Piper betle (L): Recent Review of Antibacterial and Antifungal Properties, Safety Profiles, and Commercial Applications
Abstract
:1. Introduction
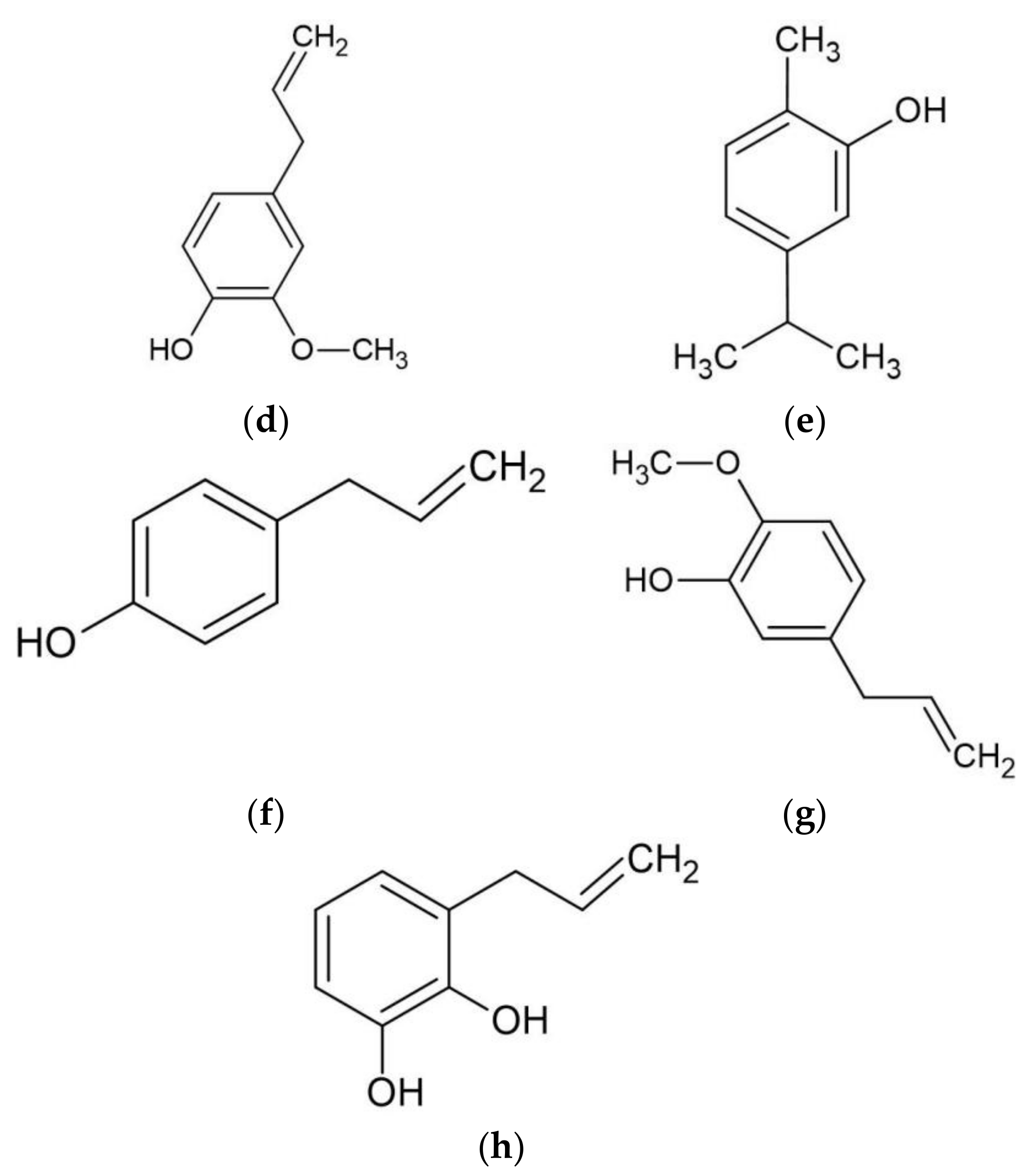
2. Phytochemicals in Betel Leaves
2.1. Betel Leaves Extract (BLE)
2.2. Betel Leaves Essential Oil (BLEO)
3. Antibacterial Property of Betel Leaves
4. Antifungal Properties of Betel Leaves
5. Safety Profiles of Betel Leaves
6. Commercial Application of Betel Leaves
7. Conclusions and Outlook
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fazal, F.; Mane, P.P.; Rai, M.P.; Thilakchand, K.R.; Bhat, H.P.; Kamble, P.S.; Palatty, P.L.; Baliga, M.S. The Phytochemistry, Traditional Uses and Pharmacology of Piper Betel. Linn (Betel Leaf): A Pan-Asiatic Medicinal Plant. Chin. J. Integr. Med. 2014. [Google Scholar] [CrossRef] [PubMed]
- Kaypetch, R.; Thaweboon, S. Antifungal Property of Piper Betle Leaf Oil against Oral Candida Species. Matec. Web Conf. 2018, 242, 01021. [Google Scholar] [CrossRef] [Green Version]
- Joesoef, M.R.; Sumampouw, H.; Linnan, M.; Schmid, S.; Idajadi, A.; St Louis, M.E. Douching and Sexually Transmitted Diseases in Pregnant Women in Surabaya, Indonesia. Am. J. Obs. Gynecol. 1996, 174, 115–119. [Google Scholar] [CrossRef]
- Chowdhury, U.; Baruah, P.K. Betelvine (Piper Betle L.): A Potential Source for Oral Care. Curr. Bot. 2020, 87–92. [Google Scholar] [CrossRef]
- Arambewela, L.; Arawwawala, M.; Withanage, D.; Kulatunga, S. Efficacy of Betel Cream on Skin Ailments. J. Complementary Integr. Med. 2010, 7. [Google Scholar] [CrossRef]
- Breijyeh, Z.; Jubeh, B.; Karaman, R. Resistance of Gram-Negative Bacteria to Current Antibacterial Agents and Approaches to Resolve It. Molecules 2020, 25, 1340. [Google Scholar] [CrossRef] [Green Version]
- Hafidh, R.R.; Abdulamir, A.S.; Vern, L.S.; Abu Bakar, F.; Abas, F.; Jahanshiri, F.; Sekawi, Z. Inhibition of Growth of Highly Resistant Bacterial and Fungal Pathogens by a Natural Product. Open Microbiol. J. 2011, 5, 96–106. [Google Scholar] [CrossRef]
- Akpan, A.; Morgan, R. Oral Candidiasis. Postgrad. Med. J. 2002, 78, 455–459. [Google Scholar] [CrossRef]
- Benedict, K.; Chiller, T.M.; Mody, R.K. Invasive Fungal Infections Acquired from Contaminated Food or Nutritional Supplements: A Review of the Literature. Foodborne Pathog. Dis. 2016, 13, 343–349. [Google Scholar] [CrossRef]
- Pawar, S.; Kalyankar, V.; Dhamangaonkar, B.; Dagade, S.; Waghmode, S.; Cukkemane, A. Biochemical Profiling of Antifungal Activity of Betel Leaf (Piper Betle L.) Extract and Its Significance in Traditional Medicine. J. Adv. Res. Biotechnol. 2017, 2, 1–4. [Google Scholar]
- Kaveti, B.; Tan, L.; Sarnnia; Kuan, T.S.; Baig, M. Antibacterial Activity Of Piper Betel Leaves. Int. J. Pharm. Teach. Pract. 2011, 2, 129–132. [Google Scholar]
- Taukoorah, U.; Lall, N.; Mahomoodally, F. Piper Betle L. (Betel Quid) Shows Bacteriostatic, Additive, and Synergistic Antimicrobial Action When Combined with Conventional Antibiotics. S. Afr. J. Bot. 2016, 105, 133–140. [Google Scholar] [CrossRef]
- Periyanayagam, K.; Jagadeesan, M.; Kavimani, S.; Vetriselvan, T. Pharmacognostical and Phyto-Physicochemical Profile of the Leaves of Piper Betle L. Var Pachaikodi (Piperaceae)—Valuable Assessment of Its Quality—ScienceDirect. Available online: https://www.sciencedirect.com/science/article/abs/pii/S2221169112602627 (accessed on 22 February 2021).
- Ali, A.; Lim, X.Y.; Wahida, P.F. The Fundamental Study of Antimicrobial Activity of Piper Betle Extract in Commercial Toothpastes. J. Herb. Med. 2018, 14, 29–34. [Google Scholar] [CrossRef]
- Kurnia, D.; Hutabarat, G.S.; Windaryanti, D.; Herlina, T.; Herdiyati, Y.; Satari, M.H. Potential Allylpyrocatechol Derivatives as Antibacterial Agent Against Oral Pathogen of S. Sanguinis ATCC 10,556 and as Inhibitor of MurA Enzymes: In Vitro and in Silico Study. Drug Des. Devel. 2020, 14, 2977–2985. [Google Scholar] [CrossRef]
- Srinivasan, R.; Devi, K.R.; Kannappan, A.; Pandian, S.K.; Ravi, A.V. Piper Betle and Its Bioactive Metabolite Phytol Mitigates Quorum Sensing Mediated Virulence Factors and Biofilm of Nosocomial Pathogen Serratia Marcescens in Vitro. J. Ethnopharmacol. 2016, 193, 592–603. [Google Scholar] [CrossRef]
- Teanpaisan, R.; Kawsud, P.; Pahumunto, N.; Puripattanavong, J. Screening for Antibacterial and Antibiofilm Activity in Thai Medicinal Plant Extracts against Oral Microorganisms. J. Tradit. Complementary Med. 2017, 7, 172–177. [Google Scholar] [CrossRef] [Green Version]
- Prakash, B.; Shukla, R.; Singh, P.; Kumar, A.; Mishra, P.K.; Dubey, N.K. Efficacy of Chemically Characterized Piper betle L. Essential Oil against Fungal and Aflatoxin Contamination of Some Edible Commodities and Its Antioxidant Activity. Int. J. Food Microbiol. 2010, 142, 114–119. [Google Scholar] [CrossRef]
- Karak, S.; Acharya, J.; Begum, S.; Mazumdar, I.; Kundu, R.; De, B. Essential Oil of Piper Betle L. Leaves: Chemical Composition, Anti-Acetylcholinesterase, Anti-β-Glucuronidase and Cytotoxic Properties. J. Appl. Res. Med. Aromat. Plants 2018, 10, 85–92. [Google Scholar] [CrossRef]
- Salehi, B.; Zakaria, Z.A.; Gyawali, R.; Ibrahim, S.A.; Rajkovic, J.; Shinwari, Z.K.; Khan, T.; Sharifi-Rad, J.; Ozleyen, A.; Turkdonmez, E.; et al. Piper Species: A Comprehensive Review on Their Phytochemistry, Biological Activities and Applications. Molecules 2019, 24, 1364. [Google Scholar] [CrossRef] [Green Version]
- Madhumita, M.; Guha, P.; Nag, A. Extraction of Betel Leaves (Piper Betle L.) Essential Oil and Its Bio-Actives Identification: Process Optimization, GC-MS Analysis and Anti-Microbial Activity. Ind. Crop. Prod. 2019, 138, 111578. [Google Scholar] [CrossRef]
- Tan, Y.P.; Chan, E.W.C. Antioxidant, Antityrosinase and Antibacterial Properties of Fresh and Processed Leaves of Anacardium Occidentale and Piper Betle. Food Biosci. 2014, 6, 17–23. [Google Scholar] [CrossRef]
- Mogana, R.; Adhikari, A.; Tzar, M.N.; Ramliza, R.; Wiart, C. Antibacterial Activities of the Extracts, Fractions and Isolated Compounds from Canarium Patentinervium Miq. against Bacterial Clinical Isolates. Bmc Complementary Med. Ther. 2020, 20, 55. [Google Scholar] [CrossRef] [Green Version]
- Aumeeruddy-Elalfi, Z.; Gurib-Fakim, A.; Mahomoodally, F. Antimicrobial, Antibiotic Potentiating Activity and Phytochemical Profile of Essential Oils from Exotic and Endemic Medicinal Plants of Mauritius. Ind. Crop. Prod. 2015, 71, 197–204. [Google Scholar] [CrossRef]
- Rashida, M.; Islam, I.; Haque, A.; Rahman, A.; Hossain, T.; Hamid, A. Antibacterial Activity of Polyaniline Coated Silver Nanoparticles Synthesized from Piper Betle Leaves Extract. Iran. J. Pharm. Res. 2016, 15, 591–597. [Google Scholar]
- Roy, A.; Guha, P. Formulation and Characterization of Betel Leaf (Piper Betle L.) Essential Oil Based Nanoemulsion and Its in Vitro Antibacterial Efficacy against Selected Food Pathogens. J. Food Process. Preserv. 2018, 42, e13617. [Google Scholar] [CrossRef]
- Valle, D.L.; Andrade, J.I.; Puzon, J.J.M.; Cabrera, E.C.; Rivera, W.L. Antibacterial Activities of Ethanol Extracts of Philippine Medicinal Plants against Multidrug-Resistant Bacteria. Asian Pac. J. Trop. Biomed. 2015, 5, 532–540. [Google Scholar] [CrossRef] [Green Version]
- Yoonus, J.; Resmi., R.; Beena, B. Greener Nanoscience: Piper Betel Leaf Extract Mediated Synthesis of CaO Nanoparticles and Evaluation of Its Antibacterial and Anticancer Activity. Mater. Today Proc. 2020. [Google Scholar] [CrossRef]
- Valle, D.L.; Cabrera, E.C.; Puzon, J.J.M.; Rivera, W.L. Antimicrobial Activities of Methanol, Ethanol and Supercritical CO2 Extracts of Philippine Piper Betle L. on Clinical Isolates of Gram Positive and Gram Negative Bacteria with Transferable Multiple Drug Resistance. PLoS ONE 2016, 11, e0146349. [Google Scholar] [CrossRef]
- Phumat, P.; Khongkhunthian, S.; Wanachantararak, P.; Okonogi, S. Potential of Piper Betle Extracts on Inhibition of Oral Pathogens. Drug Discov. 2017, 11, 307–315. [Google Scholar] [CrossRef] [Green Version]
- Abdi, R.D.; Kerro Dego, O. Antimicrobial Activity of Persicaria Pensylvanica Extract against Staphylococcus Aureus. Eur. J. Integr. Med. 2019, 29, 100921. [Google Scholar] [CrossRef]
- Srinivasan, R.; Santhakumari, S.; Ravi, A.V. In Vitro Antibiofilm Efficacy of Piper Betle against Quorum Sensing Mediated Biofilm Formation of Luminescent Vibrio Harveyi. Microb. Pathog. 2017, 110, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, M.F.; Sakinah, M.; Ismail, A.F.; Matsuura, T.; Zularisam, A.W. The Anti-Biofouling Effect of Piper Betle Extract against Pseudomonas Aeruginosa and Bacterial Consortium. Desalination 2012, 288, 24–30. [Google Scholar] [CrossRef]
- Barbieri, R.; Coppo, E.; Marchese, A.; Daglia, M.; Sobarzo-Sánchez, E.; Nabavi, S.F.; Nabavi, S.M. Phytochemicals for Human Disease: An Update on Plant-Derived Compounds Antibacterial Activity. Microbiol. Res. 2017, 196, 44–68. [Google Scholar] [CrossRef] [PubMed]
- Phumat, P.; Khongkhunthian, S.; Wanachantararak, P.; Okonogi, S. Comparative Inhibitory Effects of 4-Allylpyrocatechol Isolated from Piper Betle on Streptococcus Intermedius, Streptococcus Mutans, and Candida Albicans. Arch. Oral Biol. 2020, 113, 104690. [Google Scholar] [CrossRef]
- Faran Ali, S.M.; Tanwir, F. Oral Microbial Habitat a Dynamic Entity. J. Oral Biol. Craniofac. Res. 2012, 2, 181–187. [Google Scholar] [CrossRef] [Green Version]
- Lubis, R.R.; Marlisa; Wahyuni, D.D. Antibacterial Activity of Betle Leaf (Piper Betle L.) Extract on Inhibiting Staphylococcus Aureus in Conjunctivitis Patient. Am. J. Clin. Exp. Immunol. 2020, 9, 1–5. [Google Scholar]
- Ali, I.; Khan, F.G.; Suri, K.A.; Gupta, B.D.; Satti, N.K.; Dutt, P.; Afrin, F.; Qazi, G.N.; Khan, I.A. In Vitro Antifungal Activity of Hydroxychavicol Isolated from Piper Betle L. Ann. Clin. Microbiol. Antimicrob. 2010, 9, 7. [Google Scholar] [CrossRef] [Green Version]
- Sivareddy, B.; Reginald, B.A.; Sireesha, D.; Samatha, M.; Reddy, K.H.; Subrahamanyam, G. Antifungal Activity of Solvent Extracts of Piper Betle and Ocimum Sanctum Linn on Candida Albicans: An in Vitro Comparative Study. J. Oral Maxillofac. Pathol. 2019, 23, 333–337. [Google Scholar] [CrossRef]
- Aiemsaard, J.; Punareewattana, K. Antifungal Activities of Essential Oils of Syzygium Aromaticum, Piper Betle, and Ocimum Sanctum against Clinical Isolates of Canine Dermatophytes. Sci. Asia 2017, 43, 223. [Google Scholar] [CrossRef] [Green Version]
- Basak, S.; Guha, P. Use of Predictive Model to Describe Sporicidal and Cell Viability Efficacy of Betel Leaf (Piper Betle L.) Essential Oil on Aspergillus Flavus and Penicillium Expansum and Its Antifungal Activity in Raw Apple Juice. LWT 2017, 80, 510–516. [Google Scholar] [CrossRef]
- Nordin, M.-A.-F.; Wan Harun, W.H.A.; Abdul Razak, F. An in Vitro Study on the Anti-Adherence Effect of Brucea Javanica and Piper Betle Extracts towards Oral Candida. Arch. Oral Biol. 2013, 58, 1335–1342. [Google Scholar] [CrossRef]
- Bluma, R.; Amaiden, M.R.; Etcheverry, M. Screening of Argentine Plant Extracts: Impact on Growth Parameters and Aflatoxin B1 Accumulation by Aspergillus Section Flavi. Int. J. Food Microbiol. 2008, 122, 114–125. [Google Scholar] [CrossRef]
- de Oliveira Pereira, F.; Mendes, J.M.; de Oliveira Lima, E. Investigation on Mechanism of Antifungal Activity of Eugenol against Trichophyton Rubrum. Med. Mycol. 2013, 51, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Thuy, B.T.P.; Hieu, L.T.; My, T.T.A.; Hai, N.T.T.; Loan, H.T.P.; Thuy, N.T.T.; Triet, N.T.; Van Anh, T.T.; Dieu, N.T.X.; Quy, P.T.; et al. Screening for Streptococcus Pyogenes Antibacterial and Candida Albicans Antifungal Bioactivities of Organic Compounds in Natural Essential Oils of Piper Betle L., Cleistocalyx Operculatus L. and Ageratum Conyzoides L. Chem. Pap. 2020, 75, 1507–1519. [Google Scholar] [CrossRef]
- Pozo, J.L.D. Biofilm-Related Disease. Expert Rev. Anti-Infect. Ther. 2018, 16, 51–65. [Google Scholar] [CrossRef]
- Al-Adhroey, A.H.; Nor, Z.M.; Al-Mekhlafi, H.M.; Amran, A.A.; Mahmud, R. Antimalarial Activity of Methanolic Leaf Extract of Piper Betle L. Molecules 2010, 16, 107–118. [Google Scholar] [CrossRef]
- Sengupta, K.; Mishra, A.T.; Rao, M.K.; Sarma, K.V.; Krishnaraju, A.V.; Trimurtulu, G. Efficacy of an Herbal Formulation LI10903F Containing Dolichos Biflorus and Piper Betle Extracts on Weight Management. Lipids Health Dis. 2012, 11, 176. [Google Scholar] [CrossRef] [Green Version]
- Arambewela, L.S.R.; Arawwawala, L.D.A.M.; Kumaratunga, K.G.; Dissanayake, D.S.; Ratnasooriya, W.D.; Kumarasingha, S.P. Investigations on Piper Betle Grown in Sri Lanka. Pharm. Rev. 2011, 5, 159–163. [Google Scholar] [CrossRef] [Green Version]
- Madhumita, M.; Guha, P.; Nag, A. Bio-Actives of Betel Leaf (Piper Betle L.): A Comprehensive Review on Extraction, Isolation, Characterization, and Biological Activity. Phytother. Res. 2020, 34, 2609–2627. [Google Scholar] [CrossRef]
- Basak, S. The Use of Fuzzy Logic to Determine the Concentration of Betel Leaf Essential Oil and Its Potency as a Juice Preservative. Food Chem. 2018, 240, 1113–1120. [Google Scholar] [CrossRef]

| Classification | Compounds | Classification | Compounds |
|---|---|---|---|
| Monoterpenes | α-Thujene α-Pinene Camphene Sabinene Myrcene α-Terpinene β-Phellandrene 1,8-Cineole/Eucalyptol (E)-β-Ocimene γ-Terpinene Terpinolene Linalool Terpinen-4-ol α-Terpineol L-limonene Linalyl acetate | Sesquiterpenes | δ-Elemene α-Copaene β-Elemene E-β-Caryophyllene β-Copaene γ-Elemene Aromadendrene α-Humulene γ-Muurolene Germacrene D Germacrene B β-Selinene α-Selinene Bicyclogermacrene α-Muurolene cis-β-Guaiene δ-Cadinene or δ-amorphene Palustrol Spathulenol Caryophyllene oxide Globulol Viridiflorol Cubenol α-Cadinol Ledene α-amorphene Cubebene |
| Phenylpropanoids | Estragole/Methyl chavicol Chavicol Anethole/Isoestragole Safrole Chavicol acetate Eugenol Methyl eugenol Acetyl eugenol Phenyl acetaldehyde | Aldehydes | Undecanal Phenyl acetaldehyde |
| Extract/Preparation (Unit for Activities) | Method | Bacteria Species | Activities | Recalculated (%) | MBC/MIC | Inhibition Zone (mm) | Reference | ||
| MIC | MBC | MIC | MBC | ||||||
| Ethanol | Agar well diffusion | Pseudomenas aeruginosa | - | - | - | - | - | 6.7–7.2 | [11] |
| Escherichia coli | - | - | - | - | - | 8.9–11.0 | |||
| Water | Agar well diffusion | Pseudomenas aerugiaounosa | - | - | - | - | - | 7.2 | [11] |
| Escherichia coli | - | - | - | - | - | 8.5 | |||
| Ethanol ( µg/mL) | Disk diffusion | Escherichia coli ATCC 25922 | 625 | 625 | 0.0625 | 0.0625 | 1 * | 16 | [27] |
| Klebsiella pneumoniae ATCC BAA-1705 | 1250 | 1250 | 0.125 | 0.125 | 1 * | 17 | |||
| Pseudomenas aeruginosa ATCC 27853 | 625 | 625 | 0.0625 | 0.0625 | 1 * | 17 | |||
| MβL, Pseudomenas aeruginosa (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 17 | |||
| MβL, Acinetobacter baumannii (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 23 | |||
| ESβL, Escherichia coli (CI) | 312 | 625 | 0.0312 | 0.0625 | 2 * | 20 | |||
| ESβL, Klebsiella pneumoniae (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 20 | |||
| CRE, Klebsiella pneumoniae (CI) | 312 | 625 | 0.0312 | 0.0625 | 2 * | 21 | |||
| Ethyl acetate (µg/µL) | Micro dilution | Escherichia coli ATCC 25922 | 4.00 | - | 0.4 | - | - | - | [12] |
| Pseudomenas aeruginosa ATCC 27853 | 4.00 | - | 0.4 | - | - | - | |||
| Acetone (µg/µL) | Escherichia coli ATCC 25922 | 4.00 | - | 0.4 | - | - | - | [12] | |
| Pseudomenas aeruginosa ATCC 25922 | 4.00 | - | 0.4 | - | - | - | |||
| Ethanol (µg/mL) | Disc dilution & Broth microdilution | Escherichia coli ESβL(+) (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 20 | [29] |
| Klebsiella pneumoniae ESβL(+) (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 20 | |||
| Klebsiella pneumoniae CRE(+) 1 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 21 | |||
| Klebsiella pneumoniae CRE(+) 2 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 24 | |||
| Klebsiella pneumoniae CRE(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 23 | |||
| Klebsiella pneumoniae CRE(+) 4 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 23 | |||
| Serratia marcescens CRE(+) (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 20 | |||
| Pseudomonas aeruginosa MβL(+) 1 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 17 | |||
| Pseudomonas aeruginosa MβL(+) 2 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 19 | |||
| Pseudomonas aeruginosa MβL(+) 3 (CI) | 156 | 156 | 0.0156 | 0.0156 | 1* | 28 | |||
| Acinetobacter baumannii MβL(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 2 * | 23 | |||
| Acinetobacter baumannii MβL(+) 2 (CI) | 156 | 312 | 0.0156 | 0.0312 | 2 * | 24 | |||
| Acinetobacter baumannii MβL(+) 3 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 24 | |||
| Acinetobacter baumannii MβL(+) 4 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 23 | |||
| Acinetobacter baumannii MβL(+) 5 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 26 | |||
| Methanol (µg/mL) | Disc dilution & Broth microdilution | Escherichia coli ESBL(+) (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 19 | [29] |
| Klebsiella pneumoniae ESβL(+) (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 19 | |||
| Klebsiella pneumoniae CRE(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 21 | |||
| Klebsiella pneumoniae CRE(+) 2 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 23 | |||
| Klebsiella pneumoniae CRE(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 22 | |||
| Klebsiella pneumoniae CRE(+) 4 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 22 | |||
| Serratia marcescens CRE(+) (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 19 | |||
| Pseudomonas aeruginosa MβL(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 15 | |||
| Pseudomonas aeruginosa MβL(+) 2 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 18 | |||
| Pseudomonas aeruginosa MβL(+) 3 (CI) | 156 | 156 | 0.0156 | 0.0156 | 1 * | 27 | |||
| Acinetobacter baumannii MβL(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 22 | |||
| Acinetobacter baumannii MβL(+) 2 (CI) | 625 | 1250 | 0.0625 | 0.125 | 2 * | 24 | |||
| Acinetobacter baumannii MβL(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 23 | |||
| Acinetobacter baumannii MβL(+) 4 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 22 | |||
| Acinetobacter baumannii MβL(+) 5 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 25 | |||
| SC-CO2 15MPa (µg/mL) | Disc dilution & Broth microdilution | Escherichia coli ESβL(+) (CI) | 625 | 1250 | 0.0625 | 0.125 | 2 * | 15 | [29] |
| Klebsiella pneumoniae ESβL(+) (CI) | 1250 | 1250 | 0.125 | 0.125 | 1 * | 15 | |||
| Klebsiella pneumoniae CRE(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 15 | |||
| Klebsiella pneumoniae CRE(+) 2 (CI) | 625 | 1250 | 0.0625 | 0.125 | 2 * | 20 | |||
| Klebsiella pneumoniae CRE(+) 3 (CI) | 625 | 1250 | 0.0625 | 0.125 | 2 * | 16 | |||
| Klebsiella pneumoniae CRE(+) 4 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 16 | |||
| Serratia marcescens CRE(+) (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 18 | |||
| Pseudomonas aeruginosa MβL(+) 1 (CI) | 1250 | 1250 | 0.125 | 0.125 | 1 * | 11 | |||
| Pseudomonas aeruginosa MβL(+) 2 (CI) | 1250 | 1250 | 0.125 | 0.125 | 1 * | 14 | |||
| Pseudomonas aeruginosa MβL(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 12 | |||
| Acinetobacter baumannii MβL(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 20 | |||
| Acinetobacter baumannii MβL(+) 2 (CI) | 625 | 1250 | 0.0625 | 0.125 | 2 * | 20 | |||
| Acinetobacter baumannii MβL(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 19 | |||
| Acinetobacter baumannii MβL(+) 4 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 18 | |||
| Acinetobacter baumannii MβL(+) 5 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 21 | |||
| SC-CO2 20MPa (µg/mL) | Disc dilution & Broth microdilution | Escherichia coli ESβL(+) (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 16 | [29] |
| Klebsiella pneumoniae ESβL(+) (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 16 | |||
| Klebsiella pneumoniae CRE(+) 1 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 16 | |||
| Klebsiella pneumoniae CRE(+) 2 (CI) | 312 | 625 | 0.0312 | 0.0625 | 2 * | 20 | |||
| Klebsiella pneumoniae CRE(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 2 * | 17 | |||
| Klebsiella pneumoniae CRE(+) 4 (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 17 | |||
| Serratia marcescens CRE(+) (CI) | 312 | 312 | 0.0312 | 0.0312 | 1 * | 18 | |||
| Pseudomonas aeruginosa MβL(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 11 | |||
| Pseudomonas aeruginosa MβL(+) 2 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 15 | |||
| Pseudomonas aeruginosa MβL(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 14 | |||
| Acinetobacter baumannii MβL(+) 1 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 22 | |||
| Acinetobacter baumannii MβL(+) 2 (CI) | 312 | 625 | 0.312 | 0.0625 | 2 * | 22 | |||
| Acinetobacter baumannii MβL(+) 3 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 22 | |||
| Acinetobacter baumannii MβL(+) 4 (CI) | 312 | 312 | 0.312 | 0.312 | 1 * | 21 | |||
| Acinetobacter baumannii MβL(+) 5 (CI) | 625 | 625 | 0.0625 | 0.0625 | 1 * | 24 | |||
| Ethanol (mg/mL) | Agar well diffusion & Broth microdilution | Aggregatibacter actino-mycetemcomitans ATCC 33384 | 1.04 | 2.08 | 0.104 | 0.208 | 2 * | ≥20 | [17] |
| Fusobacterium nucleatum ATCC 25586 | 1.30 | 2.08 | 0.13 | 0.208 | 1.6 * | ≥20 | |||
| Ethyl acetate | Broth dilution | Vibrio harveyi | 1600 | - | 0.16 | - | - | - | [32] |
| Extract-Ag nanoparticles | Kirby-Bauer’s Disc diffusion | Pseudomenas aeruginosa ATCC 27853 | - | - | - | - | - | 21.95 ± 0.45 | [25] |
| Salmonella typhi ATCC 14028 | - | - | - | - | - | 29.55 ± 0.45 | |||
| Escherichia coli ATCC 25922 | - | - | - | - | - | 27.12 ± 0.38 | |||
| Extract-CaO nanoparticles | Agar well diffusion | Escherichia coli ATCC 25922 | - | - | - | - | - | 18 | [28] |
| Pseudomonas aeruginosa ATCC 27853 | - | - | - | - | - | 13 | |||
| BLEO-nanoemulsion (µL/mL) | Microdilution plate | Escherichia coli MTCC 443 | 0.5–1 | 1–1.5 | 0.05–0.1 | 0.1–0.15 | 1–3 * | - | [26] |
| Klebsiella pneumoniae MTCC 432 | 1–1.25 | 2–2.5 | 0.1–0.125 | 0.2–0.25 | 1–2 * | - | |||
| Pseudomonas aeruginosa MTCC 424 | 0.5–0.75 | 1–1.5 µL/mL | 0.05–0.075 | 0.1–0.15 | 2 * | - | |||
| BLEO (mg/mL) | Micro-dilution broth & growth inhibitory assay | Acinetobacter baumannii (CI) | 8 | 8 | 0.8 | 0.8 | 1 * | - | [24] |
| Escherichia coli ATCC 25922 | 0.3 | 0.3 | 0.03 | 0.03 | 1 * | - | |||
| Escherichia coli (CI) | 2 | 2 | 0.2 | 0.2 | 1 * | - | |||
| Klebsiella pneumoniae (CI) | 4 | 4 | 0.4 | 0.4 | 1 * | - | |||
| Pseudomonas aeruginosa ATCC 27853 | 0.5 | 0.5 | 0.05 | 0.05 | 1 * | - | |||
| Pseudomonas aeruginosa (CI) | 2 | 2 | 0.2 | 0.2 | 1 * | - | |||
| Proteus vulgaris (CI) | 4 | 4 | 0.4 | 0.4 | 1 * | - | |||
| BLEO + Gentamicin (mg/mL) | Micro-dilution broth & growth inhibitory assay | Escherichia coli ATCC 25922 | 0.5-1 | - | 0.05–0.1 | - | - | - | [24] |
| Extract/Preparation/Isolate (Unit for Activities) | Method | BACTERIA SPECIES | Activitites | Recalculated (%) | MBC/MIC | Inhibition Zone (mm) | Reference | ||
|---|---|---|---|---|---|---|---|---|---|
| MIC | MBC | MIC | MBC | ||||||
| Ethanol | Agar well diffusion | Bacillus subtilis | - | - | - | - | - | 13.2–15.8 | [11] |
| Staphylococcus aureus | - | - | - | - | - | 9.7–18.0 | |||
| Micrococcus luteus | - | - | - | - | - | 5.0–5.4 | |||
| Water | Agar well diffusion | Bacillus subtilis | - | - | - | - | - | 4.9–6.8 | [11] |
| Staphylococcus aureus | - | - | - | - | - | 5.4–12.3 | |||
| Micrococcus luteus | - | - | - | - | – | 3.5–4.2 | |||
| Ethanol (µg/mL) | Disk diffusion | Staphylococcus aureus ATCC 29223 | 312 | 312 | 0.0312 | 0.0312 | 1 * | 30 | [27] |
| MRSA #1 (CI) | 156 | 312 | 0.0156 | 0.0312 | 2 * | 32 | |||
| MRSA #2 (CI) | 156 | 156 | 0.0156 | 0.0156 | 1 * | 34 | |||
| MRSA #3 (CI) | 156 | 156 | 0.0156 | 0.0156 | 1 * | 28 | |||
| MRSA #4 (CI) | 78 | 78 | 0.0078 | 0.0078 | 1 * | 34 | |||
| VRE | 19 | 19 | 0.0019 | 0.0019 | 1 * | 28 | |||
| Ethyl acetate (µg/µL) | Broth microdilution | Staphylococcus aureus ATCC 25923 | 0.50 | - | 0.0005 | - | - | - | [12] |
| Propionibacterium acnes ATCC 6919 | 2.00 | - | 0.002 | - | - | - | |||
| Staphylococcus epidermidis ATCC 12228 | 4.00 | - | 0.004 | - | - | - | |||
| Streptococcus pyogenes ATCC 19615 | 4.00 | - | 0.004 | - | - | - | |||
| Acetone (µg/µL) | Broth microdilution | Staphylococcus aureus ATCC 25923 | 0.25 | - | 0.00025 | - | - | - | [12] |
| Propionibacterium acnes ATCC 6919 | 2.00 | - | 0.002 | - | - | - | |||
| Staphylococcus epidermidis ATCC 12228 | 4.00 | - | 0.004 | - | - | - | |||
| Streptococcus pyogenes ATCC 19615 | 4.00 | - | 0.004 | - | - | - | |||
| Dichloromethane (µg/µL) | Broth microdilution | Staphylococcus aureus ATCC 25923 | 1.00 | - | 0.001 | - | - | - | [12] |
| Propionibacterium acnes ATCC 6919 | 4.00 | - | 0.004 | - | - | - | |||
| Staphylococcus epidermidis ATCC 12228 | 4.00 | - | 0.004 | - | - | - | |||
| Streptococcus pyogenes ATCC 19615 | 4.00 | - | 0.004 | - | - | - | |||
| Ethanol (µg/mL) | Disk diffusion | MRSA 1–7 | 78–156 | 78–312 | 0.0078–0.0156 | 0.0078–0.0312 | 1–2 * | 28–3833 | [29] |
| VRE 1–3 | 19–156 | 19–156 | 0.0019–0.0156 | 0.0019–0.0156 | 1 * | 25–3228 | |||
| Methanol (µg/mL) | Disk diffusion | MRSA 1–7 | 78–312 | 78–312 | 0.0078–0.0312 | 0.0078–0.0312 | 1–2 * | 28–3432 | [29] |
| VRE 1–3 | 19–156 µg/mL19µg/mL | 19–156 µg/mL19µg/mL | 0.0019–0.0156 | 0.0019–0.0156 | 1 * | 25–3226 | |||
| SC-CO2 15MPa (µg/mL) | Disk diffusion | MRSA 1–7 | 312–625 | 312–1250 | 0.0312–0.0625 | 0.0312–0.125 | 1 * | 21–3025 | [29] |
| VRE 1–3 | 19–156 | 19–156 | 0.0019–0.0156 | 0.0019–0.0156 | 1 * | 15–2820 | |||
| SC-CO2 20MPa (µg/mL) | Disk diffusion | MRSA 1–7 | 156–625 | 156–625 | 0.0156–0.0625 | 0.0156–0.0625 | 1 * | 22–3325 | [29] |
| VRE 1–3 | 19–156 | 19–156 | 0.0019–0.0156 | 0.0019–0.0156 | 1 * | 15–3124 | |||
| Ethanol (mg/mL) | Agar well diffusion & Broth microdilution | Enterobacter faecalis ATCC 19433 | 5.21 | 8.33 | 0.521 | 0.833 | 1.6 * | 10–20 | [17] |
| Lactobacillus fermentum ATCC 14931 | 4.17 | 8.33 | 0.417 | 0.833 | 2 * | 10–20 | |||
| Lactobacillus salivarius ATCC 11741 | 4.17 | 8.33 | 0.417 | 0.833 | 2 * | 10–20 | |||
| Streptococcus sobrinus ATCC 33478 | 1.56 | 3.17 | 0.156 | 0.317 | 2 * | ≥20 | |||
| Streptococcus mutans ATCC 25175 | 1.56 | 3.17 | 0.156 | 0.317 | 2 * | ≥20 | |||
| Hexane (µg/mL) | Disk diffusion | Streptococcus gordonii DMST 38731 | 1.00 | 2.00 | 0.0001 | 0.0002 | 2 * | 8.00 ± 0.00 | [30] |
| Streptococcus mutans DMST 18777 | 2.00 | 2.00 | 0.0002 | 0.0002 | 1 * | - | |||
| Ethyl acetate (µg/mL) | Streptococcus gordonii DMST 38731 | 0.50 | 2.00 | 0.00005 | 0.0002 | 4 ** | 12.50 ± 0.70 | [30] | |
| Streptococcus mutans DMST 18777 | 1.00 | 2.00 | 0.0001 | 0.0002 | 2 * | 11.00 ± 0.00 | |||
| Ethanol | Agar well diffusion | Staphylococcus aureus (CI) | - | - | - | - | - | 2..500–20.375 | [37] |
| Extract-Ag nanoparticles | Kirby-Bauer’s Disc diffusion | Staphylococcus aureus ATCC 25923 | - | - | - | - | - | 32.78 ± 0.64 | [25] |
| Extract-CaO nanoparticles | Agar well diffusion | Staphylococcus aureus ATCC 25923 | - | - | - | - | - | 13 | [28] |
| Streptococcus mutans MTCC 890 | - | - | - | - | - | 12 | |||
| BLEO-nanoemulsion (µL/mL) | Microdilution plate | Staphylococcus aureus MTCC 1144 | 0.5–0.75 | 1–1.5 | 0.05–0.075 | 0.1–0.15 | 2 * | [26] | |
| Bacillus cereus MTCC 1272 | 0.5–0.75 | 0.75–1.5 | 0.05–0.075 | 0.1–0.15 | 2 * | - | |||
| BLEO (mg/mL) | Micro-dilution broth & growth inhibitory assay | Escherichia faecalis (CI) | 4 | 4 | 0.4 | 0.4 | 1 * | [24] | |
| Propionibacterium acnes ATCC 6919 | 1 | 1 | 0.1 | 0.1 | 1 * | - | |||
| Staphylococcus aureus ATCC 25923 | 0.5 | 0.5 | 0.05 | 0.05 | 1 * | - | |||
| Staphylococcus epidermidis ATCC 12228 | 0.5 | 0.5 | 0.05 | 0.05 | 1 * | - | |||
| Streptococcus peroris (CI) | 2 | 2 | 0.2 | 0.2 | 1 * | - | |||
| MRSA (CI) | 8 | 8 | 0.8 | 0.8 | 1 * | - | |||
| BLEO+Gentamicin (mg/mL) | Micro-dilution broth & growth inhibitory assay | Staphylococcus epidermidis ATCC 12228 | 1-2 | - | 0.1–0.2 | - | - | [24] | |
| Allylpyrocatechols I (µg/mL) | Kirby–Bauer disk diffusion | Streptococcus sanguinis ATCC 10566 | 39.1 | 78.1 | 0.00391 | 0.00781 | 2 * | 11.85–25.15 | [15] |
| 4-allylpyrocatechol (µg/mL) | Broth microdilution | Streptococcus intermedius DMST 42700 | 200 | 500 | 0.02 | 0.05 | 2.5 * | - | [35] |
| Streptococcus mutans DMST 41283 | 200 | 500 | 0.02 | 0.05 | 2.5 * | - | |||
| Extract/Preparation/Isolate (Unit for Activities) | Method | Fungal Species | Activities | Recalculated (%) | MFC/MIC | Inhibition Zone (mm) | Reference | ||
|---|---|---|---|---|---|---|---|---|---|
| MIC | MFC | MIC | MFC | ||||||
| Young leaves | [39] | ||||||||
| Ethanol (μg/mL) | Broth microdilution | Candida albicans (CI) | 500 | - | 0.05 | - | - | 8–15 | |
| Ethyl acetate (μg/mL) | Broth microdilution | Candida albicans (CI) | 250 | - | 0.025 | - | - | 10–22 | |
| Mature leaves | [39] | ||||||||
| Ethanol (μg/mL) | Broth microdilution | Candida albicans (CI) | 750 | - | 0.075 | - | - | 5–22 | |
| Ethyl acetate (μg/mL) | Broth microdilution | Candida albicans (CI) | 125 | - | 0.0125 | - | - | 17–26 | |
| Ethyl acetate | Well-diffusion | Aspergillus niger | - | - | - | - | - | 28 | [10] |
| Aspergillus sp. | - | - | - | - | - | 5 | |||
| Hexane | Well-diffusion | Aspergillus niger | - | - | - | - | - | 28 | [10] |
| Aspergillus sp. | - | - | - | - | - | 8 | |||
| Hexane (mg/mL) | Disk diffusion | Candida albicans DMST 8684 | 1.00 | 2.00 | 0.1 | 0.2 | 2 * | 21.00 ± 1.40 | [30] |
| Candida albicans DMST 5815 | 1.00 | 4.00 | 0.1 | 0.4 | 4 ** | 20.67 ± 0.58 | |||
| Ethyl acetate (mg/mL) | Disk diffusion | Candida albicans DMST 8684 | 0.50 | 2.00 | 0.05 | 0.2 | 4 ** | 23.00 ± 0.00 | [30] |
| Candida albicans DMST 5815 | 1.00 | 2.00 | 0.1 | 0.2 | 2 * | 24.33 ± 0.58 | |||
| BLEO (μL/mL) | Solid dilution | Alternaria alternate | 0.53 | - | 0.053 | - | - | - | [18] |
| Aspergillus candidus | 0.57 | - | 0.057 | - | - | - | |||
| Aspergillus flavus | 0.7 | - | 0.07 | - | - | - | |||
| Aspergillus fumigatus | 0.40 | - | 0.04 | - | - | - | |||
| Aspergillus niger | 0.73 | - | 0.073 | - | - | - | |||
| Aspergillus sydowi | 0.63 | - | 0.063 | - | - | - | |||
| Aspergillus terreus | 0.60 | - | 0.060 | - | - | - | |||
| Cladosporium cladosporoides | 0.67 | - | 0.067 | - | - | - | |||
| Culcularia lunata | 0.50 | - | 0.05 | - | - | - | |||
| Fusarium oxysporum | 0.50 | - | 0.05 | - | - | - | |||
| Mucor sp. | 0.37 | - | 0.037 | - | - | - | |||
| Mycelia sterilia | 0.30 | - | 0.03 | - | - | - | |||
| Nugrospora sp. | 0.53 | - | 0.053 | - | - | - | |||
| Penicillium italicum | 0.40 | - | 0.04 | - | - | - | |||
| BLEO (mg/mL) | Microdilution broth & growth inhibitory assay | Aspergillus niger ATCC 16404 | 2 | 2 | 0.2 | 0.2 | 1 * | - | [24] |
| Candida albicans ATCC 10231 | 1.5 | 1.5 | 0.15 | 0.15 | 1 * | - | |||
| Candida albicans (CI) | 2 | 2 | 0.2 | 0.2 | 1 * | - | |||
| Candida tropicalis ATCC 750 | 2 | 2 | 0.2 | 0.2 | 1 * | - | |||
| BLEO (μL/mL) | Broth microdilution | Trichophyton mentagrophytes (CI) | 0.2–0.4 | 0.4 | 0.00002–0.00004 | 0.00004 | 1–2 * | - | [40] |
| Trichophyton mentagrophytes DMST 19735 | 0.2–0.4 | 0.4 | 0.00002–0.00004 | 0.00004 | 1–2 * | - | |||
| Microsporum canis (CI) | 0.2–0.4 | 0.4 | 0.00002–0.00004 | 0.00004 | 1–2 * | - | |||
| Microsporum canis DMST 29297 | 0.2 | 0.4 | 0.00002–0.00004 | 0.00004 | 2 * | - | |||
| Microsporum gypseum (CI) | 0.4–0.8 | 0.8 | 0.00004–0.00008 | 0.00008 | 1–2 * | - | |||
| Microsporum gypseum DMST 21146 | 0.8 | 0.8 | 0.00008 | 0.00008 | 1 * | - | |||
| BLEO (%v/v) | Disk diffusion | Candida albicans ATCC 10231 | 0.078 | - | 0.078 | - | - | 33.83 + 0.76 | [2] |
| Candida glabrata ATCC 90030 | 0.039 | - | 0.039 | - | - | 33.83 + 0.76 | |||
| Candida krusei ATCC 6258 | 0.078 | - | 0.078 | - | - | 32.66 + 0.57 | |||
| Candida parapsilosis ATCC 22019 | 0.039 | - | 0.039 | - | - | 33.83 + 0.76 | |||
| Candida pseudotropicalis (CI) | 0.039 | - | 0.039 | - | - | 33.50+0.50 | |||
| Candida stellatoidia (CI) | 0.039 | - | 0.039 | - | - | 35.50+0.86 | |||
| Candida tropicalis (CI) | 0.078 | - | 0.078 | - | - | 30.83+0.28 | |||
| BLEO-microemulsion (μL/mL) | Broth dilution | Aspergillus flavus | - | 15 | - | 1.5 | - | - | [41] |
| Penicillium expansum | - | 15 | - | 1.5 | - | - | |||
| Hydroxychavicol (μg/mL) | Broth microdilution | Aspergillus flavus MTCC 1973, 2799 | 250 | 250 | 0.025 | 0.025 | 1 * | - | [38] |
| Aspergillus flavus (CI) | 125-500 | 125–500 | 0.0125–0.05 | 0.0125–0.05 | 1 * | ||||
| Aspergillus fumigatus MTCC 1811 | 250 | 250 | 0.025 | 0.025 | 1 * | - | |||
| Aspergillus niger ATCC 16404 | 125 | 125 | 0.0125 | 0.0125 | 1 * | - | |||
| Aspergillus niger (CI) | 125-250 | 125-250 | 0.0125–0.05 | 0.0125–0.05 | 1 * | ||||
| Aspergillus parasiticus MTCC 2796 | 250 | 250 | 0.025 | 0.025 | 1 * | - | |||
| Candida albicans ATCC 90028, 10231 | 250 | 250 | 0.025 | 0.025 | 1 * | - | |||
| Candida albicans (CI) | 125–500 | 250–500 | 0.0125–0.05 | 0.0125–0.05 | 1–2 * | ||||
| Candida glabrata ATCC 90030 | 31.25 | 31.25 | 0.003125 | 0.003125 | 1 * | - | |||
| Candida glabrata (CI) | 15.62–31.25 | 15.62–62.5 | 0.001562–0.003125 | 0.001562–0.00625 | 1–2 * | ||||
| Candida krusei ATCC 22019 | 15.62 | 62.5 | 0.001562 | 0.00625 | 4 ** | - | |||
| Candida krusei (CI) | 15.62–31.25 | 15.62–31.25 | 0.001562–0.003125 | 0.001562–0.003125 | 1 * | - | |||
| Candida neoformans ATCC 204092 | 62.5 | 62.5 | 0.00625 | 0.00625 | 1 * | - | |||
| Candida neoformans (CI) | 62.5 | 62.5 | 0.00625 | 0.00625 | 1 * | - | |||
| Candida parapsilosis ATCC 22019 | 31.25 | 31.25 | 0.003125 | 0.003125 | 1 * | - | |||
| Candida parapsilosis (CI) | 31,25–62.5 | 31,25–62.5 | 0.003125–0.00625 | 0.003125–0.00625 | 1 * | - | |||
| Candida tropicallis ATCC 750 | 250 | 250 | 0.025 | 0.025 | 1 * | - | |||
| Candida tropicallis (CI) | 125–500 | 250–500 | 0.0125–0.05 | 0.025–0.05 | 1–2 * | - | |||
| Epidermophyton floccosum MTCC 613 | 15.62 | 15.62 | 0.001562 | 0.001562 | 1 * | - | |||
| Epidermophyton floccosum (CI) | 15.62 | 31.25 | 0.001562 | 0.003125 | 2 * | ||||
| Microsporum canis MTCC 2820 | 15.62 | 31.25 | 0.001562 | 0.003125 | 2 * | - | |||
| Microsporum canis (CI) | 15.62 | 31.25 | 0.001562 | 0.003125 | 2 * | - | |||
| Micosporum gypsium MTCC 2819 | 15.62 | 31.25 | 0.001562 | 0.003125 | 2 * | - | |||
| Micosporum gypsium (CI) | 7.81–15.62 | 15.62–31.25 | 0.000781–0.001562 | 0.001562–0.003125 | 2 * | - | |||
| Trichophyton mentagrophytes ATCC 9533 | 15.62 | 15.62 | 0.001562 | 0.001562 | 1 * | - | |||
| Trichophyton mentagrophytes (CI) | 15.62–31.25 | 15.62–62.5 | 0.001562–0.003125 | 0.001562–0.00625 | 1–2 * | - | |||
| Trichophyton rubrum MTCC 296 | 31.25 | 31.25 | 0.003125 | 0.003125 | 1 * | - | |||
| Trichophyton rubrum (CI) | 15.62–62.5 | 31.25–62.5 | 0.001562–0.00625 | 0.003125–0.00625 | 1–2 * | - | |||
| 4-allylpyrocatechol (μg/mL) | Broth Microdilution | Candida albicans DMST 8684 | 400 | 500 | 0.04 | 0.05 | 1.25 * | - | [35] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nayaka, N.M.D.M.W.; Sasadara, M.M.V.; Sanjaya, D.A.; Yuda, P.E.S.K.; Dewi, N.L.K.A.A.; Cahyaningsih, E.; Hartati, R. Piper betle (L): Recent Review of Antibacterial and Antifungal Properties, Safety Profiles, and Commercial Applications. Molecules 2021, 26, 2321. https://doi.org/10.3390/molecules26082321
Nayaka NMDMW, Sasadara MMV, Sanjaya DA, Yuda PESK, Dewi NLKAA, Cahyaningsih E, Hartati R. Piper betle (L): Recent Review of Antibacterial and Antifungal Properties, Safety Profiles, and Commercial Applications. Molecules. 2021; 26(8):2321. https://doi.org/10.3390/molecules26082321
Chicago/Turabian StyleNayaka, Ni Made Dwi Mara Widyani, Maria Malida Vernandes Sasadara, Dwi Arymbhi Sanjaya, Putu Era Sandhi Kusuma Yuda, Ni Luh Kade Arman Anita Dewi, Erna Cahyaningsih, and Rika Hartati. 2021. "Piper betle (L): Recent Review of Antibacterial and Antifungal Properties, Safety Profiles, and Commercial Applications" Molecules 26, no. 8: 2321. https://doi.org/10.3390/molecules26082321








