Chemical Composition and Biological Activities of the Essential Oil of Skimmia laureola Leaves
Abstract
:1. Introduction
2. Results and Discussion
| Ki a | Ki b | % | Identification c | |
|---|---|---|---|---|
| (−)-Camphene | 953 | 1076 | T d | 1, 2, 3 |
| Δ3-Carene | 1008 | 1173 | T | 1, 2, 3 |
| Caryophyllene oxide | 1581 | 2008 | T | 1, 2, 3 |
| Geranyl acetate | 1379 | 1765 | 8.5 | 1, 2 |
| cis-p-Menth-2-en-1-ol | 1128 | 1638 | 6.2 | 1, 2 |
| Linalyl acetate | 1253 | 1665 | 50.5 | 1, 2 |
| β-Myrcene | 986 | 1162 | 3.4 | 1, 2, 3 |
| (Z)-β-Ocimene | 1034 | 1243 | 2.3 | 1, 2 |
| α-Pinene | 921 | 1032 | 2.2 | 1, 2, 3 |
| Linalool | 1096 | 1553 | 13.1 | 1, 2, 3 |
| Neryl acetate | 1367 | 2097 | 1.7 | 1, 2 |
| (E)-β-Ocimene | 1044 | 1262 | 1.6 | 1, 2 |
| Sabinene | 966 | 1132 | 1.0 | 1, 2 |
| p-Menth-1-en-8-ol, acetate | 1346 | 1738 | 1.0 | 1, 2 |
| Geraniol | 1255 | 1857 | 0.9 | 1, 2 |
| β-Phellandrene | 1029 | 1218 | 0.3 | 1, 2, 3 |
| β-Pinene | 978 | 1118 | 0.1 | 1, 2, 3 |
| 1,8-Cineole | 1024 | 1213 | 0.1 | 1, 2, 3 |
| Terpinolene | 1083 | 1265 | 0.1 | 1, 2 |
| Terpinen-4-ol | 1173 | 1611 | 0.1 | 1, 2, 3 |
| Octyl acetate | 1208 | 1436 | 0.1 | 1, 2 |
| Citral | 1270 | 1727 | 0.1 | 1, 2 |
| Bornyl acetate | 1284 | 1591 | 0.1 | 1, 2 |
| cis-Limonene oxide | 1132 | 1450 | 0.1 | 1, 2 |
| Caryophyllene | 1408 | 1666 | 0.1 | 1, 2 |
| α-Limonene diepoxide | 1345 | 0.1 | 1, 2 | |
| γ-Elemene | 1436 | 1650 | 0.1 | 1, 2 |
| trans-Nerolidol | 1565 | 2050 | 0.1 | 1, 2 |
| Total | 93.9 | |||
| Monoterpene Hydrocarbons | 11.0 | |||
| Oxygenated Monoterpenes | 82.5 | |||
| Sesquiterpene Hydrocarbons | 0.2 | |||
| Oxygenated Sesquiterpenes | 0.1 | |||
| Other compounds | 0.1 |
| Microorganism | SVO 125 µg/mL | SVO 250 µg/mL | SVO 500 µg/mL | DMSO | Imipenem |
|---|---|---|---|---|---|
| M. luteus | 20.0 ± 1.33 | 21.2 ± 1.21 | 23.5 ± 1.87 | --- | 28 ± 0.23 |
| E. coli | 11.0 ± 1.58 | 10.2 ± 0.87 | 11.3 ± 1.67 | --- | 30 ± 0.10 |
| S. aureus | 13.0 ± 1.88 | 13.8 ± 0.95 | 14.0 ± 1.40 | --- | 24 ± 0.65 |
| P. multocida | 15.8 ± 1.41 | 15.6 ± 1.98 | 16.3 ± 1.76 | --- | 32 ± 0.24 |
| P. aeruginosa | --- | --- | --- | --- | --- |
| B. subtilis | --- | --- | --- | --- | --- |
| S. viridans | 15.3 ± 0.92 | 16.2 ± 2.23 | 18.5 ± 1.45 | --- | 22 ± 0.45 |
| Percent Inhibition of Mycelia Growth | |||||
|---|---|---|---|---|---|
| Microorganism | SVO 125 µg/mL | SVO 250 µg/mL | SVO 500 µg/mL | DMSO | Miconazole |
| T. longifusis | 62.66 ± 1.34 | 63.45 ± 1.45 | 67.65 ± 1.40 | - | 70.98 ± 0.40 |
| C. albicans | 67.32 ± 0.90 | 77.0 ± 1.56 | 83.87 ± 1.98 | - | 89.87 ± 0.22 |
| F. solani | 45.64 ± 1.40 | 56.7 ± 1.21 | 62.96 ± 1.11 | - | 73.98 ± 1.87 |
| M. canis | 30.37 ± 1.97 | 32.33 ± 1.17 | 50.00 ± 1.60 | - | 94.87 ± 0.99 |
| A. flavus | 64.45 ± 1.98 | 67.77 ± 1.88 | 70.97 ± 1.66 | - | 20.56 ± 0.65 |
| C. glabrata | 28.00 ± 1.14 | 61.33 ± 1.40 | 82.35 ± 1.49 | - | 93.98 ± 0.76 |
| Essential Oil | Number of Fronds | Living Fronds | Dead Fronds |
|---|---|---|---|
| 10 µg/mL | 52 | 30 ± 0.22 | 22 ± 1.89 |
| 100 µg/mL | 52 | 21 ± 1.11 | 31± 1.99 |
| 1000 µg/mL | 52 | 22 ± 1.00 | 30 ± 1.40 |
| Essential Oil | Number of Brine Shrimps | Living Brine Shrimps | Dead Brine Shrimps |
|---|---|---|---|
| 10 µg/mL | 30 | 8 ± 1.34 | 22 ± 1.98 |
| 100 µg/mL | 30 | 3 ± 1.00 | 27 ± 1.56 |
| 1000 µg/mL | 30 | 0.9 ± 1.98 | 29.1 ± 1.75 |
3. Experimental Section
3.1. Plant Collection
3.2. Isolation of Volatile Oil
3.3. GC-FID and GC/MS Analyses and Identification of Essential Oil Components
3.4. Antibacterial Activity
3.5. Anti-Fungal Activity
3.6. Phytotoxicity
3.7. Cytotoxicity
3.8. Animals
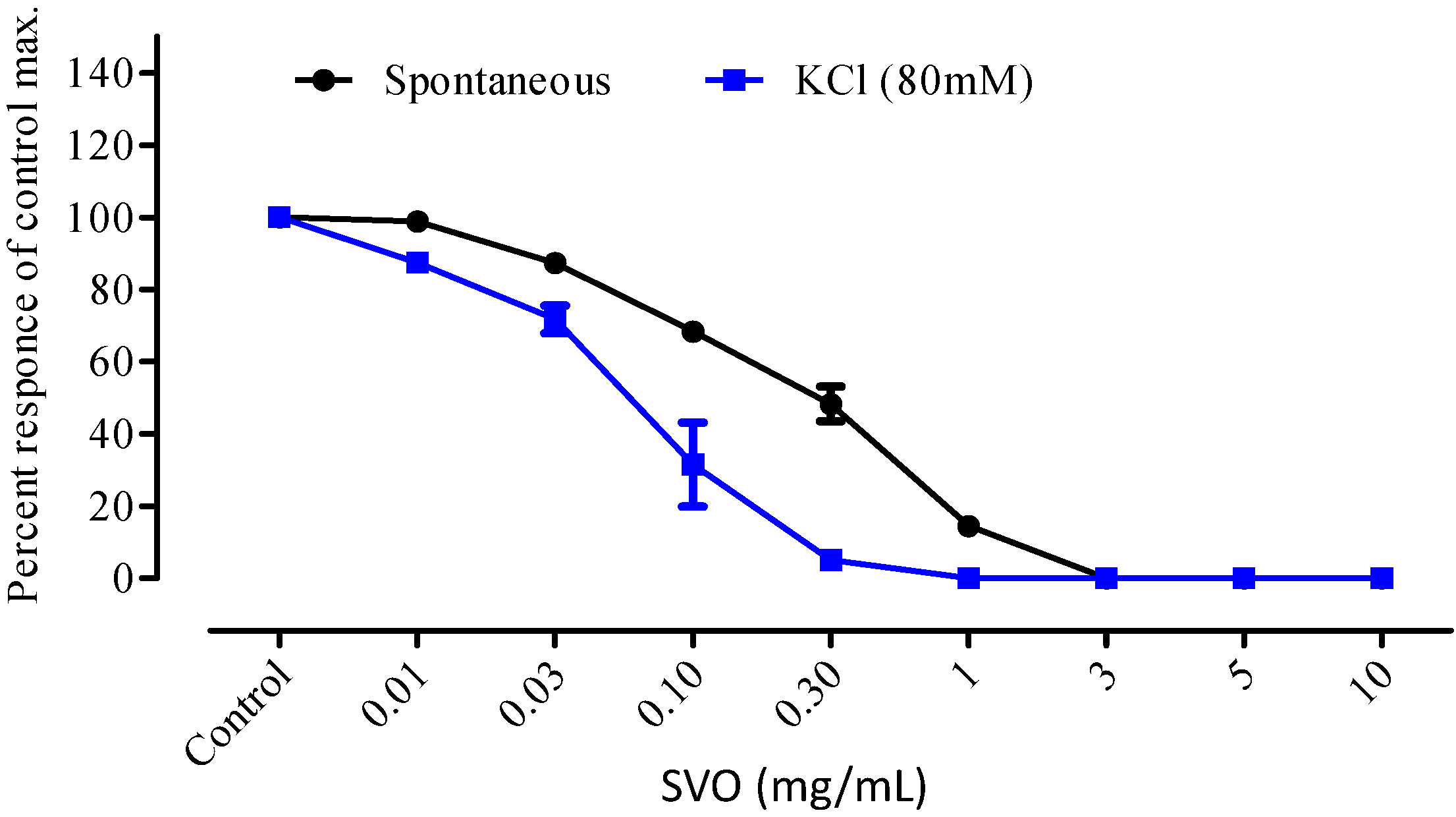
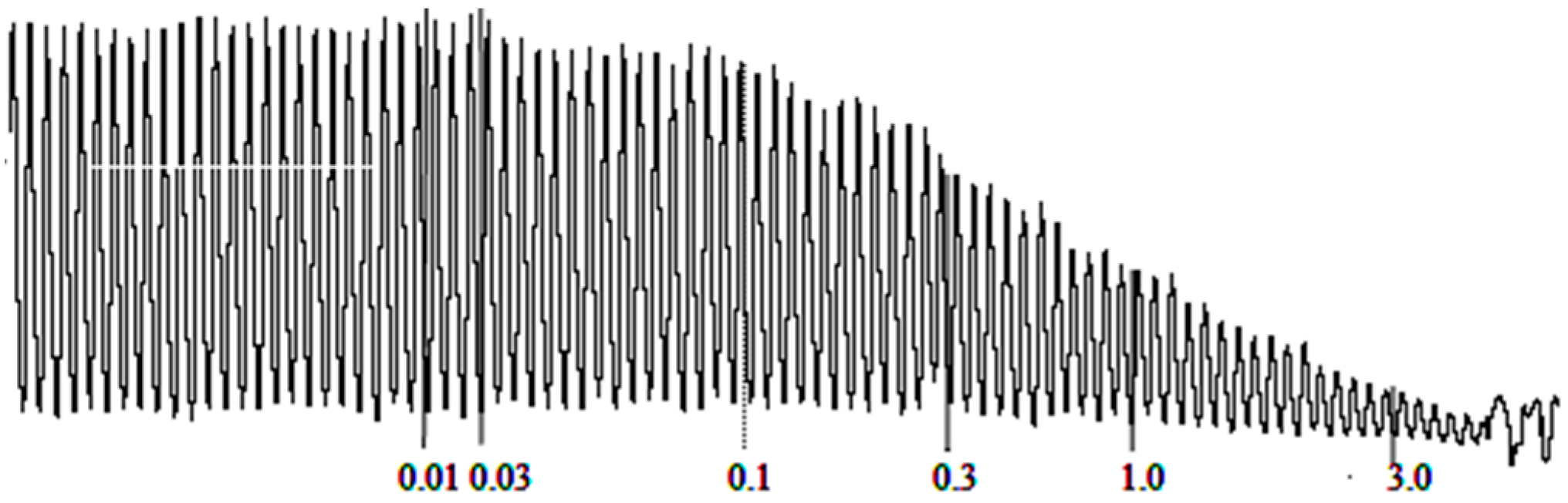
3.9. Antispasmodic Activity
3.10. Statistics and Interpretation
4. Conclusions
Author Contributions
Conflicts of Interest
References and Notes
- Hamayun, M. Traditional uses of some medicinal plants of Swat Valley, Pakistan. Indian J. Tradit. Knowl. 2007, 6, 636–641. [Google Scholar]
- Bhattarai, S.; Chaudhary, R.P.; Taylor, R.S.L. Ethnomedicinal plants used by the people of Manang District, central Nepal. J. Ethnobiol. Ethnomed. 2006, 2, 41. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, R.A.; Ghufran, M.A.; Gilani, S.; Yousaf, Z.; Abbas, G.; Batool, A. Indigenous medicinal plants used by local women in Southern Himalayan regions of Pakistan. Pak. J. Bot. 2009, 41, 19–25. [Google Scholar]
- Shah, W.A.; Qurishi, M.A.; Thappa, R.K.; Dhar, K.L. Seasonal variation in the essential oil composition on Skimmia laureola. Indian Perfurmer 2003, 47, 265–268. [Google Scholar]
- Shah, W.A.; Dar, M.Y.; Kuratull-Ai; Rather, M.A.; Qurishi, M.A. Comparison of terpene composition of Skimmia laureola using hydrodistillation and HS-SPME techniques. J. Essent. Oil Bear. Plants 2013, 15, 116–121. [Google Scholar] [CrossRef]
- Shah, W.A.; Dar, M.Y.; Zagar, M.I.; Agnihotri, V.K.; Qurishi, M.A.; Singh, B. Chemical composition and antimicrobial activity of the leaf essential oil of Skimmia laureola growing wild in Jammu and Kashmir, India. Nat. Prod. Res. 2013, 27, 1023–1027. [Google Scholar] [CrossRef] [PubMed]
- Jangwan, J.S.; Kumar, N.; Singh, R. Analysis of composition and antibacterial activity of essential oil of Skimmia laureola from Garhwal, Himalaya. Internat. J. Chem. Sci. 2010, 8, 1433–1439. [Google Scholar]
- Mathela, C.S.; Melkani, A.B.; Pant, A.K. Reinvestigation of Skimmia laureola essential oil. Indian Perfumer 1992, 36, 217–222. [Google Scholar]
- Sultana, N.; Sultana, R. A new lanostane triterpene from Skimmia laureola. Z. Naturforsch. B 2009, 64, 459–463, and references cited therein. [Google Scholar] [CrossRef]
- Atta-ur-Rahman; Khalid, A.; Sultana, N.; Ghayur, M.N.; Mesaik, M.A.; Khan, M.R; Gilani, A.H.; Choudary, M.I. New cholinesterase inhibiting and calcium blocking alkaloids. J. Enzym. Inhib. Med. Chem. 2006, 21, 703–710. [Google Scholar] [CrossRef]
- Sultana, N.; Afaza, N.; Atta-ut-Rahman. Coumarin and quinoline alkaloids from Skimmia laureola. Sci. Internat. 2004, 16, 271–274. [Google Scholar]
- Mehmood, F.; Manzoor, F.; Khan, Z.D.; Ali, M.I.; Khan, I.; Rahim, S.M.A. Evalutaion of toxicity and repellency of essential oil of family Rutaceae against black ants (Lasius niger) in Pakistan. Asian J. Chem. 2012, 24, 3087–3090. [Google Scholar]
- Muhammad, N.; Barkatullah; Ibrar, M.; Khan, H.; Saeed, M.; Kahn, A.Z.; Kaleem, W.A. In vivo screening of essential oils of Skimmia laureola leaves for antinociceptive and antipyretic activity. Asian Pac. J. Trop. Biomed. 2013, 3, 202–206. [Google Scholar] [CrossRef]
- Sultana, N.; Atta-ur-Rahman; Khan, T.H. Tyrosinase inhibitor fatty ester and a quinoline alkaloid from Skimmia laureola. Z. Naturforsch. B 2005, 60, 1186–1191. [Google Scholar]
- Barkatullah; Ibrar, M.; Muhammad, N.; Rauf, A. Antipyretic and antinociceptive profile of leaves of Skimmia laureola. Middle-East J. Sci. Res. 2013, 14, 1124–1128. [Google Scholar]
- Ahmad, K.F.; Sultana, N. Studies on bioassay directed antifungal activity of medicinal plants Calotropis procera, Skimmia laureola, Peltophorum pterocarpum and two pure natural compounds ulopterol and 4-methoxy-1-methyl-3-(2'S-hydroxy-3'-ene buthyl)-2-quinolone. J. Chem. Soc. Pak. 2003, 25, 328–330. [Google Scholar]
- Riazzudin, S.; Malik, M.M.; Nasim, A. Mutagenicity testing of some medicinal herbs. Environ. Mol. Mutagen. 1987, 10, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Gondwal, M.; Prakash, O.; Vivekanand; Pant, A.K.; Padalia, R.C.; Mathela, C.S. Essential oil composition and antioxidant of leaves and flowers of Skimmia anquetilia N.P. Taylor & Airy Shaw. J. Essent. Oil Res. 2012, 24, 83–90. [Google Scholar] [CrossRef]
- Trombetta, D.; Castelli, F.; Sarpietro, M.G.; Venuti, V.; Cristiani, M.; Daniele, M.; Sajia, A.; Mazzanti, G.; Bisignano, G. Mechanism of antibacterial action of three monoterpenes. Antimicrob. Agents Chemother. 2005, 49, 2474–2478. [Google Scholar] [CrossRef]
- Cleff, M.B.; Meinerz, A.R.; Xavier, M.; Schuch, L.F.; Meireles, M.C.A.; Rodrigues, M.R.A.; Mello, J.R.B. In vitro activity of Origanum vulgare essential oil against Candida species. Braz. J. Microbiol. 2010, 41, 116–123. [Google Scholar]
- Pattnaik, S.; Subramanyam, V.R.; Bapaji, M.; Kole, C.R. Antibacterial and antifungal activity of aromatic constituents of essential oils. Microbios 1997, 89, 39–46. [Google Scholar] [PubMed]
- Hristova, Y.; Gochev, V.; Wanner, J.; Jirovetz, L.; Schmidt, E.; Girova, T.; Kuzmanov, A. Chemical composition and antifungal activity of essential oil of Salvia sclarea L. from Bulgaria against clinical isolates of Candida species. J. Biosci. Biothechnol. 2013, 2, 39–44. [Google Scholar]
- Tworkoski, T. Herbicide effects of essential oils. Weed Sci. 2002, 50, 425–431. [Google Scholar] [CrossRef]
- De Martino, L.; Mancini, E.; Marandino, A.; Rolim de Almeida, L.F.; De Feo, V. Chemistry and antigerminative activity of essential oils and monoterpenoids from Mediterranean Plants. Curr. Bioactive Comp. 2012, 8, 13–49. [Google Scholar] [CrossRef]
- De Martino, L.; Mancini, E.; Rolim de Almeida, L.F.; De Feo, V. The antigerminative activity of twenty-seven monoterpenes. Molecules 2012, 15, 6630–6637. [Google Scholar] [CrossRef]
- Moshafi, M.H.; Sharififar, F.; Dehghan, G.R.; Ameri, A. Bioassay screening of essential oil and various extracts of fruits of Heracleum persicum Desf. and rhizomes of Zingiber officinale Rosc. using brine shrimp cytotoxicity assay. Iranian J. Pharm. Res. 2009, 8, 59–63. [Google Scholar]
- Krishnaraju, A.V.; Rao-Tayi, V.N.; Sundararaju, D.; Vanisree, M.; Tsay, H.S.; Subbaraju, G.V. Assessment of bioactivity of Indian medical plants using brine shrimp (Artemia salina) lethality assay. Int. J. Appl. Sci. Eng. 2005, 3, 125–134. [Google Scholar]
- European Pharmacopoeia, 5th ed.; Council of Europe: Strasbourg Cedex, France, 2004; Volume I, pp. 217–218.
- Jennings, W.; Shibamoto, T. Qualitative Analysis of Flavour and Fragrance Volatiles by Glass Capillary Gas Chromatography; Academic Press: New York, NY, USA, 1980. [Google Scholar]
- Davies, N.W. Gas chromatographic retention indices of monoterpenes and sesquiterpenes on methyl silicone and Carbowax 20M phases. J. Chromatogr. A 1990, 503, 1–24. [Google Scholar] [CrossRef]
- Adams, P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectrometry, 4th ed.; Allured Publishing Co.: Carol Stream, IL, USA, 2007. [Google Scholar]
- Goodner, K.L. Practical retention index models of OV-101, DB-1, DB-5, and DB-Wax for flavor and fragrance compounds. LWT-Food Sci. Technol. 2008, 41, 951–958. [Google Scholar] [CrossRef]
- Wiley Registry of Mass Spectral Data, with NIST Spectral Data CD Rom, 7th ed.; John Wiley & Sons: New York, NY, USA, 1998.
- Barkatullah; Ibrar, M.; Muhammad, N. Evaluation of Zanthoxylum armatum DC. for in vitro and in vivo pharmacological screening. Afr. J. Pharm. Pharmacol. 2011, 5, 1718–1723. [Google Scholar] [CrossRef]
- Gilani, A.H.; Khan, A.; Jabeen, Q.; Subhan, F.; Ghafar, R. Antispasmodic and blood pressure lowering effects of Valeriana wallichii are mediated through K+ channel activation. J. Ethnopharmacol. 2005, 100, 347–352. [Google Scholar] [CrossRef]
- Sample Availability: Samples of the essential oil are available from the authors.
© 2015 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barkatullah; Ibrar, M.; Muhammad, N.; De Feo, V. Chemical Composition and Biological Activities of the Essential Oil of Skimmia laureola Leaves. Molecules 2015, 20, 4735-4745. https://doi.org/10.3390/molecules20034735
Barkatullah, Ibrar M, Muhammad N, De Feo V. Chemical Composition and Biological Activities of the Essential Oil of Skimmia laureola Leaves. Molecules. 2015; 20(3):4735-4745. https://doi.org/10.3390/molecules20034735
Chicago/Turabian StyleBarkatullah, Muhammad Ibrar, Naveed Muhammad, and Vincenzo De Feo. 2015. "Chemical Composition and Biological Activities of the Essential Oil of Skimmia laureola Leaves" Molecules 20, no. 3: 4735-4745. https://doi.org/10.3390/molecules20034735






