Department of Planning and Health Information Cambodia, World Health Organisation Cambodia: Phnom Penh, Cambodia, 2012.
- Progress Report 2012. Committing to Child. Survival: A Promise Renewed; UNICEF: New York, NY, USA, 2012.
- Progress on Drinking Water and Sanitation: 2014 Update; World Health Organisation, UNICEF: Geneva, Switzerland, 2014.
- Gentry-Shields, J.; Bartram, J. Human health and the water environment: Using the DPSEEA framework to identify the driving forces of disease. Sci. Total Environ. 2014, 468, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Communicable Disease Surveillance Centre, Public Health Wales. Systematic Review of Waterborne Disease Outbreaks Following Extreme Weather Events; Public Health Wales: Cardiff, UK, 2011. [Google Scholar]
- Siddique, A.K.; Baqui, A.H.; Eusof, A.; Zaman, K. 1988 floods in Bangladesh: pattern of illness and causes of death. J. Diarrhoeal. Dis. Res. 1991, 9, 310–314. [Google Scholar] [PubMed]
- ReliefWeb. Disasters: Cambodia. Available online: http://reliefweb.int/disasters?f[0]=field_country%3A48 (accessed on 11 October 2011).
- EM-DAT The OFDA/CRED International Disaster Database. Data Version: v12.07. Available online: http://www.em-dat.net/documents/bangkok06/CambodiaDisInfoMgmtDb.pdf (accessed on 11 October 2011).
- Helmers, K.; Jegillos, S. Linkages between Flood and Drought Disasters and Cambodian Rural Livelihoods and Food Security; International Federation of Red Cross and Red Crescent Societies and Cambodian Red Cross: Phnom Penh, Cambodia, 2004. [Google Scholar]
- Hastie, T.; Tibshirani, R. Generalized Additive Models; Chapman and Hall: New York, NY, USA, 1990. [Google Scholar]
- Cambodia: Floods Appeal. No. 22/2000. Situation Report No. 5. Available online: http://www.ifrc.org/docs/appeals/00/220005.pdf (accessed on 11 October 2011).
- Cambodia—Flood Season Situation Report No. 7. Available online: http://reliefweb.int/sites/reliefweb.int/files/resources/SITREP%237_181111.pdf (accessed on 11 October 2011).
- Cambodia: Disaster Situation Report 01–17 Aug 2002. Available online: http://reliefweb.int/report/cambodia/cambodia-disaster-situation-report-01–17-aug-2002 (accessed on 11 October 2011).
- Cambodia: Floods. Appeal No. 22/2000. Situation Report No. 6. Available online: http://www.ifrc.org/docs/appeals/00/220006.pdf (accessed on 11 October 2011).
- Cambodia: Floods Appeal 29/2001 Operations Update No. 1. Available online: http://reliefweb.int/report/cambodia/cambodia-floods-appeal-292001-operations-update-no-1 (accessed on 11 October 2011).
- Cambodia: Floods Humanitarian Response Forum Situation Report No. 06. Available online: http://reliefweb.int/report/cambodia/floods-humanitarian-response-forum-hrf-situation-report-no-06–08-november-2013 (accessed on 11 October 2011).
- Cambodia. Humanitarian Response Forum Situation Report No. 02. Available online: http://reliefweb.int/sites/reliefweb.int/files/resources/Cambodia_Sitrep02_08oct2013.pdf (accessed on 11 October 2011).
- Cambodia Post-Ketsana Disaster Needs Assessment. Part 1: Main Report. Available online: http://www.adpc.net/igo/category/ID617/doc/2014-jNEq2U-ADPC-Cambodia_Post-Ketsana_PDNA.pdf (accessed on 11 October 2011).
- Cambodia Post-Flood Relief and Recovery Survey; UNICEF: Phnom Penh, Cambodia, 2012.
- Keeping Drinking Water Safe From Floods; US Agency For International Development: Washington, DC, USA, 2012.
- Acuin, J.; Firestone, R.; Htay, T.T.; Khor, G.L.; Thabrany, H.; Saphonn, V.; Wibulpolprasert, S. Southeast Asia: An emerging focus for global health. Lancet 2011, 377, 534–535. [Google Scholar] [CrossRef] [PubMed]
- Torti, J. Floods in Southeast Asia: A health priority. J. Glob. Health 2012, 2. [Google Scholar] [CrossRef]
- Currie, B.J.; Jacups, S.P. Intensity of rainfall and severity of Melioidosis, Australia. Emerg. Infect. Dis. 2003, 9, 1538–1542. [Google Scholar] [CrossRef] [PubMed]
- Ivanova, S.; Herbreteau, V.; Blasdell, K.; Chaval, Y.; Buchy, P.; Guillard, B.; Morand, S. Leptospira and rodents in Cambodia: Environmental determinants of infection. Am. J. Trop. Med. Hyg. 2012, 86, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Picardeau, M.; Bertherat, E.; Jancloes, M.; Skouloudis, A.N.; Durski, K.; Hartskeerl, R.A. Rapid tests for diagnosis of leptospirosis: Current tools and emerging technologies. Diagn. Microbiol. Infect. Dis 2014, 78, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alderman, K.; Turner, L.R.; Tong, S. Floods and human health: A systematic review. Environ. Int. 2012, 47, 37–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qadri, F.; Khan, A.I.; Faruque, A.S.G.; Begum, Y.A.; Chowdhury, F.; Nair, G.B.; Salam, M.A.; Sack, D.A.; Svennerholm, A.-M. Enterotoxigenic Escherichia coli and Vibrio cholerae diarrhea, Bangladesh, 2004. Emerg. Infect. Dis. 2005, 11, 1104–1107. [Google Scholar] [CrossRef] [PubMed]
- Kondo, H.; Seo, N.; Yasuda, T.; Hasizume, M.; Koido, Y.; Ninomiya, N.; Yamamoto, Y. Post-flood infectious diseases in Mozambique. Prehosp. Disaster Med. 2002, 17, 126–133. [Google Scholar] [PubMed]
- Ahern, M.; Kovats, R.S.; Wilkinson, P.; Few, R.; Matthies, F. Global health impacts of floods: Epidemiologic evidence. Epidemiol. Rev. 2005, 27, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Dance, D.A. Melioidosis as an emerging global problem. Acta Trop. 2000, 74, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Asia. Intergovernmental Panel on Climate Change (IPCC) WGII AR5; IPCC: Geneva, Switzerland, 2014; Chapter 24. [Google Scholar]
- McCreesh, N.; Booth, M. Challenges in predicting the effects of climate change on Schistosoma mansoni and Schistosoma haematobium transmission potential. Trends Parasitol. 2013, 29, 548–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diarrhoeal Disease Fact. sheet 330; World Health Organisation: Geneva, Switzerland, 2013.
- Bank, W. Malnutrition Environment and Health; World Bank: Washington, DC, USA, 2007. [Google Scholar]
- Schwartz, B.S.; Harris, J.B.; Ryan, E.T. Diarrheal epidemics in Dhaka, Bangladesh, during three consecutive floods: 1988, 1998, and 2004. Am. J. Trop. Med. Hyg. 2006, 74, 1067–1073. [Google Scholar] [PubMed]
- Ivers, L.C.; Ryan, E.T. Infectious diseases of severe weather-related and flood-related natural disasters. Curr. Opin. Infect. Dis. 2006, 19, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Sidley, P. Floods in Southern Africa result in cholera outbreak and displacement. BMJ 2008, 336. [Google Scholar] [CrossRef]
- Meng, C.Y.; Smith, B.L.; Bodhidatta, L.; Richard, S.A.; Vansmith, K.; Thy, B.; Srijan, A.; Serichantalergs, O.; Mason, C.J. Etiology of diarrhea in young children and patterns of antibiotic resistance in Cambodia. Pediatr. Infect. Dis. J. 2011, 30, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Jutla, A.S.; Akanda, A.S.; Griffiths, J.K.; Colwell, R.; Islam, S. Warming oceans, phytoplankton, and river discharge: Implications for cholera outbreaks. Am. J. Trop. Med. Hyg. 2011, 85, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Ding, G.; Zhang, Y.; Gao, L.; Ma, W.; Li, X.; Liu, J.; Liu, Q.; Jiang, B. Quantitative analysis of burden of infectious diarrhea associated with floods in northwest of Anhui Province, China: A mixed method evaluation. PLos One 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Nahar, P.; Alamgir, F.; Collins, A.E.; Bhuiya, A. Contextualizing disaster in relation to human health in Bangladesh. Asian J. Water Environ. Pollut. 2010, 7, 55–62. [Google Scholar]
- Floods in Pakistan-Health Cluster Bulletin No 12–16 August 2010; World Health Organisation: Geneva, Switzerland, 2010.
- Cambodia: Halving Poverty by 2015? Poverty Assessment 2006 (East Asia & Pacific); The World Bank: Phnom Penh, Cambodia, 2006.
- Poverty in Cambodia—A New Approach. Redefining the Poverty Line; Royal Government of Cambodia Ministry of Planning: Phnom Penh, Cambodia, 2013.
- Chhinh, N. Climate change adaptation in agriculture in Cambodia. In Adaptation to Climate Change in Asia; Vachani, S., Usmani, J., Eds.; Edward Elgar Publishing: London, UK, 2014; pp. 163–182. [Google Scholar]
- GLAAS 2010 UN-Water Global Annual Assessment of Sanitation and Drinking-Water; World Health Organisation, UN-Water: Geneva, Switzerland, 2010.
- Liu, L.; Johnson, H.L.; Cousens, S.; Perin, J.; Scott, S.; Lawn, J.E.; Rudan, I.; Campbell, H.; Cibulskis, R.; Li, M.; et al. Global, regional, and national causes of child mortality in 2000–2010: An updated systematic analysis. Lancet 2012, 379, 2151–2161. [Google Scholar] [CrossRef] [PubMed]
- Cambodia Appeal 2002–2003. Appeal 01.31/2002. Available online: http://reliefweb.int/report/cambodia/cambodia-appeal-2002–2003–01312002 (accessed on 11 October 2011).
- Health Service Delivery Profile Cambodia 2012; World Health Organisation, Cambodian Ministry of Health: Phnom Penh, Cambodia, 2012.
- Economic Impacts of Sanitation in Southeast. Asia: Research Report 2008; The World Bank, Water and Sanitation Program in East Asia and the Pacific: Jakarta, Indonesia, 2008.
- Human health: Impacts, adaptation, and co-benefits. In Intergovernmental Panel on Climate Change (IPCC) WGII AR5; IPCC: Geneva, Switzerland, 2014; Chapter 11.
- Baqir, M.; Sobani, Z.A.; Bhamani, A.; Bham, N.S.; Abid, S.; Farook, J.; Beg, M.A. Infectious diseases in the aftermath of monsoon flooding in Pakistan. Asian Pac. J. Trop Biomed. 2012, 2, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Cann, K.F.; Thomas, D.R.; Salmon, R.L.; Wyn-Jones, A.P.; Kay, D. Extreme water-related weather events and waterborne disease. Epidemiol. Infect. 2013, 141, 671–686. [Google Scholar] [CrossRef] [PubMed]
- Water and Climate Change in the Lower Mekong Basin: Diagnosis and Recommendations for Adaptation; Water and Development Research Group: Helsinki, Finland, 2008.
- El-Fadel, M.; Ghanimeh, S.; Maroun, R.; Alameddine, I. Climate change and temperature rise: Implications on food- and water-borne diseases. Sci. Total Environ. 2012, 437, 15–21. [Google Scholar] [CrossRef] [PubMed]
Appendix

© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davies, G.I.; McIver, L.; Kim, Y.; Hashizume, M.; Iddings, S.; Chan, V. Water-Borne Diseases and Extreme Weather Events in Cambodia: Review of Impacts and Implications of Climate Change. Int. J. Environ. Res. Public Health 2015, 12, 191-213. https://doi.org/10.3390/ijerph120100191
Davies GI, McIver L, Kim Y, Hashizume M, Iddings S, Chan V. Water-Borne Diseases and Extreme Weather Events in Cambodia: Review of Impacts and Implications of Climate Change. International Journal of Environmental Research and Public Health. 2015; 12(1):191-213. https://doi.org/10.3390/ijerph120100191
Chicago/Turabian StyleDavies, Grace I., Lachlan McIver, Yoonhee Kim, Masahiro Hashizume, Steven Iddings, and Vibol Chan. 2015. "Water-Borne Diseases and Extreme Weather Events in Cambodia: Review of Impacts and Implications of Climate Change" International Journal of Environmental Research and Public Health 12, no. 1: 191-213. https://doi.org/10.3390/ijerph120100191






