Sequential Total Variation Denoising for the Extraction of Fetal ECG from Single-Channel Maternal Abdominal ECG
Abstract
:1. Introduction
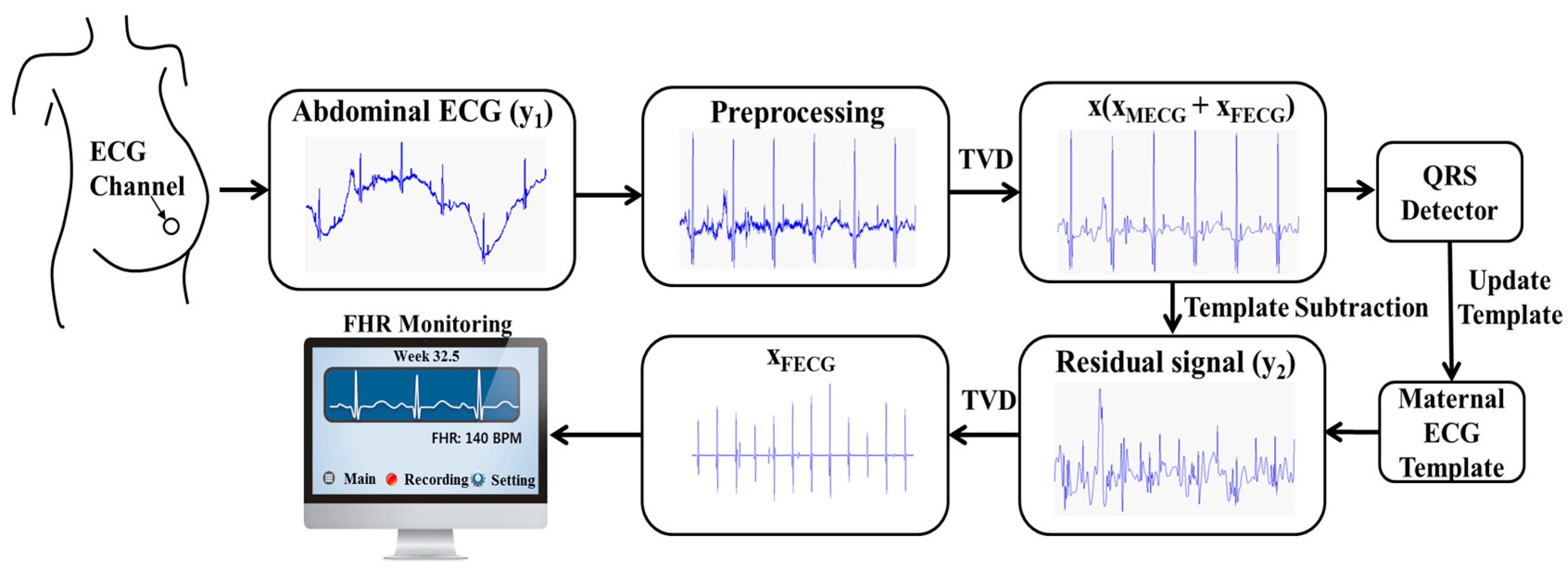
2. Methods
2.1. Preprocessing
2.2. Proposed Method: Sequential TVD with TSPCA
2.2.1. First TVD: Enhancing the Abdominal ECG
- Set i = 0, initialize .
- Choose Li(x) such that
- (1)
- for all
- (2)
- Set as the minimizer of ,
- Set i = i + 1 and go back to step 2.
2.2.2. TSPCA: Elimination of Maternal ECG
2.2.3. Second TVD: Extracting Fetal ECG
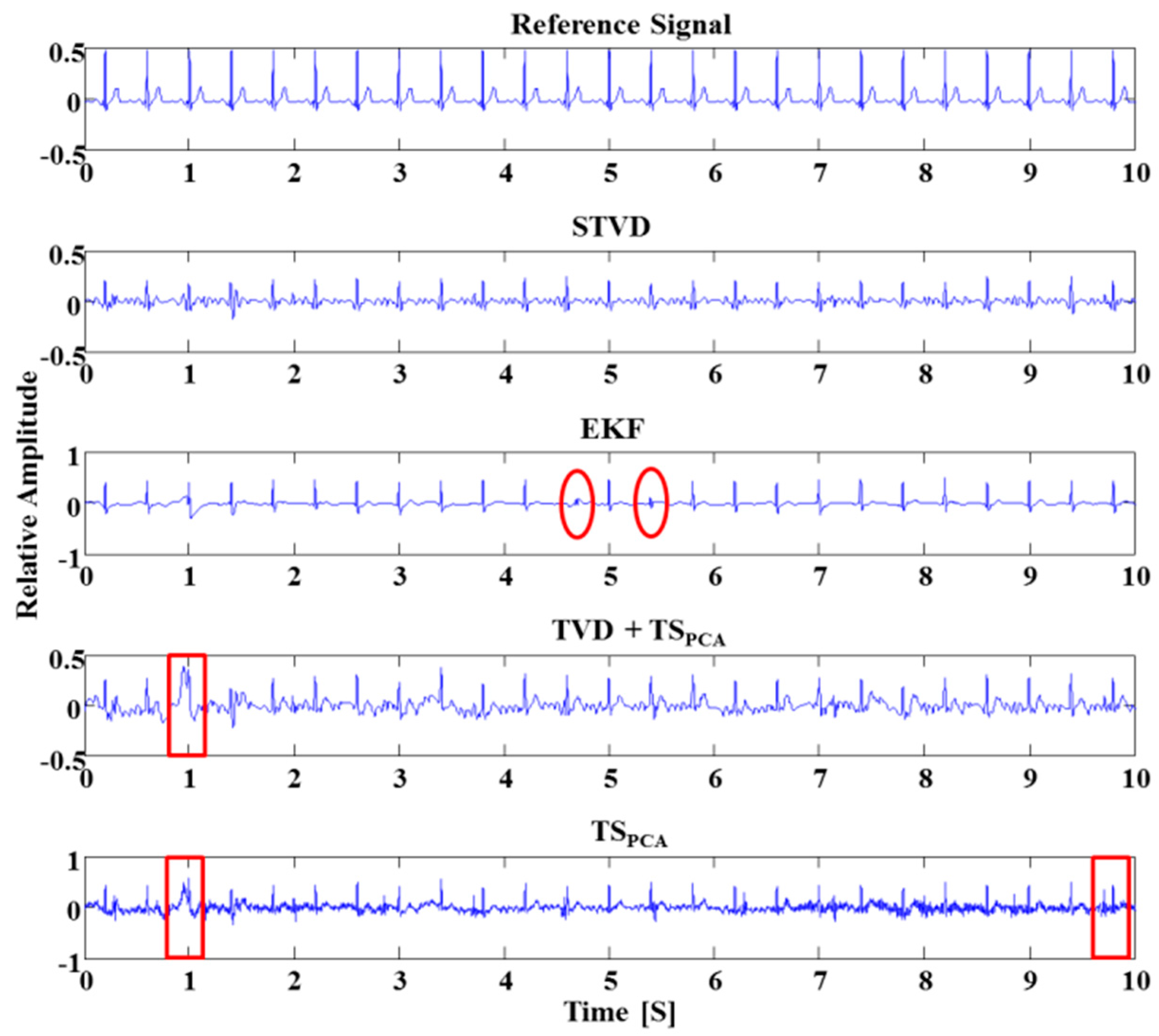
2.3. Methods for Comparison
2.3.1. Extended Kalman Filter
2.3.2. TVD + TSPCA
2.3.3. TSPCA
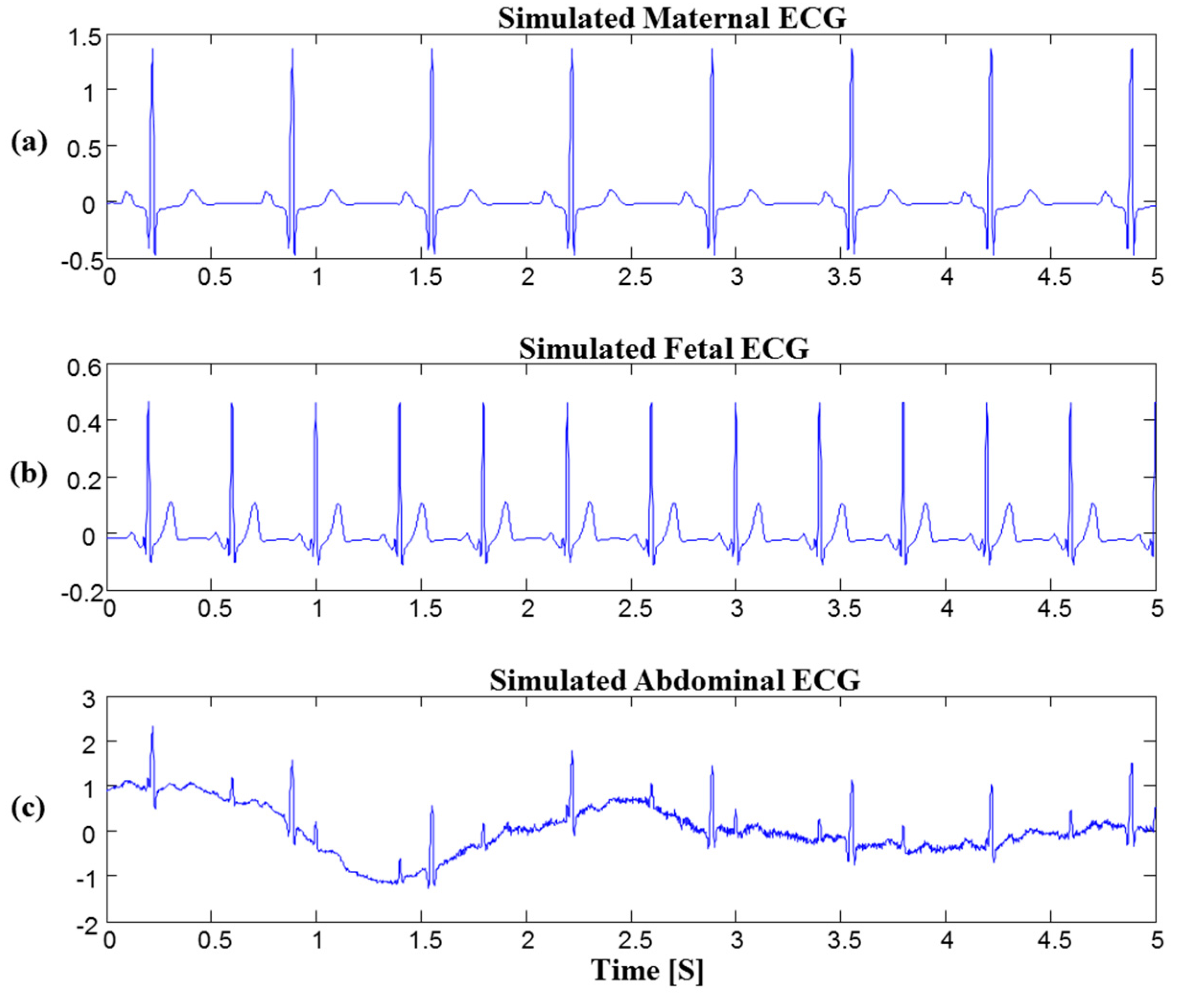
2.4. Data
2.5. Evaluation and Detection of Fetal ECG R-Peak
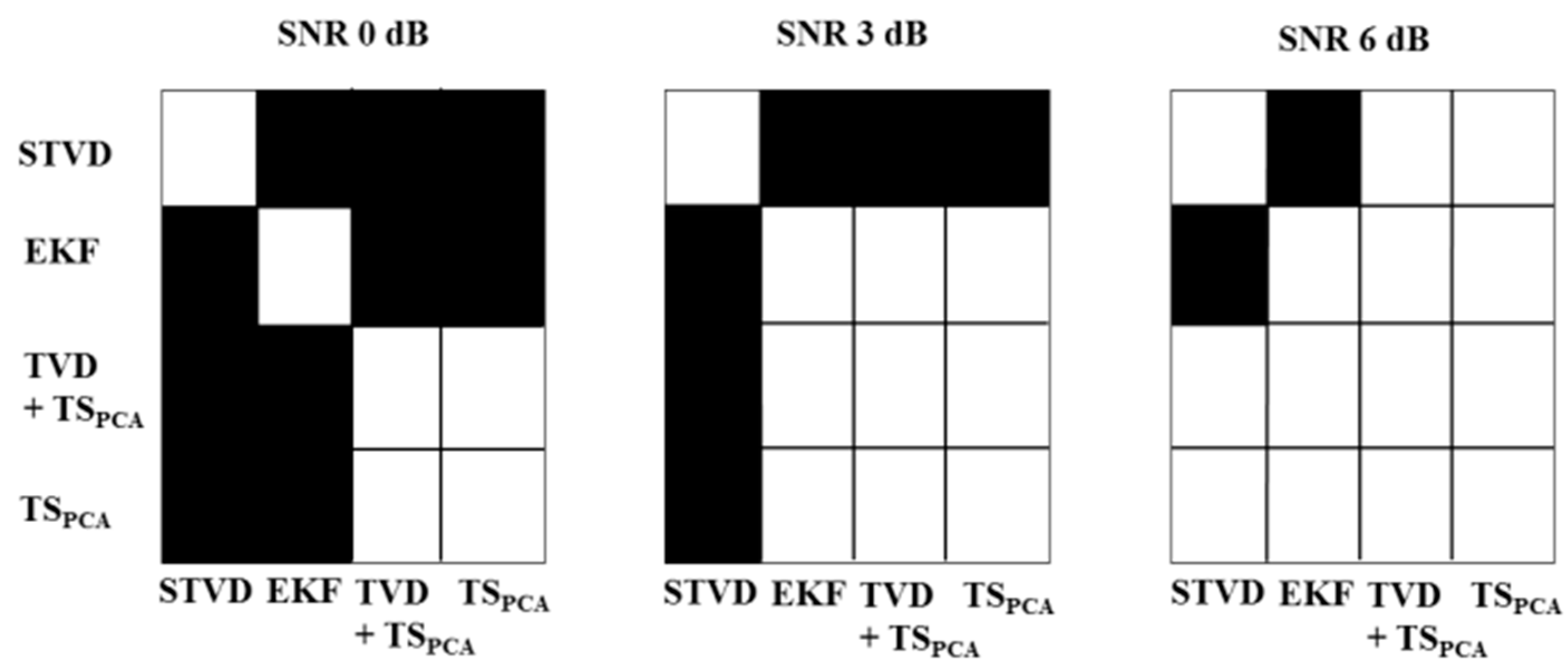
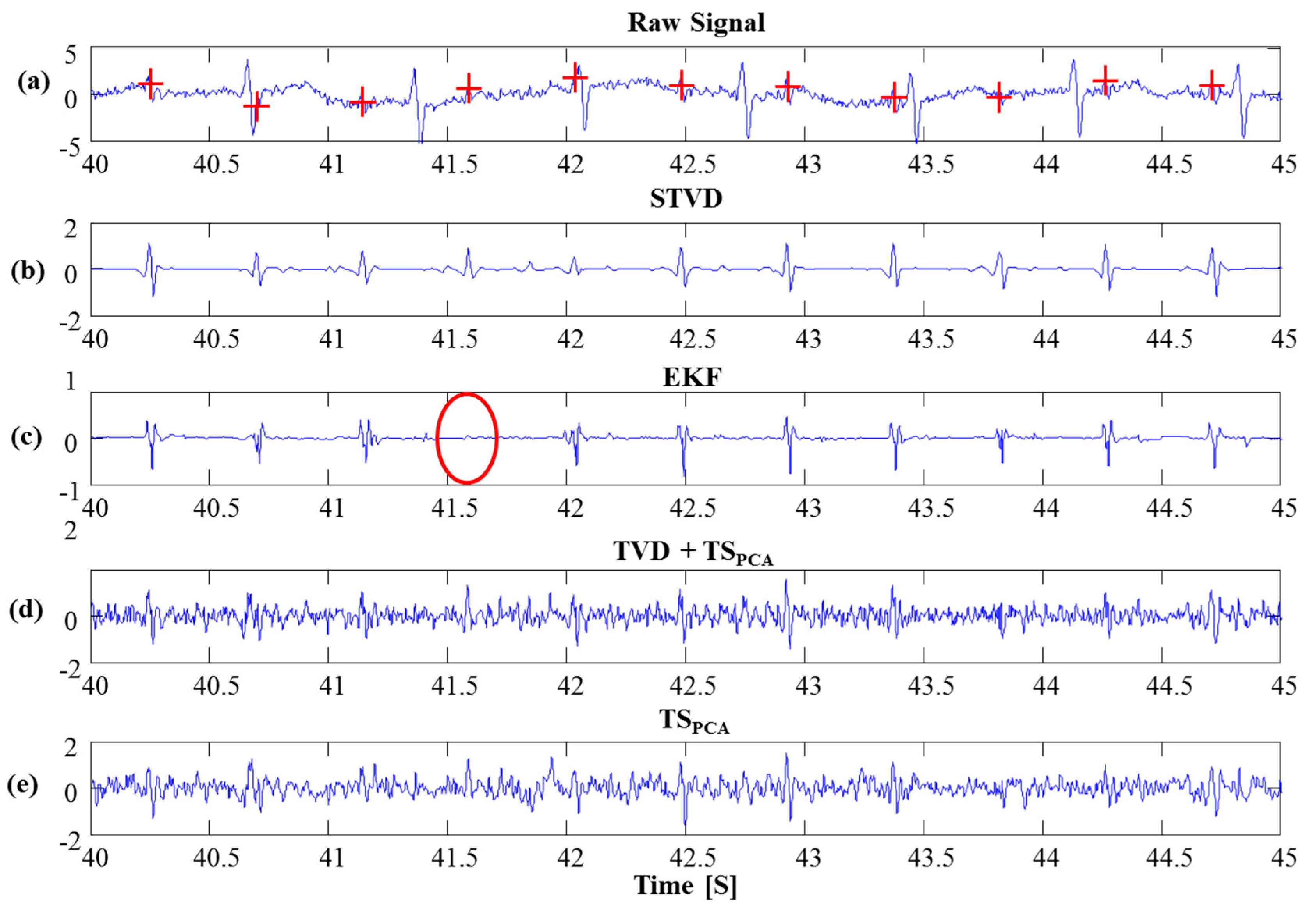
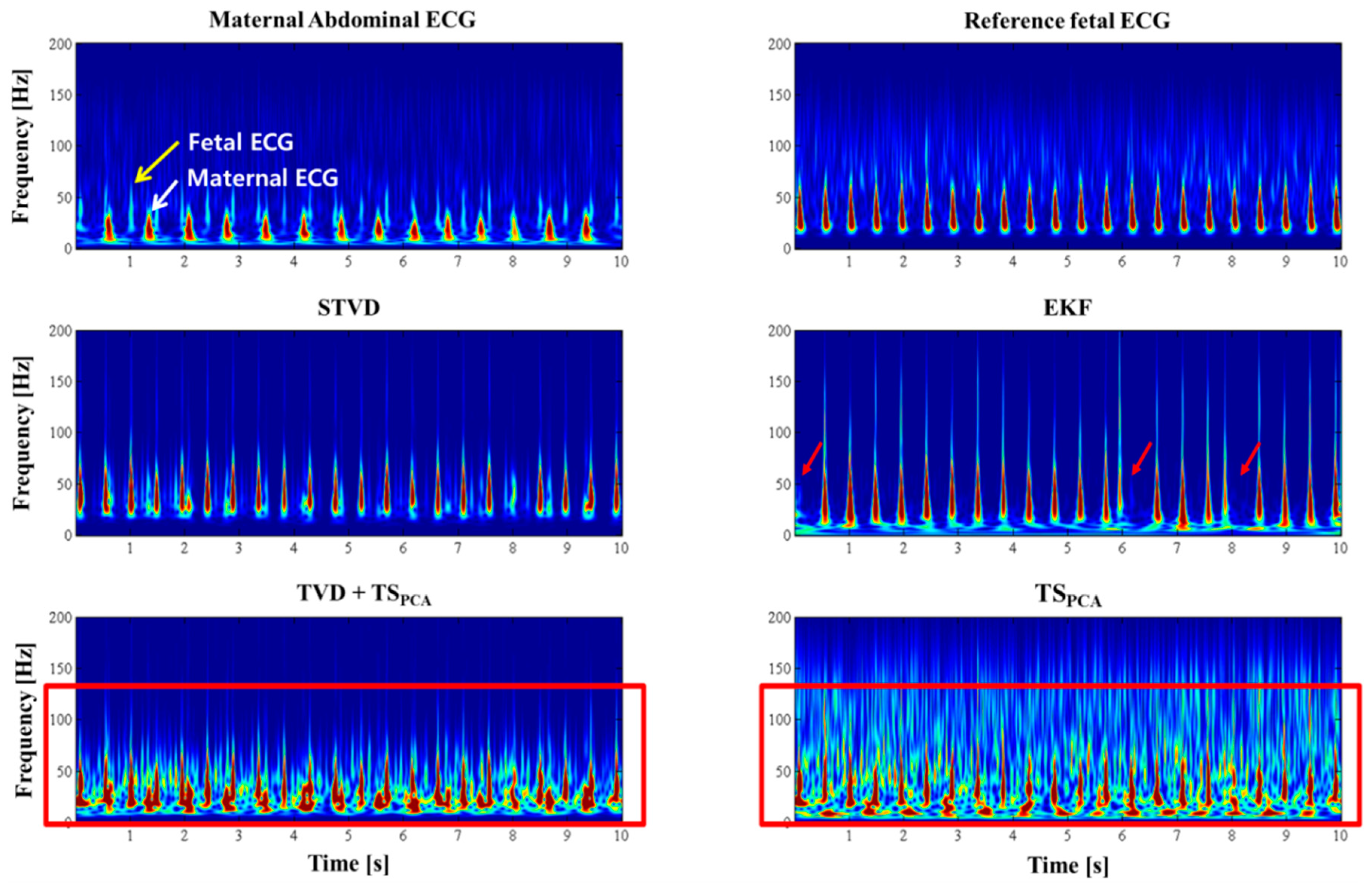
3. Results
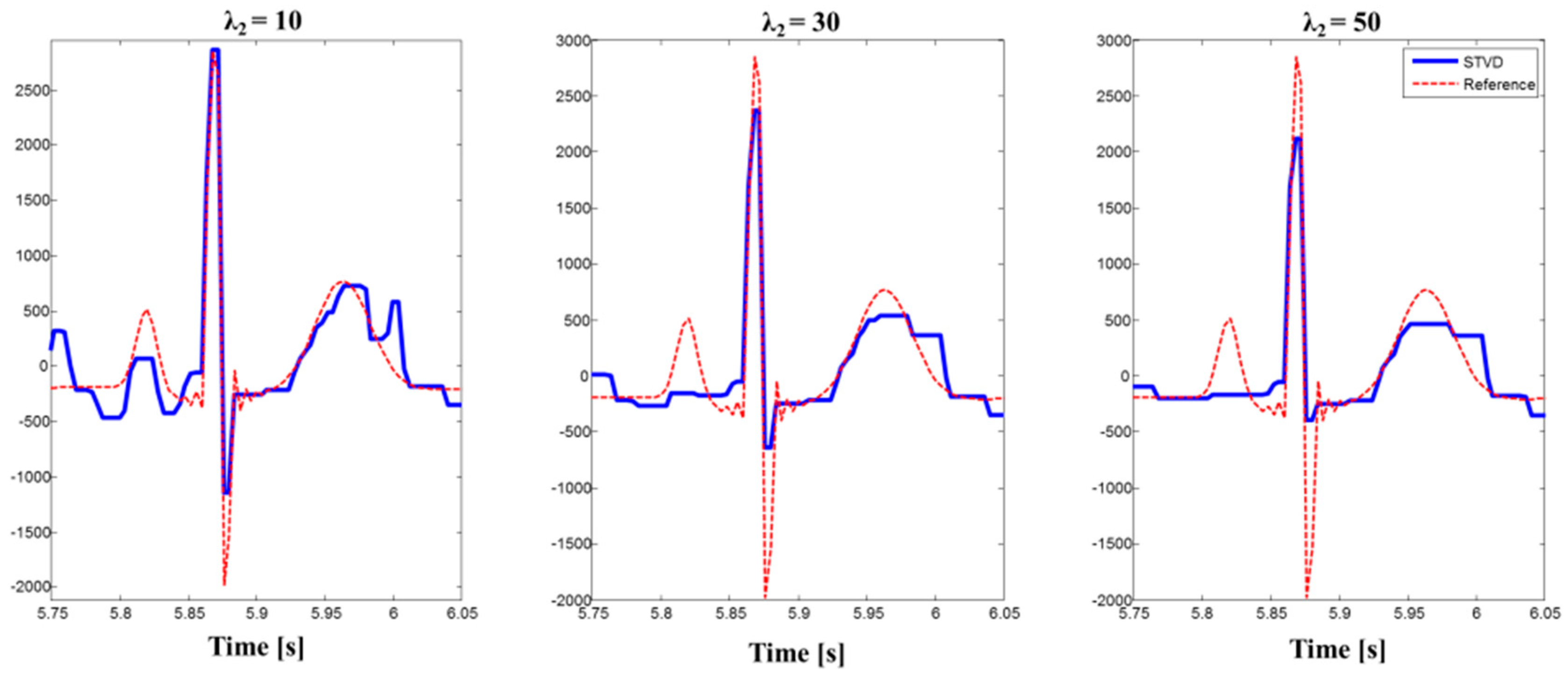
3.1. Parameter Optimization
3.2. Simulation
3.3. PhysioNet Database
4. Discussion and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| FHR | Fetal Heart Rate |
| ECG | Electrocardiograms |
| STVD | Sequential total variation denoising |
| TVD | Total variation denoising |
| ICA | Independent component analysis |
| PCA | Principle component analysis |
| TS | Template subtraction |
| EKF | Extended Kalman filter |
| MAE | Mean absolute error |
| Se | Sensitivity |
| PPV | Positive predictive value |
| SNR | Signal-to-noise ratio |
References
- Parer, J.T. Handbook of Fetal Heart Rate Monitoring; W. B. Saunders Company: Philadelphia, PA, USA, 1997. [Google Scholar]
- Peters, M.; Crowe, J.; Piéri, J.-F.; Quartero, H.; Hayes-Gill, B.; James, D.; Stinstra, J.; Shakespeare, S. Monitoring the fetal heart non-invasively: A review of methods. J. Perinat. Med. 2005, 29, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Jezewski, J.; Roj, D.; Wrobel, J.; Horoba, K. A novel technique for fetal heart rate estimation from Doppler ultrasound signal. Biomed. Eng. Online. 2011, 10. [Google Scholar] [CrossRef] [PubMed]
- Ibrahimy, M.I.; Ahmed, F.; Ali, M.A.M.; Zahedi, E. Real-time signal processing for fetal heart rate monitoring. IEEE Trans. Biomed. Eng. 2003, 50, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Assaleh, K.; Al-Nashash, H. A novel technique for the extraction of fetal ECG using polynomial networks. IEEE Trans. Biomed. Eng. 2005, 52, 1148–1152. [Google Scholar] [CrossRef] [PubMed]
- Wua, S.; Shen, Y.; Zhou, Z.; Lin, L.; Zeng, Y.; Gao, X. Research of fetal ECG extraction using wavelet analysis and adaptive filtering. Comput. Biol. Med. 2013, 43, 1622–1627. [Google Scholar] [CrossRef] [PubMed]
- Lathauwer, L.; De Moor, B.; Vandewalle, J. Fetal electrocardiogram extraction by blind source subspace separation. IEEE Trans. Biomed. Eng. 2000, 47, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Hyvärinen, A.; Karhunen, J.; Oja, E. Independent Component Analysis; Wiley: New York, NY, USA, 2001. [Google Scholar]
- Podziemski, P.; Gieraltowski, J. Fetal heart rate discovery: algorithm for detection of fetal heart rate from noisy, noninvasive fetal ECG recordings. In Proceedings of the 2013 Computing in Cardiology Conference (CinC), Zaragoza, Spain, 22–25 September 2013; pp. 333–336.
- Behar, J.; Oster, J.; Clifford, G.D. Combining and benchmarking methods of foetal ECG extraction without maternal or scalp electrode data. Physiol. Meas. 2014, 35. [Google Scholar] [CrossRef] [PubMed]
- Niknazar, M.; Rivet, B.; Jutten, C. Fetal ECG extraction by extended state Kalman filtering based on single-channel recordings. IEEE Trans. Biomed. Eng. 2013, 60, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Akhbari, M.; Niknazar, M.; Jutten, C.; Shamsollahi, M.B.; Rivet, B. Fetal electrocardiogram R-peak detection using robust tensor decomposition and extended Kalman filtering. In Proceedings of the 2013 Computing in Cardiology Conference (CinC), Zaragoza, Spain, 22–25 September 2013; pp. 189–192.
- Sameni, R. Extraction of Fetal Cardiac Signals from an Array of Maternal Abdominal Recordings. Ph.D. Thesis, Sharif University of Technology, Tehran, Iran, 2008. [Google Scholar]
- Andreotti, F.; Riedl, M.; Himmelsbach, T.; Wedekind, D.; Zaunseder, S.; Wessel, N.; Malberg, H. Maternal signal estimation by Kalman filtering and template adaptation for fetal heart rate extraction. In Proceedings of the 2013 Computing in Cardiology Conference (CinC), Zaragoza, Spain, 22–25 September 2013; pp. 193–196.
- Castillo, E.; Morales, D.P.; Botella, G.; García, A.; Parrilla, L.; Palma, A.J. Efficient wavelet-based ECG processing for single-lead FHR extraction. Digit. Signal Prog. 2013, 23, 1897–1909. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression shrinkage and selection via the LASSO. J. R. Stat. Soc. Ser. B 2008, 58, 267–288. [Google Scholar]
- Chen, S.S.; Donoho, D.L.; Saunders, A.M. Atomic decomposition by basispursuit. SIAM J. Sci. Comput. 1998, 20, 33–61. [Google Scholar] [CrossRef]
- Rudin, L.I.; Osher, S.; Fatemi, E. Nonlinear total variation based noise removal algorithms. Phys. D Nonlinear Phenom. 1992, 60, 259–268. [Google Scholar] [CrossRef]
- Ning, X.R.; Selesnick, I.W. ECG enhancement and QRS detection based on Sparse derivatives. Biomed. Signal Process. Control 2013, 8, 713–723. [Google Scholar] [CrossRef]
- Andreotti, F.; Behar, J.; Zaunseder, S.; Oster, J.; Clifford, G.D. An open-source framework for stress-testing non-invasive foetal ECG extraction algorithms. Physiol. Meas. 2016, 37, 627. [Google Scholar] [CrossRef] [PubMed]
- Behar, J.; Andreotti, F.; Zaunseder, S.; Oster, J.; Clifford, G.D. A practical guide to non-invasive foetal electrocardiogram extraction and analysis. Physiol. Meas. 2016, 37. [Google Scholar] [CrossRef]
- Silva, I.; Behar, J.; Sameni, R.; Zhu, T.; Oster, J.; Clifford, G.D.; Moody, G.B. Noninvasive fetal ECG: The physionet/computing in cardiology challenge 2013. In Proceedings of the IEEE In Computing in Cardiology Conference (CinC), Zaragoza, Spain, 22–25 September 2013; pp. 149–152.
- Figueiredo, M.A.; Bioucas-Dias, J.M.; Nowak, R.D. Majorization-minimization algorithms for wavelet-based image restoration. IEEE Trans. Image Process. 2007, 16, 2980–2991. [Google Scholar] [CrossRef] [PubMed]
- McSharry, P.E.; Clifford, G.D.; Tarassenko, L.; Smith, L.A. A dynamical model for generating synthetic electrocardiogram signals. IEEE Trans. Biomed. Eng. 2003, 50, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Kanjilal, P.P.; Palit, S.; Saha, G. Fetal ECG extraction from single-channel maternal ECG using singular value decomposition. IEEE Trans. Biomed. Eng. 1997, 44, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Behar, J.; Andreotti, F.; Zaunseder, S.; Li, Q.; Oster, J.; Clifford, G.D. An ECG simulator for generating maternal-foetal activity mixtures on abdominal ECG recordings. Physiol. Meas. 2014, 35, 1537. [Google Scholar] [CrossRef] [PubMed]
- Das, M.K.; Ari, S. Analysis of ECG signal denoising method based on S-transform. IRBM 2013, 34, 362–370. [Google Scholar] [CrossRef]
- Niknazar, M.; Rivet, B.; Jutten, C. Fetal ECG extraction from a single sensor by a non-parametric modeling. In Proceedings of the 20th European Signal Processing Conference (EUSIPCO), Bucharest, Romania, 27–31 August 2012; pp. 949–953.
- Pant, J.; Krishnan, S. Reconstruction of ECG signals for compressive sensing by promoting sparsity on the gradient. In Proceedings of the IEEE International Conference on In Acoustics, Speech and Signal Processing (ICASSP), Vancouver, BC, Canada, 26–31 May 2013; pp. 993–997.


| Case | Description |
|---|---|
| Baseline (B) | Abdominal ECG without any noise or events (maternal ECG + fetal ECG) |
| Case 0 (C0) | Baseline (no events) + noise |
| Case 1 (C1) | Fetal movement noise + noise |
| Case 2 (C2) | Acceleration or deceleration of maternal and fetal heart rate + noise |
| Case 3 (C3) | Uterine contraction + noise |
| Case 4 (C4) | Ectopic beats of maternal and fetal + noise |
| Case 5 (C5) | Twin + noise |
| Method | Parameters | FECGSYNDB | Set-a | ||||
|---|---|---|---|---|---|---|---|
| 0 dB | 3 dB | 6 dB | 9 dB | 12 dB | |||
| STVD | λ1 | 34 | 12 | 4 | 1 | 1 | 4 |
| λ2 | 16 | 9 | 2 | 1 | 1 | 3 | |
| EKF | GQ | 10 | 5 | 2 | 1 | 1 | 5 |
| GR | 84 | 75 | 10 | 1 | 1 | 100 | |
| TSPCA | The number of maternal ECG cycles | 23 | 23 | 15 | 14 | 14 | 20 |
| Method | Baseline | Case 0 | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Total |
|---|---|---|---|---|---|---|---|---|
| STVD | 100 (0.0) | 98.4 (4.3) | 99.4 (8.9) | 98.5 (9.5) | 80.2 (11.5) | 90.6 (5.9) | 97.5 (4.2) | 97.2 (9.9) |
| EKF | 100 (0.2) | 98.1 (9.9) | 98.8 (8.2) | 98.2 (9.6) | 77.8 (10.0) | 83.4 (7.3) | 94.5 (24.8) | 94.5 (19.8) |
| TVD + TSPCA | 100 (0.0) | 97.8 (8.7) | 99.4 (5.1) | 98.1 (8.0) | 78.7 (10.2) | 88.6 (17.2) | 95.9 (16.8) | 96.1 (24.8) |
| TSPCA | 100 (0.0) | 98.3 (9.9) | 99.2 (7.6) | 98.7 (9.3) | 77.5 (10.2) | 88.4 (10.8) | 94.9 (23.2) | 96 (18.5) |
| Method | Baseline | Case 0 | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Total |
|---|---|---|---|---|---|---|---|---|
| STVD | 3.3 (2.0) | 3.6 (1.9) | 3.7 (0.2) | 3.2 (1.3) | 4.5 (0.4) | 3.2 (3.6) | 3.3 (3.5) | 3.9 (2.2) |
| EKF | 4.5 (6.3) | 3.8 (4.4) | 3.1 (0.9) | 3.1 (1.1) | 3.9 (1.6) | 4.8 (1.4) | 3.5 (3.7) | 3.8 (2.7) |
| TVD + TSPCA | 3.4 (3.6) | 5.2 (3.5) | 5.1 (2.8) | 5.5 (3.3) | 4.2 (3.6) | 3.4 (2.0) | 3.8 (2.7) | 4.2 (2.1) |
| TSPCA | 4 (2.0) | 4.2 (2.1) | 4.2 (0.6) | 4.1 (0.8) | 4.7 (1.1) | 5.6 (0.8) | 4.3 (1.8) | 4.4 (1.6) |
| Method | TP | FN | FP | Se (%) | PPV (%) | F1 (%) | MAE (ms) |
|---|---|---|---|---|---|---|---|
| STVD | 9162 | 946 | 1072 | 90.5 | 89.4 | 89.9 | 9.3 |
| EKF | 7989 | 1719 | 1984 | 82.2 | 80.1 | 81.1 | 7.9 |
| TVD + TSPCA | 8519 | 1189 | 1246 | 87.7 | 87.2 | 87.4 | 16.4 |
| TSPCA | 8475 | 1233 | 1367 | 87.2 | 86.1 | 86.7 | 14.3 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.J.; Lee, B. Sequential Total Variation Denoising for the Extraction of Fetal ECG from Single-Channel Maternal Abdominal ECG. Sensors 2016, 16, 1020. https://doi.org/10.3390/s16071020
Lee KJ, Lee B. Sequential Total Variation Denoising for the Extraction of Fetal ECG from Single-Channel Maternal Abdominal ECG. Sensors. 2016; 16(7):1020. https://doi.org/10.3390/s16071020
Chicago/Turabian StyleLee, Kwang Jin, and Boreom Lee. 2016. "Sequential Total Variation Denoising for the Extraction of Fetal ECG from Single-Channel Maternal Abdominal ECG" Sensors 16, no. 7: 1020. https://doi.org/10.3390/s16071020
APA StyleLee, K. J., & Lee, B. (2016). Sequential Total Variation Denoising for the Extraction of Fetal ECG from Single-Channel Maternal Abdominal ECG. Sensors, 16(7), 1020. https://doi.org/10.3390/s16071020






