Pandemic-Driven Development of a Medical-Grade, Economic and Decentralized Applicable Polyolefin Filament for Additive Fused Filament Fabrication
Abstract
:1. Introduction
2. Additive Manufacturing (AM)
3. Materials for AM
4. Optimization of Polyolefins for Extrusion-Based AM
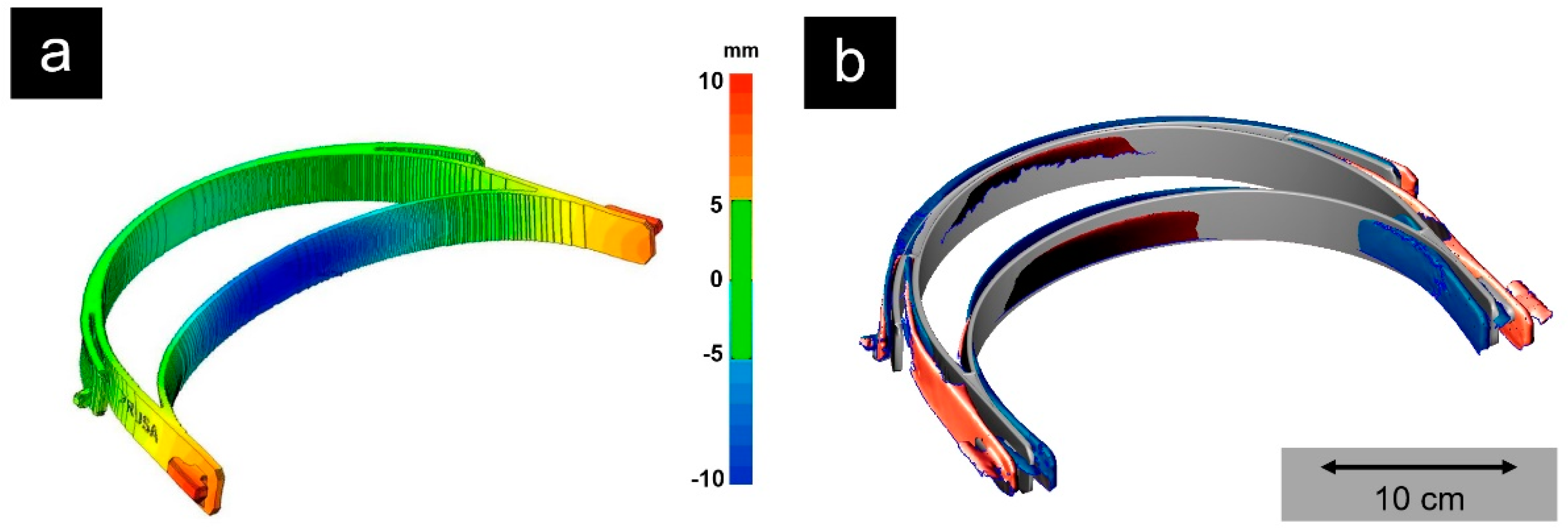
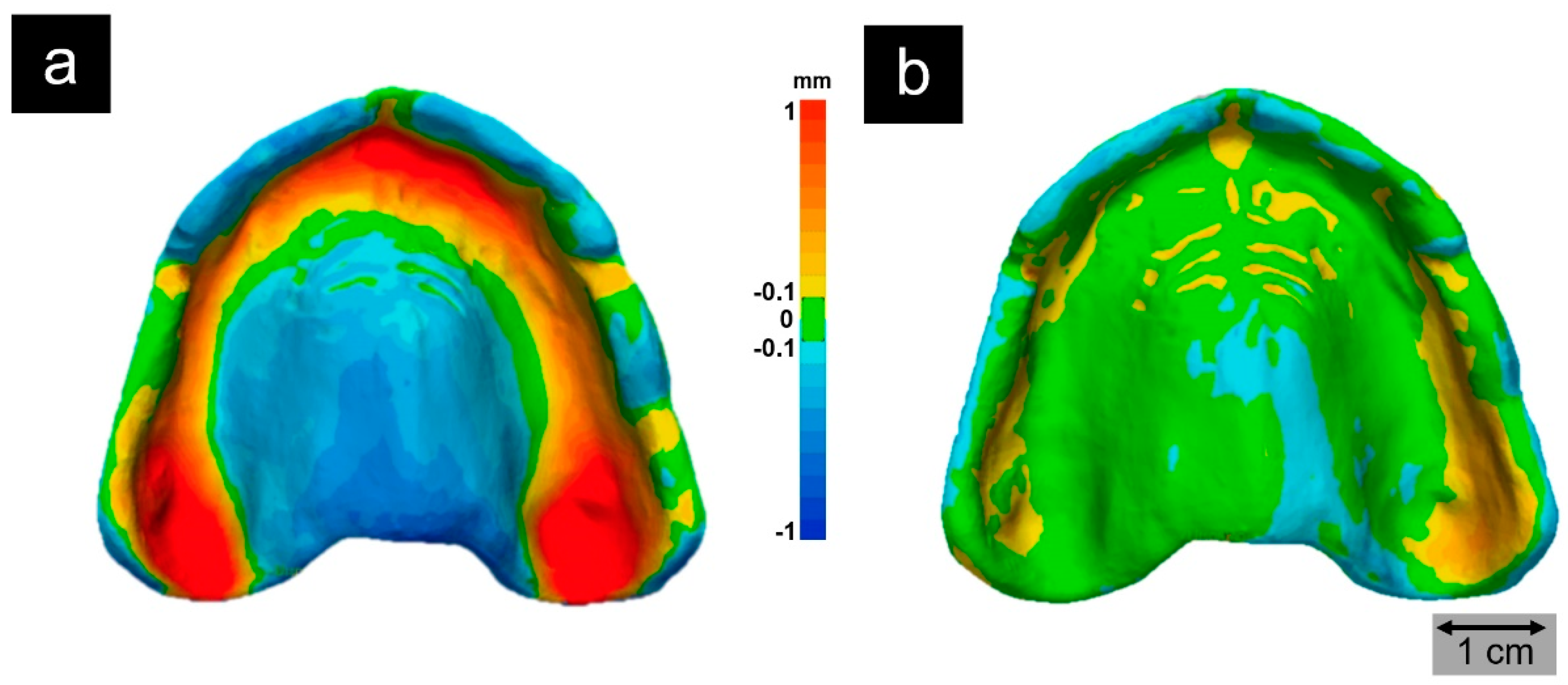
5. Extrusion and Application of a Medical-Grade Polyolefin Filament
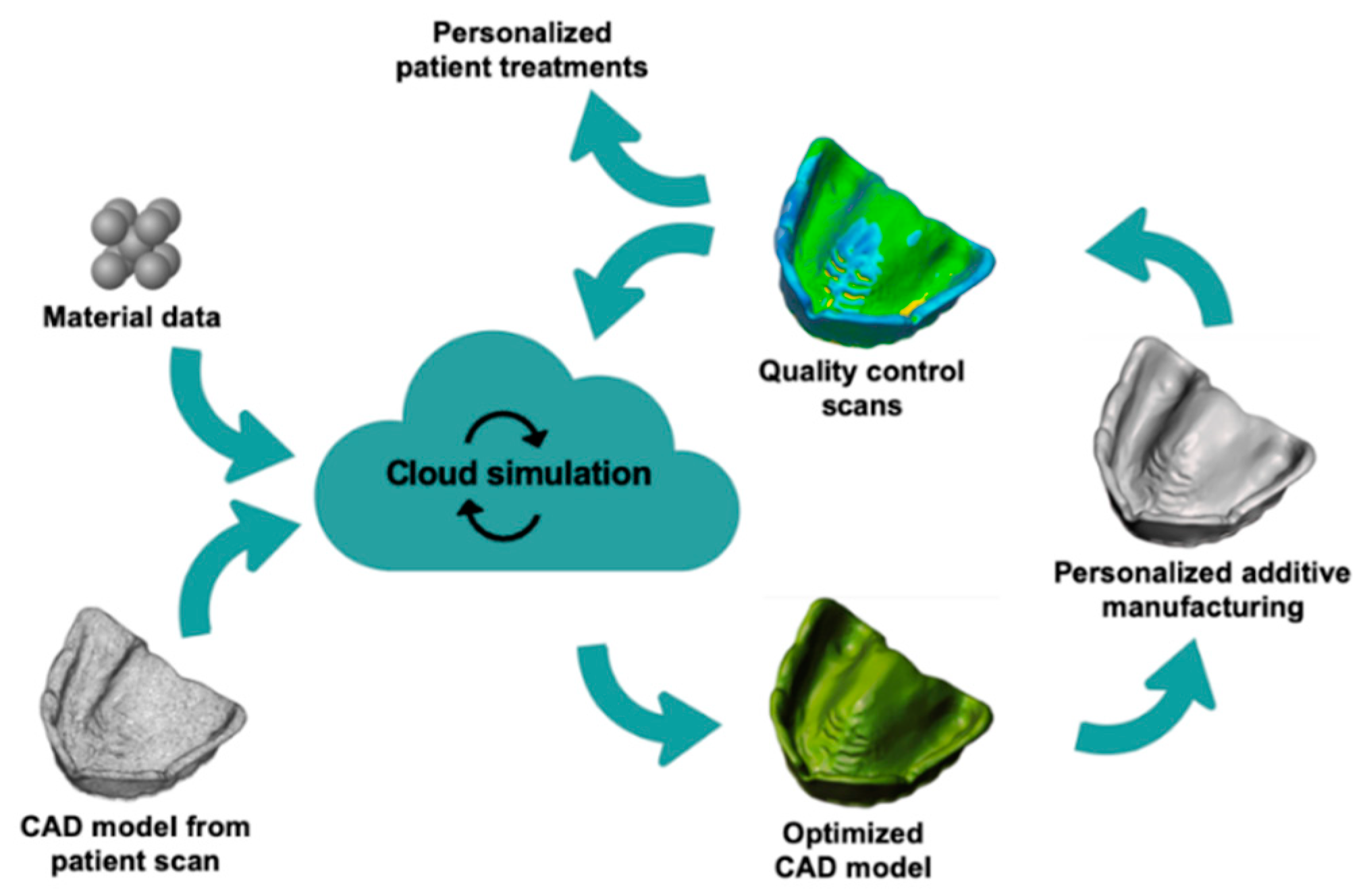
6. Validation of the Process Chain
7. Future Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sharma, A.; Tiwari, S.; Deb, M.K.; Marty, J.L. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): A global pandemic and treatment strategies. Int. J. Antimicrob. Agents 2020, 56, 106054. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.L.; Turnham, P.; Griffin, J.R.; Clarke, C.C. Consideration of the aerosol transmission for COVID-19 and public health. Risk Anal. 2020, 40, 902–907. [Google Scholar] [CrossRef] [PubMed]
- Mick, P.; Murphy, R. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: A literature review. Otolaryngol. Head Neck Surg. 2020, 49, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ge, Z.; Yang, L.; Xia, J.; Fu, X.; Zhang, Y. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J. Zhejiang Univ. Sci. B 2020, 21, 361–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; Chu, D.K.; Akl, E.A.; El-harakeh, A.; Bognanni, A.; et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Carneiro, O.S.; Silva, A.F.; Gomes, R. Fused deposition modeling with polypropylene. Mater. Des. 2015, 83, 768–776. [Google Scholar] [CrossRef]
- Schirmeister, C.G.; Hees, T.; Licht, E.H.; Mülhaupt, R. 3D printing of high density polyethylene by fused filament fabrication. Addit. Manuf. 2019, 28, 152–159. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D printing and customized additive manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [Green Version]
- Aimar, A.; Palermo, A.; Innocenti, B. The role of 3D printing in medical applications: A state of the art. J. Healthc. Eng. 2019, 2019, 5340616. [Google Scholar] [CrossRef] [Green Version]
- Crump, S.S. Apparatus and Method for Creating Three-Dimensional Objects. US5121329A, 9 June 1992. [Google Scholar]
- Genina, N.; Holländer, J.; Jukarainen, H.; Mäkilä, E.; Salonen, J.; Sandler, N. Ethylene vinyl acetate (EVA) as a new drug carrier for 3D printed medical drug delivery devices. Eur. J. Pharm. Sci. 2016, 90, 53–63. [Google Scholar] [CrossRef]
- Tan, D.; Maniruzzaman, M.; Nokhodchi, A. Advanced pharmaceutical applications of hot-melt extrusion coupled with fused deposition modelling (FDM) 3D printing for personalised drug delivery. Pharmaceutics 2018, 10, 203. [Google Scholar] [CrossRef] [Green Version]
- Jeong, H.M.; Weon, K.-Y.; Shin, B.S.; Shin, S. 3D-Printed gastroretentive sustained release drug delivery system by applying design of experiment approach. Molecules 2020, 25, 2330. [Google Scholar] [CrossRef] [PubMed]
- Kempin, W.; Franz, C.; Koster, L.-C.; Schneider, F.; Bogdahn, M.; Weitschies, W.; Seidlitz, A. Assessment of different polymers and drug loads for fused deposition modeling of drug loaded implants. Eur. J. Pharm. Biopharm. 2017, 115, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, V.S.; Malkar, T.K.; Murty, U.S.; Banerjee, S. Extruded filaments derived 3D printed medicated skin patch to mitigate destructive pulmonary tuberculosis: Design to delivery. Expert Opin. Drug Deliv. 2020. [Google Scholar] [CrossRef] [PubMed]
- Pieralli, S.; Spies, B.C.; Hromadnik, V.; Nicic, R.; Beuer, F.; Wesemann, C. How accurate is oral implant installation using surgical guides printed from a degradable and steam-sterilized biopolymer? J. Clin. Med. 2020, 9, 2322. [Google Scholar] [CrossRef] [PubMed]
- Wesemann, C.; Pieralli, S.; Fretwurst, T.; Nold, J.; Nelson, K.; Schmelzeisen, R.; Hellwig, E.; Spies, B.C. 3-D printed protective equipment during COVID-19 pandemic. Materials 2020, 13, 1997. [Google Scholar] [CrossRef]
- Cortes, A.R.G.; Galea, K.; No-Cortes, J.; Sammut, E.J.; Alzoubi, E.E.; Attard, N.J. Use of free CAD software for 3D printing individualized face masks based on face scans. Int. J. Comput. Dent. 2020, 23, 183–189. [Google Scholar]
- Mohan, N.; Senthil, P.; Vinodh, S.; Jayanth, N. A review on composite materials and process parameters optimisation for the fused deposition modelling process. Virtual Phys. Prototyp. 2017, 12, 47–59. [Google Scholar] [CrossRef]
- Goh, G.D.; Yap, Y.L.; Tan, H.K.J.; Sing, S.L.; Goh, G.L.; Yeong, W.Y. Process-Structure-Properties in Polymer Additive Manufacturing via Material Extrusion: A Review. Crit. Rev. Solid State Mater. Sci. 2020, 45, 113–133. [Google Scholar] [CrossRef]
- Singh Boparai, K.; Singh, R.; Singh, H. Wear behavior of FDM parts fabricated by composite material feed stock filament. Rapid Prototyp. J. 2016, 22, 350–357. [Google Scholar] [CrossRef]
- Solvay. Available online: https://www.solvay.com/en/chemical-categories/specialty-polymers/additive-manufacturing (accessed on 28 October 2020).
- Vestakeep PEEK. Available online: https://medical.evonik.com/product/peek-industrial/downloads/vestakeep-polymers-for-medical-applications-en.pdf (accessed on 28 October 2020).
- Fibre Tuff II. Available online: https://img1.wsimg.com/blobby/go/4fc374e5-752e-4d9c-9806-458efb923e97/downloads/FibreTuff%20II%20Data%20Sheet.pdf?ver=1603046414315 (accessed on 25 October 2020).
- Stürzel, M.; Mihan, S.; Mülhaupt, R. From multisite polymerization catalysis to sustainable materials and all-polyolefin composites. Chem. Rev. 2016, 116, 1398–1433. [Google Scholar] [CrossRef] [PubMed]
- Mülhaupt, R. Green polymer chemistry and bio-based plastics: Dreams and reality. Macromol. Chem. Phys. 2013, 214, 159–174. [Google Scholar] [CrossRef]
- Musib, M.K. A review of the history and role of UHMWPE as a component in total joint replacements. Int. J. Biol. Eng. 2012, 1, 6–10. [Google Scholar] [CrossRef] [Green Version]
- Malpass, D.B. Introduction to Industrial Polyethylene: Properties, Catalysts, Processes, Scrivener; Wiley: Salem, MA, USA; Hoboken, NJ, USA, 2010; ISBN 978-0-470-62598-9. [Google Scholar]
- Malpass, D.B.; Band, E.I. Introduction to Industrial Polypropylene: Properties, Catalysts, Processes; John Wiley & Sons: Hoboken, NJ, USA, 2012; ISBN 978-1-118-06276-0. [Google Scholar]
- Ehrenstein, G.W. Polymer-Werkstoffe: Struktur—Eigenschaften—Anwendung, 3rd ed.; Hanser: Munich, Germany, 2011; ISBN 978-3-446-42283-4. [Google Scholar]
- Tabone, M.D.; Cregg, J.J.; Beckman, E.J.; Landis, A.E. Sustainability metrics: Life cycle assessment and green design in polymers. Environ. Sci. Technol. 2010, 44, 8264–8269. [Google Scholar] [CrossRef] [PubMed]
- LyonellBasell. Available online: https://www.lyondellbasell.com/en/news-events/corporate--financial-news/lyondellbasell-successfully-starts-up-new-pilot-molecular-recycling-facility/ (accessed on 20 October 2020).
- Wang, T.-M.; Xi, J.-T.; Jin, Y. A model research for prototype warp deformation in the FDM process. Int. J. Adv. Manuf. Technol. 2007, 33, 1087–1096. [Google Scholar] [CrossRef]
- Spoerk, M.; Holzer, C.; Gonzalez-Gutierrez, J. Material extrusion-based additive manufacturing of polypropylene: A review on how to improve dimensional inaccuracy and warpage. J. Appl. Polym. Sci. 2020, 137, 48545. [Google Scholar] [CrossRef]
- Spoerk, M.; Savandaiah, C.; Arbeiter, F.; Traxler, G.; Cardon, L.; Holzer, C.; Sapkota, J. Anisotropic properties of oriented short carbon fibre filled polypropylene parts fabricated by extrusion-based additive manufacturing. Compos. Part A Appl. Sci. Manuf. 2018, 113, 95–104. [Google Scholar] [CrossRef]
- Spoerk, M.; Sapkota, J.; Weingrill, G.; Fischinger, T.; Arbeiter, F.; Holzer, C. Shrinkage and warpage optimization of expanded-perlite-filled polypropylene composites in extrusion-based additive manufacturing. Macromol. Mater. Eng. 2017, 302, 1700143. [Google Scholar] [CrossRef]
- Wang, L.; Gardner, D.J. Effect of fused layer modeling (FLM) processing parameters on impact strength of cellular polypropylene. Polymer 2017, 113, 74–80. [Google Scholar] [CrossRef]
- Turner, B.N.; Gold, S.A. A review of melt extrusion additive manufacturing processes: II. Materials, dimensional accuracy, and surface roughness. Rapid Prototyp. J. 2015, 21, 250–261. [Google Scholar] [CrossRef]
- Schmutzler, C.; Zimmermann, A.; Zaeh, M.F. Compensating warpage of 3D printed parts using free-form deformation. Procedia CIRP 2016, 41, 1017–1022. [Google Scholar] [CrossRef] [Green Version]
- USP Class VI, Chapter 88. Available online: http://www.uspbpep.com/usp29/v29240/usp29nf24s0_c88.html (accessed on 18 November 2020).
- Prusa Printers. Available online: https://www.prusaprinters.org/de/prints/25857-prusa-face-shield (accessed on 24 October 2020).
- Wunderlich, B. Thermal Aanalysis TX Z; Elsevier Science: Saint Louis, MO, USA, 2014; ISBN 978-0-323-13967-0. [Google Scholar]
- ISO 9001. Quality Management Systems—Requirements. Available online: https://www.iso.org/standard/62085.html (accessed on 12 November 2020).
- ISO 13485. Medical Devices—Quality Management Systems—Requirements for Regulatory Purposes. Available online: https://www.iso.org/standard/59752.html (accessed on 12 November 2020).
- Morrison, R.J.; Kashlan, K.N.; Flanangan, C.L.; Wright, J.K.; Green, G.E.; Hollister, S.J.; Weatherwax, K.J. Regulatory considerations in the design and manufacturing of implanTable 3D-printed medical devices: Regulatory considerations of 3D-printed implants. Clin. Transl. Sci. 2015, 8, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Drossel, W.-G.; Ihlemann, J.; Landgraf, R.; Oelsch, E.; Schmidt, M. Basic research for additive manufacturing of rubber. Polymers 2020, 12, 2266. [Google Scholar] [CrossRef] [PubMed]
- Jande, Y.A.; Erdal, M.; Dag, S. Production of graded porous polyamide structures and polyamide-epoxy composites via selective laser sintering. J. Reinf. Plast. Comp. 2014, 33, 1017–1036. [Google Scholar] [CrossRef]
- ISO 10993-1. Biological Evaluation of Medical Devices. Available online: https://www.iso.org/standard/68936.html (accessed on 12 November 2020).
- Medical Device and Diagnostic Industry. Available online: https://www.mddionline.com/news/fda-grapples-future-regulation-3-d-printed-medical-devices (accessed on 6 November 2020).
- Sharma, N.; Cao, S.; Msallem, B.; Kunz, C.; Brantner, P.; Honigmann, P.; Thieringer, F.M. Effects of steam sterilization on 3D printed biocompatible resin materials for surgical guides—An accuracy assessment study. J. Clin. Med. 2020, 9, 1506. [Google Scholar] [CrossRef] [PubMed]
- American Dental Association. Infection control reccommendations for the dental office and the dental laboratory. J. Am. Dent. Assoc. 1996, 127, 672–680. [Google Scholar] [CrossRef]
- Marei, H.F.; Alshaia, A.; Alarifi, S.; Almasoud, N.; Abdelhady, A. Effect of steam heat sterilization on the accuracy of 3D printed surgical guides. Implant Dent. 2019, 28, 372–377. [Google Scholar] [CrossRef]
- Shaheen, E.; Alhelwani, A.; Van De Casteele, E.; Politis, C.; Jacobs, R. Evaluation of dimensional changes of 3D printed models after sterilization: A pilot study. Open Dent. J. 2018, 12, 72–79. [Google Scholar] [CrossRef]



| Parameters | Value |
|---|---|
| MFR (230 °C/2.16 kg) a | 14.9 ± 0.7 g (10 min)−1 |
| Tm b | 165 °C |
| VST A/50 c | 142 °C |
| Degree of crystallinity d | 33% e/35% f |
| Tensile modulus g | (1.00 ± 0.12) h/(0.83 ± 0.08) i GPa |
| Tensile strength g | (19.85 ± 0.04) h/(18.1 ± 0.2) i MPa |
| Elongation at break g | (15 ± 2) h/(8.0 ± 1.4) i % |
Sample Availability: Samples of the compounds are available from the authors. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burkhardt, F.; Schirmeister, C.G.; Wesemann, C.; Nutini, M.; Pieralli, S.; Licht, E.H.; Metzger, M.; Wenz, F.; Mülhaupt, R.; Spies, B.C. Pandemic-Driven Development of a Medical-Grade, Economic and Decentralized Applicable Polyolefin Filament for Additive Fused Filament Fabrication. Molecules 2020, 25, 5929. https://doi.org/10.3390/molecules25245929
Burkhardt F, Schirmeister CG, Wesemann C, Nutini M, Pieralli S, Licht EH, Metzger M, Wenz F, Mülhaupt R, Spies BC. Pandemic-Driven Development of a Medical-Grade, Economic and Decentralized Applicable Polyolefin Filament for Additive Fused Filament Fabrication. Molecules. 2020; 25(24):5929. https://doi.org/10.3390/molecules25245929
Chicago/Turabian StyleBurkhardt, Felix, Carl G. Schirmeister, Christian Wesemann, Massimo Nutini, Stefano Pieralli, Erik H. Licht, Marc Metzger, Frederik Wenz, Rolf Mülhaupt, and Benedikt C. Spies. 2020. "Pandemic-Driven Development of a Medical-Grade, Economic and Decentralized Applicable Polyolefin Filament for Additive Fused Filament Fabrication" Molecules 25, no. 24: 5929. https://doi.org/10.3390/molecules25245929







