Potential Fluid Biomarkers for the Diagnosis of Mild Cognitive Impairment
Abstract
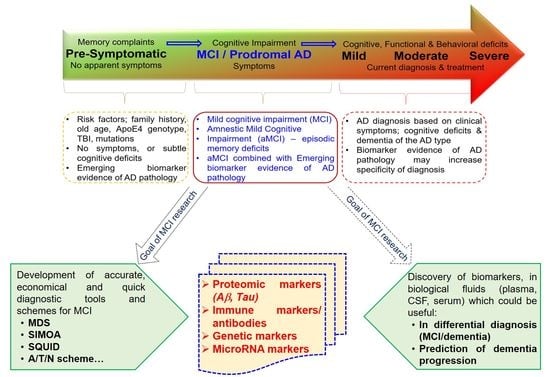
:1. Introduction
2. Diagnostic Tools of MCI and Preclinical Dementia
3. Multiple Approaches to Blood-Based Markers
4. Diagnostic Approaches and Tools of MCI
5. Mild Cognitive Impairment in Relation to CSF Biomarkers
6. Other Potential Biological Fluids
7. Micro RNA (miRNA) in the Diagnosis of MCI and the Prediction of AD
8. Genetic factors, Which Could Increase the Risk for MCI-AD Conversion
9. Challenges in MCI Diagnosis
10. Discussion and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Petersen, R.C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 2004, 256, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C. Mild Cognitive Impairment. Contin. (Minneap Minn) 2016, 22, 404–418. [Google Scholar] [CrossRef] [PubMed]
- Shah, Y.; Tangalos, E.G.; Petersen, R.C. Mild cognitive impairment. When is it a precursor to Alzheimer’s disease? Geriatrics 2000, 55, 62, 65–68. [Google Scholar] [PubMed]
- Busse, A.; Bischkopf, J.; Riedel-Heller, S.G.; Angermeyer, M.C. Mild cognitive impairment: Prevalence and predictive validity according to current approaches. Acta Neurol. Scand. 2003, 108, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Smith, G.E.; Waring, S.C.; Ivnik, R.J.; Tangalos, E.G.; Kokmen, E. Mild cognitive impairment: Clinical characterization and outcome. Arch. Neurol. 1999, 56, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Dugger, B.N.; Davis, K.; Malek-Ahmadi, M.; Hentz, J.G.; Sandhu, S.; Beach, T.G.; Adler, C.H.; Caselli, R.J.; Johnson, T.A.; Serrano, G.E.; et al. Neuropathological comparisons of amnestic and nonamnestic mild cognitive impairment. BMC Neurol. 2015, 15, 146. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.; Knopman, D.S. Classification and epidemiology of MCI. Clin. Geriatr. Med. 2013, 29, 753–772. [Google Scholar] [CrossRef] [PubMed]
- Geda, Y.E. Mild cognitive impairment in older adults. Curr. Psychiatry Rep. 2012, 14, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Subramanyam, A.; Singh, S. Mild cognitive decline: Concept, types, presentation, and management. J. Geriatr. Ment. Health 2016, 3, 10–20. [Google Scholar] [CrossRef]
- Chertkow, H.; Massoud, F.; Nasreddine, Z.; Belleville, S.; Joanette, Y.; Bocti, C.; Drolet, V.; Kirk, J.; Freedman, M.; Bergman, H. Diagnosis and treatment of dementia: 3. Mild cognitive impairment and cognitive impairment without dementia. Can. Med. Assoc. 2008, 178, 1273–1285. [Google Scholar] [CrossRef] [Green Version]
- Gomersall, T.; Smith, S.K.; Blewett, C.; Astell, A. It’s definitely not Alzheimer’s’: Perceived benefits and drawbacks of a mild cognitive impairment diagnosis. Br. J. Health Psychol. 2017, 22, 786–804. [Google Scholar] [CrossRef] [PubMed]
- Knopman, D.S.; Petersen, R.C. Mild cognitive impairment and mild dementia: A clinical perspective. Mayo Clin. Proc. 2014, 89, 1452–1459. [Google Scholar] [CrossRef] [PubMed]
- Sliwinski, M.; Lipton, R.B.; Buschke, H.; Stewart, W. The effects of preclinical dementia on estimates of normal cognitive functioning in aging. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 1996, 51, P217–P225. [Google Scholar] [CrossRef] [PubMed]
- Sperling, R.A.; Aisen, P.S.; Beckett, L.A.; Bennett, D.A.; Craft, S.; Fagan, A.M.; Iwatsubo, T.; Jack, C.R., Jr.; Kaye, J.; Montine, T.J.; et al. Toward defining the preclinical stages of Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2011, 7, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Chong, M.S.; Sahadevan, S. Preclinical Alzheimer’s disease: Diagnosis and prediction of progression. Lancet Neurol. 2005, 4, 576–579. [Google Scholar] [CrossRef]
- Nestor, P.J.; Scheltens, P.; Hodges, J.R. Advances in the early detection of Alzheimer’s disease. Nat. Med. 2004, 10, S34–S41. [Google Scholar] [CrossRef] [PubMed]
- Mak, E.; Gabel, S.; Mirette, H.; Su, L.; Williams, G.B.; Waldman, A.; Wells, K.; Ritchie, K.; Ritchie, C.; O’Brien, J. Structural neuroimaging in preclinical dementia: From microstructural deficits and grey matter atrophy to macroscale connectomic changes. Ageing Res. Rev. 2017, 35, 250–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albert, M.; Zhu, Y.; Moghekar, A.; Mori, S.; Miller, M.I.; Soldan, A.; Pettigrew, C.; Selnes, O.; Li, S.; Wang, M.C. Predicting progression from normal cognition to mild cognitive impairment for individuals at 5 years. Brain A J. Neurol. 2018, 141, 877–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, C.; Li, S.; Zhao, W.; Feng, J. Brain imaging of mild cognitive impairment and Alzheimer’s disease. Neural Regen Res. 2013, 8, 435–444. [Google Scholar]
- Rabinovici, G.D.; Gatsonis, C.; Apgar, C.; Chaudhary, K.; Gareen, I.; Hanna, L.; Hendrix, J.; Hillner, B.E.; Olson, C.; Lesman-Segev, O.H.; et al. Association of Amyloid Positron Emission Tomography With Subsequent Change in Clinical Management Among Medicare Beneficiaries With Mild Cognitive Impairment or Dementia. Jama 2019, 321, 1286–1294. [Google Scholar] [CrossRef]
- Luck, T.; Riedel-Heller, S.G.; Kaduszkiewicz, H.; Bickel, H.; Jessen, F.; Pentzek, M.; Wiese, B.; Koelsch, H.; van den Bussche, H.; Abholz, H.H.; et al. Mild cognitive impairment in general practice: Age-specific prevalence and correlate results from the German study on ageing, cognition and dementia in primary care patients (AgeCoDe). Dement. Geriatr. Cogn. Disord. 2007, 24, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.C.; Storandt, M.; Miller, J.P.; McKeel, D.W.; Price, J.L.; Rubin, E.H.; Berg, L. Mild cognitive impairment represents early-stage Alzheimer disease. Arch. Neurol. 2001, 58, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Manly, J.J.; Tang, M.X.; Schupf, N.; Stern, Y.; Vonsattel, J.P.; Mayeux, R. Frequency and course of mild cognitive impairment in a multiethnic community. Ann. Neurol. 2008, 63, 494–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tervo, S.; Kivipelto, M.; Hanninen, T.; Vanhanen, M.; Hallikainen, M.; Mannermaa, A.; Soininen, H. Incidence and risk factors for mild cognitive impairment: A population-based three-year follow-up study of cognitively healthy elderly subjects. Dement. Geriatr. Cogn. Disord. 2004, 17, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Hall, N.C.; Perry, R.P.; Ruthig, J.C.; Hladkyj, S.; Chipperfield, J.G. Primary and Secondary Control in Achievement Settings: A Longitudinal Field Study of Academic Motivation, Emotions, and Performance1. J. Appl. Soc. Psychol. 2006, 36, 1430–1470. [Google Scholar] [CrossRef]
- Etgen, T.; Chonchol, M.; Forstl, H.; Sander, D. Chronic kidney disease and cognitive impairment: A systematic review and meta-analysis. Am. J. Nephrol. 2012, 35, 474–482. [Google Scholar] [CrossRef] [PubMed]
- Ekman, U.; Ferreira, D.; Westman, E. The A/T/N biomarker scheme and patterns of brain atrophy assessed in mild cognitive impairment. Sci. Rep. 2018, 8, 8431. [Google Scholar] [CrossRef] [PubMed]
- Jack, C.R., Jr.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Feldman, H.H.; Frisoni, G.B.; Hampel, H.; Jagust, W.J.; Johnson, K.A.; Knopman, D.S.; et al. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 2016, 87, 539–547. [Google Scholar] [CrossRef]
- Lim, K.; Kim, S.Y.; Lee, B.; Segarra, C.; Kang, S.; Ju, Y.; Schmerr, M.J.; Coste, J.; Kim, S.Y.; Yokoyama, T.; et al. Magnetic microparticle-based multimer detection system for the detection of prion oligomers in sheep. Int. J. Nanomed. 2015, 10, 241–250. [Google Scholar] [Green Version]
- Van Giau, V.; An, S.S.A. Epitope Mapping Immunoassay Analysis of the Interaction between beta-Amyloid and Fibrinogen. Int. J. Mol. Sci. 2019, 20, 496. [Google Scholar] [CrossRef]
- Yang, Y.; Giau, V.V.; An, S.S.A.; Kim, S. Plasma Oligomeric Beta Amyloid in Alzheimer’s Disease with History of Agent Orange Exposure. Dement. Neurocogn. Disord. 2018, 17, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.J.; Yi, S.; Han, J.Y.; Park, S.Y.; Jang, J.W.; Chun, I.K.; Kim, S.E.; Lee, B.S.; Kim, G.J.; Yu, J.S.; et al. Oligomeric forms of amyloid-β protein in plasma as a potential blood-based biomarker for Alzheimer’s disease. Alzheimer’s Res. Ther. 2017, 9, 98. [Google Scholar] [CrossRef] [PubMed]
- An, S.S.A.; Lee, B.S.; Yu, J.S.; Lim, K.; Kim, G.J.; Lee, R.; Kim, S.; Kang, S.; Park, Y.H.; Wang, M.J.; et al. Detection of oligomerized amyloid beta in plasma of mild cognitive impairment patient. J. Neurol. Sci. 2017, 381, 1033. [Google Scholar] [CrossRef]
- Kim, J.A.; Kim, M.; Kang, S.M.; Lim, K.T.; Kim, T.S.; Kang, J.Y. Magnetic bead droplet immunoassay of oligomer amyloid beta for the diagnosis of Alzheimer’s disease using micro-pillars to enhance the stability of the oil-water interface. Biosens. Bioelectron. 2015, 67, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Lewczuk, P.; Ermann, N.; Andreasson, U.; Schultheis, C.; Podhorna, J.; Spitzer, P.; Maler, J.M.; Kornhuber, J.; Blennow, K.; Zetterberg, H. Plasma neurofilament light as a potential biomarker of neurodegeneration in Alzheimer’s disease. Alzheimers Res. 2018, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Dage, J.L.; Wennberg, A.M.V.; Airey, D.C.; Hagen, C.E.; Knopman, D.S.; Machulda, M.M.; Roberts, R.O.; Jack, C.R., Jr.; Petersen, R.C.; Mielke, M.M. Levels of tau protein in plasma are associated with neurodegeneration and cognitive function in a population-based elderly cohort. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2016, 12, 1226–1234. [Google Scholar] [CrossRef]
- Janelidze, S.; Stomrud, E.; Palmqvist, S.; Zetterberg, H.; van Westen, D.; Jeromin, A.; Song, L.; Hanlon, D.; Tan Hehir, C.A.; Baker, D.; et al. Plasma beta-amyloid in Alzheimer’s disease and vascular disease. Sci. Rep. 2016, 6, 26801. [Google Scholar] [CrossRef]
- Chieh, J.J.; Yang, S.Y.; Jian, Z.F.; Wang, W.C.; Horng, H.E.; Yang, H.C.; Hong, C.Y. Hyper-high-sensitivity wash-free magnetoreduction assay on biomolecules using high-Tc superconducting quantum interference devices. J. Appl. Phys. 2008, 103, 014703. [Google Scholar] [CrossRef]
- Chiu, M.J.; Yang, S.Y.; Horng, H.E.; Yang, C.C.; Chen, T.F.; Chieh, J.J.; Chen, H.H.; Chen, T.C.; Ho, C.S.; Chang, S.F.; et al. Combined plasma biomarkers for diagnosing mild cognition impairment and Alzheimer’s disease. ACS Chem. Neurosci. 2013, 4, 1530–1536. [Google Scholar] [CrossRef]
- Tan, C.C.; Yu, J.T.; Tan, L. Biomarkers for preclinical Alzheimer’s disease. J. Alzheimer’s Dis. 2014, 42, 1051–1069. [Google Scholar] [CrossRef]
- Herukka, S.K.; Hallikainen, M.; Soininen, H.; Pirttila, T. CSF Abeta42 and tau or phosphorylated tau and prediction of progressive mild cognitive impairment. Neurology 2005, 64, 1294–1297. [Google Scholar] [CrossRef] [PubMed]
- Blennow, K.; Hampel, H. CSF markers for incipient Alzheimer’s disease. Lancet Neurol. 2003, 2, 605–613. [Google Scholar] [CrossRef]
- Parnetti, L.; Chiasserini, D.; Eusebi, P.; Giannandrea, D.; Bellomo, G.; De Carlo, C.; Padiglioni, C.; Mastrocola, S.; Lisetti, V.; Calabresi, P. Performance of abeta1-40, abeta1-42, total tau, and phosphorylated tau as predictors of dementia in a cohort of patients with mild cognitive impairment. J. Alzheimer’s Dis. 2012, 29, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Okonkwo, O.C.; Alosco, M.L.; Griffith, H.R.; Mielke, M.M.; Shaw, L.M.; Trojanowski, J.Q.; Tremont, G. Cerebrospinal fluid abnormalities and rate of decline in everyday function across the dementia spectrum: Normal aging, mild cognitive impairment, and Alzheimer disease. Arch. Neurol. 2010, 67, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Hansson, O.; Seibyl, J.; Stomrud, E.; Zetterberg, H.; Trojanowski, J.Q.; Bittner, T.; Lifke, V.; Corradini, V.; Eichenlaub, U.; Batrla, R.; et al. CSF biomarkers of Alzheimer’s disease concord with amyloid-beta PET and predict clinical progression: A study of fully automated immunoassays in BioFINDER and ADNI cohorts. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2018, 14, 1470–1481. [Google Scholar] [CrossRef] [PubMed]
- Forlenza, O.V.; Radanovic, M.; Talib, L.L.; Aprahamian, I.; Diniz, B.S.; Zetterberg, H.; Gattaz, W.F. Cerebrospinal fluid biomarkers in Alzheimer’s disease: Diagnostic accuracy and prediction of dementia. Alzheimer’s Dement. (Amst. Neth.) 2015, 1, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Hansson, O.; Zetterberg, H.; Buchhave, P.; Londos, E.; Blennow, K.; Minthon, L. Association between CSF biomarkers and incipient Alzheimer’s disease in patients with mild cognitive impairment: A follow-up study. Lancet Neurol. 2006, 5, 228–234. [Google Scholar] [CrossRef]
- Forsberg, A.; Engler, H.; Almkvist, O.; Blomquist, G.; Hagman, G.; Wall, A.; Ringheim, A.; Langstrom, B.; Nordberg, A. PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiol. Aging 2008, 29, 1456–1465. [Google Scholar] [CrossRef]
- Bocchetta, M.; Galluzzi, S.; Kehoe, P.G.; Aguera, E.; Bernabei, R.; Bullock, R.; Ceccaldi, M.; Dartigues, J.F.; de Mendonca, A.; Didic, M.; et al. The use of biomarkers for the etiologic diagnosis of MCI in Europe: An EADC survey. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2015, 11, 195–206. e1. [Google Scholar] [CrossRef]
- Yue, J.; Dong, B.R.; Lin, X.; Yang, M.; Wu, H.M.; Wu, T. Huperzine A for mild cognitive impairment. Cochrane Database Syst. Rev. 2012, 12, CD008827. [Google Scholar] [CrossRef]
- Winblad, B.; Palmer, K.; Kivipelto, M.; Jelic, V.; Fratiglioni, L.; Wahlund, L.O.; Nordberg, A.; Backman, L.; Albert, M.; Almkvist, O.; et al. Mild cognitive impairment-beyond controversies, towards a consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Intern. Med. 2004, 256, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Gangishetti, U.; Christina Howell, J.; Perrin, R.J.; Louneva, N.; Watts, K.D.; Kollhoff, A.; Grossman, M.; Wolk, D.A.; Shaw, L.M.; Morris, J.C.; et al. Non-beta-amyloid/tau cerebrospinal fluid markers inform staging and progression in Alzheimer’s disease. Alzheimer’s Res. Ther. 2018, 10, 98. [Google Scholar] [CrossRef]
- Paterson, R.W.; Bartlett, J.W.; Blennow, K.; Fox, N.C.; Shaw, L.M.; Trojanowski, J.Q.; Zetterberg, H.; Schott, J.M. Cerebrospinal fluid markers including trefoil factor 3 are associated with neurodegeneration in amyloid-positive individuals. Transl. Psychiatry 2014, 4, e419. [Google Scholar] [CrossRef]
- Tang, B.L.; Kumar, R. Biomarkers of mild cognitive impairment and Alzheimer’s disease. Ann. Acad. Med. Singap. 2008, 37, 406–410. [Google Scholar] [PubMed]
- Forlenza, O.V.; Diniz, B.S.; Teixeira, A.L.; Stella, F.; Gattaz, W. Mild cognitive impairment. Part 2: Biological markers for diagnosis and prediction of dementia in Alzheimer’s disease. Revista brasileira de psiquiatria (Sao Paulo, Brazil: 1999) 2013, 35, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Van Giau, V.; An, S.S.A. Optimization of specific multiplex DNA primers to detect variable CLU genomic lesions in patients with Alzheimer’s disease. Biochip J. 2015, 9, 278–284. [Google Scholar] [CrossRef]
- Jongbloed, W.; van Dijk, K.D.; Mulder, S.D.; van de Berg, W.D.; Blankenstein, M.A.; van der Flier, W.; Veerhuis, R. Clusterin Levels in Plasma Predict Cognitive Decline and Progression to Alzheimer’s Disease. J. Alzheimer’s Dis. 2015, 46, 1103–1110. [Google Scholar] [CrossRef]
- Vishnu, V.Y.; Modi, M.; Sharma, S.; Mohanty, M.; Goyal, M.K.; Lal, V.; Khandelwal, N.; Mittal, B.R.; Prabhakar, S. Role of Plasma Clusterin in Alzheimer’s Disease—A Pilot Study in a Tertiary Hospital in Northern India. PLoS ONE 2016, 11, e0166369. [Google Scholar] [CrossRef]
- Reitz, C.; Mayeux, R. Use of genetic variation as biomarkers for mild cognitive impairment and progression of mild cognitive impairment to dementia. J. Alzheimer’s Dis. 2010, 19, 229–251. [Google Scholar] [CrossRef]
- Yin, Z.X.; Shi, X.M.; Kraus, V.B.; Fitzgerald, S.M.; Qian, H.Z.; Xu, J.W.; Zhai, Y.; Sereny, M.D.; Zeng, Y. High normal plasma triglycerides are associated with preserved cognitive function in Chinese oldest-old. Age Ageing 2012, 41, 600–606. [Google Scholar] [CrossRef] [Green Version]
- He, Q.; Li, Q.; Zhao, J.; Wu, T.; Ji, L.; Huang, G.; Ma, F. Relationship between plasma lipids and mild cognitive impairment in the elderly Chinese: A case-control study. Lipids Health Dis. 2016, 15, 146. [Google Scholar] [CrossRef] [PubMed]
- Stanga, S.; Lanni, C.; Sinforiani, E.; Mazzini, G.; Racchi, M. Searching for predictive blood biomarkers: Misfolded p53 in mild cognitive impairment. Curr. Alzheimer Res. 2012, 9, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Bagyinszky, E.; Giau, V.V.; Shim, K.; Suk, K.; An, S.S.A.; Kim, S. Role of inflammatory molecules in the Alzheimer’s disease progression and diagnosis. J. Neurol. Sci. 2017, 376, 242–254. [Google Scholar] [CrossRef] [PubMed]
- Alley, D.E.; Crimmins, E.M.; Karlamangla, A.; Hu, P.; Seeman, T.E. Inflammation and rate of cognitive change in high-functioning older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2008, 63, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Saleem, M.; Herrmann, N.; Swardfager, W.; Eisen, R.; Lanctot, K.L. Inflammatory Markers in Mild Cognitive Impairment: A Meta-Analysis. J. Alzheimer’s Dis. 2015, 47, 669–679. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.; Huang, X.; Li, F.; Ren, M.; Zhang, J.; Xu, M.; Wu, M. Association among plasma lactate, systemic inflammation, and mild cognitive impairment: A community-based study. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2019, 40, 1667–1673. [Google Scholar] [CrossRef]
- Shen, X.N.; Lu, Y.; Tan, C.T.Y.; Liu, L.Y.; Yu, J.T.; Feng, L.; Larbi, A. Identification of inflammatory and vascular markers associated with mild cognitive impairment. Aging 2019, 11, 2403–2419. [Google Scholar] [CrossRef]
- King, E.; O’Brien, J.T.; Donaghy, P.; Morris, C.; Barnett, N.; Olsen, K.; Martin-Ruiz, C.; Taylor, J.P.; Thomas, A.J. Peripheral inflammation in mild cognitive impairment with possible and probable Lewy body disease and Alzheimer’s disease. Int. Psychogeriatr. 2019, 31, 551–560. [Google Scholar] [CrossRef]
- Wennberg, A.M.V.; Hagen, C.E.; Machulda, M.M.; Knopman, D.S.; Petersen, R.C.; Mielke, M.M. The Cross-Sectional and Longitudinal Associations Between IL-6, IL-10, and TNFalpha and Cognitive Outcomes in the Mayo Clinic Study of Aging. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018. [Google Scholar] [CrossRef]
- Mader, S.; Brimberg, L.; Diamond, B. The Role of Brain-Reactive Autoantibodies in Brain Pathology and Cognitive Impairment. Front. Immunol. 2017, 8, 1101. [Google Scholar] [CrossRef]
- Busse, M.; Kunschmann, R.; Dobrowolny, H.; Hoffmann, J.; Bogerts, B.; Steiner, J.; Frodl, T.; Busse, S. Dysfunction of the blood-cerebrospinal fluid-barrier and N-methyl-D-aspartate glutamate receptor antibodies in dementias. Eur. Arch. Psychiatry Clin. Neurosci. 2018, 268, 483–492. [Google Scholar] [CrossRef] [PubMed]
- DeMarshall, C.A.; Nagele, E.P.; Sarkar, A.; Acharya, N.K.; Godsey, G.; Goldwaser, E.L.; Kosciuk, M.; Thayasivam, U.; Han, M.; Belinka, B.; et al. Detection of Alzheimer’s disease at mild cognitive impairment and disease progression using autoantibodies as blood-based biomarkers. Alzheimer’s Dement. (Amst. Neth.) 2016, 3, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, L. Autoantibodies in Alzheimer’s disease: Potential biomarkers, pathogenic roles, and therapeutic implications. J. Biomed. Res. 2016, 30, 361–372. [Google Scholar] [PubMed]
- Du, Y.; Dodel, R.; Hampel, H.; Buerger, K.; Lin, S.; Eastwood, B.; Bales, K.; Gao, F.; Moeller, H.J.; Oertel, W.; et al. Reduced levels of amyloid beta-peptide antibody in Alzheimer disease. Neurology 2001, 57, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Weksler, M.E.; Relkin, N.; Turkenich, R.; LaRusse, S.; Zhou, L.; Szabo, P. Patients with Alzheimer disease have lower levels of serum anti-amyloid peptide antibodies than healthy elderly individuals. Exp. Gerontol. 2002, 37, 943–948. [Google Scholar] [CrossRef]
- Song, M.S.; Mook-Jung, I.; Lee, H.J.; Min, J.Y.; Park, M.H. Serum anti-amyloid-beta antibodies and Alzheimer’s disease in elderly Korean patients. J. Int. Med. Res. 2007, 35, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Qu, B.X.; Gong, Y.; Moore, C.; Fu, M.; German, D.C.; Chang, L.Y.; Rosenberg, R.; Diaz-Arrastia, R. Beta-amyloid auto-antibodies are reduced in Alzheimer’s disease. J. Neuroimmunol. 2014, 274, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Storace, D.; Cammarata, S.; Borghi, R.; Sanguineti, R.; Giliberto, L.; Piccini, A.; Pollero, V.; Novello, C.; Caltagirone, C.; Smith, M.A.; et al. Elevation of {beta}-amyloid 1-42 autoantibodies in the blood of amnestic patients with mild cognitive impairment. Arch. Neurol. 2010, 67, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Bartos, A.; Fialova, L.; Svarcova, J.; Ripova, D. Patients with Alzheimer disease have elevated intrathecal synthesis of antibodies against tau protein and heavy neurofilament. J. Neuroimmunol. 2012, 252, 100–105. [Google Scholar] [CrossRef]
- Rosenmann, H.; Meiner, Z.; Geylis, V.; Abramsky, O.; Steinitz, M. Detection of circulating antibodies against tau protein in its unphosphorylated and in its neurofibrillary tangles-related phosphorylated state in Alzheimer’s disease and healthy subjects. Neurosci. Lett. 2006, 410, 90–93. [Google Scholar] [CrossRef]
- Masliah, E.; Mallory, M.; Hansen, L.; Richard, D.; Alford, M.; Terry, R. Synaptic and neuritic alterations during the progression of Alzheimer’s disease. Neurosci. Lett. 1994, 174, 67–72. [Google Scholar] [CrossRef]
- Thorsell, A.; Bjerke, M.; Gobom, J.; Brunhage, E.; Vanmechelen, E.; Andreasen, N.; Hansson, O.; Minthon, L.; Zetterberg, H.; Blennow, K. Neurogranin in cerebrospinal fluid as a marker of synaptic degeneration in Alzheimer’s disease. Brain Res. 2010, 1362, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Schindler, S.E.; Li, Y.; Todd, K.W.; Herries, E.M.; Henson, R.L.; Gray, J.D.; Wang, G.; Graham, D.L.; Shaw, L.M.; Trojanowski, J.Q.; et al. Emerging cerebrospinal fluid biomarkers in autosomal dominant Alzheimer’s disease. Alzheimer’s Dement. 2019, 15, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Kvartsberg, H.; Duits, F.H.; Ingelsson, M.; Andreasen, N.; Ohrfelt, A.; Andersson, K.; Brinkmalm, G.; Lannfelt, L.; Minthon, L.; Hansson, O.; et al. Cerebrospinal fluid levels of the synaptic protein neurogranin correlates with cognitive decline in prodromal Alzheimer’s disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2015, 11, 1180–1190. [Google Scholar] [CrossRef] [PubMed]
- Portelius, E.; Zetterberg, H.; Skillback, T.; Tornqvist, U.; Andreasson, U.; Trojanowski, J.Q.; Weiner, M.W.; Shaw, L.M.; Mattsson, N.; Blennow, K. Cerebrospinal fluid neurogranin: Relation to cognition and neurodegeneration in Alzheimer’s disease. Brain A J. Neurol. 2015, 138, 3373–3385. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, N.; Insel, P.S.; Palmqvist, S.; Portelius, E.; Zetterberg, H.; Weiner, M.; Blennow, K.; Hansson, O.; Alzheimer’s Disease Neuroimaging Initiative. Cerebrospinal fluid tau, neurogranin, and neurofilament light in Alzheimer’s disease. Embo Mol. Med. 2016, 8, 1184–1196. [Google Scholar] [CrossRef]
- Craig-Schapiro, R.; Perrin, R.J.; Roe, C.M.; Xiong, C.; Carter, D.; Cairns, N.J.; Mintun, M.A.; Peskind, E.R.; Li, G.; Galasko, D.R.; et al. YKL-40: A novel prognostic fluid biomarker for preclinical Alzheimer’s disease. Biol. Psychiatry 2010, 68, 903–912. [Google Scholar] [CrossRef] [PubMed]
- Rosen, C.; Andersson, C.H.; Andreasson, U.; Molinuevo, J.L.; Bjerke, M.; Rami, L.; Llado, A.; Blennow, K.; Zetterberg, H. Increased Levels of Chitotriosidase and YKL-40 in Cerebrospinal Fluid from Patients with Alzheimer’s Disease. Dement. Geriatr. Cogn. Disord. Extra 2014, 4, 297–304. [Google Scholar] [CrossRef]
- Brinkmalm, A.; Brinkmalm, G.; Honer, W.G.; Frolich, L.; Hausner, L.; Minthon, L.; Hansson, O.; Wallin, A.; Zetterberg, H.; Blennow, K.; et al. SNAP-25 is a promising novel cerebrospinal fluid biomarker for synapse degeneration in Alzheimer’s disease. Mol. Neurodegener. 2014, 9, 53. [Google Scholar] [CrossRef]
- Babic Leko, M.; Borovecki, F.; Dejanovic, N.; Hof, P.R.; Simic, G. Predictive Value of Cerebrospinal Fluid Visinin-Like Protein-1 Levels for Alzheimer’s Disease Early Detection and Differential Diagnosis in Patients with Mild Cognitive Impairment. J. Alzheimer’s Dis. 2016, 50, 765–778. [Google Scholar] [CrossRef]
- Lee, J.M.; Blennow, K.; Andreasen, N.; Laterza, O.; Modur, V.; Olander, J.; Gao, F.; Ohlendorf, M.; Ladenson, J.H. The brain injury biomarker VLP-1 is increased in the cerebrospinal fluid of Alzheimer disease patients. Clin. Chem. 2008, 54, 1617–1623. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.B.; Szijan, I.; Coulter, P.M. Localization of RC3 (neurogranin) in rat brain subcellular fractions. Mol. Brain Res. 1994, 27, 323–328. [Google Scholar] [CrossRef]
- Kang, H.J.; Voleti, B.; Hajszan, T.; Rajkowska, G.; Stockmeier, C.A.; Licznerski, P.; Lepack, A.; Majik, M.S.; Jeong, L.S.; Banasr, M.; et al. Decreased expression of synapse-related genes and loss of synapses in major depressive disorder. Nat. Med. 2012, 18, 1413–1417. [Google Scholar] [CrossRef] [PubMed]
- Sanfilippo, C.; Forlenza, O.; Zetterberg, H.; Blennow, K. Increased neurogranin concentrations in cerebrospinal fluid of Alzheimer’s disease and in mild cognitive impairment due to AD. J. Neural Transm. (Vienna, Austria: 1996) 2016, 123, 1443–1447. [Google Scholar] [CrossRef] [PubMed]
- Hellwig, K.; Kvartsberg, H.; Portelius, E.; Andreasson, U.; Oberstein, T.J.; Lewczuk, P.; Blennow, K.; Kornhuber, J.; Maler, J.M.; Zetterberg, H.; et al. Neurogranin and YKL-40: Independent markers of synaptic degeneration and neuroinflammation in Alzheimer’s disease. Alzheimer’s Res. Ther. 2015, 7, 74. [Google Scholar] [CrossRef] [PubMed]
- Hampel, H.; Toschi, N.; Baldacci, F.; Zetterberg, H.; Blennow, K.; Kilimann, I.; Teipel, S.J.; Cavedo, E.; Melo Dos Santos, A.; Epelbaum, S.; et al. Alzheimer’s disease biomarker-guided diagnostic workflow using the added value of six combined cerebrospinal fluid candidates: Abeta1-42, total-tau, phosphorylated-tau, NFL, neurogranin, and YKL-40. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2018, 14, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Olsson, B.; Hertze, J.; Lautner, R.; Zetterberg, H.; Nagga, K.; Hoglund, K.; Basun, H.; Annas, P.; Lannfelt, L.; Andreasen, N.; et al. Microglial markers are elevated in the prodromal phase of Alzheimer’s disease and vascular dementia. J. Alzheimer’s Dis. 2013, 33, 45–53. [Google Scholar] [CrossRef]
- Muszyński, P.; Groblewska, M.; Kulczyńska-Przybik, A.; Kułakowska, A.; Mroczko, B. YKL-40 as a Potential Biomarker and a Possible Target in Therapeutic Strategies of Alzheimer’s Disease. Curr. Neuropharmacol. 2017, 15, 906–917. [Google Scholar] [CrossRef]
- Danka Mohammed, C.P.; Park, J.S.; Nam, H.G.; Kim, K. MicroRNAs in brain aging. Mech. Ageing Dev. 2017, 168, 3–9. [Google Scholar] [CrossRef]
- Sheinerman, K.S.; Tsivinsky, V.G.; Abdullah, L.; Crawford, F.; Umansky, S.R. Plasma microRNA biomarkers for detection of mild cognitive impairment: Biomarker validation study. Aging 2013, 5, 925–938. [Google Scholar] [CrossRef]
- Van Giau, V.; An, S.S. Emergence of exosomal miRNAs as a diagnostic biomarker for Alzheimer’s disease. J. Neurol. Sci. 2016, 360, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Piscopo, P.; Lacorte, E.; Feligioni, M.; Mayer, F.; Crestini, A.; Piccolo, L.; Bacigalupo, I.; Filareti, M.; Ficulle, E.; Confaloni, A.; et al. MicroRNAs and mild cognitive impairment: A systematic review. Ageing Res. Rev. 2019, 50, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Sheinerman, K.S.; Tsivinsky, V.G.; Crawford, F.; Mullan, M.J.; Abdullah, L.; Umansky, S.R. Plasma microRNA biomarkers for detection of mild cognitive impairment. Aging 2012, 4, 590–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, H.; Li, J.; Huang, L.; Chen, X.; Li, D.; Wang, T.; Hu, C.; Xu, J.; Zhang, C.; Zen, K.; et al. Serum MicroRNA Profiles Serve as Novel Biomarkers for the Diagnosis of Alzheimer’s Disease. Dis. Markers 2015, 2015, 11. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Li, X.; Xin, X.; Kan, P.C.; Yan, Y. MicroRNA-613 regulates the expression of brain-derived neurotrophic factor in Alzheimer’s disease. Biosci. Trends 2016, 10, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Sun, Y.; Lu, Z.; Leak, R.K.; Zhang, F. The impact of cerebrovascular aging on vascular cognitive impairment and dementia. Ageing Res. Rev. 2017, 34, 15–29. [Google Scholar] [CrossRef]
- Wang, W.X.; Rajeev, B.W.; Stromberg, A.J.; Ren, N.; Tang, G.; Huang, Q.; Rigoutsos, I.; Nelson, P.T. The expression of microRNA miR-107 decreases early in Alzheimer’s disease and may accelerate disease progression through regulation of beta-site amyloid precursor protein-cleaving enzyme 1. J. Neurosci.: Off. J. Soc. Neurosci. 2008, 28, 1213–1223. [Google Scholar] [CrossRef]
- Hu, Y.; Lan, W.; Miller, D. Next-Generation Sequencing for MicroRNA Expression Profile. Methods Mol. Biol. (Clifton, N.J.) 2017, 1617, 169–177. [Google Scholar]
- Wang, B.; Xi, Y. Challenges for MicroRNA Microarray Data Analysis. Microarrays (Basel, Switz.) 2013, 2, 34–50. [Google Scholar] [CrossRef]
- Androvic, P.; Valihrach, L.; Elling, J.; Sjoback, R.; Kubista, M. Two-tailed RT-qPCR: A novel method for highly accurate miRNA quantification. Nucleic Acids Res. 2017, 45, e144. [Google Scholar] [CrossRef]
- Nagaraj, S.; Laskowska-Kaszub, K.; Debski, K.J.; Wojsiat, J.; Dabrowski, M.; Gabryelewicz, T.; Kuznicki, J.; Wojda, U. Profile of 6 microRNA in blood plasma distinguish early stage Alzheimer’s disease patients from non-demented subjects. Oncotarget 2017, 8, 16122–16143. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; He, X.; Li, Y.; Wang, T. Cerebrospinal fluid CD4+ T lymphocyte-derived miRNA-let-7b can enhances the diagnostic performance of Alzheimer’s disease biomarkers. Biochem. Biophys. Res. Commun. 2018, 495, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.; Kuiperij, H.B.; Versleijen, A.A.; Chiasserini, D.; Farotti, L.; Baschieri, F.; Parnetti, L.; Struyfs, H.; De Roeck, N.; Luyckx, J.; et al. Validation of microRNAs in Cerebrospinal Fluid as Biomarkers for Different Forms of Dementia in a Multicenter Study. J. Alzheimer’s Dis. 2016, 52, 1321–1333. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, R.B.; Mufson, E.J.; Counts, S.E. Evidence for a neuroprotective microRNA pathway in amnestic mild cognitive impairment. Front. Neurosci. 2015, 9, 430. [Google Scholar] [CrossRef] [PubMed]
- Kayano, M.; Higaki, S.; Satoh, J.I.; Matsumoto, K.; Matsubara, E.; Takikawa, O.; Niida, S. Plasma microRNA biomarker detection for mild cognitive impairment using differential correlation analysis. Biomark Res. 2016, 4, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giau, V.V.; Bagyinszky, E.; Yang, Y.S.; Youn, Y.C.; An, S.S.A.; Kim, S.Y. Genetic analyses of early-onset Alzheimer’s disease using next generation sequencing. Sci. Rep. 2019, 9, 8368. [Google Scholar] [CrossRef]
- Bagyinszky, E.; Kang, M.J.; Pyun, J.; Van Giau, V.; An, S.S.A.; Kim, S. Early-onset Alzheimer’s disease patient with prion (PRNP) p. Val180Ile mutation. Neuropsychiatr. Dis. Treat. 2019, 15, 2003. [Google Scholar] [CrossRef]
- Shen, L.; An, S.S.A.; Bagyinszky, E.; Van Giau, V.; Choi, S.H.; Kim, S.Y. Novel GRN mutations in Koreans with Alzheimer’s disease. Mol. Cell. Toxicol. 2019, 15, 345–352. [Google Scholar] [CrossRef]
- Giau, V.V.; Senanarong, V.; Bagyinszky, E.; An, S.S.A.; Kim, S. Analysis of 50 Neurodegenerative Genes in Clinically Diagnosed Early-Onset Alzheimer’s Disease. Int. J. Mol. Sci. 2019, 20, 1514. [Google Scholar] [CrossRef]
- Bagyinszky, E.; Giau, V.V.; Youn, Y.C.; An, S.S.A.; Kim, S. Characterization of mutations in PRNP (prion) gene and their possible roles in neurodegenerative diseases. Neuropsychiatr. Dis. Treat. 2018, 14, 2067–2085. [Google Scholar] [CrossRef]
- Giau, V.V.; Bagyinszky, E.; An, S.S.A.; Kim, S. Clinical genetic strategies for early onset neurodegenerative diseases. Mol. Cell Toxicol. 2018, 14, 123–142. [Google Scholar] [CrossRef]
- Van Giau, V.; An, S.S.A.; Bagyinszky, E.; Kim, S. Gene panels and primers for next generation sequencing studies on neurodegenerative disorders. Mol. Cell Toxicol. 2015, 11, 89–143. [Google Scholar] [CrossRef]
- Bagyinszky, E.; Lee, H.M.; Van Giau, V.; Koh, S.B.; Jeong, J.H.; An, S.S.A.; Kim, S. PSEN1 p.Thr116Ile Variant in Two Korean Families with Young Onset Alzheimer’s Disease. Int. J. Mol. Sci. 2018, 19, 2604. [Google Scholar] [CrossRef] [PubMed]
- Giau, V.V.; Lee, H.; Shim, K.H.; Bagyinszky, E.; An, S.S.A. Genome-editing applications of CRISPR-Cas9 to promote in vitro studies of Alzheimer’s disease. Clin. Interv. Aging 2018, 13, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Giau, V.V.; Pyun, J.M.; Bagyinszky, E.; An, S.S.A.; Kim, S. A pathogenic PSEN2 p.His169Asn mutation associated with early-onset Alzheimer’s disease. Clin. Interv. Aging 2018, 13, 1321–1329. [Google Scholar] [CrossRef] [PubMed]
- Giau, V.V.; Wang, M.J.; Bagyinszky, E.; Youn, Y.C.; An, S.S.A.; Kim, S. Novel PSEN1 p.Gly417Ala mutation in a Korean patient with early-onset Alzheimer’s disease with parkinsonism. Neurobiol. Aging 2018, 72, 188.e13–188.e17. [Google Scholar] [CrossRef]
- Giau, V.V.; Wu, S.Y.; Jamerlan, A.; An, S.S.A.; Kim, S.Y.; Hulme, J. Gut Microbiota and Their Neuroinflammatory Implications in Alzheimer’s Disease. Nutrients 2018, 10, 1765. [Google Scholar] [CrossRef]
- Park, J.; An, S.S.A.; Giau, V.V.; Shim, K.; Youn, Y.C.; Bagyinszky, E.; Kim, S. Identification of a novel PSEN1 mutation (Leu232Pro) in a Korean patient with early-onset Alzheimer’s disease and a family history of dementia. Neurobiol. Aging 2017, 56, e11–e212. [Google Scholar] [CrossRef]
- Van Giau, V.; Senanarong, V.; Bagyinszky, E.; Limwongse, C.; An, S.S.A.; Kim, S. Identification of a novel mutation in APP gene in a Thai subject with early-onset Alzheimer’s disease. Neuropsychiatr. Dis. Treat. 2018, 14, 3015–3023. [Google Scholar] [CrossRef]
- Giau, V.V.; Bagyinszky, E.; An, S.S.; Kim, S.Y. Role of apolipoprotein E in neurodegenerative diseases. Neuropsychiatr. Dis. Treat. 2015, 11, 1723–1737. [Google Scholar] [CrossRef]
- Youn, Y.C.; Lim, Y.K.; Han, S.H.; Giau, V.V.; Lee, M.K.; Park, K.Y.; Kim, S.; Bagyinszky, E.; An, S.S.A.; Kim, H.R. Apolipoprotein epsilon7 allele in memory complaints: Insights through protein structure prediction. Clin. Interv. Aging 2017, 12, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Barabash, A.; Marcos, A.; Ancin, I.; Vazquez-Alvarez, B.; de Ugarte, C.; Gil, P.; Fernandez, C.; Encinas, M.; Lopez-Ibor, J.J.; Cabranes, J.A. APOE, ACT and CHRNA7 genes in the conversion from amnestic mild cognitive impairment to Alzheimer’s disease. Neurobiol. Aging 2009, 30, 1254–1264. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, A.; Hernández-Olasagarre, B.; Moreno-Grau, S.; Kleineidam, L.; Heilmann-Heimbach, S.; Hernández, I.; Wolfsgruber, S.; Wagner, H.; Rosende-Roca, M.; Mauleón, A.; et al. Exploring Genetic Associations of Alzheimer’s Disease Loci with Mild Cognitive Impairment Neurocognitive Endophenotypes. Front. Aging Neurosci. 2018, 10, 340. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.M.; Luo, J.Q.; Xu, L.Y.; Zhou, H.H.; Zhang, W. Harnessing low-density lipoprotein receptor protein 6 (LRP6) genetic variation and Wnt signaling for innovative diagnostics in complex diseases. Pharm. J. 2018, 18, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Buechler, J.; Salinas, P.C. Deficient Wnt Signaling and Synaptic Vulnerability in Alzheimer’s Disease: Emerging Roles for the LRP6 Receptor. Front. Synaptic Neurosci. 2018, 10, 38. [Google Scholar] [CrossRef] [PubMed]
- Mengel-From, J.; Thinggaard, M.; Lindahl-Jacobsen, R.; McGue, M.; Christensen, K.; Christiansen, L. CLU Genetic Variants and Cognitive Decline among Elderly and Oldest Old. PLoS ONE 2013, 8, e79105. [Google Scholar] [CrossRef] [PubMed]
- Mullan, G.M.; McEneny, J.; Fuchs, M.; McMaster, C.; Todd, S.; McGuinness, B.; Henry, M.; Passmore, A.P.; Young, I.S.; Johnston, J.A. Plasma clusterin levels and the rs11136000 genotype in individuals with mild cognitive impairment and Alzheimer’s disease. Curr. Alzheimer Res. 2013, 10, 973–978. [Google Scholar] [CrossRef]
- Fernandez-Martinez, M.; Elcoroaristizabal Martin, X.; Blanco Martin, E.; Galdos Alcelay, L.; Ugarriza Serrano, I.; Gomez Busto, F.; Alvarez-Alvarez, M.; Molano Salazar, A.; Bereincua Gandarias, R.; Ingles Borda, S.; et al. Oestrogen receptor polymorphisms are an associated risk factor for mild cognitive impairment and Alzheimer disease in women APOE {varepsilon}4 carriers: A case-control study. BMJ Open 2013, 3, e003200. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, Z.; Deng, L.; Bai, F.; Shi, Y.; Yu, H.; Xie, C.; Yuan, Y.; Zhang, Z. Genetic variation in angiotensin converting-enzyme affects the white matter integrity and cognitive function of amnestic mild cognitive impairment patients. J. Neurol. Sci. 2017, 380, 177–181. [Google Scholar] [CrossRef]
- Adams, H.H.; de Bruijn, R.F.; Hofman, A.; Uitterlinden, A.G.; van Duijn, C.M.; Vernooij, M.W.; Koudstaal, P.J.; Ikram, M.A. Genetic risk of neurodegenerative diseases is associated with mild cognitive impairment and conversion to dementia. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2015, 11, 1277–1285. [Google Scholar] [CrossRef] [Green Version]
- Thambisetty, M.; Lovestone, S. Blood-based biomarkers of Alzheimer’s disease: Challenging but feasible. Biomark Med. 2010, 4, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Negash, S. Mild cognitive impairment: An overview. CNS Spectr. 2008, 13, 45–53. [Google Scholar] [CrossRef]
- Rosenberg, P.B.; Mielke, M.M.; Appleby, B.; Oh, E.; Leoutsakos, J.M.; Lyketsos, C.G. Neuropsychiatric symptoms in MCI subtypes: The importance of executive dysfunction. Int. J. Geriatr. Psychiatry 2011, 26, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Mansbach, W.E.; Mace, R.A.; Clark, K.M. Mild cognitive impairment (MCI) in long-term care patients: Subtype classification and occurrence. Aging Ment. Health 2016, 20, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Putcha, D.; Tremont, G. Predictors of independence in instrumental activities of daily living: Amnestic versus nonamnestic MCI. J. Clin. Exp. Neuropsychol. 2016, 38, 991–1004. [Google Scholar] [CrossRef] [PubMed]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2011, 7, 270–279. [Google Scholar] [CrossRef]
- Diaz-Mardomingo, M.D.C.; Garcia-Herranz, S.; Rodriguez-Fernandez, R.; Venero, C.; Peraita, H. Problems in Classifying Mild Cognitive Impairment (MCI): One or Multiple Syndromes? Brain Sci. 2017, 7, 111. [Google Scholar] [CrossRef]
- Klekociuk, S.Z.; Summers, J.J.; Vickers, J.C.; Summers, M.J. Reducing false positive diagnoses in mild cognitive impairment: The importance of comprehensive neuropsychological assessment. Eur. J. Neurol. 2014, 21, 1330–1336, e82–e83. [Google Scholar] [CrossRef]
- Eliassen, C.F.; Reinvang, I.; Selnes, P.; Grambaite, R.; Fladby, T.; Hessen, E. Biomarkers in subtypes of mild cognitive impairment and subjective cognitive decline. Brain Behav. 2017, 7, e00776. [Google Scholar] [CrossRef] [Green Version]
- Van Giau, V.; An, S.S.A.; Hulme, J.P. Mitochondrial therapeutic interventions in Alzheimer’s disease. J. Neurol. Sci. 2018, 395, 62–70. [Google Scholar] [CrossRef]
- Van Giau, V.; Pyun, J.M.; Suh, J.; Bagyinszky, E.; An, S.S.A.; Kim, S.Y. A pathogenic PSEN1 Trp165Cys mutation associated with early-onset Alzheimer’s disease. BMC Neurol. 2019, 7, 188. [Google Scholar] [CrossRef] [PubMed]
- Bagyinszky, E.; Yang, Y.; Van Giau, V.; Youn, Y.C.; An, S.S.A.; Kim, S. Novel prion mutation (p. Tyr225Cys) in a Korean patient with atypical Creutzfeldt–Jakob disease. Clin. Interv. Aging 2019, 14, 1387–1397. [Google Scholar] [CrossRef]



| Controls | MCI Patients, Remained Stable | MCI Patients, Progressed to AD | AD | |
|---|---|---|---|---|
| A+T+N+ | 19% | 29% | 54% | 63% |
| A+T+N− | 9% | 19% | 30% | 19% |
| A+T−N− | 18% | 11% | 5% | 10% |
| A−T+N− | 10% | 6% | 1.5% | 2% |
| A−T+N+ | 7% | 5% | 1.5% | 2% |
| A−T−N− | 2% | NA | NA | NA |
| A+T−N+ | NA | NA | NA | NA |
| A−T−N− | 43% | 31% | 8% | 4% |
| Diagnosis | Aβ1–42 (pg/mL) | t-tau (pg/mL) | p-tau (pg/mL) | Diagnostic Criteria | Findings | Reference |
|---|---|---|---|---|---|---|
| Controls (n = 28) | 721 | 177 | 34 | MMSE & MDB | Aβ1-42 and p-tau predictive in MCI-AD conversion | Parnetti et al. (2012) [43] |
| MCI (n = 58) | 919 | 261 | 41 | |||
| MCI-AD (n = 32) | 480 | 475 | 90 | |||
| AD (n = 28) | 446 | 680 | 72 | |||
| Cut offs | 1372 | 416 | 59 | |||
| Controls (n = 114) | 205.63 | 69.65 | 24.84 | NINCDS-ADRDA | Tau and Aβ42 abnormalities are cognitive decline marker | Okonkwo et al. (2010) [44] |
| MCI (n = 95) | 163.31 | 103.54 | 35.68 | |||
| AD (n = 100) | 143.51 | 121.57 | 41.73 | |||
| Cut offs | 192 | 93 | 23 | |||
| Controls (n = 94) | 1325 | 217 | 19.0 | NIA-AA | Tau/Aβ ratios may be accurate marker for MCI/AD | Hansson et al. (2018) [45] |
| Early MCI (n = 272) | 1066 | 234 | 20.7 | |||
| Late MCI (n = 152) | 784 | 291 | 28.0 | |||
| AD (n = 128) | 595 | 340 | 33.8 | |||
| Cut offs | 880 | 0.33 | 0.028 | |||
| Controls (n = 41) | 503.99 | 86.03 | 41.59 | NINCDS-ADRDA | CSF biomarkers could have successful predictive value of AD/dementia | Forlenza et al. (2015) [46] |
| MCI (n = 68) | 410.91 | 88.38 | 45.92 | |||
| AD (n = 41) | 328.76 | 145.69 | 66.72 | |||
| Cut offs | 416 | 76.7 | 36.1 |
| Tool | Basic Properties | Advantages | Disadvantages | Reference |
|---|---|---|---|---|
| MDS | ELISA assay, which measures the toxic soluble Aβ oligomers in blood | Easy to perform, accessible, non-invasive, cost-effective, compared with CSF methods | Lower sensitivity than CSF methods. Level of blood biomarkers may be lower in plasma, compared with CSF | [30,31,32,33] |
| Simoa | Magnetic bead immunoassay on microfluidic array, detects oligomers in any biological fluids | Sensitive, quick, precise, flexible method, requires small sample size, | Requires special tool, higher cost | [35,36,37] |
| SQUID | Detects interactions between magnetic nanoparticles and biomarkers in any biological fluids | High sensitivity, flexible method, several markers can be monitored | Requires low temperatures, higher cost | [38,39] |
| CSF markers | Imaging and immunoassay methods, which screen Aβ42/Aβ40 ratio and Tau. Additional candidates were also discovered | Sensitive method, useful in differential diagnosis, useful in early diagnosis of cognitive decline | Higher cost, requires higher sample size, difficult to obtain | [48,49,50,51] |
| Reference | No. of Patients, Gender | Mean Age/Mean MMSE | Source | Screening Method/Validation Method | Dysregulated miRNAs | Functional Outcomes, Specificity and Sensitivity |
|---|---|---|---|---|---|---|
| Nagaraj et al. (2017) [111] | 7M/8F | 68.1 years/score 25.9 | Plasma without hemolysis and blood cells | RT-qPCR | Increased levels of miR486 and miR483-5p were the most significant indicators of MCI and AD. Also, upregulation of miR502-3p and miR-200a-3p in MCI and AD compared with NC was observed. | ROC indicated that miR483-5p and miR-502-3p are good tests to distinguish AD from NC, and MCI from NC (AUC > 0.9, specificity and sensitivity > 0.8, repeatedly, in both screening and validation studies). |
| Müller et al. (2016) [113] | 15M/22F | 73.1 years/score 24.8 | CSF | qPCR | Increased expression levels of miRNA-146a in MCI compared with NC were lost when confounding factors were considered. Similarly, increased expression levels of miRNA-27a, -125b, -146a in MCI compared with AD were lost after correcting for confounding factors. | After correcting for confounding factors, no differences in miRNA levels were found between AD, MCI and NC |
| Weinberg et al., (2015) [114] | 5M/5F | 82.9 years/score 28.0 | Frontal and interior temporal cortex obtained at postmortem (60% MCI as Braak stages III-VI) | Microarray/qPCR | miR-150 was upregulated in MCI, compared with NC. Also, two distinct clusters miR-212/miR-132 and miR-23a/miR-23b were significantly downregulated in MCI | SIFT1 mRNA levels were significantly upregulated by 40% in frontal cortex of MCI compared with AD and NC |
| Liu et al., (2018) [112] | 19M/17F, | 72.4 years/score 56.6 | CSF | RT-PCR | Let-7b was significantly increased in MCI compared with SMC. Let-7b expression in CD4+ lymphocyte population from MCI was higher than SMC. | Addition of let-7b improves diagnostic performance of Aβ40 and Aβ42, and of t-tau and p-tau |
| Kayano et al., (2016) [115] | 11M/12F, | 72.8 years/score 24.3 | Plasma | RT-qPCR | Differential correlation analysis was applied to the data set with 85 miRNAs. The 20 pairs of miRNAs which had the difference of correction coefficients > 0.8 were selected as biomarkers that distinguish MCI from NC | Two miRNA pairs miR-191/miR-101 and miR-103/miR-222 have the highest value AUC 0.96 and are good tests to distinguish MCI from NC. Also, miR-191 and miR-125b and miRN-590-5p have a high AUC > 0.95 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giau, V.V.; Bagyinszky, E.; An, S.S.A. Potential Fluid Biomarkers for the Diagnosis of Mild Cognitive Impairment. Int. J. Mol. Sci. 2019, 20, 4149. https://doi.org/10.3390/ijms20174149
Giau VV, Bagyinszky E, An SSA. Potential Fluid Biomarkers for the Diagnosis of Mild Cognitive Impairment. International Journal of Molecular Sciences. 2019; 20(17):4149. https://doi.org/10.3390/ijms20174149
Chicago/Turabian StyleGiau, Vo Van, Eva Bagyinszky, and Seong Soo A. An. 2019. "Potential Fluid Biomarkers for the Diagnosis of Mild Cognitive Impairment" International Journal of Molecular Sciences 20, no. 17: 4149. https://doi.org/10.3390/ijms20174149