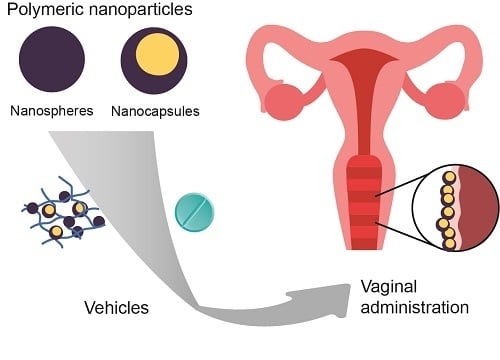
Approaches in Polymeric Nanoparticles for Vaginal Drug Delivery: A Review of the State of the Art
Abstract
:1. Introduction
2. Brief Description of the Anatomy of the Vagina
3. Definitions and Classification of Nanoparticles
4. Nanoparticles from Natural Polymers for Vaginal Treatments
5. Synthetic and Biodegradable Polymer-Based Nanoparticles
6. Nanoparticles Prepared from Synthetic Non-Biodegradable Polymers
7. Vehicles for the Administration of Polymeric Nanoparticles by the Vaginal Route
8. Conclusions and Future Trends
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Ensign, L.M.; Cone, R.; Hanes, J. Nanoparticle-based drug delivery to the vagina: A review. J. Control. Release 2014, 190, 500–514. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Nunes, R.; Machado, A.; Sarmento, B. Polymer-based nanocarriers for vaginal drug delivery. Adv. Drug Deliv. Rev. 2015, 92, 53–70. [Google Scholar] [CrossRef] [PubMed]
- Palmeira-de-Oliveira, R.; Palmeira-de-Oliveira, A.; Martinez-de-Oliveira, J. New strategies for local treatment of vaginal infections. Adv. Drug Deliv. Rev. 2015, 92, 105–122. [Google Scholar] [CrossRef] [PubMed]
- Vanić, Ž.; Škalko-Basnet, N. Nanoformulations for Vaginal Therapy. In Nanotechnology Applied to Pharmaceutical Technology; Rai, M., Alves dos Santos, C., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 183–221. ISBN 9783319702995. [Google Scholar]
- Date, A.A.; Destache, C.J. A review of nanotechnological approaches for the prophylaxis of HIV/AIDS. Biomaterials 2013, 34, 6202–6228. [Google Scholar] [CrossRef] [PubMed]
- Vanić, Z.; Škalko-Basnet, N. Mucosal nanosystems for improved topical drug delivery: Vaginal route of administration. J. Drug Deliv. Sci. Technol. 2014, 24, 435–444. [Google Scholar] [CrossRef]
- Das Neves, J.; Amaral, M.H.; Bahia, M.F. Vaginal Drug Delivery. In Pharmaceutical Manufacturing Handbook: Production and Processes; Wiley: New York, NY, USA, 2007; pp. 809–878. [Google Scholar] [CrossRef]
- Krukemeyer, M.; Krenn, V.; Huebner, F. History and Possible Uses of Nanomedicine Based on Nanoparticles and Nanotechnological Progress. J. Nanomed. Nanotechnol. 2015, 6, 1–7. [Google Scholar] [CrossRef]
- Tang, Z.; He, C.; Tian, H.; Ding, J.; Hsiao, B.S.; Chu, B.; Chen, X. Polymeric nanostructured materials for biomedical applications. Prog. Polym. Sci. 2016, 60, 86–128. [Google Scholar] [CrossRef]
- Gültekİn, H.E.; Değİm, Z. Biodegradable Polymeric Nanoparticles are effective Systems for Controlled Drug Delivery. FABAD J. Pharm. Sci. 2013, 38, 107–118. [Google Scholar]
- Amoabediny, G.; Haghiralsadat, F.; Naderinezhad, S.; Helder, M.N.; Akhoundi Kharanaghi, E.; Mohammadnejad Arough, J.; Zandieh-Doulabi, B. Overview of preparation methods of polymeric and lipid-based (noisome, solid lipid, liposome) nanoparticles: A comprehensive review. Int. J. Polym. Mater. Polym. Biomater. 2018, 67, 1–18. [Google Scholar] [CrossRef]
- Nguyen, N.-T.; Shaegh, S.A.M.; Kashaninejad, N.; Phan, D.-T. Design, fabrication and characterization of drug delivery systems based on lab-on-a-chip technology. Adv. Drug Deliv. Rev. 2013, 65, 1403–1419. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, R.H.; Patravale, V.B.; Joshi, M.D. Polymeric nanoparticles for targeted treatment in oncology: Current insights. Int. J. Nanomed. 2015, 10, 1001–1018. [Google Scholar] [CrossRef]
- De Jong, W.H.; Borm, P.J.A. Drug delivery and nanoparticles: Applications and hazzards. Int. J. Nanomed. 2008, 3, 133–149. [Google Scholar] [CrossRef]
- Quintanar-Guerrero, D.; Fessi, H.; Allémann, E.; Doelker, E. Influence of stabilizing agents and preparative variables on the formation of poly(d,l-lactic acid) nanoparticles by an emulsification-diffusion technique. Int. J. Pharm. 1996, 143, 133–141. [Google Scholar] [CrossRef]
- Quintanar-Guerrero, D.; Allémann, E.; Doelker, E.; Fessi, H. A mechanistic study of the formation of polymer nanoparticles by the emulsification-diffusion technique. Colloid Polym. Sci. 1997, 275, 640–647. [Google Scholar] [CrossRef]
- Hillareau, H.; Couvreur, P. Polymeric nanoparticles as drug carriers. In Polymers in Drug Delivery; Uchegbu, I.F., Schatzlein, A.G., Eds.; CRC: Boca Ratón, FL, USA, 2006; pp. 101–110. ISBN 0849325331. [Google Scholar]
- Akala, E.O.; Okunola, O. Novel stealth degradable nanoparticles prepared by dispersion polymerization for the delivery of bioactive agents Part I. Pharm. Ind. 2013, 75, 1191–1196. [Google Scholar]
- Ogunwuyi, O.; Adesina, S.; Akala, E.O. d-Optimal mixture experimental design for stealth biodegradable crosslinked docetaxel-loaded poly-ε-caprolactone nanoparticles manufactured by dispersion polymerization. Pharmazie 2015, 70, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Kelkar, S.S.; Reineke, T.M. Theranostics: Combining imaging and therapy. Bioconjug. Chem. 2011, 22, 1879–1903. [Google Scholar] [CrossRef] [PubMed]
- Quintanar-Guerrero, D.; Allémann, E.; Fessi, H.; Doelker, E. Preparation Techniques and Mechanisms of Formation of Biodegradable Nanoparticles from Preformed Polymers. Drug Dev. Ind. Pharm. 1998, 24, 1113–1128. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, P.B.S.; Coelho, L.C.B.B.; Teixeira, L.A.T.; Carneiro-da-Cunha, M. Approaches in biotechnological applications of natural polymers. AIMS Mol. Sci. 2016, 3, 386–425. [Google Scholar] [CrossRef] [Green Version]
- Bhatia, S. Natural Polymer Drug Delivery Systems, 1st ed.; Springer International Publishing: Cham, Switzerland, 2016; ISBN 978-3-319-41128-6. [Google Scholar]
- Hamid Akash, M.S.; Rehman, K.; Chen, S. Natural and synthetic polymers as drug carriers for delivery of therapeutic proteins. Polym. Rev. 2015, 55, 371–406. [Google Scholar] [CrossRef]
- Rossi, S.; Vigani, B.; Puccio, A.; Bonferoni, M.C.; Sandri, G.; Ferrari, F. Chitosan ascorbate nanoparticles for the vaginal delivery of antibiotic drugs in atrophic vaginitis. Mar. Drugs 2017, 15. [Google Scholar] [CrossRef] [PubMed]
- De Castro Spadari, C.; Lopes, L.B.; Ishida, K. Potential use of alginate-based carriers as antifungal delivery system. Front. Microbiol. 2017, 8, 97. [Google Scholar] [CrossRef]
- Das, R.K.; Kasoju, N.; Bora, U. Encapsulation of curcumin in alginate-chitosan-pluronic composite nanoparticles for delivery to cancer cells. Nanomed. Nanotechnol. Biol. Med. 2010, 6, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Baspinar, Y.; Üstündas, M.; Bayraktar, O.; Sezgin, C. Curcumin and piperine loaded zein-chitosan nanoparticles: Development and in-vitro characterisation. Saudi Pharm. J. 2018, 26, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Marciello, M.; Rossi, S.; Caramella, C.; Remuñán-López, C. Freeze-dried cylinders carrying chitosan nanoparticles for vaginal peptide delivery. Carbohydr. Polym. 2017, 170, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Shapira, A.; Assaraf, Y.G.; Epstein, D.; Livney, Y.D. Beta-casein nanoparticles as an oral delivery system for chemotherapeutic drugs: Impact of drug structure and properties on co-assembly. Pharm. Res. 2010, 27, 2175–2186. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Felipe, L.; Silva, E.F.; Araújo, K.C.; Fabrino, D.L. Lactoferrin, chitosan and Melaleuca alternifolia—Natural products that show promise in candidiasis treatment. Braz. J. Microbiol. 2018, 49, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Berginc, K.; Suljaković, S.; Škalko-Basnet, N.; Kristl, A. Mucoadhesive liposomes as new formulation for vaginal delivery of curcumin. Eur. J. Pharm. Biopharm. 2014, 87, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Severino, R.; Vu, K.D.; Donsì, F.; Salmieri, S.; Ferrari, G.; Lacroix, M. Antibacterial and physical effects of modified chitosan based-coating containing nanoemulsion of mandarin essential oil and three non-thermal treatments against Listeria innocua in green beans. Int. J. Food Microbiol. 2014, 191, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Sekar, V.; Rajendran, K.; Vallinayagam, S.; Deepak, V.; Mahadevan, S. Synthesis and characterization of chitosan ascorbate nanoparticles for therapeutic inhibition for cervical cancer and their in silico modeling. J. Ind. Eng. Chem. 2018, 62, 239–249. [Google Scholar] [CrossRef]
- Damelin, L.H.; Fernandes, M.A.; Tiemessen, C.T. Alginate microbead-encapsulated silver complexes for selective delivery of broad-spectrum silver-based microbicides. Int. J. Antimicrob. Agents 2015, 46, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Manna, S.; Lakshmi, U.S.; Racharla, M.; Sinha, P.; Kanthal, L.K.; Kumar, S.P.N. Bioadhesive HPMC gel containing gelatin nanoparticles for intravaginal delivery of tenofovir. J. Appl. Pharm. Sci. 2016, 6, 22–29. [Google Scholar] [CrossRef]
- Akbari, A.; Wu, J. Ovomucin nanoparticles: Promising carriers for mucosal delivery of drugs and bioactive compounds. Drug Deliv. Transl. Res. 2017, 7, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.; Cunha-Reis, C.; Araújo, F.; Nunes, R.; Seabra, V.; Ferreira, D.; das Neves, J.; Sarmento, B. Development and in vivo safety assessment of tenofovir-loaded nanoparticles-in-film as a novel vaginal microbicide delivery system. Acta Biomater. 2016, 44, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Ramyadevi, D.; Rajan, K.S.; Vedhahari, B.N.; Ruckmani, K.; Subramanian, N. Heterogeneous polymer composite nanoparticles loaded in situ gel for controlled release intra-vaginal therapy of genital herpes. Colloids Surf. B Biointerfaces 2016, 146, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Reis, C.; Machado, A.; Barreiros, L.; Araújo, F.; Nunes, R.; Seabra, V.; Ferreira, D.; Segundo, M.A.; Sarmento, B.; das Neves, J. Nanoparticles-in-film for the combined vaginal delivery of anti-HIV microbicide drugs. J. Control. Release 2016, 243, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Sarmento, B. Precise engineering of dapivirine-loaded nanoparticles for the development of anti-HIV vaginal microbicides. Acta Biomater. 2015, 18, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Pérez, B.; Quintanar-Guerrero, D.; Tapia-Tapia, M.; Cisneros-Tamayo, R.; Zambrano-Zaragoza, M.L.; Alcalá-Alcalá, S.; Mendoza-Muñoz, N.; Piñón-Segundo, E. Controlled-release biodegradable nanoparticles: From preparation to vaginal applications. Eur. J. Pharm. Sci. 2018, 115, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Mert, O.; Lai, S.K.; Ensign, L.; Yang, M.; Wang, Y.Y.; Wood, J.; Hanes, J. A poly(ethylene glycol)-based surfactant for formulation of drug-loaded mucus penetrating particles. J. Control. Release 2012, 157, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Sáenz, M.; Espina, M.; Bolaños, N.; Calpena, A.C.; Gomara, M.J.; Haro, I.; García, M.L. Penetration of polymeric nanoparticles loaded with an HIV-1 inhibitor peptide derived from GB virus C in a vaginal mucosa model. Eur. J. Pharm. Biopharm. 2017, 120, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Mohideen, M.; Quijano, E.; Song, E.; Deng, Y.; Panse, G.; Zhang, W.; Clark, M.R.; Saltzman, W.M. Degradable bioadhesive nanoparticles for prolonged intravaginal delivery and retention of elvitegravir. Biomaterials 2017, 144, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.A.; Chaves, P.S.; D’Amore, C.M.; Contri, R.V.; Frank, A.G.; Beck, R.C.R.; Pohlmann, A.R.; Buffon, A.; Guterres, S.S. The use of chitosan as cationic coating or gel vehicle for polymeric nanocapsules: Increasing penetration and adhesion of imiquimod in vaginal tissue. Eur. J. Pharm. Biopharm. 2017, 114, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Amiji, M.; Bahia, M.F.; Sarmento, B. Assessing the physical-chemical properties and stability of dapivirine-loaded polymeric nanoparticles. Int. J. Pharm. 2013, 456, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Steinbach, J.M.; Weller, C.E.; Booth, C.J.; Saltzman, W.M. Polymer nanoparticles encapsulating siRNA for treatment of HSV-2 genital infection. J. Control. Release 2012, 162, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Michiels, J.; Ariën, K.K.; Vanham, G.; Amiji, M.; Bahia, M.F.; Sarmento, B. Polymeric nanoparticles affect the intracellular delivery, antiretroviral activity and cytotoxicity of the microbicide drug candidate dapivirine. Pharm. Res. 2012, 29, 1468–1484. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Araújo, F.; Andrade, F.; Amiji, M.; Bahia, M.F.; Sarmento, B. Biodistribution and pharmacokinetics of Dapivirine-loaded nanoparticles after vaginal delivery in mice. Pharm. Res. 2014, 31, 1834–1845. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Amiji, M.; Sarmento, B. Mucoadhesive nanosystems for vaginal microbicide development: Friend or foe? Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2011, 3, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99, 28–51. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Saucier-Sawyer, J.K.; Hoimes, C.J.; Zhang, J.; Seo, Y.E.; Andrejecsk, J.W.; Saltzman, W.M. The effect of hyperbranched polyglycerol coatings on drug delivery using degradable polymer nanoparticles. Biomaterials 2014, 35, 6595–6602. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.K.; O’Hanlon, D.E.; Harrold, S.; Man, S.T.; Wang, Y.-Y.; Cone, R.; Hanes, J. Rapid transport of large polymeric nanoparticles in fresh undiluted human mucus. Proc. Natl. Acad. Sci. USA 2007, 104, 1482–1487. [Google Scholar] [CrossRef] [PubMed]
- Cu, Y.; Booth, C.J.; Saltzman, W.M. In vivo distribution of surface-modified PLGA nanoparticles following intravaginal delivery. J. Control. Release 2011, 156, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Van Eyk, A.D.; Van Der Bijl, P. Porcine vaginal mucosa as an in vitro permeability model for human vaginal mucosa. Int. J. Pharm. 2005, 305, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Lai, S.K.; Yu, T.; Wang, Y.Y.; Happe, C.; Zhong, W.; Zhang, M.; Anonuevo, A.; Fridley, C.; Hung, A.; et al. Nanoparticle penetration of human cervicovaginal mucus: The effect of polyvinyl alcohol. J. Control. Release 2014, 192, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Popov, A.; Enlow, E.; Bourassa, J.; Chen, H. Mucus-penetrating nanoparticles made with “mucoadhesive” poly(vinyl alcohol). Nanomed. Nanotechnol. Biol. Med. 2016, 12, 1863–1871. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.H.-Y.; Simmons, A.; Poole-Warren, L.A. Non-degradable polymer nanocomposites for drug delivery. Expert Opin. Drug Deliv. 2011, 8, 765–778. [Google Scholar] [CrossRef] [PubMed]
- Major, I.; Fuenmayor, E.; McConville, C. The Production of Solid Dosage Forms from Non-Degradable Polymers. Curr. Pharm. Des. 2016, 22, 2738–2760. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.S.; Lorenzoni, A.; Pegoraro, N.S.; Denardi, L.B.; Alves, S.H.; Schaffazick, S.R.; Cruz, L. Formulation and in vitro evaluation of coconut oil-core cationic nanocapsules intended for vaginal delivery of clotrimazole. Colloids Surf. B Biointerfaces 2014, 116, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Cassano, R.; Ferrarelli, T.; Mauro, M.V.; Cavalcanti, P.; Picci, N.; Trombino, S. Preparation, characterization and in vitro activities evaluation of solid lipid nanoparticles based on PEG-40 stearate for antifungal drugs vaginal delivery. Drug Deliv. 2016, 23, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.S.; Lorenzoni, A.; Ferreira, L.M.; Mattiazzi, J.; Adams, A.I.H.; Denardi, L.B.; Alves, S.H.; Schaffazick, S.R.; Cruz, L. Clotrimazole-loaded Eudragit® RS100 nanocapsules: Preparation, characterization and in vitro evaluation of antifungal activity against Candida species. Mater. Sci. Eng. C 2013, 33, 1389–1394. [Google Scholar] [CrossRef] [PubMed]
- De Lima, J.A.; Paines, T.C.; Motta, M.H.; Weber, W.B.; dos Santos, S.S.; Cruz, L.; da Silva, C.D.B. Novel Pemulen/Pullulan blended hydrogel containing clotrimazole-loaded cationic nanocapsules: Evaluation of mucoadhesion and vaginal permeation. Mater. Sci. Eng. C 2017, 79, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Contri, R.V.; Kulkamp-Guerreiro, I.C.; da Silva, S.J.; Frank, L.A.; Pohlmann, A.R.; Guterres, S.S. Nanoencapsulation of Rose-Hip Oil Prevents Oil Oxidation and Allows Obtainment of Gel and Film Topical Formulations. AAPS PharmSciTech 2016, 17, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Vedha Hari, B.N.; Narayanan, N.; Dhevedaran, K. Efavirenz–eudragit E-100 nanoparticle-loaded aerosol foam for sustained release: In-Vitro and ex-vivo evaluation. Chem. Pap. 2015, 69, 358–367. [Google Scholar] [CrossRef]
- Hari, B.N.V.; Narayanan, N.; Dhevendaran, K.; Ramyadevi, D. Engineered nanoparticles of Efavirenz using methacrylate co-polymer (Eudragit-E100) and its biological effects in-vivo. Mater. Sci. Eng. C 2016, 67, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Cautela, M.P.; Moshe, H.; Sosnik, A.; Sarmento, B.; das Neves, J. Composite films for vaginal delivery of tenofovir disoproxil fumarate and emtricitabine. Eur. J. Pharm. Biopharm. 2018. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.-W.; Giri, N.; Lee, C.H. pH-sensitive Eudragit nanoparticles for mucosal drug delivery. Int. J. Pharm. 2011, 403, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Guterres, S.; Frank, L.A.; Sandri, G.; D’Autilia, F.; Contri, R.V.; Bonferoni, M.C.; Caramella, C.; Frank, A.G.; Pohlmann, A.R. Chitosan gel containing polymeric nanocapsules: A new formulation for vaginal drug delivery. Int. J. Nanomed. 2014, 9, 3151–3161. [Google Scholar] [CrossRef] [PubMed]
- Contri, R.V.; Fiel, L.A.; Alnasif, N.; Pohlmann, A.R.; Guterres, S.S.; Schäfer-Korting, M. Skin penetration and dermal tolerability of acrylic nanocapsules: Influence of the surface charge and a chitosan gel used as vehicle. Int. J. Pharm. 2016, 507, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Date, A.A.; Shibata, A.; Goede, M.; Sanford, B.; La Bruzzo, K.; Belshan, M.; Destache, C.J. Development and evaluation of a thermosensitive vaginal gel containing raltegravir+efavirenz loaded nanoparticles for HIV prophylaxis. Antivir. Res. 2012, 96, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Dunton, C.; Holtz, D.; Parva, M.; Stampler, K.; Forwood, M.; Gogoi, R.; Lace, M.J.; Anderson, D.G.; Sawicki, J.A. DNA nanotherapy for pre-neoplastic cervical lesions. Gynecol. Oncol. 2013, 128, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Ramyadevi, D.; Rajan, K.S. Synthesis of hybrid polymer blend nanoparticles and incorporation into in situ gel foam spray for controlled release therapy using a versatile synthetic purine nucleoside analogue antiviral drug. RSC Adv. 2015, 5, 12956–12973. [Google Scholar] [CrossRef]
- Akil, A.; Parniak, M.A.; Dezzutti, C.S.; Moncla, B.J.; Cost, M.R.; Li, M.; Rohan, L.C. Development and characterization of a vaginal film containing dapivirine, a non-nucleoside reverse transcriptase inhibitor (NNRTI), for prevention of HIV-1 sexual transmission. Drug Deliv. Transl. Res. 2011, 1, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Das Neves, J.; Sarmento, B. Antiretroviral drug-loaded nanoparticles-in-films: A new option for developing vaginal microbicides? Expert Opin. Drug Deliv. 2017, 14, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Yang, S.; Ho, E.A. Biodegradable Film for the Targeted Delivery of siRNA-Loaded Nanoparticles to Vaginal Immune Cells. Mol. Pharm. 2015, 12, 2889–2903. [Google Scholar] [CrossRef] [PubMed]


| Loaded Drug | Natural Polymer | Preparation Method | Treatment | Main | Findings |
|---|---|---|---|---|---|
| Afamoxicillin trihydrate | Chitosan ascorbate | Ionotropic gelation | Atrophic Vaginitis | Particle size was 210–268 nm according to the % of Afamoxicillin encapsulated | Antibacterial expressed as minimal concentration of antibiotic was 0.004% for S. pyogenes and 0.0001% for E. hirae [25] |
| Ascorbic acid | Chitosan | Ionotropic gelation | Cervical Cancer | Particle size decreased with increase of ascorbic acid load in chitosan | An increase in chitosan-ascorbic acid concentration declined the survival of HeLa cells [34] |
| Insulin | Chitosan | Ionotropic gelation | Model for peptides delivery | Cylindrical sponges prepared by freeze-drying with different excipient type (mannitol, sucrose, gelatin) | Confirmed the good penetration properties of nanoparticles for use in the treatment of sexually transmitted diseases [29] |
| Silver saccharinate (AgS) | Alginate | Reverse emulsification | HSV-2 and Neisseria gonorrhoeae inhibition | Silver saccharinate showed excellent stability in vaginal fluid simulant | Silver saccharinate showed prevention both of HIV-1 infection and STIs via sexual intercourse in women [35] |
| Tenofovir | Gelatin | Desolvation method | Sexual transmission of HIV in women | Particle size was 294.7–445 nm | The in vitro dissolution study for nanoparticle formulation revealed sustained release of Tenofovir over 8 h [36] |
| Ciprofloxacin Riboflavin | Ovomucin | Nano-precipitation | Not reported | Ovomucin is suitable for encapsulating heat-sensitive drugs | Ovomucin particles exhibited sustained release; particles were resistant to degradation in both simulated mucus media and intestinal fluid [37] |
| Drug or Active Compound | Polymer(s) | Preparation Method | Diameter (nm) | AE, EE, or DL (%) | Findings |
|---|---|---|---|---|---|
| Tenofovir | PLGA 50:50 | Double emulsion-solvent evaporation | 118 | AE = 18.5 | When 12.5% of PLGA was substituted for stearylamine, the drug association increased to 48.4%. Nanoparticles were incorporated into a HPMC/PVA-based film [38]. |
| Acyclovir | PVPK30-EC (F1) | Nano-precipitation | 403 (F1) | DL = 80 | Freeze-dried nanoparticles were incorporated into Pluronic® F-127 gel [39]. |
| PVPK30-ERSPO (F2) | 99 (F2) | ||||
| Efavirenz | PLGA 50:50 | Emulsion-solvent evaporation | 275 | AE = 96.8 | Efavirenz-loaded nanoparticles and free tenofovir were incorporated into fast-dissolving films (72% HPMC, 18% PVA, 10% glycerin) [40]. |
| Dapivirine | PLGA 50:50 | Emulsion-solvent evaporation | 168 | DL = 1.8 | An enhanced safety profile of drug-loaded nanoparticles over free dapivirine. A decrease in drug permeability with increased epithelial cell membrane retention [41]. |
| AE = 90.2 | |||||
| Clotrimazole | PLGA 50:50 | Emulsification-diffusion | 492 | DL = 68.2 | Mucoadhesive chitosan-coated nanoparticles showed an increment in antifungal activity inhibition compared to drug solution [42]. |
| Paclitaxel | PLGA 50:50 | Solvent diffusion/nano-precipitation | 245 | DL = 7.9 | Mucus-penetrating nanoparticles. In vitro paclitaxel sustained release for 5 days [43]. |
| An HIV fusion inhibitor peptide (E2) | PLGA 50:50 | Double emulsion method-solvent evaporation | 305 | EE = 62.0 | Mucoadhesive nanoparticles covered with glycol-chitosan with mobility across the mucus [44]. |
| Elvitegravir (EVG) | PLA conjugated with HPG | Nano-emulsion protocol | 135 non-adhesive | EE = 94 | Both nanoparticles demonstrated a slower and more stable release up to 3 days in simulated vaginal fluid [45]. |
| 131 bioadhesive | |||||
| Imiquimod | PCL | Interfacial deposition | 199 uncoating | EE = 97 uncoating | Chitosan-coated PCL nanocapsules were incorporated into HEC gel, and uncoated PCL nanocapsules were incorporated into chitosan hydrogel. The latter formulation showed the most promising performance for the treatment of human papillomavirus [46]. |
| 213 coating with chitosan | EE = 57 coating with chitosan | ||||
| Dapivirine | PCL | Solvent displacement method | 194 (PEO-PPO-PEO) | AE = 97.8, DL = 12.8 (PEO-PPO-PEO) | Three surface-engineered dapivirine-loaded, PCL-based nanoparticles were obtained using PEO-PPO-PEO, SLS, or CTAB as surface modifiers. Negatively charged nanoparticles were stable up to 1 year; as for CTAB–PCL nanoparticles, particle aggregation was observed [47]. |
| 178 (SLS) | AE = 97.5, DL = 12.8 (SLS) | ||||
| 185 (CTAB) | AE = 97.8, DL = 12.8 (CTAB) | ||||
| siRNA against nectin-1 | PLGA 50:50 | Double emulsion-solvent evaporation | 299 (3:1) | EE = 92 (3:1) | Three complexes were formed between the siRNA and spermidine at molar ratios of the polyamine nitrogen to the nucleotide phosphate (N:P ratio) of 3:1, 8:1, or 14:1, ahead of nanoparticles preparation. The intravaginal administration with nanoparticles of PLGA encapsulating siRNA molecules was effective for the prevention of genital HSV-2 infections in mice [48]. |
| 331 (8:1) | EE = 82 (8:1) | ||||
| 323 (14:1) | EE = 43 (14:1) | ||||
| Dapivirine | PCL | Solvent displacement method | 198 (PEO-PPO-PEO) | AE = 97.3, DL = 12.7 (PEO-PPO-PEO) | Nanoparticles with three different surface modifiers: PEO-PPO-PEO, SLS, or CTAB. Antiretroviral activity of nanoparticles was determined in different cell models, as well as their cytotoxicity. CTAB-PCL nanoparticles provided higher intracellular concentrations of dapivirine than the two other formulations in VK2/E6E7 human vaginal epithelial cells [49]. |
| 182 (SLS) | AE = 97.6, DL = 12.7 (SLS) | ||||
| 193 (CTAB) | AE = 97.9, DL = 12.8 (CTAB) | ||||
| Dapivirine | PCL | Solvent displacement method | 199 | AE = 97.6 | Dapivirine-loaded PCL nanoparticles coated with PEO-PPO-PEO. Nanoparticles were rapidly eliminated after vaginal administration (mouse model) but able to distribute throughout the vagina and lower uterus, and capable of tackling mucus and penetrating the epithelial lining [50]. |
| DL = 12.7 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leyva-Gómez, G.; Piñón-Segundo, E.; Mendoza-Muñoz, N.; Zambrano-Zaragoza, M.L.; Mendoza-Elvira, S.; Quintanar-Guerrero, D. Approaches in Polymeric Nanoparticles for Vaginal Drug Delivery: A Review of the State of the Art. Int. J. Mol. Sci. 2018, 19, 1549. https://doi.org/10.3390/ijms19061549
Leyva-Gómez G, Piñón-Segundo E, Mendoza-Muñoz N, Zambrano-Zaragoza ML, Mendoza-Elvira S, Quintanar-Guerrero D. Approaches in Polymeric Nanoparticles for Vaginal Drug Delivery: A Review of the State of the Art. International Journal of Molecular Sciences. 2018; 19(6):1549. https://doi.org/10.3390/ijms19061549
Chicago/Turabian StyleLeyva-Gómez, Gerardo, Elizabeth Piñón-Segundo, Néstor Mendoza-Muñoz, María L. Zambrano-Zaragoza, Susana Mendoza-Elvira, and David Quintanar-Guerrero. 2018. "Approaches in Polymeric Nanoparticles for Vaginal Drug Delivery: A Review of the State of the Art" International Journal of Molecular Sciences 19, no. 6: 1549. https://doi.org/10.3390/ijms19061549