Prognostic Relevance of Methylenetetrahydrofolate Reductase Polymorphisms for Prostate Cancer
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Patient Recruitment and Data Collection
4.2. Single-Nucleotide Polymorphism (SNP) Selection and Genotyping
4.3. Human Tissue Complementary DNA (cDNA) Array and TaqMan Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR) Analysis
4.4. Statistical Analysis
4.5. Bioinformatics Analysis
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kim, Y.I. Folate and carcinogenesis: Evidence, mechanisms, and implications. J. Nutr. Biochem. 1999, 10, 66–88. [Google Scholar] [CrossRef]
- Duthie, S.J.; Narayanan, S.; Brand, G.M.; Pirie, L.; Grant, G. Impact of folate deficiency on DNA stability. J. Nutr. 2002, 132, 2444S–2449S. [Google Scholar] [PubMed]
- Fang, J.Y.; Zhu, S.S.; Xiao, S.D.; Jiang, S.J.; Shi, Y.; Chen, X.Y.; Zhou, X.M.; Qian, L.F. Studies on the hypomethylation of c-myc, c-ha-ras oncogenes and histopathological changes in human gastric carcinoma. J. Gastroenterol. Hepatol. 1996, 11, 1079–1082. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Jiang, X.; Chen, X.; Chen, L.; Li, X.; Jia, Y. The protective effect of methylenetetrahydrofolate reductase C677T polymorphism against prostate cancer risk: Evidence from 23 case-control studies. Gene 2015, 565, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Yadav, U.; Rai, V. Methylenetetrahydrofolate reductase gene C677T polymorphism and breast cancer risk: Evidence for genetic susceptibility. Meta Gene 2015, 6, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Yang, L.J.; Deng, M.Z.; Luo, Y.Y.; Wu, S.; Xiong, L.; Wang, D.; Liu, Y.; Liu, H. Mthfr C677T and A1298C polymorphisms and risk of lung cancer: A comprehensive evaluation. Genet. Mol. Res. 2016, 15. [Google Scholar] [CrossRef] [PubMed]
- Frosst, P.; Blom, H.J.; Milos, R.; Goyette, P.; Sheppard, C.A.; Matthews, R.G.; Boers, G.J.; den Heijer, M.; Kluijtmans, L.A.; van den Heuvel, L.P.; et al. A candidate genetic risk factor for vascular disease: A common mutation in methylenetetrahydrofolate reductase. Nat. Genet. 1995, 10, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Gulzar, Z.G.; McKenney, J.K.; Brooks, J.D. Increased expression of nusap in recurrent prostate cancer is mediated by E2F1. Oncogene 2013, 32, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Kollmeyer, T.M.; Morlan, B.W.; Anderson, S.K.; Bergstralh, E.J.; Davis, B.J.; Asmann, Y.W.; Klee, G.G.; Ballman, K.V.; Jenkins, R.B. A tissue biomarker panel predicting systemic progression after PSA recurrence post-definitive prostate cancer therapy. PLoS ONE 2008, 3, e2318. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.K.; Varga, J. The transcriptional coactivator and acetyltransferase p300 in fibroblast biology and fibrosis. J. Cell. Physiol. 2007, 213, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Debes, J.D.; Comuzzi, B.; Schmidt, L.J.; Dehm, S.M.; Culig, Z.; Tindall, D.J. P300 regulates androgen receptor-independent expression of prostate-specific antigen in prostate cancer cells treated chronically with interleukin-6. Cancer Res. 2005, 65, 5965–5973. [Google Scholar] [CrossRef] [PubMed]
- Swartz, M.D.; Peterson, C.B.; Lupo, P.J.; Wu, X.; Forman, M.R.; Spitz, M.R.; Hernandez, L.M.; Vannucci, M.; Shete, S. Investigating multiple candidate genes and nutrients in the folate metabolism pathway to detect genetic and nutritional risk factors for lung cancer. PLoS ONE 2013, 8, e53475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, Q.; Jiang, K.; Li, Q.; Ji, Y.J.; Chen, W.L.; Xue, X.H. Polymorphisms in the mthfr gene are associated with breast cancer risk and prognosis in a Chinese population. Tumor Biol. 2015, 36, 3757–3762. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, J.W.; Kang, G.H.; Park, N.H.; Song, Y.S.; Kang, S.B.; Lee, H.P. Polymorphism in folate- and methionine-metabolizing enzyme and aberrant CpG island hypermethylation in uterine cervical cancer. Gynecol. Oncol. 2005, 96, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Bao, B.Y.; Pao, J.B.; Lin, V.C.; Huang, C.N.; Chang, T.Y.; Lan, Y.H.; Lu, T.L.; Lee, H.Z.; Chen, L.M.; Ting, W.C.; et al. Individual and cumulative association of prostate cancer susceptibility variants with clinicopathologic characteristics of the disease. Clin. Chim. Acta 2010, 411, 1232–1237. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.P.; Huang, L.C.; Ting, W.C.; Chen, L.M.; Chang, T.Y.; Lu, T.L.; Lan, Y.H.; Liu, C.C.; Yang, W.H.; Lee, H.Z.; et al. Prognostic significance of prostate cancer susceptibility variants on prostate-specific antigen recurrence after radical prostatectomy. Cancer Epidemiol. Biomark. Prev. 2009, 18, 3068–3074. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.P.; Lan, Y.H.; Lu, T.L.; Pao, J.B.; Chang, T.Y.; Lee, H.Z.; Yang, W.H.; Hsieh, C.J.; Chen, L.M.; Huang, L.C.; et al. Clinical significance of runt-related transcription factor 1 polymorphism in prostate cancer. BJU Int. 2011, 107, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.C.; Lin, V.C.; Huang, C.Y.; Liu, C.C.; Wang, J.S.; Wu, T.T.; Pu, Y.S.; Huang, C.H.; Huang, C.N.; Huang, S.P.; et al. Prognostic significance of cyclin d1 polymorphisms on prostate-specific antigen recurrence after radical prostatectomy. Ann. Surg. Oncol. 2013, 20, S492–S499. [Google Scholar] [CrossRef] [PubMed]
- Freedland, S.J.; Sutter, M.E.; Dorey, F.; Aronson, W.J. Defining the ideal cutpoint for determining PSA recurrence after radical prostatectomy: Prostate-specific antigen. Urology 2003, 61, 365–369. [Google Scholar] [CrossRef]
- Huang, S.P.; Levesque, E.; Guillemette, C.; Yu, C.C.; Huang, C.Y.; Lin, V.C.; Chung, I.C.; Chen, L.C.; Laverdiere, I.; Lacombe, L.; et al. Genetic variants in micrornas and microrna target sites predict biochemical recurrence after radical prostatectomy in localized prostate cancer. Int. J. Cancer 2014, 135, 2661–2667. [Google Scholar] [CrossRef] [PubMed]
- Genomes Project, C.; Abecasis, G.R.; Auton, A.; Brooks, L.D.; DePristo, M.A.; Durbin, R.M.; Handsaker, R.E.; Kang, H.M.; Marth, G.T.; McVean, G.A. An integrated map of genetic variation from 1092 human genomes. Nature 2012, 491, 56–65. [Google Scholar]
- Barrett, J.C.; Fry, B.; Maller, J.; Daly, M.J. Haploview: Analysis and visualization of ld and haplotype maps. Bioinformatics 2005, 21, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.D.; Kellis, M. Haploreg: A resource for exploring chromatin states, conservation, and regulatory motif alterations within sets of genetically linked variants. Nucleic Acids Res. 2012, 40, D930–D934. [Google Scholar] [CrossRef] [PubMed]
- Lonsdale, J.; Thomas, J.; Salvatore, M.; Phillips, R.; Lo, E.; Shad, S.; Hasz, R.; Walters, G.; Garcia, F.; Young, N.; et al. The genotype-tissue expression (GTEx) project. Nat. Genet. 2013, 45, 580–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pound, C.R.; Partin, A.W.; Eisenberger, M.A.; Chan, D.W.; Pearson, J.D.; Walsh, P.C. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999, 281, 1591–1597. [Google Scholar] [CrossRef] [PubMed]

| SNP ID | Location | Chromosome | Position | Alleles | MAF | p | ||
|---|---|---|---|---|---|---|---|---|
| Additive | Dominant | Recessive | ||||||
| rs3753582 | Intron 1 | 1 | 11805485 | T > G | 0.136 | 0.971 | 0.463 | - |
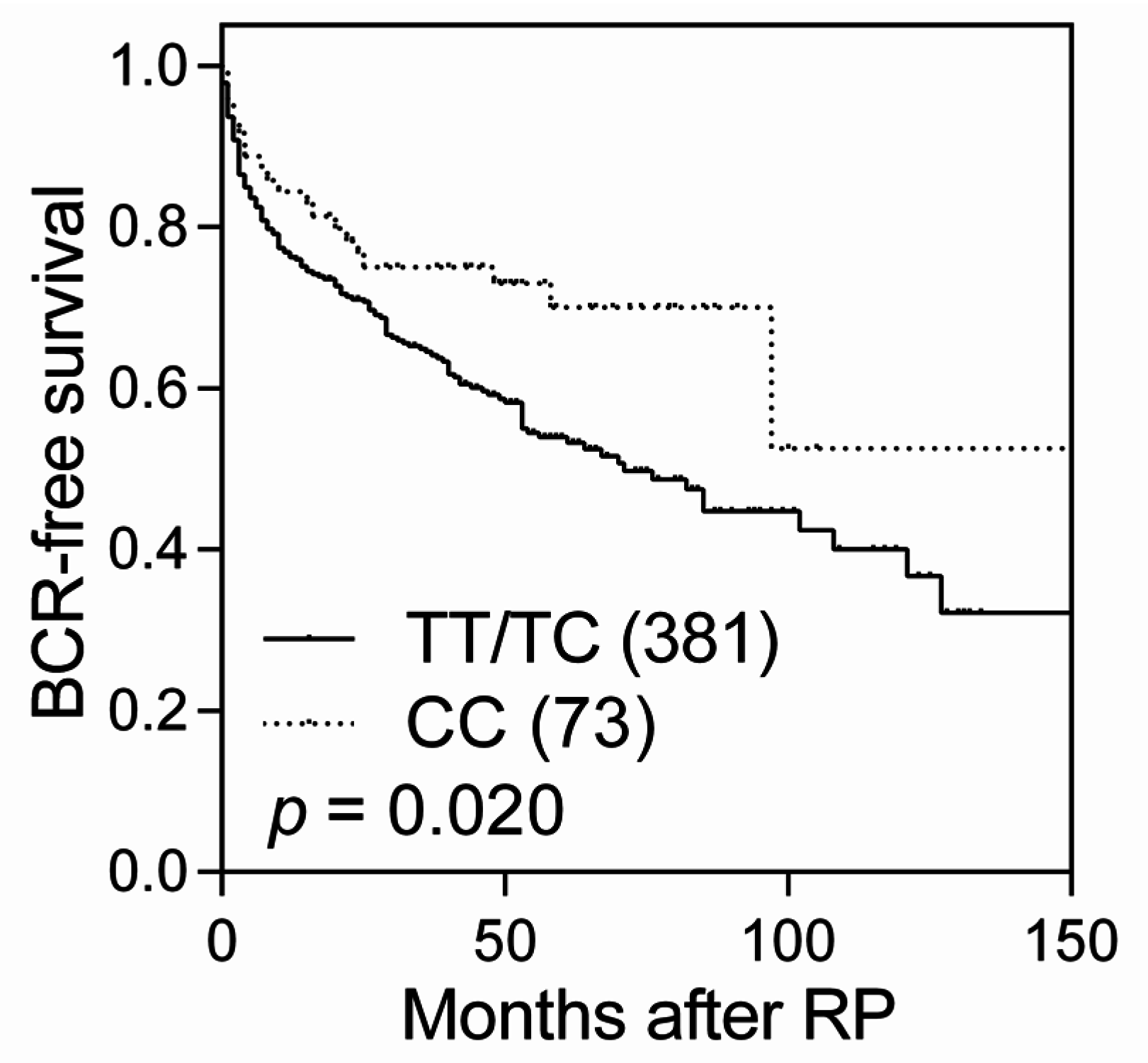
| rs9651118 | Intron 2 | 1 | 11802157 | T > C | 0.404 | 0.096 | 0.555 | 0.020 |
| rs1801133 | Exon 5 | 1 | 11796321 | C > T | 0.300 | 0.535 | 0.538 | 0.751 |
| SNP Genotype | Patients, n | BCR, n (%) | 5-Year BCR-Free Survival, % | HR (95% CI) | p | HR (95% CI) a | p a |
|---|---|---|---|---|---|---|---|
| rs9651118 | |||||||
| TT | 163 | 66 (40.5) | 54.6 | 1.00 | 1.00 | ||
| TC | 218 | 94 (43.1) | 53.3 | 1.03 (0.75–1.41) | 0.846 | 1.00 (0.68–1.47) | 0.997 |
| CC | 73 | 20 (27.4) | 70.1 | 0.59 (0.36–0.98) | 0.041 | 0.51 (0.26–1.02) | 0.057 |
| TC/CC vs. TT | 0.91 (0.67–1.24) | 0.559 | 0.89 (0.61–1.29) | 0.537 | |||
| CC vs. TT/TC | 0.58 (0.37–0.93) | 0.023 | 0.51 (0.27–0.98) | 0.044 | |||
| Trend | 0.84 (0.68–1.04) | 0.100 | 0.81 (0.62–1.07) | 0.132 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, V.C.; Lu, T.-L.; Yin, H.-L.; Yang, S.-F.; Lee, Y.-C.; Liu, C.-C.; Huang, C.-Y.; Yu, C.-C.; Chang, T.-Y.; Huang, S.-P.; et al. Prognostic Relevance of Methylenetetrahydrofolate Reductase Polymorphisms for Prostate Cancer. Int. J. Mol. Sci. 2016, 17, 1996. https://doi.org/10.3390/ijms17121996
Lin VC, Lu T-L, Yin H-L, Yang S-F, Lee Y-C, Liu C-C, Huang C-Y, Yu C-C, Chang T-Y, Huang S-P, et al. Prognostic Relevance of Methylenetetrahydrofolate Reductase Polymorphisms for Prostate Cancer. International Journal of Molecular Sciences. 2016; 17(12):1996. https://doi.org/10.3390/ijms17121996
Chicago/Turabian StyleLin, Victor C., Te-Ling Lu, Hsin-Ling Yin, Sheau-Fang Yang, Yung-Chin Lee, Chia-Chu Liu, Chao-Yuan Huang, Chia-Cheng Yu, Ta-Yuan Chang, Shu-Pin Huang, and et al. 2016. "Prognostic Relevance of Methylenetetrahydrofolate Reductase Polymorphisms for Prostate Cancer" International Journal of Molecular Sciences 17, no. 12: 1996. https://doi.org/10.3390/ijms17121996
APA StyleLin, V. C., Lu, T.-L., Yin, H.-L., Yang, S.-F., Lee, Y.-C., Liu, C.-C., Huang, C.-Y., Yu, C.-C., Chang, T.-Y., Huang, S.-P., & Bao, B.-Y. (2016). Prognostic Relevance of Methylenetetrahydrofolate Reductase Polymorphisms for Prostate Cancer. International Journal of Molecular Sciences, 17(12), 1996. https://doi.org/10.3390/ijms17121996







