Biomechanical Load of Neck and Lumbar Joints in Open-Surgery Training
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
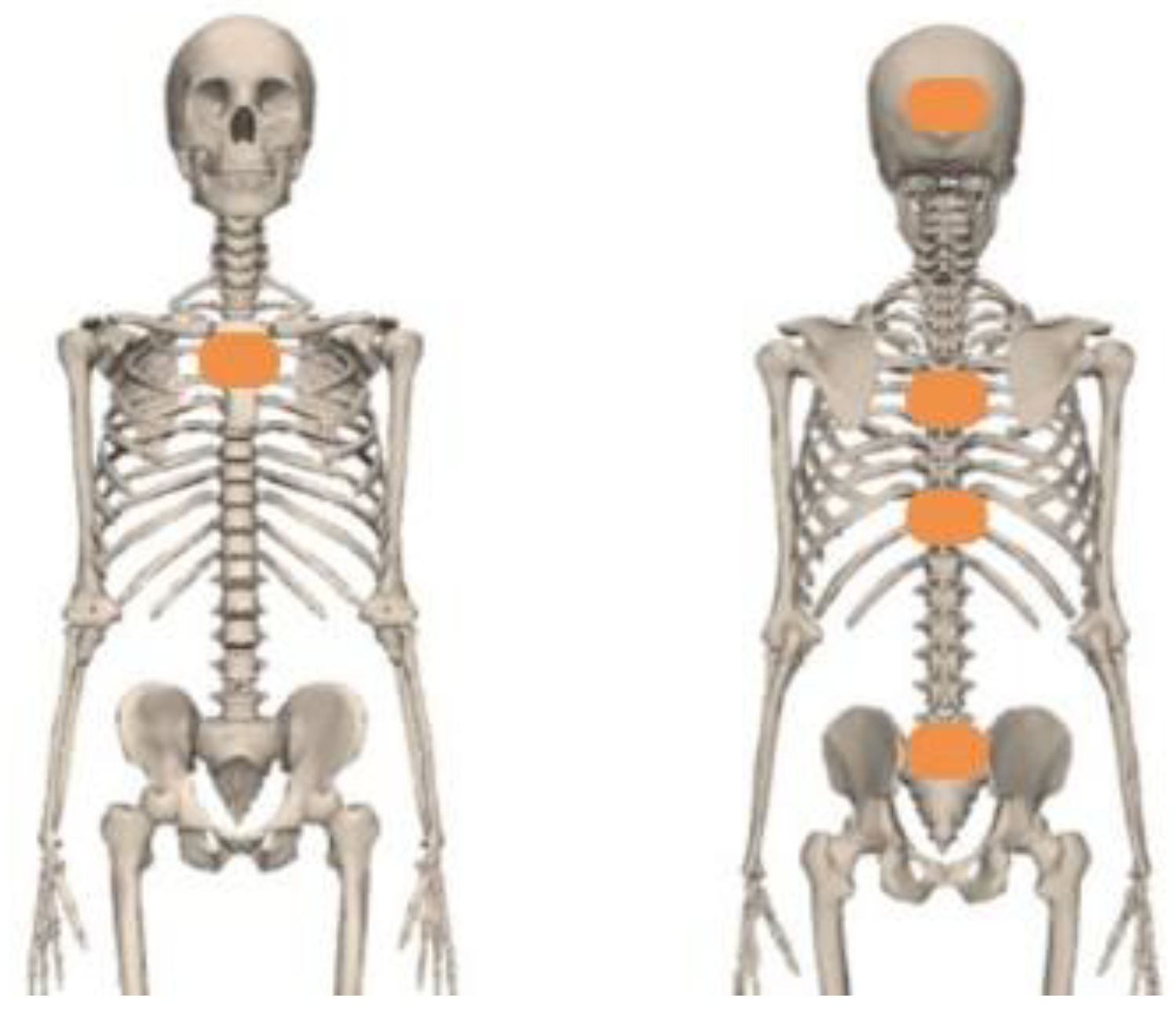
2.2. Experimental Set-Up
2.2.1. IMU Sensors
2.2.2. Experimental Procedures
2.2.3. Model
2.3. Data Analysis
2.3.1. Kinematics Calculation
2.3.2. Joint Moment and Reaction Force Calculation
3. Results
3.1. Kinematics
3.1.1. Mean Working Posture and Range of Motion
3.1.2. Joint Angle Distribution
3.2. Kinetics
3.2.1. Mean Lumbar and Neck Moment
3.2.2. Lumbar and Neck Moment Distribution
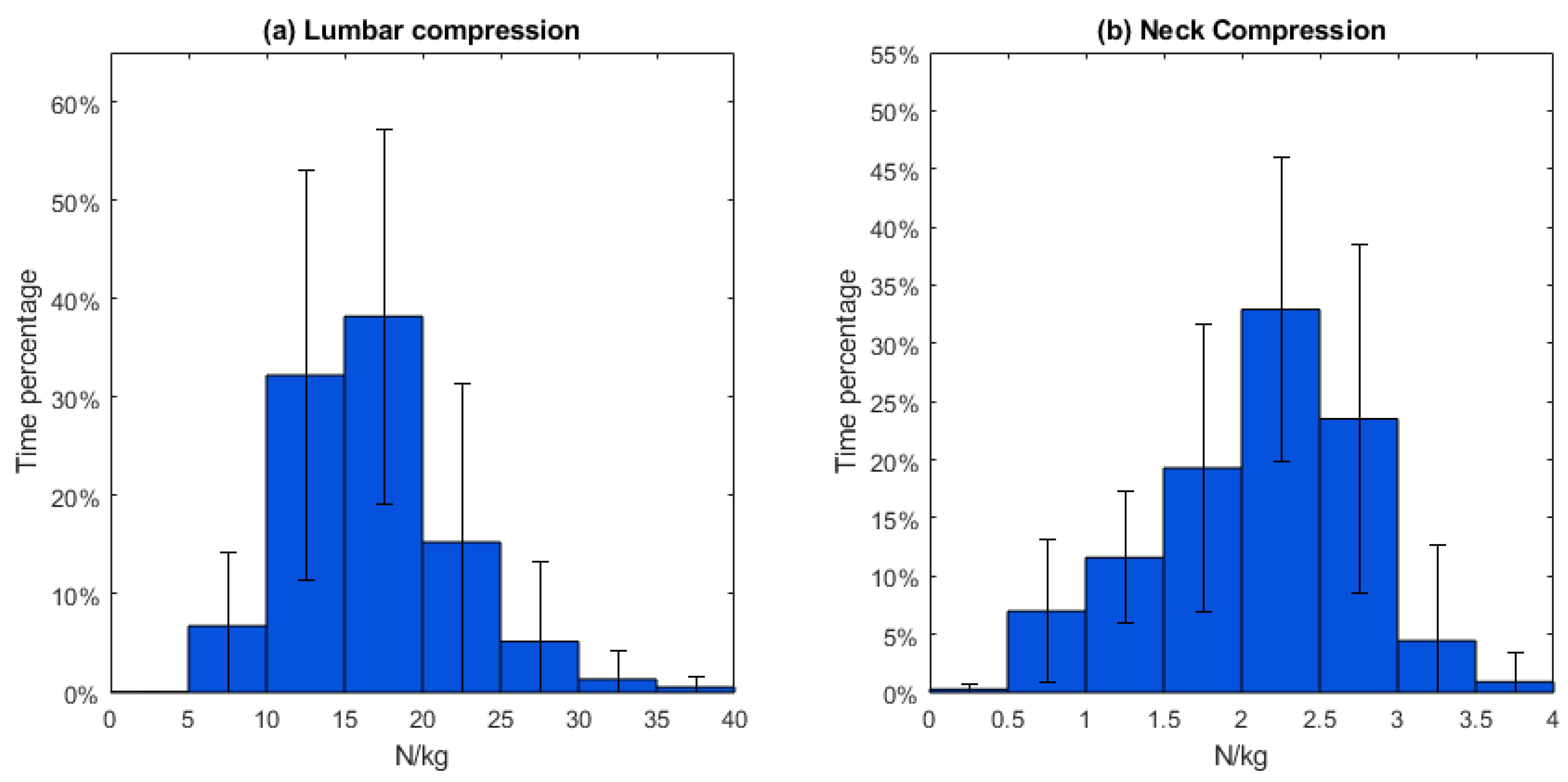
3.2.3. Lumbar and Neck Joint Reaction Forces
4. Discussion
4.1. Biomechanical Profile during the Open-Surgery Training
4.2. Implications for Designing a Neck and Trunk Exoskeleton
4.3. Limitation and Recommendation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
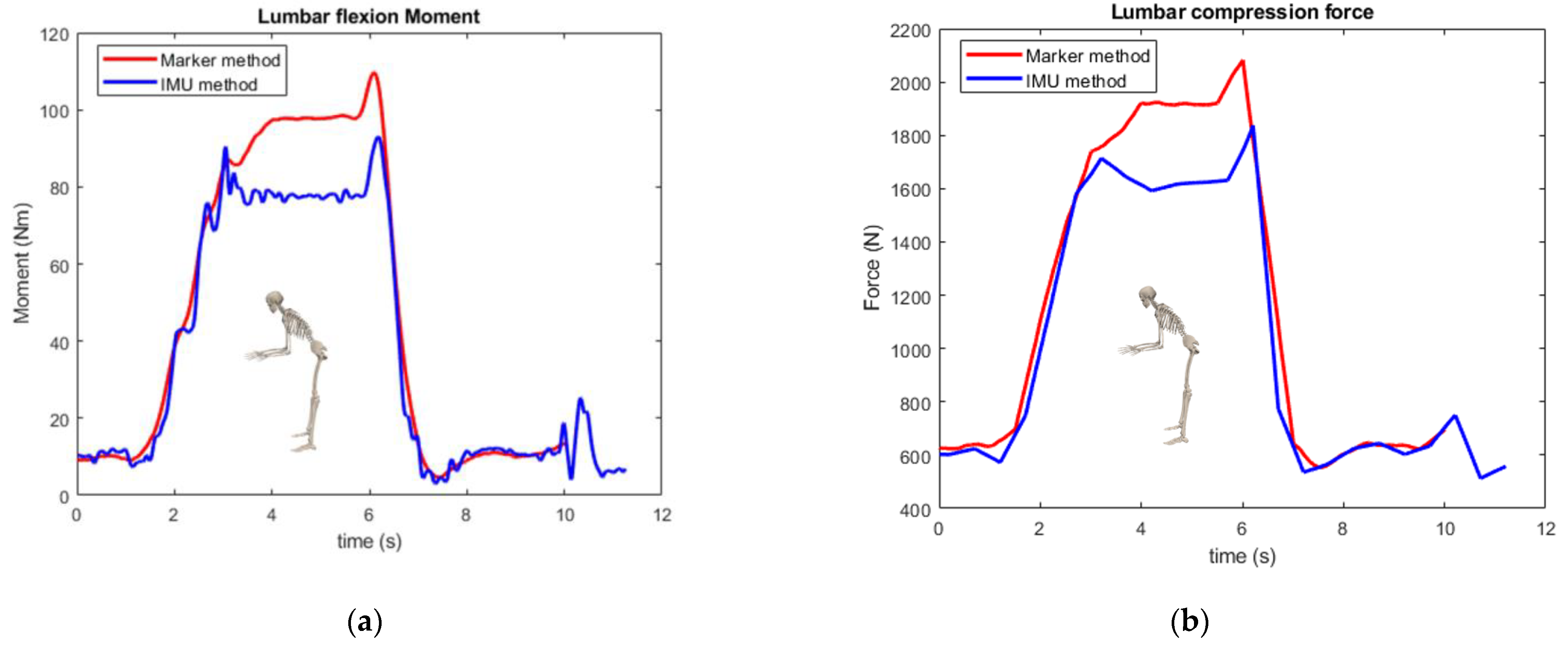
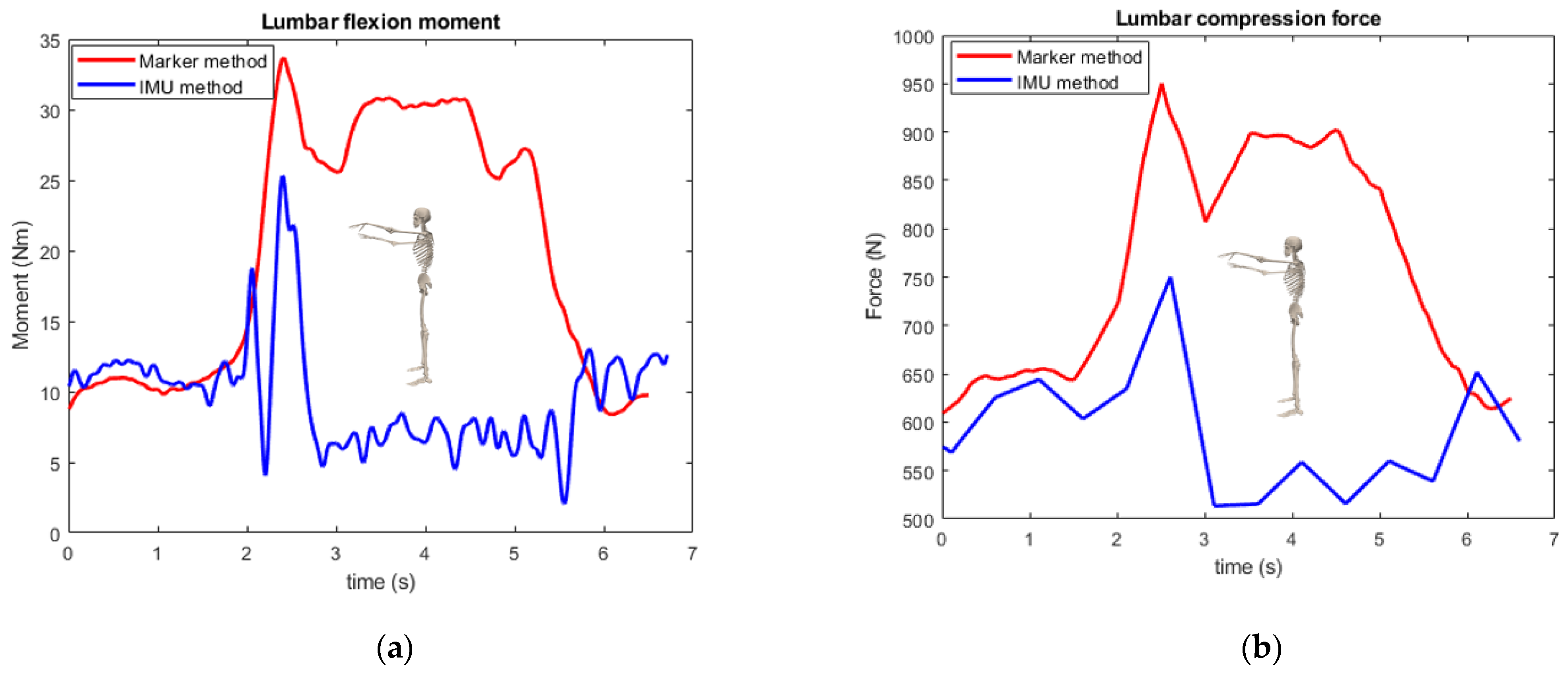
Appendix A. Kinetic Validation
| Movement | Moment | Compression Force | ||||
|---|---|---|---|---|---|---|
| RMSE (Nm) | Peak Moment Difference | Correlation | RMSE (N) | Peak Force Difference | Correlation | |
| Neck flexion | 0.430 | 10.4% | 0.992 | 10.8 | 9.10% | 0.996 |
| Lumbar flexion | 2.62 | 2.41% | 0.999 | 62.1 | 4.85% | 0.993 |
| Lumbar flexion with stretched arm | 10.8 | 15.2% | 0.990 | 164 | 11.8% | 0.988 |
| Stand straight with stretched arm | 15.3 | 23.8% | −0.230 | 228 | 21.1% | −0.212 |
| Movement | Moment | Compression Force | ||
|---|---|---|---|---|
| GS RSD | IMU RSD | GS RSD | IMU RSD | |
| Neck flexion | 2.70% | 3.43% | 2.52% | 2.69% |
| Lumbar flexion | 2.61% | 3.72% | 1.36% | 1.81% |
| Lumbar flexion with stretched arm | 6.10% | 5.06% | 5.09% | 3.25% |
| Stand straight with stretched arm | 7.23% | 12.9% | 14.0% | 9.79% |


References
- Dianat, I.; Bazazan, A.; Souraki Azad, M.A.; Salimi, S.S. Work-Related Physical, Psychosocial and Individual Factors Associated with Musculoskeletal Symptoms among Surgeons: Implications for Ergonomic Interventions. Appl. Ergon. 2018, 67, 115–124. [Google Scholar] [CrossRef]
- Davis, W.T.; Fletcher, S.A.; Guillamondegui, O.D. Musculoskeletal Occupational Injury among Surgeons: Effects for Patients, Providers, and Institutions. J. Surg. Res. 2014, 189, 207–212.e6. [Google Scholar] [CrossRef]
- Soueid, A.; Oudit, D.; Thiagarajah, S.; Laitung, G. The Pain of Surgery: Pain Experienced by Surgeons While Operating. Int. J. Surg. 2010, 8, 118–120. [Google Scholar] [CrossRef] [Green Version]
- Yu, D.; Lowndes, B.; Thiels, C.; Bingener, J.; Abdelrahman, A.; Lyons, R.; Hallbeck, S. Quantifying Intraoperative Workloads Across the Surgical Team Roles: Room for Better Balance? World J. Surg. 2016, 40, 1565–1574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woolf, A.D.; Erwin, J.; March, L. The Need to Address the Burden of Musculoskeletal Conditions. Best Pract. Res. Clin. Rheumatol. 2012, 26, 183–224. [Google Scholar] [CrossRef]
- Ciolac, E.G.; Rodrigues-da-Silva, J.M. Resistance Training as a Tool for Preventing and Treating Musculoskeletal Disorders. Sports Med. 2016, 46, 1239–1248. [Google Scholar] [CrossRef]
- Yang, L.; Wang, T.; Weidner, T.K.; Madura, J.A.; Morrow, M.M.; Hallbeck, M.S. Intraoperative Musculoskeletal Discomfort and Risk for Surgeons during Open and Laparoscopic Surgery. Surg. Endosc. 2021, 35, 6335–6343. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, M.L.; Ludewig, P.M.; Braman, J.P. Musculoskeletal Pain in Resident Orthopaedic Surgeons: Results of a Novel Survey. Iowa Orthop. J. 2014, 34, 190–196. [Google Scholar]
- Pejčić, N.; Petrović, V.; Marković, D.; Miličić, B.; Dimitrijević, I.I.; Perunović, N.; Čakić, S. Assessment of Risk Factors and Preventive Measures and Their Relations to Work-Related Musculoskeletal Pain among Dentists. Work 2017, 57, 573–593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voss, R.K.; Chiang, Y.J.; Cromwell, K.D.; Urbauer, D.L.; Lee, J.E.; Cormier, J.N.; Stucky, C.C.H. Do No Harm, Except to Ourselves? A Survey of Symptoms and Injuries in Oncologic Surgeons and Pilot Study of an Intraoperative Ergonomic Intervention. J. Am. Coll. Surg. 2017, 224, 16–25.e1. [Google Scholar] [CrossRef]
- Zarra, T.; Lambrianidis, T. Musculoskeletal Disorders amongst Greek Endodontists: A National Questionnaire Survey. Int. Endod. J. 2014, 47, 791–801. [Google Scholar] [CrossRef]
- Koopman, A.S.; Näf, M.; Baltrusch, S.J.; Kingma, I.; Rodriguez-Guerrero, C.; Babič, J.; de Looze, M.P.; van Dieën, J.H. Biomechanical Evaluation of a New Passive Back Support Exoskeleton. J. Biomech. 2020, 105, 109795. [Google Scholar] [CrossRef]
- Koopman, A.S.; Kingma, I.; Faber, G.S.; de Looze, M.P.; van Dieën, J.H. Effects of a Passive Exoskeleton on the Mechanical Loading of the Low Back in Static Holding Tasks. J. Biomech. 2019, 83, 97–103. [Google Scholar] [CrossRef] [Green Version]
- Alemi, M.M.; Geissinger, J.; Simon, A.A.; Chang, S.E.; Asbeck, A.T. A Passive Exoskeleton Reduces Peak and Mean EMG during Symmetric and Asymmetric Lifting. J. Electromyogr. Kinesiol. 2019, 47, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Koopman, A.S.; Kingma, I.; de Looze, M.P.; van Dieën, J.H. Effects of a Passive Back Exoskeleton on the Mechanical Loading of the Low-Back during Symmetric Lifting. J. Biomech. 2020, 102, 109486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, X.; Huang, T.H.; Hu, H.; Yu, S.; Zhang, S.; Zhou, X.; Carriero, A.; Yue, G.; Su, H. Spine-Inspired Continuum Soft Exoskeleton for Stoop Lifting Assistance. IEEE Robot. Autom. Lett. 2019, 4, 4547–4554. [Google Scholar] [CrossRef] [Green Version]
- Alessa, F.; Ning, X. Changes of Lumbar Posture and Tissue Loading during Static Trunk Bending. Hum. Mov. Sci. 2018, 57, 59–68. [Google Scholar] [CrossRef]
- Hallbeck, M.S.; Lowndes, B.R.; McCrory, B.; Morrow, M.M.; Kaufman, K.R.; LaGrange, C.A. Kinematic and Ergonomic Assessment of Laparoendoscopic Single-Site Surgical Instruments during Simulator Training Tasks. Appl. Ergon. 2017, 62, 118–130. [Google Scholar] [CrossRef]
- Yurteri-Kaplan, L.A.; Zhu, X.; Iglesia, C.B.; Gutman, R.E.; Sokol, A.I.; Paquet, V.; Park, A.J. Differences in Postural Loading between Primary and Assistant Surgeons during Vaginal Surgery. Int. J. Ind. Ergon. 2018, 65, 60–67. [Google Scholar] [CrossRef]
- Lobo, D.; Anuarbe, P.; López-Higuera, J.M.; Viera, J.; Castillo, N.; Megía, R. Estimation of Surgeons’ Ergonomic Dynamics with a Structured Light System during Endoscopic Surgery. Int. Forum Allergy Rhinol. 2019, 9, 857–864. [Google Scholar] [CrossRef]
- Leung, K.L.; Segal, R.M.; Bernstein, J.D.; Orosco, R.K.; Reid, C.M. Surgical Ergonomics: Assessment of Surgeon Posture and Impact of Training Device during Otolaryngology Procedures. Laryngoscope Investig. Otolaryngol. 2022, 7, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, A.; Huckleby, J.; Kabbani, M.; Delano, A.; De Sutter, M.; Crawford, D. Ergonomic Assessment of Robotic General Surgeons: A Pilot Study. J. Robot. Surg. 2020, 14, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Norasi, H.; Tetteh, E.; Money, S.R.; Davila, V.J.; Meltzer, A.J.; Morrow, M.M.; Fortune, E.; Mendes, B.C.; Hallbeck, M.S. Intraoperative Posture and Workload Assessment in Vascular Surgery. Appl. Ergon. 2021, 92, 103344. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Greve, C.; Verkerke, G.J.; Roossien, C.C.; Houdijk, H.; Hijmans, J.M. Pilot Validation Study of Inertial Measurement Units and Markerless Methods for 3D Neck and Trunk Kinematics during a Simulated Surgery Task. Sensors 2022, 22, 8342. [Google Scholar] [CrossRef]
- Bruno, A.G.; Bouxsein, M.L.; Anderson, D.E. Development and Validation of a Musculoskeletal Model of the Fully Articulated Thoracolumbar Spine and Rib Cage. J. Biomech. Eng. 2015, 137, 081003. [Google Scholar] [CrossRef]
- Xsens Technologies B.V. MT Manager User Manual Revision 2020.A; Xsens Technologies B.V.: Enschede, The Netherlands, 2020. [Google Scholar]
- Paulich, M.; Schepers, M.; Rudigkeit, N.; Bellusci, G. Xsens MTw Awinda: Miniature Wireless Inertial-Magnetic Motion Tracker for Highly Accurate 3D Kinematic Applications; Xsens: Enschede, The Netherlands, 2018; pp. 1–9. [Google Scholar]
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-Source Software to Create and Analyze Dynamic Simulations of Movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef] [Green Version]
- Al Borno, M.; O’Day, J.; Ibarra, V.; Dunne, J.; Seth, A.; Habib, A.; Ong, C.; Hicks, J.; Uhlrich, S.; Delp, S. OpenSense: An Open-Source Toolbox for Inertial-Measurement-Unit-Based Measurement of Lower Extremity Kinematics over Long Durations. J. Neuroeng. Rehabil. 2022, 19, 22. [Google Scholar] [CrossRef]
- Seth, A.; Sherman, M.; Reinbolt, J.A.; Delp, S.L. OpenSim: A Musculoskeletal Modeling and Simulation Framework for in Silico Investigations and Exchange. Procedia IUTAM 2011, 2, 212–232. [Google Scholar] [CrossRef]
- Banks, J.J.; Alemi, M.M.; Allaire, B.T.; Lynch, A.C.; Bouxsein, M.L.; Anderson, D.E. Using Static Postures to Estimate Spinal Loading during Dynamic Lifts with Participant-Specific Thoracolumbar Musculoskeletal Models. Appl. Ergon. 2023, 106, 103869. [Google Scholar] [CrossRef]
- Yang, L.; Money, S.R.; Morrow, M.M.; Lowndes, B.R.; Weidner, T.K.; Fortune, E.; Davila, V.J.; Meltzer, A.J.; Stone, W.M.; Hallbeck, M.S. Impact of Procedure Type, Case Duration, and Adjunctive Equipment on Surgeon Intraoperative Musculoskeletal Discomfort. J. Am. Coll. Surg. 2020, 230, 554–560. [Google Scholar] [CrossRef] [Green Version]
- Näf, M.B.; Koopman, A.S.; Baltrusch, S.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Passive Back Support Exoskeleton Improves Range of Motion Using Flexible Beams. Front. Robot. AI 2018, 5, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madinei, S.; Alemi, M.M.; Kim, S.; Srinivasan, D.; Nussbaum, M.A. Biomechanical Assessment of Two Back-Support Exoskeletons in Symmetric and Asymmetric Repetitive Lifting with Moderate Postural Demands. Appl. Ergon. 2020, 88, 103156. [Google Scholar] [CrossRef] [PubMed]
- Yee, C.A.; Kazerooni, H. A Neck Support for Alleviating Occupational Neck Pain. Proc. Hum. Factors Ergon. Soc. 2015, 59, 1404–1408. [Google Scholar] [CrossRef]
- Mahmood, M.N.; Tabasi, A.; Kingma, I.; van Dieën, J.H. A Novel Passive Neck Orthosis for Patients with Degenerative Muscle Diseases: Development & Evaluation. J. Electromyogr. Kinesiol. 2021, 57, 102515. [Google Scholar] [CrossRef]
- Beaucage-Gauvreau, E.; Robertson, W.S.P.; Brandon, S.C.E.; Fraser, R.; Freeman, B.J.C.; Graham, R.B.; Thewlis, D.; Jones, C.F. Validation of an OpenSim Full-Body Model with Detailed Lumbar Spine for Estimating Lower Lumbar Spine Loads during Symmetric and Asymmetric Lifting Tasks. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 451–464. [Google Scholar] [CrossRef]
- Kim, H.K.; Zhang, Y. Estimation of Lumbar Spinal Loading and Trunk Muscle Forces during Asymmetric Lifting Tasks: Application of Whole-Body Musculoskeletal Modelling in OpenSim. Ergonomics 2017, 60, 563–576. [Google Scholar] [CrossRef]
- Li, S.S.W.; Chow, D.H.K. Effects of Backpack Load on Critical Changes of Trunk Muscle Activation and Lumbar Spine Loading during Walking. Ergonomics 2018, 61, 553–565. [Google Scholar] [CrossRef]
- Vicon Motion Systems Ltd. Vicon® Plug-in Gait Reference Guide; Vicon Motion Systems Ltd.: Oxford, UK, 2017. [Google Scholar]






| Lumbar FE | Lumbar LB | Lumbar AR | Neck FE | Neck LB | Neck AR | |
|---|---|---|---|---|---|---|
| Mean posture (°) | −20.4 | −0.373 | 0.291 | −19.8 | 0.0393 | −1.65 |
| SD (°) | 10.0 | 5.05 | 2.23 | 6.69 | 5.04 | 4.81 |
| ROM (°) | 53.4 | 45.6 | 54.1 | 102 | 68.6 | 149 |
| SD (°) | 12.2 | 10.4 | 17.4 | 25.6 | 11.6 | 11.8 |
| Moment/Mass (Nm/kg) | Lumbar FE | Lumbar LB | Lumbar AR | Neck FE | Neck LB | Neck AR |
|---|---|---|---|---|---|---|
| Mean | 0.503 | 0.0101 | 0.00210 | 0.0419 | 4.65 × 10−4 | −3.24 × 10−9 |
| SD | 0.179 | 0.0907 | 0.0282 | 0.00743 | 0.00842 | 1.38 × 10−8 |
| N/kg | Lumbar Compression | Neck Compression |
|---|---|---|
| Mean | 17.0 | 2.11 |
| SD | 3.71 | 0.284 |
| Max. | 35.9 | 3.63 |
| SD | 17.7 | 0.913 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Roossien, C.C.; Verkerke, G.J.; Houdijk, H.; Hijmans, J.M.; Greve, C. Biomechanical Load of Neck and Lumbar Joints in Open-Surgery Training. Sensors 2023, 23, 6974. https://doi.org/10.3390/s23156974
Zhang C, Roossien CC, Verkerke GJ, Houdijk H, Hijmans JM, Greve C. Biomechanical Load of Neck and Lumbar Joints in Open-Surgery Training. Sensors. 2023; 23(15):6974. https://doi.org/10.3390/s23156974
Chicago/Turabian StyleZhang, Ce, Charlotte Christina Roossien, Gijsbertus Jacob Verkerke, Han Houdijk, Juha M. Hijmans, and Christian Greve. 2023. "Biomechanical Load of Neck and Lumbar Joints in Open-Surgery Training" Sensors 23, no. 15: 6974. https://doi.org/10.3390/s23156974






