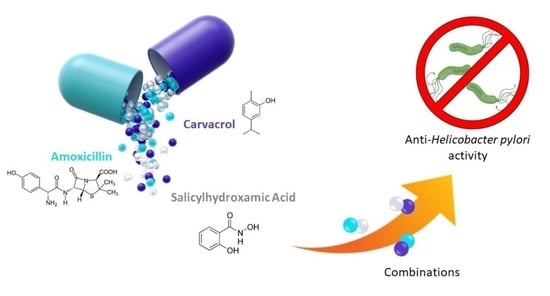
Antimicrobial and Antibiofilm Activities of Carvacrol, Amoxicillin and Salicylhydroxamic Acid Alone and in Combination vs. Helicobacter pylori: Towards a New Multi-Targeted Therapy
Abstract
:1. Introduction
2. Results
2.1. MIC and MBC Determination of Carvacrol, Amoxicillin and Salicylhydroxamic Acid, Alone and in Combination with the Checkerboard Method
2.2. Time Killing Assay
2.3. MBEC Determination of Carvacrol, Amoxicillin and Salicylhydroxamic Acid, Alone and in Combination vs. H. pylori
2.3.1. Combination of Carvacrol and Amoxicillin (CAR-AMX)
2.3.2. Combination of Carvacrol and Salicylhydroxamic Acid (CAR-SHA)
2.3.3. Combination of Salicylhydroxamic Acid and Amoxicillin (SHA-AMX)
2.4. MBIC of Carvacrol, Amoxicillin and Salicylhydroxamic Acid, Alone and in Combination, vs. H. pylori ATCC 43504/NCTC11637
2.5. Effects of Carvacrol, Amoxicillin and Salicylhydroxamic Acid, Alone and in Combination, on H. pylori Ultrastructure
3. Discussion
4. Materials and Methods
4.1. Bacterial Strain and Media
4.2. Antimicrobial Activity of Carvacrol, Amoxicillin and Salicylhydroxamic Acid vs. H. pylori ATCC 43504
- (1)
- FICI = FICA + FICB;
- (2)
- FICA = (MICAcomb/MICAalone) and FICB = (MICBcomb/MICBalone), where MICAcomb and MICBcomb are the MIC values of the drugs A and B, respectively, in the combination AB and MICAalone and MICBalone are the MIC values of the drugs A and B individually evaluated;
- (3)
- FBCI = FBCA + FBCB;
- (4)
- FBCI = (MBCAcomb/MBCAalone) + (MBCBcomb/MBCBalone), where MBCAcomb and MBCBcomb are the MBC values of the drugs A and B, respectively, in the combination AB and MBCAalone and MBCBalone are the MBC values of the drugs A and B individually evaluated.
4.3. Time Killing Assay of CAR, AMX and SHA and their Combinations vs. H. pylori ATCC 43504
4.4. Antibiofilm Activity of Carvacrol, Amoxicillin and Salicylhydroxamic Acid, Alone and in Combination, vs. H. pylori ATCC 43504/NCTC11637
4.5. TEM Analysis of H. pylori Treated with CAR, AMX, SHA and Their Combinations CAR-AMX, CAR-SHA and SHA-AMX
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Argueta, E.A.; Moss, S.F. The Prevention of Gastric Cancer by Helicobacter pylori Eradication. Curr. Opin. Gastroenterol. 2021, 37, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Piscione, M.; Mazzone, M.; Di Marcantonio, M.C.; Muraro, R.; Mincione, G. Eradication of Helicobacter pylori and Gastric Cancer: A Controversial Relationship. Front. Microbiol. 2021, 12, 630852. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Yuan, Y.; Moayyedi, P. Helicobacter pylori Eradication Therapy to Prevent Gastric Cancer: Systematic Review and Meta-Analysis. Gut 2020, 69, 2113–2121. [Google Scholar] [CrossRef]
- Grande, R.; Perez, G.I.P. Editorial: Keep Calm and Care for Your Microbiota: The Role of H. pylori and Microbiota in Gastric Diseases. Front. Microbiol. 2021, 12, 692472. [Google Scholar] [CrossRef] [PubMed]
- Cellini, L.; Del Vecchio, A.; Di Candia, M.; Di Campli, E.; Favaro, M.; Donelli, G. Detection of free and plankton-associated Helicobacter pylori in seawater. J. Appl. Microbiol. 2004, 97, 285–292. [Google Scholar] [CrossRef]
- Grande, R.; Puca, V.; Muraro, R. Antibiotic Resistance and Bacterial Biofilm. Expert Opin. Ther. Pat. 2020, 30, 897–900. [Google Scholar] [CrossRef]
- Megraud, F.; Bruyndonckx, R.; Coenen, S.; Wittkop, L.; Huang, T.-D.; Hoebeke, M.; Bénéjat, L.; Lehours, P.; Goossens, H.; Glupczynski, Y. Helicobacter pylori Resistance to Antibiotics in Europe in 2018 and Its Relationship to Antibiotic Consumption in the Community. Gut 2021, 70, 1815–1822. [Google Scholar] [CrossRef]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of Antibiotic Resistance in Helicobacter pylori: A Systematic Review and Meta-Analysis in World Health Organization Regions. Gastroenterology 2018, 155, 1372–1382.e17. [Google Scholar] [CrossRef] [Green Version]
- Marzio, L.; Cellini, L.; Amitrano, M.; Grande, R.; Serio, M.; Cappello, G.; Grossi, L. Helicobacter pylori Isolates from Proximal and Distal Stomach of Patients Never Treated and Already Treated Show Genetic Variability and Discordant Antibiotic Resistance. Eur. J. Gastroenterol. Hepatol. 2011, 23, 467–472. [Google Scholar] [CrossRef]
- Percival, S.L.; Suleman, L. Biofilms and Helicobacter pylori: Dissemination and Persistence within the Environment and Host. World J. Gastrointest. Pathophysiol. 2014, 5, 122–132. [Google Scholar] [CrossRef]
- Krzyżek, P.; Grande, R.; Migdał, P.; Paluch, E.; Gościniak, G. Biofilm Formation as a Complex Result of Virulence and Adaptive Responses of Helicobacter pylori. Pathogens 2020, 9, 1062. [Google Scholar] [CrossRef]
- Krzyżek, P.; Migdał, P.; Grande, R.; Gościniak, G. Biofilm Formation of Helicobacter pylori in Both Static and Microfluidic Conditions Is Associated with Resistance to Clarithromycin. Front. Cell. Infect. Microbiol. 2022, 12, 868905. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori Infection—The Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: Https://Www.Who.Int/News/Item/27-02-2017-Who-Publishes-List-of-Bacteria-for-Which-New-Antibiotics-Are-Urgently-Needed (accessed on 27 February 2017).
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Biological Agents. Volume 100 B. A Review of Human Carcinogens. IARC Monogr. Eval. Carcinog. Risks Hum. 2012, 100, 1–441. [Google Scholar]
- Weeks, D.L.; Eskandari, S.; Scott, D.R.; Sachs, G. A H+-Gated Urea Channel: The Link between Helicobacter pylori Urease and Gastric Colonization. Science 2000, 287, 482–485. [Google Scholar] [CrossRef] [Green Version]
- Ansari, S.; Yamaoka, Y. Survival of Helicobacter pylori in Gastric Acidic Territory. Helicobacter 2017, 22, e12386. [Google Scholar] [CrossRef]
- Campestre, C.; De Luca, V.; Carradori, S.; Grande, R.; Carginale, V.; Scaloni, A.; Supuran, C.T.; Capasso, C. Carbonic Anhydrases: New Perspectives on Protein Functional Role and Inhibition in Helicobacter pylori. Front. Microbiol. 2021, 12, 629163. [Google Scholar] [CrossRef]
- Nishimori, I.; Minakuchi, T.; Morimoto, K.; Sano, S.; Onishi, S.; Takeuchi, H.; Vullo, D.; Scozzafava, A.; Supuran, C.T. Carbonic Anhydrase Inhibitors: DNA Cloning and Inhibition Studies of the α-Carbonic Anhydrase from Helicobacter pylori, a New Target for Developing Sulfonamide and Sulfamate Gastric Drugs. J. Med. Chem. 2006, 49, 2117–2126. [Google Scholar] [CrossRef]
- Morishita, S.; Nishimori, I.; Minakuchi, T.; Onishi, S.; Takeuchi, H.; Sugiura, T.; Vullo, D.; Scozzafava, A.; Supuran, C.T. Cloning, Polymorphism, and Inhibition of β-Carbonic Anhydrase of Helicobacter pylori. J. Gastroenterol. 2008, 43, 849–857. [Google Scholar] [CrossRef]
- Ronci, M.; Del Prete, S.; Puca, V.; Carradori, S.; Carginale, V.; Muraro, R.; Mincione, G.; Aceto, A.; Sisto, F.; Supuran, C.T.; et al. Identification and Characterization of the α-CA in the Outer Membrane Vesicles Produced by Helicobacter pylori. J. Enzym. Inhib. Med. Chem. 2019, 34, 189–195. [Google Scholar] [CrossRef] [Green Version]
- Rahman, M.M.; Tikhomirova, A.; Modak, J.K.; Hutton, M.L.; Supuran, C.T.; Roujeinikova, A. Antibacterial Activity of Ethoxzolamide against Helicobacter pylori Strains SS1 and 26695. Gut Pathog. 2020, 12, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maresca, A.; Vullo, D.; Scozzafava, A.; Supuran, C.T. Inhibition of the Alpha- and Beta-Carbonic Anhydrases from the Gastric Pathogen Helycobacter pylori with Anions. J. Enzym. Inhib. Med. Chem. 2013, 28, 388–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angeli, A.; Ferraroni, M.; Supuran, C.T. Famotidine, an Antiulcer Agent, Strongly Inhibits Helicobacter pylori and Human Carbonic Anhydrases. ACS Med. Chem. Lett. 2018, 9, 1035–1038. [Google Scholar] [CrossRef] [PubMed]
- Nishimori, I.; Minakuchi, T.; Kohsaki, T.; Onishi, S.; Takeuchi, H.; Vullo, D.; Scozzafava, A.; Supuran, C.T. Carbonic Anhydrase Inhibitors: The β-Carbonic Anhydrase from Helicobacter pylori Is a New Target for Sulfonamide and Sulfamate Inhibitors. Bioorganic Med. Chem. Lett. 2007, 17, 3585–3594. [Google Scholar] [CrossRef]
- Supuran, C.T.; Capasso, C. Antibacterial Carbonic Anhydrase Inhibitors: An Update on the Recent Literature. Expert Opin. Ther. Pat. 2020, 30, 963–982. [Google Scholar] [CrossRef]
- Modak, J.K.; Tikhomirova, A.; Gorrell, R.J.; Rahman, M.M.; Kotsanas, D.; Korman, T.M.; Garcia-Bustos, J.; Kwok, T.; Ferrero, R.L.; Supuran, C.T.; et al. Anti-Helicobacter pylori Activity of Ethoxzolamide. J. Enzym. Inhib. Med. Chem. 2019, 34, 1660–1667. [Google Scholar] [CrossRef] [Green Version]
- Angeli, A.; Pinteala, M.; Maier, S.S.; Del Prete, S.; Capasso, C.; Simionescu, B.C.; Supuran, C.T. Inhibition of Bacterial α-, β- and γ-Class Carbonic Anhydrases with Selenazoles Incorporating Benzenesulfonamide Moieties. J. Enzym. Inhib. Med. Chem. 2019, 34, 244–249. [Google Scholar] [CrossRef] [Green Version]
- Grande, R.; Di Marcantonio, M.C.; Robuffo, I.; Pompilio, A.; Celia, C.; Di Marzio, L.; Paolino, D.; Codagnone, M.; Muraro, R.; Stoodley, P.; et al. Helicobacter pylori ATCC 43629/NCTC 11639 Outer Membrane Vesicles (OMVs) from Biofilm and Planktonic Phase Associated with Extracellular DNA (eDNA). Front. Microbiol. 2015, 6, 1369. [Google Scholar] [CrossRef] [Green Version]
- Sharifi-Rad, M.; Varoni, E.M.; Iriti, M.; Martorell, M.; Setzer, W.N.; Del Mar Contreras, M.; Salehi, B.; Soltani-Nejad, A.; Rajabi, S.; Tajbakhsh, M.; et al. Carvacrol and Human Health: A Comprehensive Review. Phytother. Res. 2018, 32, 1675–1687. [Google Scholar] [CrossRef]
- Grande, R.; Carradori, S.; Puca, V.; Vitale, I.; Angeli, A.; Nocentini, A.; Bonardi, A.; Gratteri, P.; Lanuti, P.; Bologna, G.; et al. Selective Inhibition of Helicobacter pylori Carbonic Anhydrases by Carvacrol and Thymol Could Impair Biofilm Production and the Release of Outer Membrane Vesicles. Int. J. Mol. Sci. 2021, 22, 11583. [Google Scholar] [CrossRef]
- Sisto, F.; Carradori, S.; Guglielmi, P.; Traversi, C.B.; Spano, M.; Sobolev, A.P.; Secci, D.; Di Marcantonio, M.C.; Haloci, E.; Grande, R.; et al. Synthesis and Biological Evaluation of Carvacrol-Based Derivatives as Dual Inhibitors of H. pylori Strains and AGS Cell Proliferation. Pharmaceuticals 2020, 13, 405. [Google Scholar] [CrossRef]
- Phillips, K.; Munster, D.J.; Allardyce, R.A.; Bagshaw, P.F. Antibacterial Action of the Urease Inhibitor Acetohydroxamic Acid on Helicobacter pylori. J. Clin. Pathol. 1993, 46, 372–373. [Google Scholar] [CrossRef]
- Pathak, A.; Blair, V.L.; Ferrero, R.L.; Junk, P.C.; Tabor, R.F.; Andrews, P.C. Synthesis and Structural Characterisation of Bismuth(III) Hydroxamates and Their Activity against Helicobacter pylori. Dalton Trans. 2015, 44, 16903–16913. [Google Scholar] [CrossRef] [Green Version]
- Konieczna, I.; Żarnowiec, P.; Kwinkowski, M.; Kolesińska, B.; Frączyk, J.; Kamiński, Z.; Kaca, W. Bacterial Urease and Its Role in Long-Lasting Human Diseases. Curr. Protein Pept. Sci. 2012, 13, 789–806. [Google Scholar] [CrossRef] [Green Version]
- Debraekeleer, A.; Remaut, H. Future Perspective for Potential Helicobacter pylori Eradication Therapies. Future Microbiol. 2018, 13, 671–687. [Google Scholar] [CrossRef] [Green Version]
- Griffith, D.P.; Gleeson, M.J.; Lee, H.; Longuet, R.; Deman, E.; Earle, N. Randomized, Double-Blind Trial of Lithostat™ (Acetohydroxamic Acid) in the Palliative Treatment of Infection-Induced Urinary Calculi. Eur. Urol. 1991, 20, 243–247. [Google Scholar] [CrossRef]
- El-Nasr, A. SHAM Prophylaxis and Prevention of Recurrent Renal Stones; Cairo, Egypt, 1999. [Google Scholar]
- Broutet, N.; Tchamgoué, S.; Pereira, E.; Lamouliatte, H.; Salamon, R.; Mégraud, F. Risk Factors for Failure of Helicobacter pylori Therapy—Results of an Individual Data Analysis of 2751 Patients. Aliment. Pharmacol. Ther. 2003, 17, 99–109. [Google Scholar] [CrossRef]
- Muñoz, N.; Sánchez-Delgado, J.; Baylina, M.; López-Góngora, S.; Calvet, X. Prevalence of Helicobacter pylori Resistance after Failure of First-Line Therapy. A Systematic Review. Gastroenterol. Y Hepatol. Engl. Ed. 2018, 41, 654–662. [Google Scholar] [CrossRef]
- Hathroubi, S.; Zerebinski, J.; Ottemann, K.M. Helicobacter pylori Biofilm Cells Are Metabolically Distinct, Express Flagella, and Antibiotic Tolerant. biorXiv 2019, 728766. [Google Scholar] [CrossRef] [Green Version]
- Yonezawa, H.; Osaki, T.; Hojo, F.; Kamiya, S. Effect of Helicobacter pylori Biofilm Formation on Susceptibility to Amoxicillin, Metronidazole and Clarithromycin. Microb. Pathog. 2019, 132, 100–108. [Google Scholar] [CrossRef]
- Gisbert, J.P. Empirical or Susceptibility-Guided Treatment for Helicobacter pylori Infection? A Comprehensive Review. Ther. Adv. Gastroenterol. 2020, 13, 1756284820968736. [Google Scholar] [CrossRef] [PubMed]
- Erah, P.O.; Goddard, A.F.; Barrett, D.A.; Shaw, P.N.; Spiller, R.C. The Stability of Amoxycillin, Clarithromycin and Metronidazole in Gastric Juice: Relevance to the Treatment of Helicobacter pylori Infection. J. Antimicrob. Chemother. 1997, 39, 5–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, J.; Patel, M. Stomach Specific Anti-Helicobacter pylori Therapy: Preparation and Evaluation of Amoxicillin-Loaded Chitosan Mucoadhesive Microspheres. Curr. Drug Deliv. 2007, 4, 41–50. [Google Scholar] [CrossRef]
- Ciandrini, E.; Campana, R.; Federici, S.; Manti, A.; Battistelli, M.; Falcieri, E.; Papa, S.; Baffone, W. In Vitro Activity of Carvacrol against Titanium-Adherent Oral Biofilms and Planktonic Cultures. Clin. Oral Investig. 2014, 18, 2001–2013. [Google Scholar] [CrossRef]
- Ma, M.; Zhao, J.; Yan, X.; Zeng, Z.; Wan, D.; Yu, P.; Xia, J.; Zhang, G.; Gong, D. Synergistic Effects of Monocaprin and Carvacrol against Escherichia coli O157:H7 and Salmonella Typhimurium in Chicken Meat Preservation. Food Control 2022, 132, 108480. [Google Scholar] [CrossRef]
- Ultee, A.; Bennik, M.H.J.; Moezelaar, R. The Phenolic Hydroxyl Group of Carvacrol Is Essential for Action against the Food-Borne Pathogen Bacillus cereus. Appl. Environ. Microbiol. 2002, 68, 1561–1568. [Google Scholar] [CrossRef] [Green Version]
- Horii, T.; Mase, K.; Suzuki, Y.; Kimura, T.; Ohta, M.; Maekawa, M.; Kanno, T.; Kobayashi, M. Antibacterial Activities of Beta-Lactamase Inhibitors Associated with Morphological Changes of Cell Wall in Helicobacter pylori. Helicobacter 2002, 7, 39–45. [Google Scholar] [CrossRef]
- Makobongo, M.O.; Einck, L.; Peek, R.M.; Merrell, D.S. In Vitro Characterization of the Anti-Bacterial Activity of SQ109 against Helicobacter pylori. PLoS ONE 2013, 8, e68917. [Google Scholar] [CrossRef]
- Sharaf, M.; Arif, M.; Hamouda, H.I.; Khan, S.; Abdalla, M.; Shabana, S.; Rozan, H.E.; Khan, T.U.; Chi, Z.; Liu, C. Preparation, Urease Inhibition Mechanisms, and Anti-Helicobacter pylori Activities of Hesperetin-7-Rhamnoglucoside. Curr. Res. Microb. Sci. 2022, 3, 100103. [Google Scholar] [CrossRef]
- Grande, R.; Sisto, F.; Puca, V.; Carradori, S.; Ronci, M.; Aceto, A.; Muraro, R.; Mincione, G.; Scotti, L. Antimicrobial and Antibiofilm Activities of New Synthesized Silver Ultra-NanoClusters (SUNCs) against Helicobacter pylori. Front. Microbiol. 2020, 11, 1705. [Google Scholar] [CrossRef]
- Ben Khalifa, R.; Cacciatore, I.; Dimmito, M.P.; Ciulla, M.; Grande, R.; Puca, V.; Robuffo, I.; De Laurenzi, V.; Chekir-Ghedira, L.; Di Stefano, A.; et al. Multiple Lipid Nanoparticles as Antimicrobial Drug Delivery Systems. J. Drug Deliv. Sci. Technol. 2022, 67, 102887. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standard Institute [CLSI]. Performance Standards for Antimicrobial Susceptibility Testing. Seventeenth Informational Supplement M100–S17; Clinical and Laboratory Standard Institute: Wayne, PA, USA, 2007; Volume 27. [Google Scholar]
- Puca, V.; Traini, T.; Guarnieri, S.; Carradori, S.; Sisto, F.; Macchione, N.; Muraro, R.; Mincione, G.; Grande, R. The Antibiofilm Effect of a Medical Device Containing TIAB on Microorganisms Associated with Surgical Site Infection. Molecules 2019, 24, 2280. [Google Scholar] [CrossRef] [Green Version]





| H. pylori ATCC 43504 | CAR [µg/mL] | AMX [µg/mL] | SHA [µg/mL] | FICI a | FBCI b | |||
|---|---|---|---|---|---|---|---|---|
| MIC | MBC | MIC | MBC | MIC | MBC | |||
| DRUG ALONE | 128 | 256 | 0.032 | 0.064 | 64 | 128 | - | - |
| COMBINATIONS | ||||||||
| CAR-AMX | 64 | 64 | 0.008 | 0.064 | - | - | 0.75 | 1.25 |
| CAR-SHA | 32 | 64 | - | - | 32 | 64 | 0.75 | 0.75 |
| SHA-AMX | - | - | 0.008 | 0.064 | 64 | 128 | 1.25 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puca, V.; Turacchio, G.; Marinacci, B.; Supuran, C.T.; Capasso, C.; Di Giovanni, P.; D’Agostino, I.; Carradori, S.; Grande, R. Antimicrobial and Antibiofilm Activities of Carvacrol, Amoxicillin and Salicylhydroxamic Acid Alone and in Combination vs. Helicobacter pylori: Towards a New Multi-Targeted Therapy. Int. J. Mol. Sci. 2023, 24, 4455. https://doi.org/10.3390/ijms24054455
Puca V, Turacchio G, Marinacci B, Supuran CT, Capasso C, Di Giovanni P, D’Agostino I, Carradori S, Grande R. Antimicrobial and Antibiofilm Activities of Carvacrol, Amoxicillin and Salicylhydroxamic Acid Alone and in Combination vs. Helicobacter pylori: Towards a New Multi-Targeted Therapy. International Journal of Molecular Sciences. 2023; 24(5):4455. https://doi.org/10.3390/ijms24054455
Chicago/Turabian StylePuca, Valentina, Gabriele Turacchio, Beatrice Marinacci, Claudiu T. Supuran, Clemente Capasso, Pamela Di Giovanni, Ilaria D’Agostino, Simone Carradori, and Rossella Grande. 2023. "Antimicrobial and Antibiofilm Activities of Carvacrol, Amoxicillin and Salicylhydroxamic Acid Alone and in Combination vs. Helicobacter pylori: Towards a New Multi-Targeted Therapy" International Journal of Molecular Sciences 24, no. 5: 4455. https://doi.org/10.3390/ijms24054455