lncRNAs in Non-Malignant Tissue Have Prognostic Value in Colorectal Cancer
Abstract
:1. Introduction
2. Results
2.1. Patient´s Characteristics
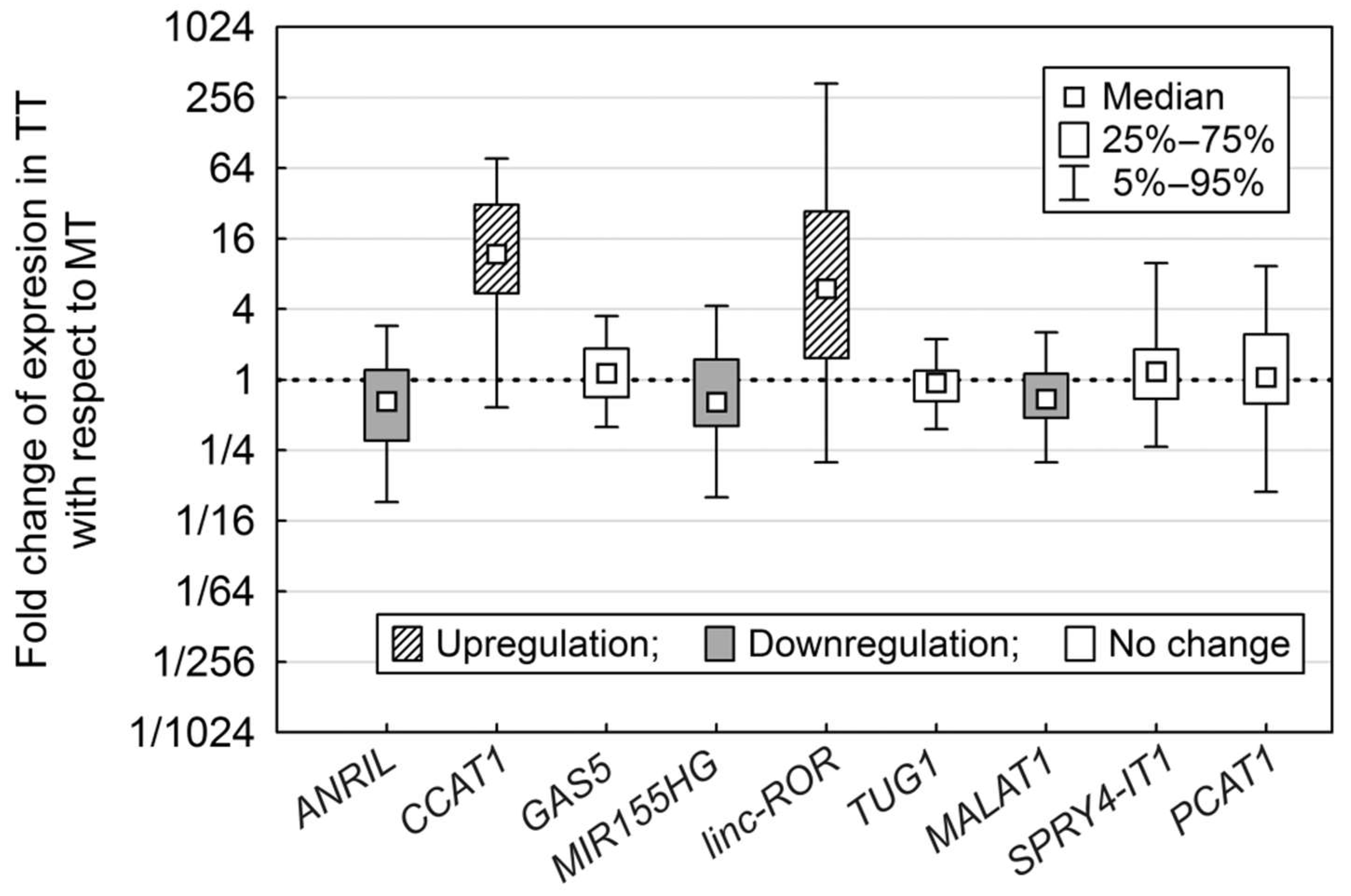
2.2. Expression Fold Change of lncRNAs (long non-coding RNAs) in Tumour Tissue (TT) Compared to Non-Malignant Tissue (MT)
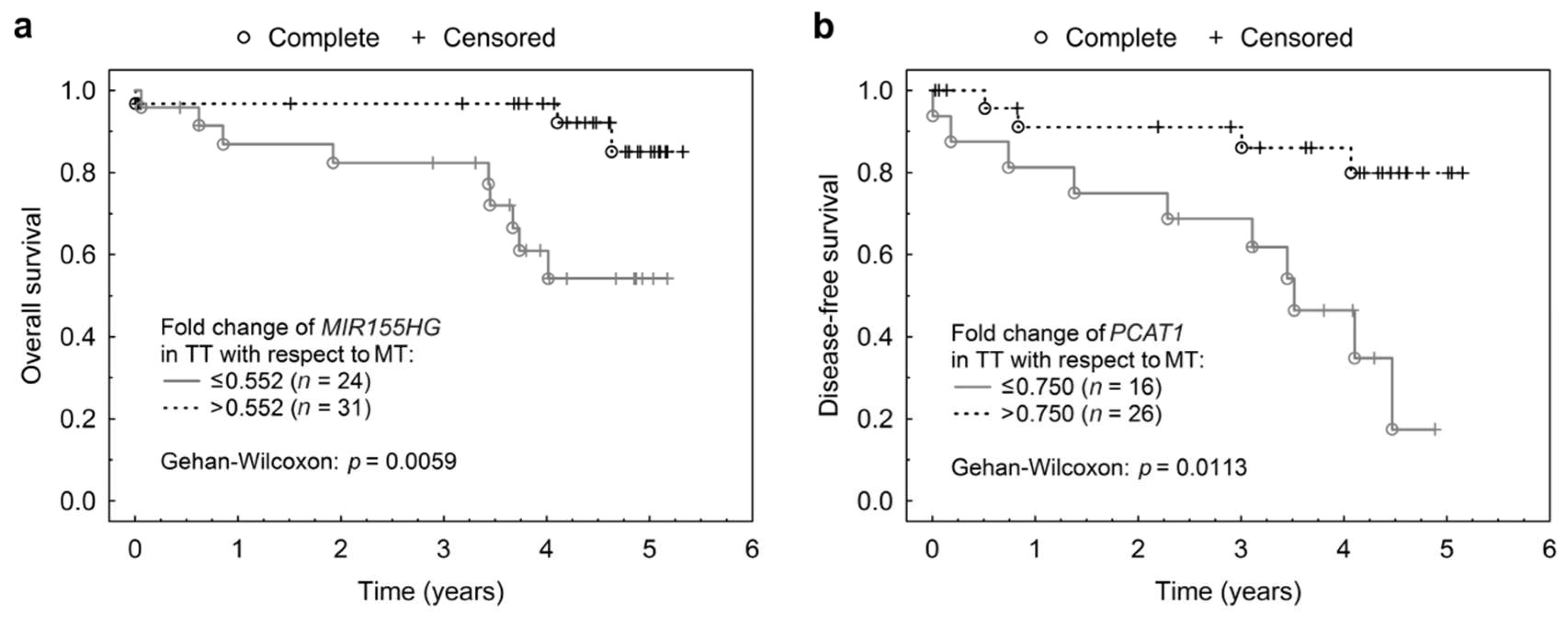
2.3. Expression of lncRNAs in Non-malignant and Tumour Tissue
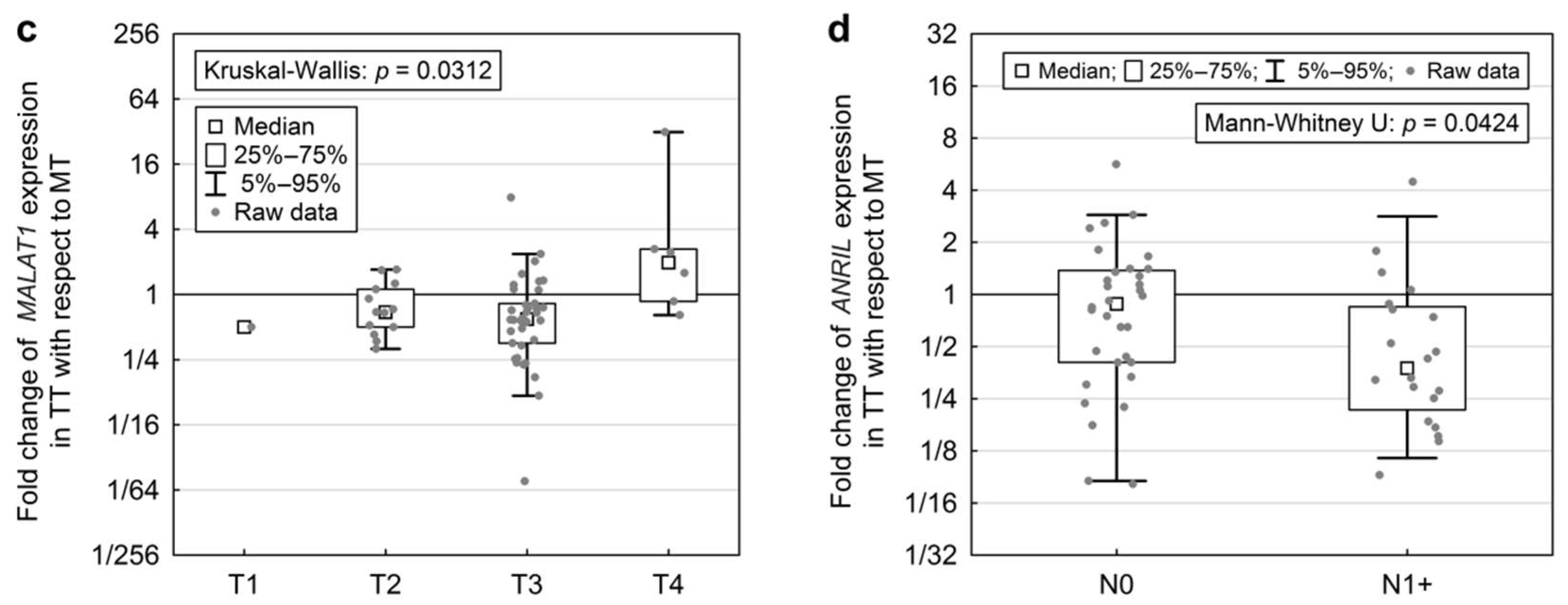
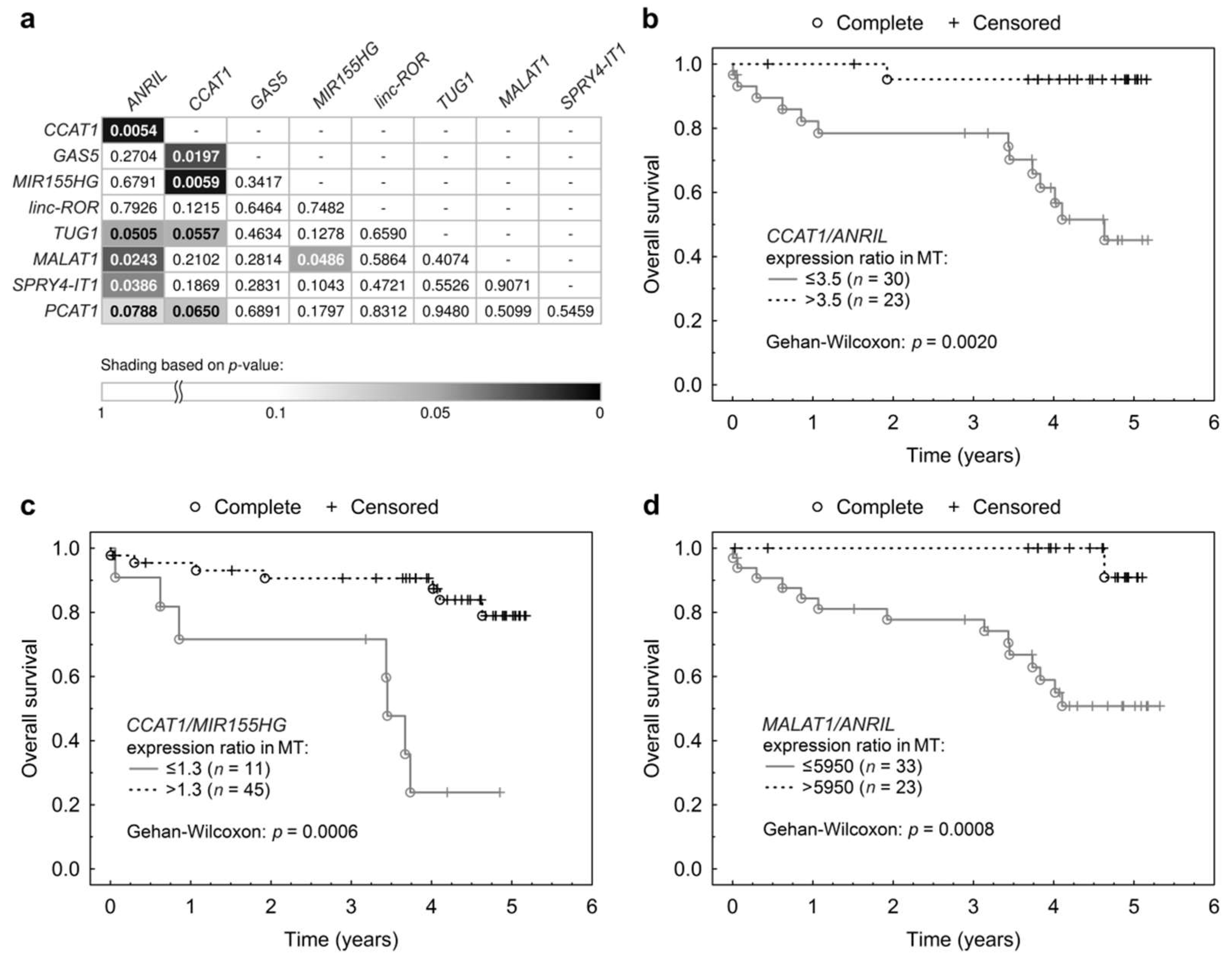
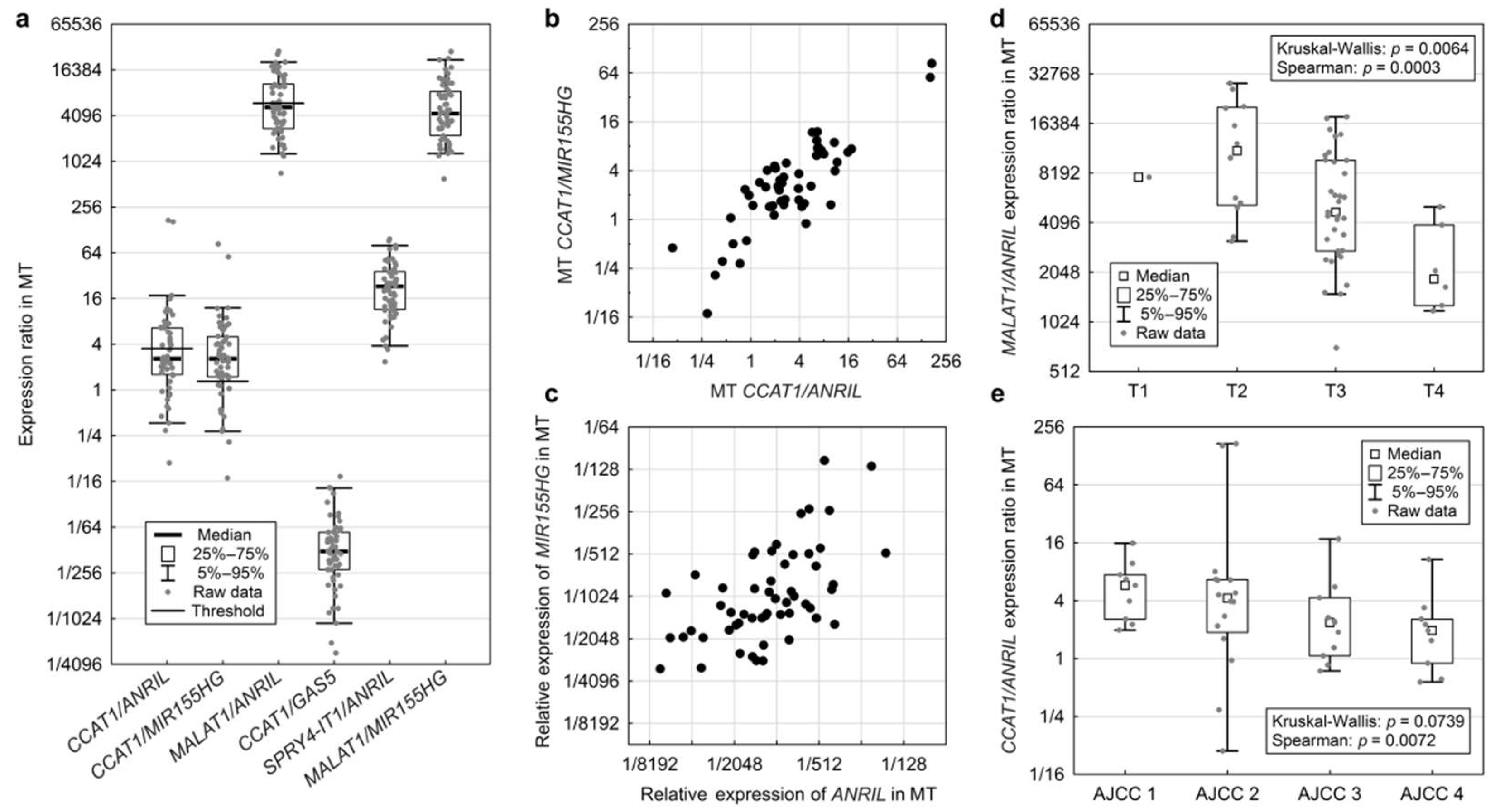
2.4. Expression Ratios of Two lncRNAs in Non-Malignant and Tumour Tissues
3. Discussion
3.1. Differential Expression Values in TT Compared to MT
3.2. Normalized Expression in TT and MT
3.3. lncRNA Expression Ratios
4. Materials and Methods
4.1. Patient Selection
4.2. RNA Extraction
4.3. RT-PCR
4.4. Quantitative-PCR (qPCR)
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AJCC | American joint committee on cancer |
| ANRIL | CDKN2B antisense RNA 1 |
| CCAT1 | Colon cancer associated transcript 1 |
| CCND | Cyclin D |
| CRC | Colorectal cancer |
| Ct | Cycle threshold |
| DFS | Disease free survival |
| EMT | Epithelial to mesenchymal transition |
| GAS5 | Growth arrest-specific 5 |
| HR | Hazard rate |
| Linc-ROR | Long intergenic non-protein coding regulator of reprogramming |
| lncRNA | Long non-coding RNA |
| MALAT1 | Metastasis associated lung adenocarcinoma transcript 1 |
| MIR155HG | MIR155 host gene |
| MMR | DNA mismatch repair |
| MT | Non-malignant (mucosa) tissue |
| OS | Overall survival |
| PCAT1 | Prostate cancer associated transcript 1 |
| q-PCR | Quantitative PCR |
| RT-PCR | Reverse transcription PCR |
| SPRY4-IT1 | Sprouty homolog 4 intronic transcript 1 |
| TP53 | Tumour protein p53 |
| TT | Tumour tissue |
| TUG1 | Taurine up-regulated 1 |
References
- Malvezzi, M.; Carioli, G.; Bertuccio, P.; Boffetta, P.; Levi, F.; Vecchia, C.L.; Negri, E. European cancer mortality predictions for the year 2017, with focus on lung cancer. Ann. Oncol. 2017, 28, 1117–1123. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fedewa, S.A.; Ahnen, D.J.; Meester, R.G.S.; Barzi, A.; Jemal, A. Colorectal cancer statistics, 2017. CA. Cancer J. Clin. 2017, 67, 177–193. [Google Scholar] [CrossRef] [PubMed]
- What Are the Survival Rates for Colorectal Cancer, By Stage? Available online: https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/survival-rates.html (accessed on 2 February 2018).
- Can Colorectal Polyps and Cancer Be Found Early? Available online: https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/detection.html (accessed on 2 February 2018).
- Hu, X.; Sood, A.K.; Dang, C.V.; Zhang, L. The role of long noncoding RNAs in cancer: The dark matter matters. Curr. Opin. Genet. Dev. 2018, 48, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Svoboda, M.; Slyskova, J.; Schneiderova, M.; Makovicky, P.; Bielik, L.; Levy, M.; Lipska, L.; Hemmelova, B.; Kala, Z.; Protivankova, M.; et al. HOTAIR long non-coding RNA is a negative prognostic factor not only in primary tumors, but also in the blood of colorectal cancer patients. Carcinogenesis 2014, 35, 1510–1515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Zhang, P.; Wang, L.; Piao, H.L.; Ma, L. Long non-coding RNA HOTAIR in carcinogenesis and metastasis. Acta Biochim. Biophys. Sin. 2014, 46, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Qiao, L.; Liu, X.; Tang, Y.; Zhao, Z.; Zhang, J.; Feng, Y. Down regulation of the long non-coding RNA PCAT-1 induced growth arrest and apoptosis of colorectal cancer cells. Life Sci. 2017, 188, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Bai, Y.; Luo, B.; Zhou, X. Upregulation of lncRNA BANCR associated with the lymph node metastasis and poor prognosis in colorectal cancer. Biol. Res. 2017, 50, 32. [Google Scholar] [CrossRef] [PubMed]
- Yin, D.; He, X.; Zhang, E.; Kong, R.; De, W.; Zhang, Z. Long noncoding RNA GAS5 affects cell proliferation and predicts a poor prognosis in patients with colorectal cancer. Med. Oncol. 2014, 31, 253. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhao, Z.; Feng, W.; Ye, Z.; Dai, W.; Zhang, C.; Peng, J.; Wu, K. Long non-coding RNA TUG1 promotes colorectal cancer metastasis via EMT pathway. Oncotarget 2016, 7, 51713–51719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, J.; Chu, Z.; Ma, P.; Meng, Y.; Yang, Y. Long non-coding RNA SPRY4-IT1 promotes proliferation and invasion by acting as a ceRNA of miR-101-3p in colorectal cancer cells. Tumor Biol. 2017, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, P.; Sun, L.; Liu, D.; Liu, C.; Sun, L. Long non-coding rna lincrna-ror promotes the progression of colon cancer and holds prognostic value by associating with miR-145. Pathol. Oncol. Res. 2016, 22, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Liu, Z.; Ning, X.; Huang, L.; Jiang, B. The long noncoding RNA HOTAIR promotes colorectal cancer progression by sponging miR-197. Oncol. Res. 2017. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.T.; Shi, D.B.; Wang, Y.W.; Li, X.X.; Xu, Y.; Tripathi, P.; Gu, W.L.; Cai, G.X.; Cai, S.J. High expression of lncRNA MALAT1 suggests a biomarker of poor prognosis in colorectal cancer. Int. J. Clin. Exp. Pathol. 2014, 7, 3174–3181. [Google Scholar] [PubMed]
- He, X.; Tan, X.; Wang, X.; Jin, H.; Liu, L.; Ma, L.; Yu, H.; Fan, Z. C-Myc-activated long noncoding RNA CCAT1 promotes colon cancer cell proliferation and invasion. Tumor Biol. 2014, 35, 12181–12188. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zheng, Z.P.; Li, H.; Zhang, H.Q.; Ma, F.Q. ANRIL is associated with the survival rate of patients with colorectal cancer, and affects cell migration and invasion in vitro. Mol. Med. Rep. 2016, 14, 1714–1720. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Zhou, N.; Huang, J.; Liu, Q.; Fukuda, K.; Ma, D.; Lu, Z.; Bai, C.; Watabe, K.; Mo, Y.Y. The human long non-coding RNA-RoR is a p53 repressor in response to DNA damage. Cell Res. 2013, 23, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wang, Y.; Yu, T.; Nie, E.; Hu, Q.; Wu, W.; Zhi, T.; Jiang, K.; Wang, X.; Lu, X.; et al. Blocking MIR155HG/miR-155 axis inhibits mesenchymal transition in glioma. Neuro Oncol. 2017, 19, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Dai, Y.; Wang, F.; Hou, S. Differentially expressed long non-coding RNAs and the prognostic potential in colorectal cancer. Neoplasma 2016, 63, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Liu, J.; Hu, Y.; Wang, W.; Xu, F.; Xu, W.; Han, J.; Biskup, E. STK31 as novel biomarker of metastatic potential and tumorigenicity of colorectal cancer. Oncotarget 2017, 8, 24354–24361. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.D.; Darnell, K.H.; Warnke, R.A.; Zehnder, J.L. CyclinD1/CyclinD3 ratio by real-time PCR improves specificity for the diagnosis of mantle cell lymphoma. J. Mol. Diagn. 2004, 6, 84–89. [Google Scholar] [CrossRef]
- Eis, P.S.; Tam, W.; Sun, L.; Chadburn, A.; Li, Z.; Gomez, M.F.; Lund, E.; Dahlberg, J.E. Accumulation of miR-155 and BIC RNA in human B cell lymphomas. Proc. Natl. Acad. Sci. USA 2005, 102, 3627–3632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valeri, N.; Gasparini, P.; Fabbri, M.; Braconi, C.; Veronese, A.; Lovat, F.; Adair, B.; Vannini, I.; Fanini, F.; Bottoni, A.; et al. Modulation of mismatch repair and genomic stability by miR-155. Proc. Natl. Acad. Sci. USA 2010, 107, 6982–6987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teng, G.; Papavasiliou, F.N. Shhh! Silencing by microRNA-155. Philos. Trans. R. Soc. B Biol. Sci. 2009, 364, 631–637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, G.J.; Xiao, H.X.; Tian, H.P.; Liu, Z.L.; Xia, S.S.; Zhou, T. Upregulation of microRNA-155 promotes the migration and invasion of colorectal cancer cells through the regulation of claudin-1 expression. Int. J. Mol. Med. 2013, 31, 1375–1380. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Chen, Z.; Xiang, J.; Gu, X. MicroRNA-155 acts as a tumor suppressor in colorectal cancer by targeting CTHRC1 in vitro. Oncol. Lett. 2018, 15, 5561–5568. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Song, J.H.; Kim, S.; Qu, P.; Martin, B.K.; Sehareen, W.S.; Haines, D.C.; Lin, P.C.; Sharan, S.K.; Chang, S. Loss of oncogenic miR-155 in tumor cells promotes tumor growth by enhancing C/EBP-β-mediated MDSC infiltration. Oncotarget 2016, 7, 11094–11112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Zhang, J.Q.; Chen, J.Z.; Chen, H.X.; Qiu, F.N.; Yan, M.L.; Chen, Y.L.; Peng, C.H.; Tian, Y.F.; Wang, Y.D. The over expression of long non-coding RNA ANRIL promotes epithelial-mesenchymal transition by activating the ATM-E2F1 signaling pathway in pancreatic cancer: An in vivo and in vitro study. Int. J. Biol. Macromol. 2017, 102, 718–728. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Ou, C.; Ren, W.; Xie, X.; Li, X.; Li, G. Downregulation of long non-coding RNA ANRIL suppresses lymphangiogenesis and lymphatic metastasis in colorectal cancer. Oncotarget 2016, 7, 47536–47555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Congrains, A.; Kamide, K.; Ohishi, M.; Rakugi, H. ANRIL: Molecular Mechanisms and Implications in Human Health. Int. J. Mol. Sci. 2013, 14, 1278–1292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunnington, M.S.; Santibanez Koref, M.; Mayosi, B.M.; Burn, J.; Keavney, B. Chromosome 9p21 SNPs Associated with Multiple Disease Phenotypes Correlate with ANRIL Expression. PLoS Genet. 2010, 6, e1000899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, N.; Papagiannakopoulos, T.; Pan, G.; Thomson, J.A.; Kosik, K.S. MicroRNA-145 regulates OCT4, SOX2, and KLF4 and represses pluripotency in human embryonic stem cells. Cell. 2009, 137, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Chen, Y.; Liao, X.; Liu, D.; Li, F.; Ruan, H.; Jia, W. Overexpression of long noncoding RNA PCAT-1 is a novel biomarker of poor prognosis in patients with colorectal cancer. Med. Oncol. 2013, 30, 588. [Google Scholar] [CrossRef] [PubMed]
- Prensner, J.R.; Chen, W.; Iyer, M.K.; Cao, Q.; Ma, T.; Han, S.; Sahu, A.; Malik, R.; Wilder-Romans, K.; Navone, N.; et al. PCAT-1, a long noncoding RNA, regulates BRCA2 and controls homologous recombination in cancer. Cancer Res. 2014, 74, 1651–1660. [Google Scholar] [CrossRef] [PubMed]
- PCAT1 Gene-GeneCards|PCAT1 RNA Gene. Available online: http://www.genecards.org/cgi-bin/carddisp.pl?gene=PCAT1 (accessed on 9 April 2018).
- Zhai, H.; Sui, M.; Yu, X.; Qu, Z.; Hu, J.; Sun, H.; Zheng, H.; Zhou, K.; Jiang, L. Overexpression of long non-coding RNA TUG1 promotes colon cancer progression. Med. Sci. Monit. 2016, 22, 3281–3287. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Ding, C.; Yang, Z.; Liu, T.; Zhang, X.; Zhao, C.; Wang, J. The long non-coding RNA TUG1 indicates a poor prognosis for colorectal cancer and promotes metastasis by affecting epithelial-mesenchymal transition. J. Transl. Med. 2016, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.; Cai, W.S.; Feng, Z.; Chen, J.; Feng, J.; Liu, Q.; Fang, Y.; Li, K.; Xiao, H.; Cao, J.; et al. Long non-coding RNA SPRY4-IT1 promotes colorectal cancer metastasis by regulate epithelial-mesenchymal transition. Oncotarget 2017, 8, 14479–14486. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Shen, Z.; Yan, Y.; Wang, B.; Zhang, J.; Shen, C.; Li, T.; Ye, C.; Gao, Z.; Peng, G.; et al. Long non-coding RNA GAS5 inhibits cell proliferation, induces G0/G1 arrest and apoptosis, and functions as a prognostic marker in colorectal cancer. Oncol. Lett. 2017, 13, 3151–3158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ji, Q.; Zhang, L.; Liu, X.; Zhou, L.; Wang, W.; Han, Z.; Sui, H.; Tang, Y.; Wang, Y.; Liu, N.; et al. Long non-coding RNA MALAT1 promotes tumour growth and metastasis in colorectal cancer through binding to SFPQ and releasing oncogene PTBP2 from SFPQ/PTBP2 complex. Br. J. Cancer 2014, 111, 736–748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwok, Z.H.; Roche, V.; Chew, X.H.; Fadieieva, A.; Tay, Y. A non-canonical tumor suppressive role for the long non-coding RNA MALAT1 in colon and breast cancers. Int. J. Cancer 2018, 143, 668–678. [Google Scholar] [CrossRef] [PubMed]
- Kozera, B.; Rapacz, M. Reference genes in real-time PCR. J. Appl. Genet. 2013, 54, 391–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Characteristic | Category | Number | % |
|---|---|---|---|
| gender | F | 24 | 38.1 |
| M | 39 | 61.9 | |
| age (in years) | 30–50 | 8 | 12.7 |
| 50–70 | 32 | 50.8 | |
| >70 | 23 | 36.5 | |
| T stage | T1 | 1 | 1.6 |
| T2 | 14 | 22.2 | |
| T3 | 40 | 63.5 | |
| T4 | 6 | 9.5 | |
| unknown | 2 | 3.2 | |
| N stage | N0 | 39 | 61.9 |
| N1 | 13 | 20.6 | |
| N2 | 10 | 15.9 | |
| unknown | 1 | 1.6 | |
| M stage | 0 | 47 | 74.6 |
| 1 | 11 | 17.5 | |
| unknown | 5 | 7.9 | |
| tumour grade | G1 | 12 | 19.0 |
| G2 | 42 | 66.7 | |
| G3 | 5 | 7.9 | |
| unknown | 4 | 6.3 | |
| AJCC staging | I | 11 | 17.5 |
| II | 19 | 30.2 | |
| III | 14 | 22.2 | |
| IV | 11 | 17.5 | |
| unknown | 8 | 12.7 | |
| primary tumour location | right or transversum | 16 | 25.4 |
| Left or sigma | 10 | 15.9 | |
| rectum or rectosigma | 31 | 49.2 | |
| non-specific | 6 | 9.5 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thiele, J.-A.; Hosek, P.; Kralovcova, E.; Ostasov, P.; Liska, V.; Bruha, J.; Vycital, O.; Rosendorf, J.; Opattova, A.; Horak, J.; et al. lncRNAs in Non-Malignant Tissue Have Prognostic Value in Colorectal Cancer. Int. J. Mol. Sci. 2018, 19, 2672. https://doi.org/10.3390/ijms19092672
Thiele J-A, Hosek P, Kralovcova E, Ostasov P, Liska V, Bruha J, Vycital O, Rosendorf J, Opattova A, Horak J, et al. lncRNAs in Non-Malignant Tissue Have Prognostic Value in Colorectal Cancer. International Journal of Molecular Sciences. 2018; 19(9):2672. https://doi.org/10.3390/ijms19092672
Chicago/Turabian StyleThiele, Jana-Aletta, Petr Hosek, Eva Kralovcova, Pavel Ostasov, Vaclav Liska, Jan Bruha, Ondrej Vycital, Jachym Rosendorf, Alena Opattova, Josef Horak, and et al. 2018. "lncRNAs in Non-Malignant Tissue Have Prognostic Value in Colorectal Cancer" International Journal of Molecular Sciences 19, no. 9: 2672. https://doi.org/10.3390/ijms19092672






