Technologies for Monitoring Lifestyle Habits Related to Brain Health: A Systematic Review
Abstract
:1. Introduction
- Physical exercise: The regular practice of physical exercise has been shown to have a deep impact on mood and stress tolerance, improving depression and anxiety. In addition, physical activity can improve cognitive function and improve wellbeing in a number of neurodegenerative diseases. It also has been repeatedly associated with the upregulation of neurotrophic factors. Different studies have linked being active with a lower prevalence of neurological and psychiatric diseases [10,11].
- Sleep: Sleep disorders have implications for daily life, including fatigue, low performance, and difficulties to complete professional, family or social obligations. There is also a correlation between sleep disorders and neurological disorders [12]. Even in the absence of sleep disorders, the amount and quality of sleep have a major impact on brain health, cognitive function, and mental wellbeing.
- Nutrition: How much we eat and what we eat represent an important pillar for brain health. An unbalanced diet can result in a lack of nutrients, which can have a deep impact on our overall health. In addition, nutritional factors have been linked to diseases such as dementia or Alzheimer’s disease [10]. A balanced Mediterranean diet can impact cognitive function, and certain nutritional supplements might have an effect on mood, motivation, and initiative. Furthermore, the body mass index (BMI) appears to correlate with mental wellbeing and cognitive abilities [13,14].
- Cognitive activity: As we get older, our brains require less strain to perform everyday activities. However, our brain needs to face new challenges in order to stay healthy. It is as important to “exercise” our mind as it is to exercise our bodies. Cognitive impairment can be the result of neurological diseases such as Alzheimer’s disease or Parkinson’s disease. Keeping an active brain can preserve brain plasticity and promote brain resilience and cognitive reserve. Cognitive activity can, but does not necessarily have to, involve computer-supported cognitive training [15].
- Vital plan: Meaning in life and life purpose are the focus of many psychology studies from the last decades of 20th century [16,17,18] and alterations or lack of a defined vital plan are associated with many disorders like anxiety, depression, or even mortality. These disorders are known to interfere in brain health [19]. Our human brain has a property that animals lack: It allows us to project ourselves into the future. Prospecting, the ability to imagine what it will be like to try to make a goal or a dream into a reality, is an essential function for our brain and we need to encourage it by defining a vital plan, a purpose in life that transcends us as individuals. This is so important that it seems to mediate the effect of all other pillars onto our brain health.
- Social interactions: We are social beings and our brain needs relationships. The time spent with family and friends or getting to know and relating to our neighbors and colleagues is important. Loneliness is not only bad for brain health, it is a deadly disease. Individuals with a high number of social interactions experience significantly less cognitive decline compared to those who are lonely or isolated [20,21]. It also has been shown that social interactions and environment can help to improve brain plasticity after a brain lesion [22].
- Overall health: Overall health is an important factor due to the existing strong relations between overall health and brain health. For example, there is a close link between chronic diseases and depression [23,24] and systemic diseases, such as diabetes or hypertension, pose critical risks for brain health. Therefore, we should have check-ups, go to the doctor regularly, follow their recommendations, and pay attention to the conditions and diseases we have. However, we now also know that the opposite direction is also important, good mental and brain health promote overall health and wellbeing.
2. Materials and Methods
2.1. Keywords Definition
- General: Terms that define the main field of the study. In this case, terms related to brain health or cognitive functioning, including cognitive deterioration and cognitive reserve. The terms ‘brain health’ and ‘cognitive’ (which include terms above and more) were chosen.
- Associated: Terms associated with the topic. In this case, terms associated with cognitive decline (e.g., age, aging).
- Pillars: Terms that are associated with the specific pillars of intervention (as defined in [3]) identified as critical variables that affect brain health. (e.g., nutrition, sleep or socialization).
- Techniques: Terms that are often used in projects related to interventions and monitoring of daily life activities (e.g., intervention, monitoring, adherence, etc.).
- Technologies: Technical terms that usually appear in studies related to eHealth and telemedicine (e.g., wearable, eHealth, ICT, etc.).
2.2. Identification
2.3. Screening & Eligibility
- Population: Participants had to be at least 18 years old as we aimed to focus on adults and exclude pediatric populations. Participants had to be healthy and thus could not be diagnosed with any particular disease or disability.
- Intervention: The intervention should not be related to one particular disease (e.g., Alzheimer’s disease or multiple sclerosis) or to any single particular ability or problem (e.g., driving). Rather, the intervention should be focused on habit improvement and daily life monitoring. It also must involve the use of at least one of the following technologies: (1) Web application (2) mobile phone (3) wearables (4) biosensors (5) medical devices (e.g., fMRI) (6) computer tasks.
- Comparator: Both placebo and active interventions were taken into consideration.
- Outcome: The outcome must be referred to core aspects of brain health or cognitive function, including (but not exclusively) one or more of the seven pillars (e.g., sleep or physical activity). Ideally, the publications should also contain an outcome of therapy adherence or usability.
- Timeframe: Both short- and long-term outcomes were taken into account.
- Study: Studies could be either randomized controlled trials (RCTs) or observational studies. Protocols, systematic reviews, nonsystematic reviews, case studies, commentaries, and letters or editorials were excluded.
2.4. Included
- Heavy monitoring: When people needed a hospital or a controlled site to do specific tasks or specific tests.
- Medium monitoring: When participants were monitored using smartphones, wearables or biosensors that are not intrusive.
- Light monitoring: When participants were only monitored using questionnaires and tests or providing self-report data, through web or mobile applications.
- No monitoring: When no monitoring took place or is not reported.
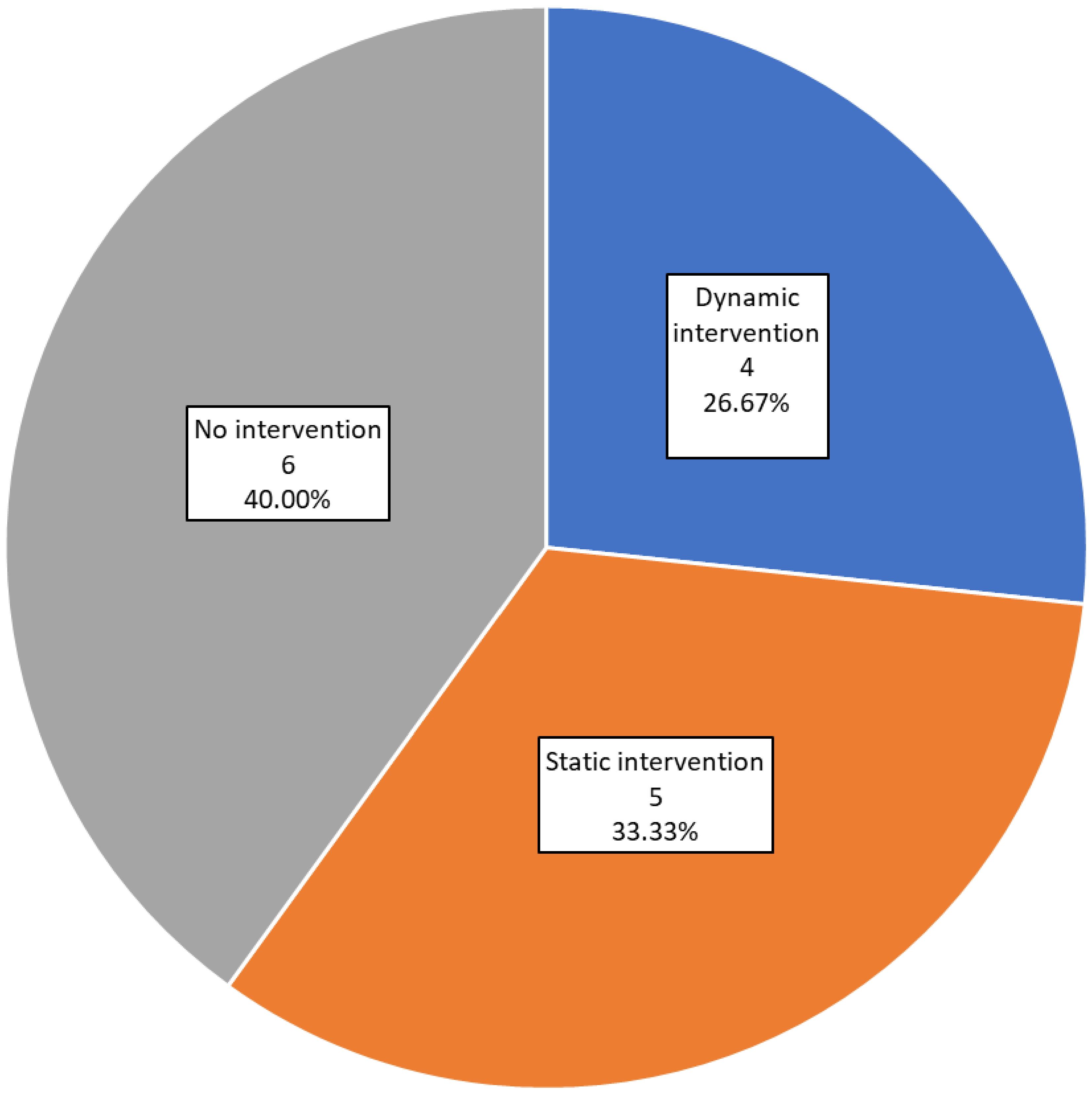
- Studies were also subcategorized according to how the intervention was carried out. We defined two categories:
- Dynamic intervention: When the intervention was adaptive and could change to fit the participant’s behavior patterns and evolution.
- Static intervention: When the intervention was the same for all participants, based on pre-specified criteria and rules, and was not modified throughout the study.
3. Results and Discussion
3.1. Distribution on Pillars
3.2. Monitoring
3.3. Intervention Style
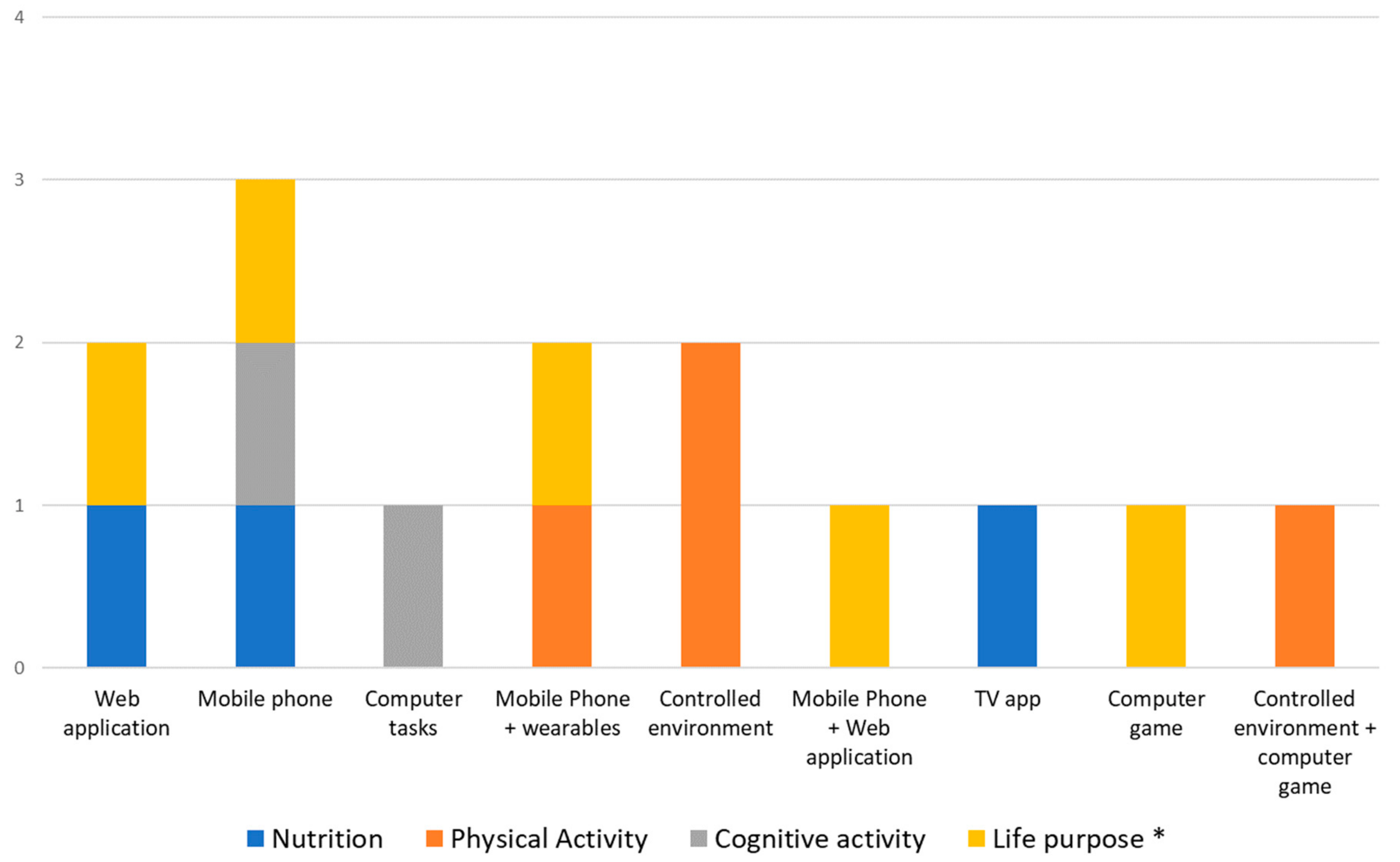
3.4. Technology Used
3.5. Technologies Related to Pillars
- The vast majority (75%) of studies related to physical exercise focus on proofs of concept and use specific controlled environments, where they integrate or replicate the sensors that could be found in a wearable device. Future studies, therefore, are likely to employ wearables to capture similar outcomes.
- Nutrition is difficult to monitor with sensors, so it is usual to find that both, monitoring and intervention, are carried out with questionnaires and guidelines. This is why web and mobile applications are the most used (75% of them).
- Surprisingly, the same occurs with the cognitive pillar, where only tasks or questionnaires are used. Future studies ought to leverage mobile trackers, wearables, and phones to try to capture relevant information regarding cognitive function in a real-life setting and employing passive, non-intrusive designs.
- Although there exist some non-intrusive devices to measure brain signals (mainly EEG), these are not yet comfortable, portable or reliable enough to use in daily life tasks and in long periods.
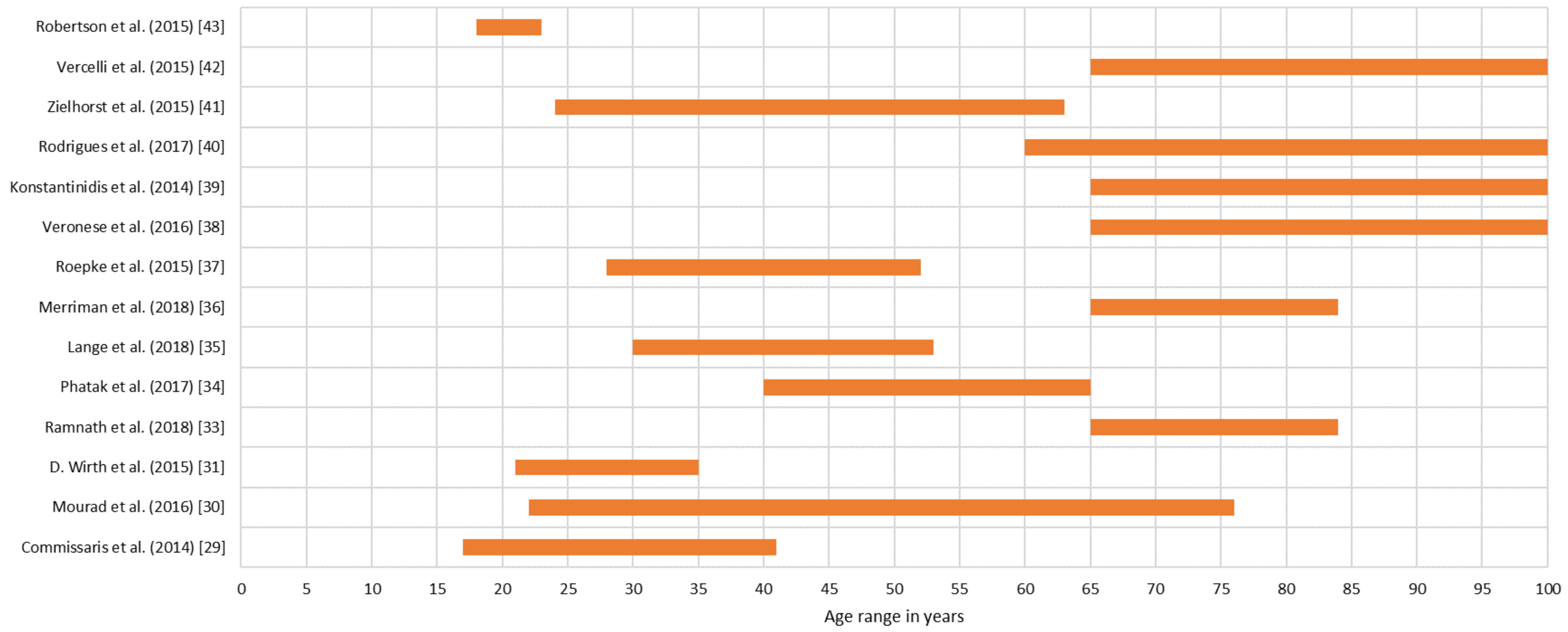
3.6. Demographic Data
3.7. Correlation between Lifestyle Habits Factors and Brain Health
3.8. Limitations and Out of Criteria Studies
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Index | Query | Category |
|---|---|---|
| 1 | ( “brain health” OR “cognitive” ) | General Terms |
| 2 | ( “brain health” OR “cognitive” OR “young elders” OR “aging” OR “older adults” OR “ageing” OR “elderly” OR “aged” OR “older person” OR “geriatrics” ) | Associated Terms |
| 3 | ( “nutrition” OR “diet” OR “physical” OR “physical exercise” OR “physical activity” OR “cognitive” OR “cognition” OR “cognitive activity” OR “cognitive training” OR “social” OR “socialization” OR “vital plan” OR “purpose in life” OR “psychological wellbeing” OR “mindfulness” OR “general health” OR “comprehensive health” OR “global health” OR “sleep” OR “sleeping” OR “relax” OR “rest”) | Pillar related Terms |
| 4 | ( “adherence” OR “motivation” OR “monitoring” OR “coaching” OR “coach” OR “treatment” OR “intervention” OR “exercise” ) | Technique related terms |
| 5 | ( “smartphone” OR “mobile” OR “ICT” OR “RMT”OR “mHealth” OR “eHealth” OR “data mining” OR “predictor” OR “machine learning” OR “deep learning” OR “neuronal network” OR “artificial intelligence” OR “computer” OR “biosensor” OR “wearable” OR “technology” OR “technologies”) | Technology related terms |
| 6 | ( “observational study” OR “controlled study” ) | Study filter |
| 7 | NOT ( “schizophrenia” ) AND NOT ( “cancer” ) AND NOT ( “pediatrics” ) AND NOT ( “epilepsy” ) AND NOT ( “drugs” ) AND NOT ( “diabetes” ) AND NOT ( “stroke” ) AND NOT ( “dementia” ) AND NOT ( “transplant” ) AND NOT ( “fracture” ) AND NOT ( “traumatic” ) AND NOT ( “surgical” ) AND NOT ( “EEG” ) AND NOT ( “disorder” ) | Exclusions |
| 8 | [1] AND [2] AND [3] AND [4] AND [5] AND [6] AND [7] | Resultant query |
References
- Whiteford, H.A.; Ferrari, A.J.; Degenhardt, L.; Feigin, V.; Vos, T. Global Burden of Mental, Neurological, and Substance Use Disorders: An Analysis from the Global Burden of Disease Study 2010. In Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, 3rd ed.; Patel, V., Chisholm, D., Dua, T., Eds.; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2016; Volume 4, pp. 29–40. [Google Scholar]
- Cattaneo, G.; Bartrés-Faz, D.; Morris, T.P.; Sánchez, J.S.; Macià, D.; Tarrero, C.; Tormos, J.M.; Pascual-Leone, A. The Barcelona Brain Health Initiative: A Cohort Study to Define and Promote Determinants of Brain Health. Front. Aging Neurosci. 2018, 10, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Leone, A. Chapter 19 Disrupting the brain to guide plasticity and improve behavior. Prog. Brain Res. 2006, 157, 315–329. [Google Scholar] [PubMed]
- Pascual-Leone, A.; Freitas, C.; Oberman, L.; Horvath, J.C.; Halko, M.; Eldaief, M.; Bashir, S.; Vernet, M.; Shafi, M.; Westover, B.; et al. Characterizing brain cortical plasticity and network dynamics across the age-span in health and disease with TMS-EEG and TMS-fMRI. Brain Topogr. 2011, 24, 302–315. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, K.; Fiocco, A.J.; Lindquist, K.; Vittinghoff, E.; Simonsick, E.M.; Newman, A.B.; Satterfield, S.; Rosano, C.; Rubin, S.M.; Ayonayon, H.N.; et al. Predictors of maintaining cognitive function in older adults. Neurology 2009, 72, 2029–2035. [Google Scholar] [CrossRef]
- Barnard, N.D.; Bush, A.I.; Ceccarelli, A.; Cooper, J.; de Jager, C.A.; Erickson, K.I.; Fraser, G.; Kesler, S.; Levin, S.M.; Lucey, B.; et al. Dietary and lifestyle guidelines for the prevention of Alzheimer’s disease. Neurobiol. Aging 2014, 35, S74–S78. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.L.; Drummond, P.D. Obesity and psychiatric disorders: Commonalities in dysregulated biological pathways and their implications for treatment. Prog. Neuro-Psychopharmacolog. Biol. Psychiatry 2013, 45, 92–99. [Google Scholar] [CrossRef] [Green Version]
- Wirth, M.; Haase, C.M.; Villeneuve, S.; Vogel, J.; Jagust, W.J. Neuroprotective pathways: Lifestyle activity, brain pathology, and cognition in cognitively normal older adults. Neurobiol. Aging 2014, 35, 1873–1882. [Google Scholar] [CrossRef]
- Bamidis, P.D.; Vivas, A.B.; Styliadis, C.; Frantzidis, C.; Klados, M.; Schlee, W.; Siountas, A.; Papageorgiou, S.G. A review of physical and cognitive interventions in aging. Neurosci. Biobehav. Rev. 2014, 44, 206–220. [Google Scholar] [CrossRef]
- Wilcox, S.; Sharkey, J.R.; Mathews, A.E.; Laditka, J.N.; Laditka, S.B.; Logsdon, R.G.; Sahyoun, N.; Robare, J.F.; Liu, R. Perceptions and beliefs about the role of physical activity and nutrition on brain health in older adults. Gerontologist 2009, 49, S61–S71. [Google Scholar] [CrossRef]
- Cotman, C.W.; Berchtold, N.C. Exercise: A behavioral intervention to enhance brain health and plasticity. Trends Neurosci. 2002, 25, 295–301. [Google Scholar] [CrossRef]
- McCarter, S.J.; St. Louis, E.K.; Boeve, B.F. REM sleep behavior disorder and REM sleep without atonia as an early manifestation of degenerative neurological disease. Curr. Neurol. Neurosci. Rep. 2012, 12, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Gunstad, J.; Paul, R.H.; Cohen, R.A.; Tate, D.F.; Spitznagel, M.B.; Grieve, S.; Gordon, E. Relationship Between Body Mass Index and Brain Volume in Healthy Adults. Int. J. Neurosci. 2008, 118, 1582–1593. [Google Scholar] [CrossRef] [PubMed]
- Cournot, M.; Marquié, J.C.; Ansiau, D.; Martinaud, C.; Fonds, H.; Ferrières, J.; Ruidavets, J.B. Relation between body mass index and cognitive function in healthy middle-aged men and women. Neurology 2006, 67, 1208–1214. [Google Scholar] [CrossRef] [PubMed]
- Solana, J.; Cáceres, C.; García-Molina, A.; Opisso, E.; Roig, T.; Tormos, J.M.; Gómez, E.J. Improving brain injury cognitive rehabilitation by personalized telerehabilitation services: Guttmann neuropersonal trainer. IEEE J. Biomed. Heal. Inf. 2015, 19, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Phillips, W.M. Purpose in life, depression, and locus of control. J. Clin. Psychol. 1980, 36, 661–667. [Google Scholar] [CrossRef]
- Boyle, P.A.; Barnes, L.L.; Buchman, A.S.; Bennett, D.A. Purpose in life is associated with mortality among community-dwelling older persons. Psychosom. Med. 2009, 71, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Robak, R.W.; Griffin, P.W. Purpose in life: What is its relationship to happiness, depression, and grieving? N. Am. J. Psychol. 2000, 2, 113–119. [Google Scholar]
- Bartrés-Faz, D.; Cattaneo, G.; Solana, J.; Tormos, J.M.; Pascual-Leone, A. Meaning in life: Resilience beyond reserve. Alzheimer’s Res. Ther. 2018, 10, 1–10. [Google Scholar]
- Ristau, S. People Do Need People: Social Interaction Boosts Brain Health In Older Age. Heal. San Fr. 2011, 35, 70–76. [Google Scholar]
- Mortimer, J.A.; Ding, D.; Borenstein, A.R.; Decarli, C.; Guo, Q.; Wu, Y.; Zhao, Q.; Chu, S. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented chinese elders. J. Alzheimer’s Dis. 2012, 30, 757–766. [Google Scholar] [CrossRef]
- Johansson, B.B. Environmental influence on recovery after brain lesions–Experimental and clinical data. J. Rehabil. Med. 2003, 35, 11–16. [Google Scholar] [CrossRef]
- Jetté, N.; Patten, S.B.; Lavorato, D.H.; Eliasziw, M.; Williams, J.V.A.; Modgill, G. Major depression as a risk factor for chronic disease incidence: Longitudinal analyses in a general population cohort. Gen. Hosp. Psychiatry 2008, 30, 407–413. [Google Scholar]
- Katon, W.J. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin. Neurosci. 2011, 13, 7–24. [Google Scholar] [PubMed]
- Mukhopadhyay, S.C. Wearable sensors for human activity monitoring: A review. IEEE Sens. J. 2015, 15, 1321–1330. [Google Scholar] [CrossRef]
- Panic, N.; Leoncini, E.; De Belvis, G.; Ricciardi, W.; Boccia, S. Evaluation of the Endorsement of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement on the Quality of Published Systematic Review and Meta-Analyses. PLoS ONE 2013, 8, e83138. [Google Scholar] [CrossRef] [PubMed]
- Vegesna, A.; Tran, M.; Angelaccio, M.; Arcona, S. Remote Patient Monitoring via Non-Invasive Digital Technologies: A Systematic Review. Telemed. e-Health 2017, 23, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Riva, J.J.; Malik, K.M.; Burnie, S.J.; Endicott, A.R.; Busse, J.W. What is your research question ? An introduction to the PICOT format for clinicians. J. Chiropratic Assoc. 2012, 56, 167–171. [Google Scholar]
- Commissaris, D.A.C.M.; Könemann, R.; Hiemstra-van Mastrigt, S.; Burford, E.M.; Botter, J.; Douwes, M.; Ellegast, R.P. Effects of a standing and three dynamic workstations on computer task performance and cognitive function tests. Appl. Ergon. 2014, 45, 1570–1578. [Google Scholar] [CrossRef]
- Mourad, G.; Strömberg, A.; Jonsbu, E.; Gustafsson, M.; Johansson, P.; Jaarsma, T. Guided Internet-delivered cognitive behavioural therapy in patients with non-cardiac chest pain–a pilot randomized controlled study. Trials 2016, 17, 352. [Google Scholar] [CrossRef]
- Wirth, M.D.; Hébert, J.R.; Shivappa, N.; Hand, G.A.; Hurley, T.G.; Drenowatz, C.; McMahon, D.; Shook, R.P.; Blair, S.N. Anti-inflammatory Dietary Inflammatory Index scores are associated with healthier scores on other dietary indices. Nutr. Res. 2016, 36, 214–219. [Google Scholar] [CrossRef]
- Pavel, M.; Jimison, H.; Spring, B. Behavioral informatics: Dynamical models for measuring and assessing behaviors for precision interventions. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBS), Orlando, FL, USA, 16–20 August 2016; Volume 2016, pp. 190–193. [Google Scholar]
- Ramnath, U.; Rauch, L.; Lambert, E.V.; Kolbe-Alexander, T.L. The relationship between functional status, physical fitness and cognitive performance in physically active older adults: A pilot study. PLoS ONE 2018, 13, e0194918. [Google Scholar] [CrossRef]
- Phatak, S.S.; Freigoun, M.T.; Martín, C.A.; Rivera, D.E.; Korinek, E.V.; Adams, M.A.; Buman, M.P.; Klasnja, P.; Hekler, E.B. Modeling individual differences: A case study of the application of system identification for personalizing a physical activity intervention. J. Biomed. Inform. 2018, 79, 82–97. [Google Scholar] [CrossRef]
- Lange, D.; Corbett, J.; Knoll, N.; Schwarzer, R.; Lippke, S. Fruit and Vegetable Intake: The Interplay of Planning, Social Support, and Sex. Int. J. Behav. Med. 2018, 1–10. [Google Scholar] [CrossRef]
- Merriman, N.A.; Roudaia, E.; Romagnoli, M.; Orvieto, I.; Newell, F.N. Acceptability of a custom-designed game, CityQuest, aimed at improving balance confidence and spatial cognition in fall-prone and healthy older adults. Behav. Inf. Technol. 2018, 37, 538–557. [Google Scholar] [CrossRef]
- Roepke, A.M.; Jaffee, S.R.; Riffle, O.M.; McGonigal, J.; Broome, R.; Maxwell, B. Randomized Controlled Trial of SuperBetter, a Smartphone-Based/Internet-Based Self-Help Tool to Reduce Depressive Symptoms. Games Health J. 2015, 4, 235–246. [Google Scholar] [CrossRef]
- Veronese, N.; Stubbs, B.; Trevisan, C.; Bolzetta, F.; De Rui, M.; Solmi, M.; Sartori, L.; Musacchio, E.; Zambon, S.; Perissinotto, E.; et al. What physical performance measures predict incident cognitive decline among intact older adults? A 4.4 year follow up study. Exp. Gerontol. 2016, 81, 110–118. [Google Scholar] [CrossRef]
- Konstantinidis, E.I.; Billis, A.S.; Mouzakidis, C.A.; Zilidou, V.I.; Antoniou, P.E.; Bamidis, P.D. Design, Implementation, and Wide Pilot Deployment of FitForAll: An Easy to use Exergaming Platform Improving Physical Fitness and Life Quality of Senior Citizens. IEEE J. Biomed. Heal. Inf. 2016, 20, 189–200. [Google Scholar] [CrossRef]
- Rodrigues, A.M.; Gregório, M.J.; Gein, P.; Eusébio, M.; Santos, M.J.; de Sousa, R.D.; Coelho, P.S.; Mendes, J.M.; Graça, P.; Oliveira, P.; et al. Home-Based Intervention Program to Reduce Food Insecurity in Elderly Populations Using a TV App: Study Protocol of the Randomized Controlled Trial Saúde.Come Senior. JMIR Res. Protoc. 2017, 6, e40. [Google Scholar] [CrossRef]
- Zielhorst, T.; van den Brule, D.; Visch, V.; Melles, M.; van Tienhoven, S.; Sinkbaek, H.; Schrieken, B.; Tan, E.S.-H.; Lange, A. Using a Digital Game for Training Desirable Behavior in Cognitive–Behavioral Therapy of Burnout Syndrome: A Controlled Study. Cyberpsychology, Behav. Soc. Netw. 2015, 18, 101–111. [Google Scholar] [CrossRef]
- Vercelli, A.; Rainero, I.; De Rosario, H.; Summers, M.; Wieching, R.; Aumayr, G.; Bandelow, S.; Ciferri, L.; Bazzani, M. My-active and healthy ageing (My-AHA): An ICT platform to detect frailty risk and propose intervention. In Proceedings of the 2017 25th International Conference on Software, Telecommunications and Computer Networks, SoftCOM 2017, Split, Croatia, 21–23 September 2017; IEEE: Piscataway, NJ, USA, 2017; Volume 2020, pp. 1–4. [Google Scholar]
- Robertson, K.; Rosasco, C.; Feuz, K.; Schmitter-Edgecombe, M.; Cook, D. Prompting technologies: A comparison of time-based and context-aware transition-based prompting. Technol. Heal. Care 2015, 23, 745–756. [Google Scholar] [CrossRef] [Green Version]
- AIMC 20° encuesta AIMC a usuarios de Internet. Marzo 2018; Madrid. 2018. Available online: https://www.aimc.es/otros-estudios-trabajos/navegantes-la-red/ (accessed on 29 May 2019).
- Robert, P.; Castelli, E.; Chung, P.C.; Chiroux, T.; Crispim-Junior, C.F.; Mallea, P.; Bremond, F. SWEET-HOME ICT technologies for the assessment of elderly subjects. IRBM 2013, 34, 186–190. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Epps, J. Automatic classification of eye activity for cognitive load measurement with emotion interference. Comput. Methods Programs Biomed. 2013, 110, 111–124. [Google Scholar] [CrossRef]
- Cerasa, A.; Gioia, M.C.; Salsone, M.; Donzuso, G.; Chiriaco, C.; Realmuto, S.; Nicoletti, A.; Bellavia, G.; Banco, A.; D’amelio, M.; et al. Neurofunctional correlates of attention rehabilitation in Parkinson’s disease: An explorative study. Neurol. Sci. 2014, 35, 1173–1180. [Google Scholar] [CrossRef]
- Baglio, F.; Griffanti, L.; Saibene, F.L.; Ricci, C.; Alberoni, M.; Critelli, R.; Villanelli, F.; Fioravanti, R.; Mantovani, F.; D’Amico, A.; et al. Multistimulation group therapy in alzheimer’s disease promotes changes in brain functioning. Neurorehabil. Neural Repair 2015, 29, 13–24. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Cesa, G.L.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual Reality–Enhanced Cognitive–Behavioral Therapy for Morbid Obesity: A Randomized Controlled Study with 1 Year Follow-Up. Cyberpsychology Behav. Soc. Netw. 2016, 19, 134–140. [Google Scholar] [CrossRef]
- Mehrabian, S.; Extra, J.; Wu, Y.H.; Pino, M.; Traykov, L.; Rigaud, A.S. The perceptions of cognitively impaired patients and their caregivers of a home telecare system. Med. Devices Evid. Res. 2014, 8, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Cerasa, A.; Gioia, M.C.; Valentino, P.; Nisticò, R.; Chiriaco, C.; Pirritano, D.; Tomaiuolo, F.; Mangone, G.; Trotta, M.; Talarico, T.; et al. Computer-assisted cognitive rehabilitation of attention deficits for multiple sclerosis: A randomized trial with fMRI correlates. Neurorehabil. Neural Repair 2013, 27, 284–295. [Google Scholar] [CrossRef]
- Evensen, S.; Sletvold, O.; Lydersen, S.; Taraldsen, K. Physical activity among hospitalized older adults–An observational study. BMC Geriatr. 2017, 17, 1–8. [Google Scholar] [CrossRef]
- Hacker, R.L.; Hardy, A.O.; Webster, J.; Xue (Yidan), Z.; Horan, J.J.; Atkinson, R.K.; Homer, J. The Impact of Ethnically Matched Animated Agents (Avatars) in the Cognitive Restructuring of Irrational Career Beliefs Held by Young Women. Int. J. Cyber Behav. Psychol. Learn. 2015, 5, 1–12. [Google Scholar] [CrossRef]
- Seeing Machines. Available online: https://www.seeingmachines.com/ (accessed on 13 March 2019).
- Miotto, R.; Wang, F.; Wang, S.; Jiang, X.; Dudley, J.T. Deep learning for healthcare: Review, opportunities and challenges. Brief. Bioinform. 2018, 19, 1236–1246. [Google Scholar] [CrossRef]





| Categories | Terms |
|---|---|
| General | Brain Health; Cognitive |
| Associated | Older Adults; Aging; Ageing; Elderly; Geriatrics; Young elders; Aged; Older Person |
| Pillars | Nutrition; Physical exercise; Cognition; Social; Purpose in life; General health; Diet; Physical activity; Cognitive activity; Socialization; Psychological wellbeing; Comprehensive health; Physical; Cognitive; Cognitive training; Vital plan; Mindfulness; Rest; Sleep; Sleeping; Relax; Global health |
| Techniques | Exercise; Coach; Intervention; Coaching; Treatment; Monitoring; Adherence; Motivation |
| Technologies | Wearable; Computer; ICT 1; Machine learning; Data mining; RMT 2; Data mining; Artificial intelligence; Deep Learning; eHealth; mHealth; Biosensor; Neuronal network; Predictor; Mobile; Smartphone; Technology |
| First Author, Year | Region | Variable | Study Design/Study Duration | Methodology and Technologies | Sample Size | Age Groups | Feedback Loop/End-User | Results | Funding Body |
|---|---|---|---|---|---|---|---|---|---|
| Commissaris et al. (2014) [29] | Netherlands and Germany | Physical exercise | Cohort/1 working day (7–8 h) | Heart Rate Monitor/3D kinematics measurement system | 15 | 29 years (SD 12) | Office Workers and Employers | Neutral | German Social Accident Insurance (DGUV) |
| Mourad et al. (2016) [30] | Sweden | Life purpose 1 | RCT/4 weeks | Internet-delivered program with questionnaires | 15 | 22–76 | Self/User | Neutral | County Council of Östergötland/Medical Research of Southeast Sweden |
| D. Wirth et al. (2015) [31] | South Carolina (USA) | Nutrition | Cohort/14 days | Phone questionnaires | 430 | 21–35 | NR | Positive | Coca Cola Company |
| Pavel et al. (2016) [32] | NR | Life purpose 2 | RCT/25 weeks | Mobile phone | 204 | NR | Self/User | Positive | NR |
| Ramnath et al. (2018) [33] | South Africa | Physical exercise and cognitive activity | Cohort/1 session | Questionnaires & physical tasks | 70 | 65–84 | Self/User | Neutral | NR |
| Phatak et al. (2017) [34] | United States | Physical exercise | Cohort/14 weeks | Fitbit Zip/Mobile App/Personalization | 20 | 40–65 | Self/User | Positive | National Science Foundation |
| Lange et al. (2018) [35] | Germany | Nutrition | Cohort/2 years | Web App | 3000 | 41,5 (SD 11.9) | Self/User | Positive | German Ministry of Education and Research |
| Merriman et al. (2018) [36] | Ireland | Physical exercise | RCT/5 weeks | PC game/Wii Balance Board/Gamification/Serious Game | 70 | 65–84 | Self/User | Positive | European Commission Seventh Framework Programme ‘VERVE’ Project and by Principal Investigator award and TIDA award to FNN from Science Foundation Ireland |
| Roepke et al. (2015) [37] | World | Life purpose 3 | RCT/6 weeks | Smartphone-Based/Internet-Based Self-Help Tool | 283 | 40.15 (SD 12.4) | Self/User | Neutral | Private donation |
| Veronese et al. (2016) [38] | Italy | Physical exercise | Cohort/4.4 years | Data Analysis | 3099 | >65 | NR | Positive | Fondazione Cassa di Risparmio di Padova e Rovigo/University of Padova/Azienda Unità Locale Socio Sanitaria |
| Konstantinidis et al. (2014) [39] | Europe | Physical exercise | Cohort/7–8 weeks | Serious Game/Computer application/Data analysis/Exergaming/Wii Balance Board | 116 | >65 | Self/User | Positive | European Union |
| Rodrigues et al. (2017) [40] | Portugal | Nutrition and Physical exercise | RCT/6 months | TV app | 282 | >60 | Self/User | NR | European Economic Area |
| Zielhorst et al. (2015) [41] | Netherlands | Life purpose 4 | Cohort/10–15 days | CBT/Gamification | 101 | 24–63 | Self/User | Positive | NR |
| Vercelli et al. (2017) [42] | Europe, Australia, and Asia | Life purpose 5 | NR | Smartphone app/wearables | NR | >65 | Self/User | NR | European Union |
| Robertson et al. (2015) [43] | United States | Cognitive activity | RCT/1 h | Mobile app/Motion sensors/Real Time Annotation Tool | 42 | 19.88 | Self/User | Positive | National Science Foundation |
| First Author, Year | Region | Variable | Study Design/Study Duration | Methodology and Technologies | Sample Size | Age Groups | Feedback Loop/End-User | Results | Funding Body | Exclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| Robert et al. (2013) [45] | France and Taiwan | Physical exercise | Cohort/1 day | Intelligent room (2D video camera, ambiance microphone, motion sensor, and tri-axial accelerometer mounted on the shoes) | 64 | >65 | Therapist | Positive | Innovation Alzheimer and ARMEP associations | Alzheimer |
| Chen et al. (2013) [46] | Australia | Cognitive activity | Cohort/1 session | FaceLAB for pupil dilation and position | 15 | 20–48 | Therapist | Negative | Australian Government | No Brain Health |
| Cerasa et al. (2014) [47] | Italy | Cognitive activity | RCT/6 weeks | RehaCom (Cognitive training tasks), 3T Scanner for images | 20 | 61.1 (12.4 SD) | Therapist | Positive | Ministerio Univesita’ e Ricerca | Parkinson |
| Baglio et al. (2015) [48] | Italy | Stress. Multidisciplinary intervention | RCT/32 Weeks | fMRI and questionnaires | 60 | 65–85 | Therapist | Positive | Ricerca Corrente (Italian Ministry of Health) | Alzheimer |
| Manzoni et al. (2016) [49] | Italy | Habits | RCT/11 weeks | Virtual Reality/CBT | 158 | 18–50 | Self/Patient | Positive | NR | Obese people |
| Mehrabian et al. (2018) [50] | France | Intervention | Cohort/40 min | Interviews + web app | 92 | 54–85 | Patient/Caregiver | Positive | National Research Agency and the Foundation Mederic Alzheimer | Cognitively impaired/caregivers |
| Cerasa et al. (2013) [51] | Italy | Cognitive Function | RCT/6 weeks | fMRI/cognitive computerized tasks | 26 | 32 (SD 10) | Clinicians | Positive | Fondazione Italiana Sclerosi Multipla onlus and Ministero Universita’ e Ricerca | Multiple sclerosis |
| Evensen et al. (2017) [52] | Norway | Physical Activity | Cohort/3 months | accelerometers/activePal | 38 | 82.9 (SD 6.3) | Clinicians | Positive | Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology | Hospitalized patients |
| Hacker et al. (2015) [53] | USA | Personalization | Cohort/4, 20 days | Web application | 176 | 11 to 15 | Self/User | Positive | National Science Foundation | Not health-oriented |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Blanco, D.; Solana-Sánchez, J.; Sánchez-González, P.; Oropesa, I.; Cáceres, C.; Cattaneo, G.; Tormos-Muñoz, J.M.; Bartrés-Faz, D.; Pascual-Leone, Á.; Gómez, E.J. Technologies for Monitoring Lifestyle Habits Related to Brain Health: A Systematic Review. Sensors 2019, 19, 4183. https://doi.org/10.3390/s19194183
Moreno-Blanco D, Solana-Sánchez J, Sánchez-González P, Oropesa I, Cáceres C, Cattaneo G, Tormos-Muñoz JM, Bartrés-Faz D, Pascual-Leone Á, Gómez EJ. Technologies for Monitoring Lifestyle Habits Related to Brain Health: A Systematic Review. Sensors. 2019; 19(19):4183. https://doi.org/10.3390/s19194183
Chicago/Turabian StyleMoreno-Blanco, Diego, Javier Solana-Sánchez, Patricia Sánchez-González, Ignacio Oropesa, César Cáceres, Gabriele Cattaneo, Josep M. Tormos-Muñoz, David Bartrés-Faz, Álvaro Pascual-Leone, and Enrique J. Gómez. 2019. "Technologies for Monitoring Lifestyle Habits Related to Brain Health: A Systematic Review" Sensors 19, no. 19: 4183. https://doi.org/10.3390/s19194183





